Birthing under the Condition of the COVID-19 Pandemic in Germany: Interviews with Mothers, Partners, and Obstetric Health Care Workers
Abstract
:1. Introduction
Objective
- A.
- What was the subjective impact of the restrictions to contain the COVID-19 pandemic on birth experiences from (becoming) mother’s and partner’s perspectives?
- 1.
- How did the COVID-19 regulations impact all phases of birth from the mother’s perspectives?
- a.
- During the first phase of birth?
- b.
- At the delivery room?
- c.
- At the maternity ward?
- 2.
- How was the accompanying partner affected?
- 3.
- How could the perceived burdens be managed?
- 4.
- How did a COVID-19 diagnosis challenge the birth?
- B.
- What was the impact of COVID-19 pandemic restrictions on childbirth from the perspective of obstetric staff?
- 1.
- What adjustments did the COVID-19 pandemic containment rules require?
- 2.
- How was the caring for the (pregnant) women affected?
- 3.
- How were the professional obstetric standards affected?
- 4.
- How did the mothers (and partners) cope with the restrictions from the professionals’ point of view?
- 5.
- How could the birth of COVID-19 infected mothers be managed?
- C.
- What were resilience and weakness factors of obstetric health care under COVID-19 conditions?
2. Materials and Methods
2.1. Data Collection
2.2. Data Analysis
2.3. Triangulation
2.4. Ethical Considerations
3. Results
3.1. How Did the COVID-19 Regulations Impact All Phases of Birth and Pregnancy from the Mother’s and Partner’s Perspectives?
3.1.1. During the First Phase of Birth
3.1.2. At the Delivery Room
3.1.3. At the Maternity Ward
3.2. How Was the Accompanying Partner Affected?
3.3. How Could the Perceived Burdens Be Managed?
3.4. How Did a COVID-19 Diagnosis Challenge a Birth?
3.5. Obstetric HCW Interviews
3.6. What Adjustments Did the COVID-19 Pandemic Containment Rules Require?
3.6.1. How Was the Care for the Women Affected?
3.6.2. Perception of the No-Visit Policy on the Ward
3.7. How Were Professional Obstetric Standards Affected?
3.8. How Did the Mothers (and Partners) Cope with the Restrictions from the Professionals’ Point of View?
3.9. How Could the Birth of COVID-19 Infected Mothers Be Managed?
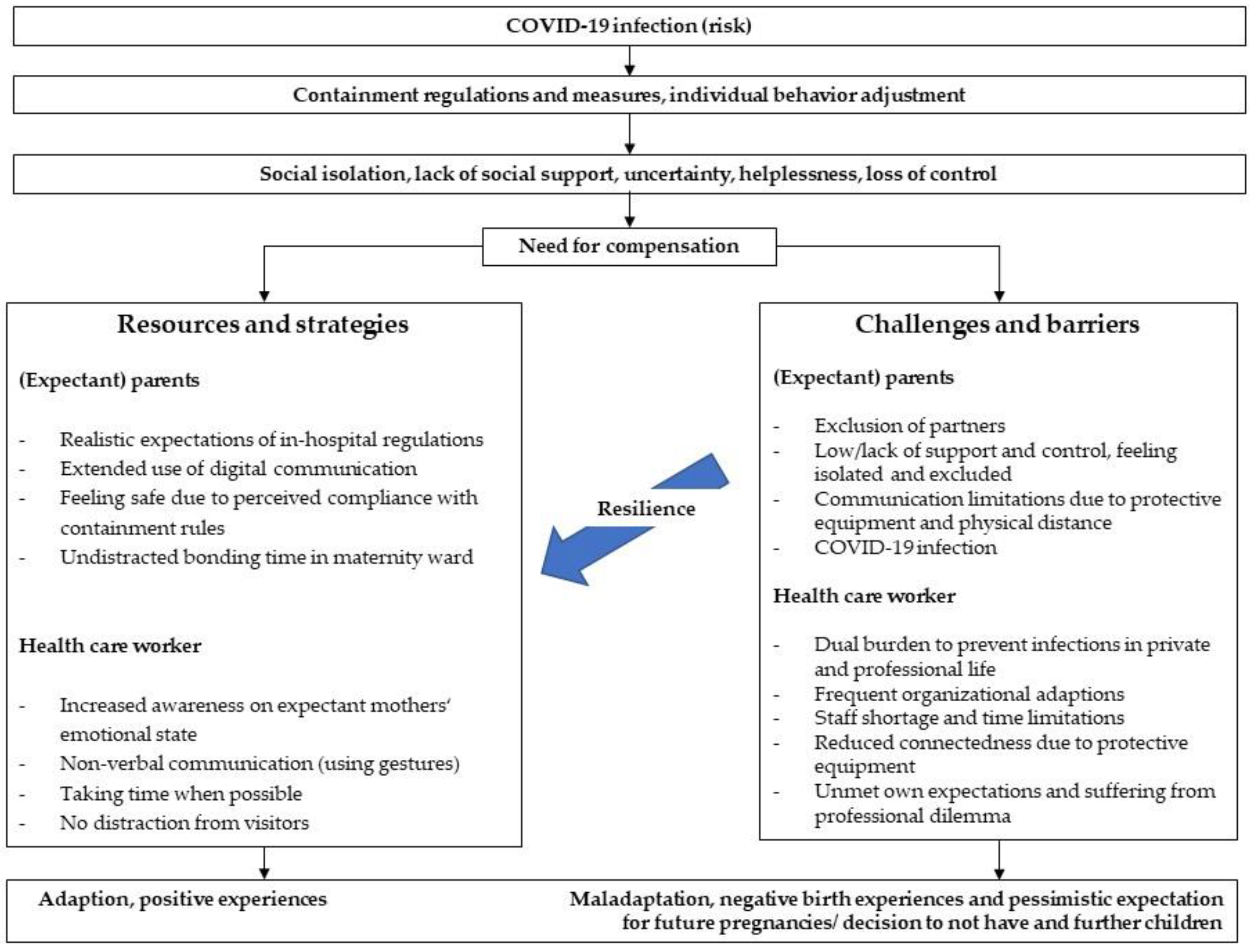
3.10. What Were Resilience and Weakness Factors of Obstetric Health Care under COVID-19 Conditions?
4. Discussion
4.1. How Do the COVID-19 Restriction Rules Affect all Phases of Pregnancy from Mothers and Professionals’ Perspectives?
4.2. How Is the Role of the Partners and the Professional Obstetrics Standard Impacted?
4.3. How Are the Perceived Burdens Managed?
4.4. How Is a COVID-19 Diagnosis Challenging the Birth from Women’s and Staff Perspectives?
4.5. Resilience and Weakness of the Obstetric Health Care under the COVID-19 Conditions
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| A.1. How Did the COVID-19 Regulations Impact All Phases of Birth and Pregnancy from the Mother’s and Partner’s Perspectives? |
|---|
| A.1a During the first phase of birth |
| “I went out with these strong labor pains and tried to wait for my husband, but it didn’t work at all. I couldn’t get a hundred meters and had to stop every few meters to breathe the contractions and that’s when I actually felt very alone” (M_07). |
| “And also this helplessness. This being left alone. Knowing my husband is outside. He could help me. He knows me. My history. My fears”(M_21). |
| “My water broke and then we went straight away, but it was then three o’clock in the morning and there was only the bell available, and we were then told that I was welcome to come to the delivery room. Without a partner for the time being. And then I had frequent strong contractions and it was unbelievably difficult to find the delivery room and I walked in the wrong direction at first. After a few pauses in labor in the corridor, I eventually reached the delivery room (M_35). |
| A.1b At the delivery room |
| “When I went into the delivery room, it was much more relaxed than the time before. It was a bit because my husband was there and not only my husband, but also the midwives who were there all the time, also the doctor, more or less all the time, who took care of me” (M_01). |
| “Fortunately, we still had a beautiful birth, although compared to the previous births, this time of course with a mask. It just causes an extreme distance in general. And acoustically. I often didn’t understand anything that was said to me. But luckily, I had my husband with me, who was able to translate everything for me” (M_02). |
| “So of course, all the doctors wear masks all the time. That’s always a bit difficult, especially if you’re somehow, yes, maybe unconfident and want to build up trust, it’s of course nicer to look into a face than to only be able to look into two eyes” (M_05). |
| “And then they left us alone for quite a long time. Which I thought was nice. I don’t know if that’s normal. But now with Corona it’s so that your husband isn’t allowed to visit you either, that you’re completely alone in the maternity ward. And maybe because of that, and maybe also because they still had enough capacity, thank God, we were allowed to stay for a really long time. And that was really wonderful. It was really nice” (M_24). |
| A.1c At the maternity ward |
| “No one was allowed to visit the maternity ward. I found that a bit worrying, because you think, “OK—you’re on your own for a few days, completely. And you feel a bit uneasy because it’s unpleasant, especially after a C-section, that you always have to ring the bell and ask a stranger for help. Of course, it would have been nicer if your partner was at least there to say “OK, help me with this”. You feel a bit stupid when you have to ask the midwives and nurses all the time” (M_04). |
| “I have to be honest, I liked it from the beginning. I knew that no visitors were allowed in because of Corona. Understandable and comprehensible, and I think it’s all the better because you simply need peace and quiet, and it’s difficult to get peace and quiet in the clinic. Simply because in our room, there were three of us plus babies, six, and then there was a new person in our room every half hour anyway. Yes, the staff, midwives, then nurses, doctors or other people who wanted to ask something and brought food or cleaned and I found it exhausting that the door was always opening and closing. So if partners from the other women had also come, that would have been too much for all of us” (M_16). |
| A.2 How was the partner affected? |
| “You have to go and then you put everything in her hands, yeah, there’s not much I can do now. Except of talk to her on the phone, but it was strange. Also a bit helpless, even before. But we both talked about the fact that I might not be allowed to be present at the birth because of the current situation, and I had to fight hard to deal with that. I have to admit that (...) and yes, you just accept it. What else can you do” (M_18_Partner)? |
| “He had to stand outside in the cold. And of course, when the woman from the delivery room calls and says, “Come up now” but the security won’t let him in, it was a very difficult situation for him, too” (M_ 07). |
| “At noon during this walk it looked like the birth was about to start, because we were having labor pains every ten minutes. (…) I brought her back to the ward and then she had this collapse, which I didn’t notice. I sat outside in the car and thought about it. Two hours later, when I still hadn’t received an answer to my 18 WhatsApps, I started calling the ward. They said she was no longer on the ward. So I thought, okay, then it must have actually started. Then why didn’t anyone tell me? And then I called the delivery room and the person said, ‘I couldn’t give you any information’. Yes, of course I understand on the phone. But something must be going on. In the end, however, my wife called me (…) and then I was led in (...) My wife was lying there. She was just completely in a daze. Delirious. She was so out with pain that she could hardly react. Every touch was just a hell of a pain” (M_21_Partner). |
| In the maternity room: “My husband was told: ‘Wait a minute, you are not allowed to go out the door, not allowed to leave the room’. That was quite difficult because we were there for four days. Then you’re in a room for four days and you’re not allowed to leave it either. Not at all” (M_07). |
| A.3 How could the perceived burdens be managed? |
| So I think it was actually less bad for me than for my husband. Well, modern media makes it possible. I made an unbelievable number of phone calls. Also with video and so on. Yes, otherwise it’s like an unfamiliar child that comes home at some point. That’s how it feels” (M_27). |
| “But when I was brought into the delivery room (...) the midwife told me to call my husband now. He can come in now, although the cervix is not yet open enough. But because the contractions come at such short intervals, she said it would be good for me to have some support” (M_37). |
| “Fortunately, I have to say that I personally found the people who always came totally nice and pleasant. And I never had the feeling that they were somehow annoyed or something, but they always helped with everything and came by regularly. So despite my fears about Corona and the fact that no one is allowed to visit, I didn’t feel pushed away or, rather, that they put a lot of work into it, that they were still there to support the women” (M_04). |
| He was diagnosed with [a handicap] and, of course, further examinations had to take place. That’s why we had to stay two more nights. However, the doctors made it possible, even though men were not allowed in the neonatal ward at that time, for him (partner) to stay” (M_02). |
| “The midwife joined me, she took my backpack and my suitcase. The security man also helped me with my things, it was very nice. She also put it [newborn] on the baby seat and then put a blanket on her, that was very pleasant” (M_22). |
| So I think it was actually less bad for me than for my husband. Well, modern media makes it possible. I made an unbelievable number of phone calls. Also with video and so on. Yes, otherwise it’s like an unfamiliar child that comes home at some point. That’s how it feels” (M_27). |
| A.4 How did a COVID-19 diagnosis challenge the birth |
| “I was walking around there normally all day; I was in the corridor all day and at half past three they came and told me that. And from then on, everything went off the rails, really. As soon as this test result was in the air, it felt like only Martians came to see me. (...) I can’t understand how such a test result can cause such changes. Even within the people, the same people still looked after me. They were just behind a mask. This positive test made people completely different from what they were before” (M_13_Birth in Jan). |
| I didn’t know about many people during my stay. Whether they are midwives or doctors. (...) There were no name tags either. They were completely hooded, so to speak” (M_37_Birth in May). |
| “I felt quite socially isolated. At some point I moved into the separation room. I was then isolated again with my baby monitor, so to speak. All these standards, ‘why don’t you go for a walk’, all took place in these ten square meters. And I think that’s why it took so long with the birth. That means I was there for 24 h, during which my cervix opened maybe one centimeter, but the whole time I was in labor without a partner, without going for a walk, without anything else. (...) I took two showers in between, kind of warm. At least to be able to do something” (M_37_Birth in May). |
| “That night I had such pain, but I didn’t know where the phone was, and I just screamed. And they only heard me through my screaming and then came to me. And then they criticized me for not calling” (M_13_Birth in Jan 2021). |
| “Until the afternoon, I stayed with the thought that he was not allowed to be there, my partner. He talked to the head of the clinic or the ward about why that wasn’t possible. And they in turn said that this would have to be discussed with the hygiene commission. And then in the evening the information came that he could be present in the delivery room.” (…) “I can only keep saying, I don’t know how this would have gone if my partner hadn’t been there” (M_37_Birth in May). |
| “It was still the case that when I rang the bell, it took a while before someone was there. Which wasn’t easy, of course, because sometimes she [newborn] cried a bit and, because this is my first child, I didn’t know exactly how to put her on. When someone was there, I felt well looked after. So everything was okay so far. It just took a long time” (M_M37_Birth in May). |
| “So mentally I had already come to the conclusion that I didn’t want to go through the vaginal birthing process alone, that I didn’t have the strength for it. But then they tried to persuade me and my husband (on the phone) also said ‘go for it’ (…) „I was just crying the whole time. I just said, ‚this is not how I imagined it’. I had to keep the mask on, the whole time. I think that was the worst thing. I didn’t even say goodbye to my husband because I was so exhausted. And then they took her out [of the uterus] and I couldn’t be happy at all, about my child. And the midwife said, ‘Why aren’t you happy about your child’ and I said ‘I can’t be happy about my child’. It was very damaging for me. I couldn’t hold her. Everything was so sterile that it was really horrible for me” (M_13_Birth in Jan). |
| “But sometimes I really asked myself the question: ‘Am I exaggerating now? Can’t I just take it, what’s the problem now?’ So you put the blame on yourself like that, partly. ‘Why are people treating me like this (…) It was a traumatic experience, I definitely don’t want another child in the future. That was it for me. I can’t imagine it [giving birth again] any more” (M_13_Birth in Jan)? |
| B.1 What Adjustments Did the COVID-19 Pandemic Containment Rules Require? |
|---|
| “I myself was also shocked that we could be in such a situation here in Germany in 2020. And then we realized that it’s really severe now. And of course, we consulted with our bosses about what we could do to calm down the patients. Because everyone of us was afraid somehow” (HCW_03_Assistant). |
| “All of a sudden there were an incredible number of rules. Starting with wearing a face mask in the clinic, disinfecting your hands, showing your staff ID, in the past you went in and out, you had to make sure there were spare clothes in your locker so you could always change” (HCW_06_Midwife). |
| “We had two wards, one of which was for the women who did not yet have the result of the COVID test. If possible, they were not allowed to lie together in the same room. So it was a huge organizational effort that had to be made” (HCW_05_Midwife). |
| “After weekends or days off, we were asked who we had been in contact with. Where we were. Sometimes we were not allowed to visit relatives who lived 50 km away. And holidays were cancelled for the time being” (HCW_03_Assistant). |
| “I had, you could say, the luxury situation that he [interviewees’ child] was allowed to go to daycare. But only as long as I worked. So I found this time brutally exhausting. Because I was either at work or I had my child 24 h a day, seven days a week. And then the playgrounds were closed. Then you weren’t allowed to go to the swimming pool. You weren’t allowed to meet anyone. That was really hard” (HCW_05_Midwife). |
| B.2a How was the care for the women affected? |
| “The facial expressions, you can’t do them anymore, it’s funny. (...) You still have the words. I don’t know if people have got into the habit of doing more with their hands. That might be interesting. I don’t know if you suddenly use more gestures. But I think we still communicated well with the women” (HCW_07_Doctor). |
| “They don’t see any emotions at all and they don’t know what you mean. And maybe you say something joking and they don’t know any German anyway and then they just don’t understand any more” (HCW_09_Nurse). |
| “Yes, speaking more clearly, demonstrating many things, what you mean or gesturing a lot with your hands. We must look at the breast or at the lower part of the body, then I point to my eyes, ‘look’ here, I always make sure that the women are very independent (…) I talk to her. Or, yes, in extreme cases I sometimes get a chair, sit down next to them, let them cry first, listen to their problem, I can either take care of it or sometimes they just need someone to, yes, cry to and tell me what’s going on and then they often say ‘I feel much better now, thank you for listening to me, nobody listens to me’” (HCW_09_Nurse). |
| “Also in terms of induction of labor, that is also a burden. They want support, they don’t have that at the time” (HCW_07_Doctor). |
| “The men still pick up their wives and we join the women and the children outside the door. That is always a very nice moment. I like to do that, too. That is always wonderful” (HCW_01_Nurse). |
| “The facial expressions, you can’t do them anymore, it’s funny. (...) You still have the words. I don’t know if people have got into the habit of doing more with their hands. That might be interesting. I don’t know if you suddenly use more gestures. But I think we still communicated well with the women” (HCW_07_Doctor). |
| B 2b. Perception of the no-visit policy on the ward |
| “So after the birth, (...) the women can concentrate extremely well on the child. (…) The child was actually in their arms all the time, it was nice to be in contact, because they were alone in the hospital, but ‘well, I have my child, and it’s with me,’ and that we sometimes had the feeling that the positive thing was that they didn’t have to worry about the mother-in-law who was sitting next to their bed. They only had their child and that was actually quite good” (HCW_10_Midwife). |
| “But I think the men are missing. Yes, simply as emotional support and I think they also support nursing activities when the woman, yes, there are also very temperamental women who first have to be brought down a bit by their husband and also understand the view of us as nurses and who then sit in our boat and only want the best for the women, I think that’s quite cool” (HCW_09_Nurse). |
| “A lot of women wanted to be discharged early. I noticed that and some of the midwives said that they went home even though some of them were not yet coping very well. We don’t know how things went on in outpatient care. Whether they stopped breastfeeding more. Or whether the children lost more weight. Or whether they got more ” (HCW_07_Doctor). |
| “And we have already discussed in the team that when everything is back to normal and the visiting hours are also normal, that we can perhaps somehow take something with us, that the visiting hours are somehow extremely shortened. And that it wouldn’t be the same as before, with whole busloads coming in, but that we could control it a bit” (HCW_02_Nurse). |
| B.3 How were professional obstetric standards affected? |
| “One coworker had a crying man standing in front of the door, begging and pleading with her to come in and she had to tell him ‘I can’t’ and afterwards she said, ‘I won’t do it again. I can’t do that’ (…) That was terrible, because we don’t want to work like that at all, because that is not our attitude towards birth at all, because accompanying persons or relatives, father or whoever, are simply very, very essential during birth and that was very difficult to really explain to people, of course it was met with resentment, but secondarily it had the effect that the number of patients dropped rapidly” (HCW_10_Midwife). |
| “What we have been working for years, that the fathers or the next of kin, the second parent, are integrated, that they are recognized as a full part of the pregnancy and that this has finally been established, was such a setback. That they really weren’t present at any preventive care and that it was again a ‘it’s outside and not important enough’, so to speak. I think that was difficult and the crowning glory of it all was that they were not allowed to be present at the birth either. That was a pity because the current image of parents, not just the mother, not only the woman, but the family is actually at the center, was crushed. I know why and I understand why, but it would be a bad thing if it were to be lost” (HCW_10_Midwife). |
| “And we are a hospital with a level of care that there are not so many of and that cannot be replaced. Let me say that if a hospital with 200 births [a year] closes because Corona breaks out, that’s not a bad thing, but if that were the case here, there would simply be no more important care places. That was the issue where we said we understood the logic, the infection control, and hopefully we only have such a special time once in our lives, so everyone has to go along with it and live with it” (HCW_10_Midwife). |
| B.4 How did the mothers (and partners) cope with the restrictions from the professionals’ point of view? |
| “In the beginning you had to explain a lot. You had to fight a lot against a bit of incomprehension. And then we had to say again and again that these are simply rules that the clinic management has set up. It’s not something we determine personally. And we have to stick to them” (HCW_07_Doctor). |
| And of course there were some, as there always are, who got very upset about it and what a mess it would be and that was not acceptable at all. But I have to say that I understood (...) that it is a stupid situation when you are already emotionally in this situation. And then your wife is in the clinic and you are sitting outside in the cold or heat and can’t do anything. Of course, you also feel helpless in the situation (HCW_08_Midwife). |
| “Does the partner have to wear a mask all the time?’ People had a hard time with that, although sometimes we thought, well, we also wear a mask all the time and it’s appropriate. So it’s acceptable for the man in particular. And in the case of the woman, if the test is negative, she can take off the mask. But we are still struggling with the fact that some of the men do not accept that they have to keep it on” (HCW_07_Doctor). |
| “The women, because they also got tips from us that they should go for a walk to stimulate the birth, liked to go out to their husbands in the car park and have lunch together, for example. So, that’s nice to see” (HCW_06_Midwife). |
| “Exactly, when they are fit enough that the activity on the mobile phone has increased. Whether it’s texting, video chatting or doing anything else on the phone, it’s showing up more now in this phase” (HCW_06_Midwife). |
| B.5 How could the birth of COVID-19-infected women be managed? |
| “The women were treated like lepers, you never saw anyone. If someone came, he or she was so fully packed, you couldn’t see a face, and that was really bad for the women. And we also had some cases that were discovered here and that was particularly bad (...) with this Corona test result, they were suddenly in isolation, so to speak, suddenly no one was there. This turnaround in between was always really bad. (…) Often they were also weakened physically in some way and were so worried about what might happen to the child. That was really bad“ (HCW_10_Midwife). |
| “I think it’s even more difficult in all that protective material and the woman with the mouth cover when they’re wrapped up like that and the woman is in a lot of pain and struggling to breathe, it was even more difficult to stand. Because this equipment alone gives you even more distance. So I had the feeling that I made an extra effort to discuss things or to verbalize them, because I noticed that this visual aspect was missing. But whether that helped the women much in the situation, I don’t know” (HCW_04_Doctor). |
| “But all in all, we have tried to provide just as good care as we do for women who are not isolated. But of course, the frequency with which you are in the room is lower. Most of the time you are in the room longer, because when you go in you take everything with you. And then you stay longer. So, they have already received good care, but you are not in the room as often as with a woman who is usually in the ward” (HCW_08_Midwife). |
| “You kind of want to be there and be close, but you know you have to be careful. For example, last year in spring, when we didn’t have a vaccination, I was never really worried that I would catch it. My worry was always that if I made a mistake here, if I got infected and then transmitted it and the other women in our delivery room got infected, that was my worry. And that was very difficult. And at the same time, we wanted to be there for the women who were positive and perhaps had to go through their birth alone. We always tried to make sure that no woman, who was in pain during the birth was isolated, alone, but I think is was still difficult and unlike the usual birth care” (HCW_10_Midwife). |
| “I took in one patient. She was not well. She had breathing difficulties. She actually died of Corona” (HCW_04_Doctor). |
References
- Bruinen de Bruin, Y.; Lequarre, A.-S.; McCourt, J.; Clevestig, P.; Pigazzani, F.; Zare Jeddi, M.; Colosio, C.; Goulart, M. Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Saf. Sci. 2020, 128, 104773. [Google Scholar] [CrossRef]
- Deutscher Bundestag, German infection Protection Act. Gesetz zum Schutz der Bevölkerung bei einer epidemischen Lage nationaler Tragweite. Bundesgesetzblatt 2020, 2020, 587–592. [Google Scholar]
- Collaborative, C.O. Global guidance for surgical care during the COVID-19 pandemic. Br. J. Surg. 2020, 107, 1097–1103. [Google Scholar] [CrossRef] [Green Version]
- Deutsches Ärzteblatt, Mangel an Schutzmasken Behindert Kampf Gegen SARS-CoV-2. Available online: https://www.aerzteblatt.de/nachrichten/110812/Mangel-an-Schutzmasken-behindert-Kampf-gegen-SARS-CoV-2 (accessed on 12 January 2022).
- Schreyögg, J. Corona-Krise trifft auf Strukturprobleme im Gesundheitswesen. Wirtschaftsdienst 2020, 100, 226–227. [Google Scholar] [CrossRef] [Green Version]
- Michalowsky, B.; Hoffmann, W.; Bohlken, J.; Kostev, K. Effect of the COVID-19 lockdown on disease recognition and utilisation of healthcare services in the older population in Germany: A cross-sectional study. Age Ageing 2020, 50, 317–325. [Google Scholar] [CrossRef]
- Dopfer, C.; Wetzke, M.; Zychlinsky Scharff, A.; Mueller, F.; Dressler, F.; Baumann, U.; Sasse, M.; Hansen, G.; Jablonka, A.; Happle, C. COVID-19 related reduction in pediatric emergency healthcare utilization—A concerning trend. BMC Pediatr. 2020, 20, 427. [Google Scholar] [CrossRef]
- Alfieri, N.; Manodoro, S.; Marconi, A.M. COVID-19 does not stop obstetrics: What we need to change to go on safely birthing. The experience of a University Obstetrics and Gynecology Department in Milan. J. Perinat. Med. 2020, 48, 997–1000. [Google Scholar] [CrossRef]
- Smith, V.; Flaherty, S.J.; Matvienko-Sikar, K.; Delaney, H. Maternity care during COVID-19: A protocol for a qualitative evidence synthesis of women’s and maternity care providers’ views and experiences. version 1; peer review: 2 approved, 1 approved with reservations. HRB Open Res. 2021, 4, 21. [Google Scholar] [CrossRef]
- WHO. WHO’s World Patient Safety Day Goals 2021 Promote Safe Maternal and Newborn Practices. Available online: https://www.who.int/news/item/16-09-2021-who-s-world-patient-safety-day-goals-2021-promote-safe-maternal-and-newborn-practices (accessed on 14 January 2021).
- Coxon, K.; Turienzo, C.F.; Kweekel, L.; Goodarzi, B.; Brigante, L.; Simon, A.; Lanau, M.M. The impact of the coronavirus (COVID-19) pandemic on maternity care in Europe. Midwifery 2020, 88, 102779. [Google Scholar] [CrossRef]
- Bailey, E.; Nightingale, S. Navigating maternity service redesign in a global pandemic: A report from the field. Midwifery 2020, 89, 102780. [Google Scholar] [CrossRef]
- Bender, W.R.; Srinivas, S.; Coutifaris, P.; Acker, A.; Hirshberg, A. The Psychological Experience of Obstetric Patients and Health Care Workers after Implementation of Universal SARS-CoV-2 Testing. Am. J. Perinatol. 2020, 37, 1271–1279. [Google Scholar] [CrossRef]
- World Health Organization (WHO); Regional Office for Europe. Fatherhood and Health Outcomes in Europe: A Summary Report. Available online: https://www.euro.who.int/__data/assets/pdf_file/0019/69013/E91129sum.pdf (accessed on 14 January 2022).
- Lista, G.; Bresesti, I. Fatherhood during the COVID-19 pandemic: An unexpected turnaround. Early Hum. Dev. 2020, 144, 105048. [Google Scholar] [CrossRef] [PubMed]
- Helmy Abdelmalek Fahmy, E.; Yeap, B.T.; Pg Baharuddin, D.M.; M A Abdelhafez, M.; Than, W.W.; Soe, M.Z.; Hayati, F.; Chin, Y.S. Obstetric challenges during COVID-19 pandemic: A narrative review. Ann. Med. Surg. 2021, 71, 102995. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, N.; Mattern, E.; Cignacco, E.; Seliger, G.; König-Bachmann, M.; Striebich, S.; Ayerle, G.M. Effects of the Covid-19 pandemic on maternity staff in 2020—A scoping review. BMC Health Serv. Res. 2021, 21, 1364. [Google Scholar] [CrossRef] [PubMed]
- Green, L.; Fateen, D.; Gupta, D.; McHale, T.; Nelson, T.; Mishori, R. Providing women’s health care during COVID-19: Personal and professional challenges faced by health workers. Int. J. Gynecol. Obstet. 2020, 151, 3–6. [Google Scholar] [CrossRef]
- Mojdeh, B.; Vida, G.; Marzieh, S.G.N.; Zahra, K.; Farzaneh, R.-F.; Sedigheh, B.B.; Behzad, M.S.; Mohsen, R. Obstetrics and Neonatal Outcomes in Pregnant Women with COVID-19: A Systematic Review. Iran. J. Public Health 2020, 49, 38. [Google Scholar] [CrossRef]
- Arab, W.; Atallah, D. Cesarean section rates in the COVID-19 era: False alarms and the safety of the mother and child. Eur. J. Midwifery 2021, 5, 1–2. [Google Scholar] [CrossRef]
- Kasaven, L.; Saso, S.; Barcroft, J.; Yazbek, J.; Joash, K.; Stalder, C.; Ben Nagi, J.; Smith, J.; Lees, C.; Bourne, T.; et al. Implications for the future of Obstetrics and Gynaecology following the COVID-19 pandemic: A commentary. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 1318–1323. [Google Scholar] [CrossRef]
- Armbrust, R.; Untch, M.; Ramsauer, B.; Scharf, J.-P.; Rohne, J.; Mangler, M.; Lanowska, M.; Dombrowski, M.; Hartmann, W.; Barinoff, J.; et al. Die Versorgung gynäkologischer und geburtsmedizinischer Patientinnen in der COVID-19-Pandemie. Ein Zwischenbericht des COVID-19-Aktionsbündnis der “Berliner Frauenkliniken”. Geburtshilfe Frauenheilkd 2021, 81, 1014–1017. [Google Scholar]
- Huener, B.; Derksen, C.; Schmiedhofer, M.; Lippke, S.; Janni, W.; Scholz, C. Preventable Adverse Events in Obstetrics—Systemic Assessment of Their Incidence and Linked Risk Factors. Healthcare 2022, 10, 97. [Google Scholar] [CrossRef]
- Lippke, S.; Wienert, J.; Keller, F.M.; Derksen, C.; Welp, A.; Kotting, L.; Hofreuter-Gatgens, K.; Muller, H.; Louwen, F.; Weigand, M.; et al. Communication and patient safety in gynecology and obstetrics—Study protocol of an intervention study. BMC Health Serv. Res. 2019, 19, 908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schreier, M. Sampling and generalization. In The Sage Handbook of Qualitative Data Collection; Flick, U., Ed.; SAGE: London, UK, 2018; pp. 84–98. [Google Scholar]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef] [PubMed]
- Schreier, M. Qualitative Content Analysis in Practice; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Flick, U. Triangulation. Eine Einführung. 3. Aktualisierte Einführung; Springer Fachmedizin GmbH: Wiesbaden, Germany, 2011. [Google Scholar]
- Corbin, J.; Morse, J.M. The Unstructured Interactive Interview: Issues of Reciprocity and Risks when Dealing with Sensitive Topics. Qual. Inq. 2003, 9, 335–354. [Google Scholar] [CrossRef]
- Gläser, J.; Laudel, G. Experteninterviews und Qualitative Inhaltsanalyse als Instrumente Rekonstruierende Untersuchungen, 4th ed.; VS Verlag für Sozialwissenschaften/Springer Fachmedien Wiesbaden GmbH: Wiesbaden, Germany, 2010. [Google Scholar]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J. Psychiatry 2020, 51, 102119. [Google Scholar] [CrossRef]
- Leite, H.; Lindsay, C.; Kumar, M. COVID-19 outbreak: Implications on healthcare operations. TQM J. 2021, 33, 247–256. [Google Scholar] [CrossRef]
- Holopainen, A.; Verhage, M.L.; Oosterman, M. Childbirth Experience Associated With Maternal and Paternal Stress During the First Year, but Not Child Attachment. Front. Psychiatry 2020, 11, 562394. [Google Scholar] [CrossRef]
- Dashraath, P.; Wong, J.L.J.; Lim, M.X.K.; Lim, L.M.; Li, S.; Biswas, A.; Choolani, M.; Mattar, C.; Su, L.L. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020, 222, 521–531. [Google Scholar] [CrossRef]
- Riley, V.; Ellis, N.; Mackay, L.; Taylor, J. The impact of COVID-19 restrictions on women’s pregnancy and postpartum experience in England: A qualitative exploration. Midwifery 2021, 101, 103061. [Google Scholar] [CrossRef]
- Janevic, T.; Maru, S.; Nowlin, S.; McCarthy, K.; Bergink, V.; Stone, J.; Dias, J.; Wu, S.; Howell, E.A. Pandemic Birthing: Childbirth Satisfaction, Perceived Health Care Bias, and Postpartum Health During the COVID-19 Pandemic. Matern. Child Health J. 2021, 25, 860–869. [Google Scholar] [CrossRef]
- Sadler, M.; Leiva, G.; Olza, I. COVID-19 as a risk factor for obstetric violence. Sex. Reprod. Health Matters 2020, 28, 1785379. [Google Scholar] [CrossRef]
- Chen, E.-M.; Gau, M.-L.; Liu, C.-Y.; Lee, T.-Y. Effects of Father-Neonate Skin-to-Skin Contact on Attachment: A Randomized Controlled Trial. Nurs. Res. Pract. 2017, 2017, 8612024. [Google Scholar] [CrossRef] [Green Version]
- Altman, M.R.; Gavin, A.R.; Eagen-Torkko, M.K.; Kantrowitz-Gordon, I.; Khosa, R.M.; Mohammed, S.A. Where the System Failed: The COVID-19 Pandemic’s Impact on Pregnancy and Birth Care. Glob. Qual. Nurs. Res. 2021, 8, 23333936211006397. [Google Scholar] [CrossRef]
- Mayopoulos, G.A.; Ein-Dor, T.; Li, K.G.; Chan, S.J.; Dekel, S. COVID-19 positivity associated with traumatic stress response to childbirth and no visitors and infant separation in the hospital. Sci. Rep. 2021, 11, 13535. [Google Scholar] [CrossRef]
- Choi, K.R.; Records, K.; Low, L.K.; Alhusen, J.L.; Kenner, C.; Bloch, J.R.; Premji, S.S.; Hannan, J.; Anderson, C.M.; Yeo, S.; et al. Promotion of Maternal–Infant Mental Health and Trauma-Informed Care During the COVID-19 Pandemic. J. Obstet. Gynecol. Neonatal Nurs. 2020, 49, 409–415. [Google Scholar] [CrossRef]
- Semaan, A.; Audet, C.; Huysmans, E.; Afolabi, B.; Assarag, B.; Banke-Thomas, A.; Blencowe, H.; Caluwaerts, S.; Campbell, O.M.R.; Cavallaro, F.L.; et al. Voices from the frontline: Findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob. Health 2020, 5, e002967. [Google Scholar] [CrossRef]
- Del Piccolo, L.; Donisi, V.; Raffaelli, R.; Garzon, S.; Perlini, C.; Rimondini, M.; Uccella, S.; Cromi, A.; Ghezzi, F.; Ginami, M.; et al. The Psychological Impact of COVID-19 on Healthcare Providers in Obstetrics: A Cross-Sectional Survey Study. Front. Psychol. 2021, 12, 949. [Google Scholar] [CrossRef]
- Skjefte, M.; Ngirbabul, M.; Akeju, O.; Escudero, D.; Hernandez-Diaz, S.; Wyszynski, D.F.; Wu, J.W. COVID-19 vaccine acceptance among pregnant women and mothers of young children: Results of a survey in 16 countries. Eur. J. Epidemiol. 2021, 36, 197–211. [Google Scholar] [CrossRef]
- Jamieson, D.J.; Rasmussen, S.A. An update on COVID-19 and pregnancy. Am. J. Obstet. Gynecol. 2021, 226, 177–186. [Google Scholar] [CrossRef]
- Deutsche Gesellschaft für Gynäkologie und Geburtshilfe e. V. DGGG Empfiehlt: Väter Bei Der Geburt Zulassen—Auch in Zeiten Der Corona-Pandemie. Available online: https://www.dggg.de/presse/pressemitteilungen-und-nachrichten/dggg-empfiehlt-vaeter-bei-der-geburt-zulassen-auch-in-zeiten-der-corona-pandemie (accessed on 12 January 2022).
- Zöllkau, J.; Hagenbeck, C.; Hecher, K.; Pecks, U.; Schlembach, D.; Simon, A.; Schlösser, R.; Schleußner, E. Recommendations for SARS-CoV-2/COVID-19 during Pregnancy, Birth and Childbed—Update November 2021 (Long Version). Z. Geburtshilfe Neonatol 2021, 135. [Google Scholar] [CrossRef]
- Rocca-Ihenacho, L.; Alonso, C. Where do women birth during a pandemic? Changing perspectives on Safe Motherhood during the COVID-19 pandemic. J. Glob. Health Sci. 2020, 2, e4. [Google Scholar] [CrossRef] [Green Version]
- Pustulka, P.; Buler, M. Pregnancy and childbirth during the COVID-19 pandemic in Poland: Qualitative evidence from expert interviews—Preprint. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Schmiedhofer, M.; Derksen, C.; Keller, F.M.; Dietl, J.E.; Haussler, F.; Strametz, R.; Koester-Steinebach, I.; Lippke, S. Barriers and Facilitators of Safe Communication in Obstetrics: Results from Qualitative Interviews with Physicians, Midwives and Nurses. Int. J. Environ. Res. Public Health 2021, 18, 915. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Every Woman’s Right to a Companion of Choice during Childbirth. Available online: https://www.who.int/news/item/09-09-2020-every-woman-s-right-to-a-companion-of-choice-during-childbirth (accessed on 12 January 2022).
- World Health Organization. Clinical Management of COVID-19: Interim Guidance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Nespoli, A.; Ornaghi, S.; Borrelli, S.; Vergani, P.; Fumagalli, S. Lived experiences of the partners of COVID-19 positive childbearing women: A qualitative study. Women Birth 2021, in press. [Google Scholar] [CrossRef]
- Denning, M.; Goh, E.T.; Tan, B.; Kanneganti, A.; Almonte, M.; Scott, A.; Kinross, J. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: A multinational cross-sectional study. PLoS ONE 2021, 16, e0238666. [Google Scholar] [CrossRef]
- Chirico, F.; Ferrari, G.; Nucera, G.; Szarpak, L.; Crescenz, P.; InkaIlesanmi, O. Prevalence of anxiety, depression, burnout syndrome, and mental health disorders among healthcare workers during the COVID-19 pandemic: A rapid umbrella review of systematic reviews. J. Health Soc. Sci. 2021, 6, 209–220. [Google Scholar]
| Characteristics | Distribution in the Sample of Mothers |
|---|---|
| Age at birth | 22–46 years, Median 34 years, mean 33 years (SD = 5) |
| Migration Status | 5 (20%) of which: 3 (12%) < 10 years immigrated themselves 2 (8%) second generation |
| Parity | 19 (76%) first-time mothers 6 (24%) second and multiple births |
| Birth mode | 18 (72) vaginal 7 (28%) caesarean section |
| Twin birth | 1 (4%) |
| Child with disability | 1 (4%) |
| COVID-19 tested positive | 2 (8%) |
| Interview duration | 19–95 min Median 35, mean 38 min; (SD = 15) |
| Interview format | 22 (88%) via TEAMS with camera on 3 (12%) by telephone/TEAMS camera off |
| Interview period | February to July 2021 |
| Period of birth | July 2020 to May 2021 |
| Characteristics | Distribution in the Sample of HCW |
|---|---|
| Occupational Age | 2–30 years Median 6 years, mean 12 years (SD = 7) |
| Gender | Female, n = 9, male n = 1 |
| Profession | Midwives n = 4 Doctors n = 2 Nurses n = 2 Assistant n = 1 |
| Professional level | Superior n = 3 |
| Interview duration | 17–75 min Median 32, mean 35 min (SD = 16) |
| Interview format | 9 (90%) in person in the clinic 1 (10%) via TEAMS camera on |
| Interview period | July to August 2021 |
| Do You Remember Getting Your First Information About births in Your Life, and If Yes from Whom? Do You Recall Emotional Association to Birth Experience—What Describes the Feeling You Associate with Your Birth the Best? |
|---|
| How were you affected from COVID-19 during your pregnancy? |
| Current birth experience: How and with whom did you prepare for your birth? |
| Could you please describe your birthing experience as precisely a possible from the moment you decided you have to go to the hospital? Who did you get support from? How did you stay in touch with your partner? If a partner participated: How did you feel after you left your partner at the hospital door? When was the partner allowed in? If a partner participated: When were you allowed in? How did you spend the meantime? |
| How was the communication affected by the COVID containment measures? |
| If you stayed at the maternity ward, what was the care there like? |
| Overall, what was good? What did you miss? |
| What could have been better? Who should have done something differently? |
| How Long Have You Been Working in Obstetrics? |
|---|
| What major challenges have you had to overcome so far? |
| Do you remember the first time you became aware that a pandemic was emerging? |
| What organizational changes were implemented at your facility? What level made the decisions? (Hospital leadership, birth center leadership, group autonomously?) Did you have sufficient protective materials? How were the structural adjustments communicated? |
| How did you perceive the reaction of the women? Resistance, reactions, acceptance, questions? Were there changes over time? What feelings did you perceive among the women? Fear, insecurity, feelings of being left alone or socially isolated? |
| (How) have you tried to compensate for the absence of partners? (Staying in the delivery room, more caring, reassurance). What was your experience with limited partner access? |
| How did you perceive the impact in the maternity ward? (No support from partner/‘room arrest’ partner, no other visitors) |
| Are there any changes that you would like to see to be continued after the pandemic? |
| Target Group | During the First Phase of Labor (Period Before Admission to the Delivery Room) | In the Delivery Room | In the Maternity Ward |
|---|---|---|---|
| (Becoming) mothers |
|
|
|
|
|
| |
|
|
| |
|
|
| |
|
|
| |
| HCW (obstetricians, midwives, and nurses) |
|
|
|
|
|
| |
|
|
| |
|
| ||
| Partners |
|
|
|
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmiedhofer, M.; Derksen, C.; Dietl, J.E.; Häussler, F.; Louwen, F.; Hüner, B.; Reister, F.; Strametz, R.; Lippke, S. Birthing under the Condition of the COVID-19 Pandemic in Germany: Interviews with Mothers, Partners, and Obstetric Health Care Workers. Int. J. Environ. Res. Public Health 2022, 19, 1486. https://doi.org/10.3390/ijerph19031486
Schmiedhofer M, Derksen C, Dietl JE, Häussler F, Louwen F, Hüner B, Reister F, Strametz R, Lippke S. Birthing under the Condition of the COVID-19 Pandemic in Germany: Interviews with Mothers, Partners, and Obstetric Health Care Workers. International Journal of Environmental Research and Public Health. 2022; 19(3):1486. https://doi.org/10.3390/ijerph19031486
Chicago/Turabian StyleSchmiedhofer, Martina, Christina Derksen, Johanna Elisa Dietl, Freya Häussler, Frank Louwen, Beate Hüner, Frank Reister, Reinhard Strametz, and Sonia Lippke. 2022. "Birthing under the Condition of the COVID-19 Pandemic in Germany: Interviews with Mothers, Partners, and Obstetric Health Care Workers" International Journal of Environmental Research and Public Health 19, no. 3: 1486. https://doi.org/10.3390/ijerph19031486
APA StyleSchmiedhofer, M., Derksen, C., Dietl, J. E., Häussler, F., Louwen, F., Hüner, B., Reister, F., Strametz, R., & Lippke, S. (2022). Birthing under the Condition of the COVID-19 Pandemic in Germany: Interviews with Mothers, Partners, and Obstetric Health Care Workers. International Journal of Environmental Research and Public Health, 19(3), 1486. https://doi.org/10.3390/ijerph19031486







