Child-, Family-, and Community-Level Facilitators for Promoting Oral Health Practices among Indigenous Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Approval
2.3. Participants and Sampling
2.4. Data Analysis
2.5. Fisher-Owens’ Conceptual Model
2.6. Consideration of Socioeconomic Positions
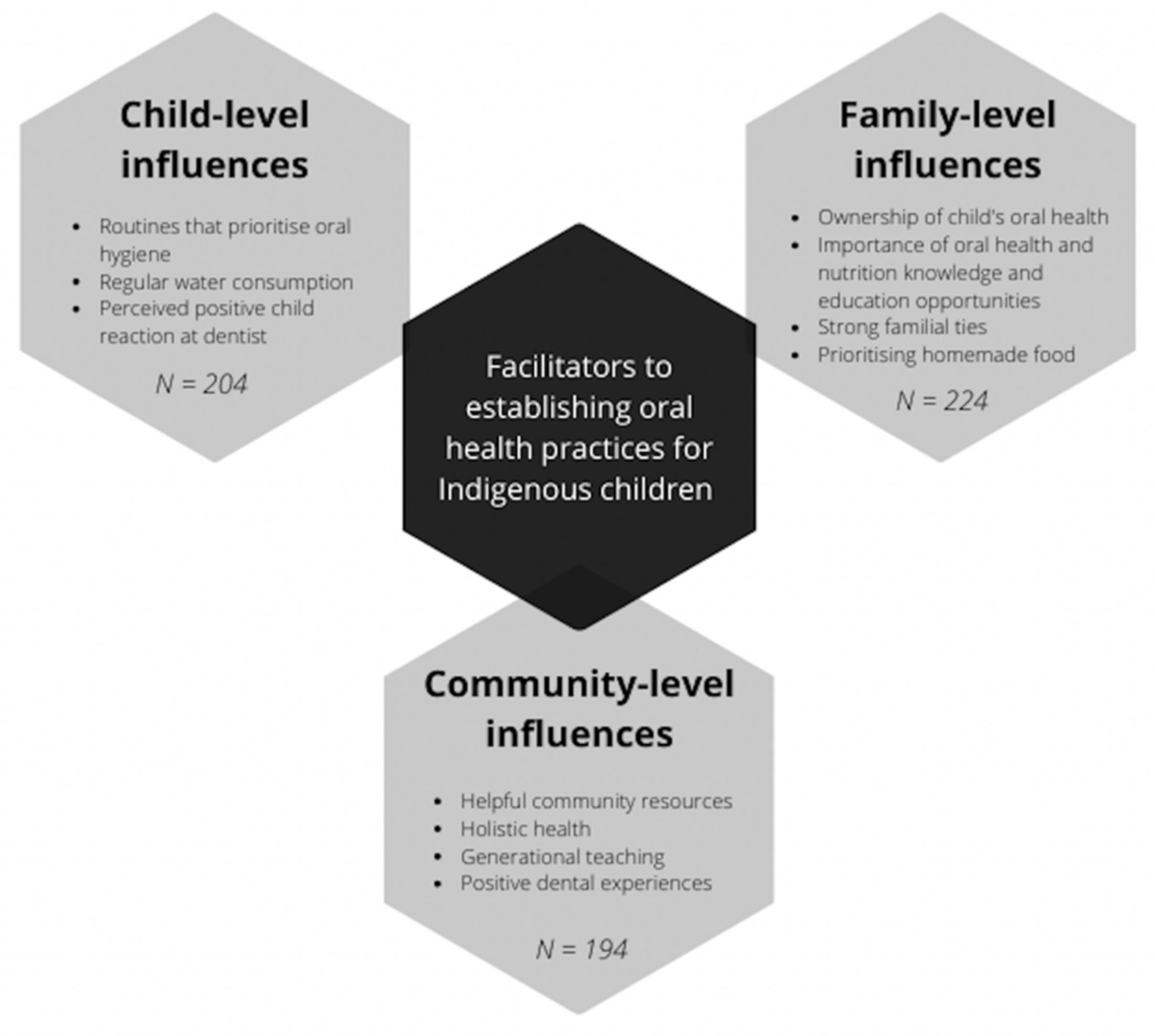
3. Results
3.1. Family-Level Influences
3.1.1. Ownership of Child’s Oral Health
“I probably will give less juice and yes, wow, yes, maybe try and rethink some choices like, because … when you go out to places and you get kids meal deals and various things, you get the juice, like you pick that one, but I’ll pick differently in future”.(P161; High SEP mother)
“Well like I said, I’ve got [dental caries] in my mouth, so I don’t want my kids to have them, because they’re horrible. I’ve got yucky teeth, and that’s from growing up where I didn’t brush my teeth because nobody told me I had to brush my teeth. I just don’t want that [for them] because my teeth are all falling out and it’s horrible”.(P124; High SEP mother)
3.1.2. Oral Health and Nutrition Knowledge and Education Opportunities
“Like I said to my doctor … it’s being educated. When you have that education and understanding, you can change things in your life. Where beforehand I didn’t have that understanding of what foods are good and some foods that you’d always considered good, turn into sugars and you eat them and all that, so education [is the most important] I think”.(P20; Low SEP mother)
“Yes, because you told me about that, so that’s just made me aware of, you know, letting him sleep with a bottle, because the milk just lays on their teeth, and see I never knew that… because the first boy, he was on the titty all the time, and then when he come off, he was just on water, see, so, he had no problems with his teeth, but [this child] just wanted bottle all the time”.(P33; Low SEP mother)
“Just sad, you know, kids going to have to go under a local anaesthetic to get their teeth out…the parents should, you know, should know better, not to… Like I said, they need tough love, you know, not to give in straight away. A lot of kids do cry to get their way, but that’s where I just, no, I’m not going to give in to you, you can cry, chuck a tantrum all you want”.(P64; Low SEP mother)
3.1.3. Strong Familial Ties
“Family have helped in getting us to where we are now. So it’s like looking after babies and everything like that. It is like a necessity basically that we teach our children and in that way they can teach their children and so on, and so on and so on. So it does play a big role in healthy teeth”.(P18; High SEP mother)
“Well even with me, I’ve gone on a diet myself, so I’ve cut out the cool drinks and the juice… so I’ve been more on the water myself. So maybe the kids are seeing that too, because all I’m doing is drinking water, so they’ll end up grabbing my water bottle and, you know, if it’s got a pull top then they’re drinking that. So that’s good”.(P110; High SEP mother)
3.1.4. Prioritising Homemade Foods
“I don’t give into lollies, I don’t give into that. They do have their odd ice-cream every now and then, but not every time…Yes, so it’s not always about lollies or soft drinks, or things like that. I give them treats in other ways, like buying them a toy, or you know going to the street, go to the beach, going to the playground, and things like that”.(P64; Low SEP mother)
3.2. Child-Level Influences
3.2.1. Routines That Prioritise Oral Hygiene
“I think it’s just the toothbrush I bought for him, it’s a little Batman light up one, it’s lights up for [the time] that you have to brush for and as soon as it stops you stop brushing, yes, so I think that’s what it is, the toothbrush, he likes it”.(P70; Low SEP mother)
3.2.2. Regular Water Consumption
“He’s been looking for the water … we’ve got one of those water fountains, you know, that you can go on press and it’ll come out. We’ve been finding water on the floor, because he’s going and standing underneath it and drinking it. His dad growled him, and I said don’t growl at him, you encourage him, he’s drinking water, you know, that’s the best thing for him”.(P10; High SEP mother)
3.2.3. Perceived Positive Child Reaction at The Dentist
“Well he just loves being the centre of attention. I guess being the second child he always… The first ones always try to get all the attention and I think him being up in that chair with the dentist and everyone focused on him, I think he will like it”.(P57; High SEP mother)
3.3. Community-Level Influences
3.3.1. Helpful Community Resources
“If you want your dental work … [the support person] can go with you and pick you up and take you to a dental clinic… You know, for the fella’s that have got really bad teeth … I suppose she explains to the dentist beforehand that, you know, like be prepared more or less, like don’t say this is this… You know, don’t let these fella’s walk in and be like oh my God you didn’t brush your teeth, because obviously they haven’t… She prepares them so you don’t feel bad about not looking after your teeth”.(P19; Low SEP mother)
“[The school] keep[s] carrying on about the packaged foods and things so that’s helped us with our snacks and things like that I’ll get other things… because [some snacks have] higher sugars and higher salts… And even though they might be labelled school snacks not necessarily healthy so being quite conscious since we’ve come to this school it’s helped to you know, open our eyes up a bit more. As in the packaging’s and yes, so we tend to read and they’ll be like but it’s in the school snack aisle. I’m like yes but look what it says here in the little bar of how high the sugar actually is in this and the school’s going to go you can’t eat that”.(P40; Low SEP mother)
3.3.2. Holistic Health
“I go [to the Aboriginal health workers] a lot. Like, even if it’s got nothing to do with health, when I need, just, to chat about something, I will go there… So they’re good not just for health but for everything, whereas, when you go to the doctors it’s not really the same”.(P26; Low SEP mother)
3.3.3. Generational Teaching
“It was good that my mum and dad were so concerned with our oral health, you know, that’s why I’m so with my kids…Yes, well, I want our line to stay strong. Do you know what I mean? For generations my family was always wiped out, and then it was only in my mum’s generation that we’ve just sort of started to come back together”.(P2; High SEP mother)
“[The kids] understand that, you know, you’ve got to look after their teeth otherwise… Because my Dads got all falsies and I try and explain to them, oh you’ll have no teeth when you’re old. You’ll look like your Poppa”.(P63; Low SEP mother)
3.3.4. Positive Dental Experiences
“I know, you know, [the dentist] can detect things that I can’t see and catching anything, you know, at an early stage would be good. And it gets her used to it too, you know, she won’t be scared of the dentist when she goes in kinder or school or whatever. She’ll know that going to the dentist is a good thing not a scary thing like other kids”.(P131; Low SEP mother)
4. Discussion
4.1. Family-Level Influences
4.2. Child-Level Influences
4.3. Community-Level Influences
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Jamieson, L.M.; Paradies, Y.C.; Gunthorpe, W.; Cairney, S.J.; Sayers, S.M. Oral health and social and emotional well-being in a birth cohort of Aboriginal Australian young adults. BMC Public Health 2011, 11, 656. [Google Scholar] [CrossRef] [Green Version]
- Baghdadi, Z.D. Effects of Dental Rehabilitation under General Anesthesia on Children’s Oral Health-Related Quality of Life Using Proxy Short Versions of OHRQoL Instruments. Sci. World J. 2013, 2014, 308435–308439. [Google Scholar] [CrossRef]
- Alkarimi, H.A.; Watt, R.G.; Pikhart, H.; Sheiham, A.; Tsakos, G. Dental caries and growth in school-age children. Pediatrics (Evanston) 2014, 133, e616–e623. [Google Scholar] [CrossRef] [Green Version]
- De Silva, A.M.; Martin-Kerry, J.; Geale, A.; Cole, D. Flying blind: Trying to find solutions to Indigenous oral health. Aust. Health Rev. 2016, 40, 570–583. [Google Scholar] [CrossRef]
- Schroth, R.J.D.M.D.M.; Harrison, R.L.D.M.D.M.M.; Moffatt, M.K.M.D.M.F. Oral Health of Indigenous Children and the Influence of Early Childhood Caries on Childhood Health and Well-being. Pediat. Clin. N. 2009, 56, 1481–1499. [Google Scholar] [CrossRef]
- Kramer, P.F.; Feldens, C.A.; Helena Ferreira, S.; Bervian, J.; Rodrigues, P.H.; Peres, M.A. Exploring the impact of oral diseases and disorders on quality of life of preschool children. Community Dent. 2013, 41, 327–335. [Google Scholar] [CrossRef]
- Watt, R.G.; Mathur, M.R.; Aida, J.; Bönecker, M.; Venturelli, R.; Gansky, S.A. Oral Health Disparities in Children: A Canary in the Coalmine? Pediat. Clin. N. 2018, 65, 965–979. [Google Scholar] [CrossRef] [PubMed]
- Bagramian, R.A.; Garcia-Godoy, F.; Volpe, A.R. The global increase in dental caries. A pending public health crisis. Am. J. Dent. 2009, 22, 3–8. [Google Scholar] [PubMed]
- Petersen, P.E. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century—the approach of the WHO Global Oral Health Programme. Community Dent. 2003, 31, 3–24. [Google Scholar] [CrossRef] [PubMed]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.-J.; Bramlett, M.D.; Newacheck, P.W. Influences on Children’s Oral Health: A Conceptual Model. Pediatrics 2007, 120, e510–e520. [Google Scholar] [CrossRef] [Green Version]
- Jamieson, L.; Haag, D.; Schuch, H.; Kapellas, K.; Arantes, R.; Thomson, W.M. Indigenous Oral Health Inequalities at an International Level: A Commentary. Int. J. Environ. Res. Public Health 2020, 17, 3958. [Google Scholar] [CrossRef] [PubMed]
- King, M.P.; Smith, A.M.D.; Gracey, M.P. Indigenous health part 2: The underlying causes of the health gap. Lancet 2009, 374, 76–85. [Google Scholar] [CrossRef]
- Czyzewski, K. Colonialism as a Broader Social Determinant of Health. Int. Indig. Policy J. 2011, 2, 5. [Google Scholar] [CrossRef]
- Dudgeon, W.; Wright, M.; Paradies, Y.; Garvey, D.; Walker, I. The Social, Cultural and Historical Context of Aboriginal and Torres Strait Islander Australians. In Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice; Purdie, N., Dudgeon, P., Walker, R., Eds.; Australian Government Department of Health and Ageing: Barton, Australia, 2010; pp. 25–42. [Google Scholar]
- Dudgeon, P.W.M.; Paradies, Y.; Garvey, D.; Walker, I. The Social, Cultural and Historical Context of Aboriginal and Torres Strait Islander Australians; Australian Institue of Health and Welfare: Canberra, Australia, 2010; pp. 25–42. [Google Scholar]
- Gracey, M. Historical, cultural, political, and social influences on dietary patterns and nutrition in Australian Aboriginal children. Am. J. Clin. Nutr. 2000, 72, 1361S–1367S. [Google Scholar] [CrossRef] [Green Version]
- Menzies, K. Understanding the Australian Aboriginal experience of collective, historical and intergenerational trauma. Int. Soc. Work 2019, 62, 1522–1534. [Google Scholar] [CrossRef]
- Durey, A.; McAullay, D.; Gibson, B.; Slack-Smith, L. Aboriginal Health Worker perceptions of oral health: A qualitative study in Perth, Western Australia. Int. J. Equity Health 2016, 15, 4. [Google Scholar] [CrossRef] [Green Version]
- Paradies, Y. Colonisation, racism and indigenous health. J. Popul. Res. 2016, 33, 83–96. [Google Scholar] [CrossRef]
- Butten, K.; Johnson, N.W.; Hall, K.K.; Toombs, M.; King, N.; O’Grady, K.-A.F. Yarning about oral health: Perceptions of urban Australian Aboriginal and Torres Strait Islander women. BMC Oral. Health 2020, 20, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crocombe, L.A.; Broadbent, J.M.; Thomson, W.M.; Brennan, D.S.; Poulton, R. Impact of dental visiting trajectory patterns on clinical oral health and oral health-related quality of life. J. Public Health Dent. 2012, 72, 36–44. [Google Scholar] [CrossRef]
- Jamieson, L.M.; Parker, E.J.; Armfield, J.M. Indigenous child oral health at a regional and state level. J. Paediatr. Child Heal. 2007, 43, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, L.M.; Roberts-Thomson, K.F. Oral Health of Aboriginal and Torres Strait Islander Children; Australian Institute of Health and Welfare: Canberra, Australia, 2007. [Google Scholar]
- Jamieson, L.M.; Roberts-Thomson, K.F. Dental general anaesthetic trends among Australian children. BMC Oral. Health 2006, 6, 16. [Google Scholar] [CrossRef] [Green Version]
- Kay, E.J.; Locker, D. Is dental health education effective? A systematic review of current evidence. Community Dent. 1996, 24, 231–235. [Google Scholar] [CrossRef]
- Council of Australian Government Health Council. Healthy Mouths, Healthy Lives; Australia’s National Oral Health Plan 2015–2024; COAG Health Council: Canberra, Australia, 2015.
- Australian Institute of Health and Welfare. The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples 2015; AIHW: Canberra, Australia, 2015.
- Government of South Australia. 2018 Consultation Paper: South Australia’s Oral Health Plan; Government of South Australia: Adelaide, Australia, 2018.
- Biddle, N.; Swee, H. The Relationship between Wellbeing and Indigenous Land, Language and Culture in Australia. Aust. Geogr. 2012, 43, 215–232. [Google Scholar] [CrossRef]
- Abbott, P.; Gordon, E.; Davison, J. Expanding roles of Aboriginal health workers in the primary care setting: Seeking recognition. Contemp. Nurse 2008, 27, 157–164. [Google Scholar] [CrossRef]
- Chi, D.L. Reducing Alaska Native paediatric oral health disparities: A systematic review of oral health interventions and a case study on multilevel strategies to reduce sugar-sweetened beverage intake. Int. J. Circumpolar. Health 2013, 72, 21066. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ha, D.H.; Do, L.G.; Roberts-Thomson, K.; Jamieson, L. Risk indicators for untreated dental decay among Indigenous Australian children. Community Dent. 2019, 47, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Bruerd, B.; Jones, C. Preventing baby bottle tooth decay: Eight-year results. Public Health Rep. 1996, 111, 63–65. [Google Scholar]
- Newton, J.T.; Bower, E.J. The social determinants of oral health: New approaches to conceptualizing and researching complex causal networks. Community Dent. 2005, 33, 25–34. [Google Scholar] [CrossRef]
- Patel, J.; Hearn, L.; Gibson, B.; Slack-Smith, L.M. International approaches to Indigenous dental care: What can we learn? Aust. Dent. J. 2014, 59, 439–445. [Google Scholar] [CrossRef]
- Ashcroft, R. Health inequities: Evaluation of two paradigms. Health Soc. Work 2010, 35, 249–256. [Google Scholar] [CrossRef]
- Hoeft, K.S.; Masterson, E.E.; Barker, J.C. Mexican American Mothers’ Initiation and Understanding of Home Oral Hygiene for Young Children. Pediatr. Dent. 2009, 31, 395–404. [Google Scholar]
- Elison, S.; Norgate, S.; Dugdill, L.; Pine, C. Maternally perceived barriers to and facilitators of establishing and maintaining tooth-brushing routines with infants and preschoolers. Int. J. Environ. Res. Public Health 2014, 11, 6808–6826. [Google Scholar] [CrossRef] [Green Version]
- Amin, M.S.; Harrison, R.L. Understanding parents’ oral health behaviors for their young children. Qual. Health Res. 2009, 19, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Isong, I.A.; Luff, D.; Perrin, J.M.; Winickoff, J.P.; Ng, M.W. Parental Perspectives of Early Childhood Caries. Clin. Pedatr. 2012, 51, 77–85. [Google Scholar] [CrossRef]
- Chandler, M.J.; Lalonde, C. Cultural Continuity as a Hedge against Suicide in Canada’s First Nations. Transcult Psychiatry 1998, 35, 191–219. [Google Scholar] [CrossRef]
- Cox, A.; Dudgeon, P.; Holland, C.; Kelly, K.; Scrine, C.; Walker, R. Using participatory action research to prevent suicide in Aboriginal and Torres Strait Islander communities. Aust. J. Prim. Health 2014, 20, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.; Carlisle, K.; Farmer, J.; Larkins, S.; Dickson-Swift, V.; Kenny, A. Implementation of oral health initiatives by Australian rural communities: Factors for success. Health Soc. Care Community 2018, 26, e102–e110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kilcullen, M.; Swinbourne, A.; Cadet-James, Y. Aboriginal and Torres Strait Islander health and wellbeing: Social emotional wellbeing and strengths-based psychology. Clin. Psych. 2018, 22, 16–26. [Google Scholar] [CrossRef] [Green Version]
- Fogarty, W.; Bulloch, H.; McDonnell, S.; Davis, M. Deficit Discourse and Indigenous Health: How Narrative Framings of Aboriginal and Torres Strait Islander People are Reproduced in Policy; The Lowitja Institute: Melbourne, Australia, 2018. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulz, K.F.; Altman, D.G.; Moher, D.; the CONSORT Group. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010, 8, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Merrick, J.; Chong, A.; Parker, E.; Roberts-Thomson, K.; Misan, G.; Spencer, J.; Broughton, J.; Lawrence, H.; Jamieson, L. Reducing disease burden and health inequalities arising from chronic disease among Indigenous children: An early childhood caries intervention. BMC Public Health 2012, 12, 323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jamieson, L.; Smithers, L.; Hedges, J.; Parker, E.; Mills, H.; Kapellas, K.; Lawrence, H.P.; Broughton, J.R.; Ju, X. Dental Disease Outcomes Following a 2-Year Oral Health Promotion Program for Australian Aboriginal Children and Their Families: A 2-Arm Parallel, Single-blind, Randomised Controlled Trial. E Clin. Med. 2018, 1, 43–50. [Google Scholar] [CrossRef] [Green Version]
- Jamieson, L.M.; Hedges, J.; Ju, X.; Kapellas, K.; Leane, C.; Haag, D.G.; Santiago, P.R.; Macedo, D.M.; Roberts, R.M.; Smithers, L.G. Cohort profile: South Australian Aboriginal Birth Cohort (SAABC)—A prospective longitudinal birth cohort. BMJ Open 2021, 11, e043559. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Ten Things that Motivational Interviewing Is Not. Behav. Cogn. Psychother. 2009, 37, 129–140. [Google Scholar] [CrossRef]
- Walker, M.; Fredericks, B.; Mills, K.; Anderson, D. ”Yarning” as a Method for Community-Based Health Research With Indigenous Women: The Indigenous Women’s Wellness Research Program. Health Care Women Int. 2014, 35, 1216–1226. [Google Scholar] [CrossRef] [Green Version]
- Kovach, M. Conversation Method in Indigenous Research. First Peoples Child Fam. Rev. 2010, 5, 40–48. [Google Scholar] [CrossRef]
- Smith, L.T. Decolonizing Methodologies: Research and Indigenous Peoples; Zed Books: London, UK, 1999. [Google Scholar]
- Harrison, R.; Benton, T.; Everson-Stewart, S.; Weinstein, P. Effect of Motivational Interviewing on Rates of Early Childhood Caries: A Randomized Trial. Pediatr. Dent. 2007, 29, 16–22. [Google Scholar]
- Weinstein, P.; Harrison, R.; Benton, T. Motivating parents to prevent caries in their young children: One-year findings. JADA 2004, 135, 731–738. [Google Scholar] [PubMed] [Green Version]
- Gaume, J.M.A.; Gmel, G.P.D.; Faouzi, M.P.D.; Daeppen, J.-B.M.D. Counselor skill influences outcomes of brief motivational interventions. J. Subst. Abuse Treat. 2009, 37, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Santacroce, S.J.; Maccarelli, L.M.; Grey, M. Intervention Fidelity. Nurs. Res. (N. Y.) 2004, 53, 63–66. [Google Scholar] [CrossRef]
- Jamieson, L.; Bradshaw, J.; Lawrence, H.; Broughton, J.; Venner, K. Fidelity of Motivational Interviewing in an Early Childhood Caries Intervention Involving Indigenous Australian Mothers. J. Health Care Poor Underserved 2016, 27, 125–138. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual. Res. Psychol. 2020, 18, 328–352. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Successful Qualitative Research: A Practical Guide for Beginners; SAGE Publications Ltd.: London, UK, 2013. [Google Scholar]
- Braun, V.; Clarke, V. Reflecting on reflexive thematic analysis. Qual. Res. Sport Exerc. 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Watt, R.G. From victim blaming to upstream action: Tackling the social determinants of oral health inequalities. Community Dent. 2007, 35, 1–11. [Google Scholar] [CrossRef]
- Ben, J.J.L.; Parker, E.J.; Roberts-Thomson, K.F.; Lawrence, H.P.; Broughton, J.; Paradies, Y. Experience of racism and tooth brushing among pregnant Aboriginal Australians: Exploring psychosocial mediators. Community Dent. Health 2014, 31, 145–152. [Google Scholar] [PubMed]
- Steffens, M.; Jamieson, L.; Kapellas, K. Historical Factors, Discrimination and Oral Health among Aboriginal Australians. J. Health Care Poor Underserved 2016, 27, 30–45. [Google Scholar] [CrossRef]
- Jamieson, L.M.; Do, L.G.; Bailie, R.S.; Sayers, S.M.; Turrell, G. Associations between area-level disadvantage and DMFT among a birth cohort of Indigenous Australians. Aust. Dent. J. 2013, 58, 75–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Australian Institue of Health and Welfare. Aboriginal and Torres Strait Islander Health Performance Framework 2017 Report; Australian Institute of Health and Welfare: Canberra, Australia, 2017.
- Krieger, N.; Williams, D.R.; Moss, N.E. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annu. Rev. Public Health 1997, 18, 341–378. [Google Scholar] [CrossRef] [Green Version]
- Phelan, J.C.; Link, B.G.; Tehranifar, P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. J. Health Soc. Behav. 2010, 51, S28–S40. [Google Scholar] [CrossRef] [Green Version]
- Schwarz, E. Access to oral health care—an Australian perspective. Community Dent. 2006, 34, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Pink, B. Socio-Economic Indexes for Areas (SEIFA); Australian Bureau of Statistics: Canberra, Australia, 2011. [Google Scholar]
- Turrell, G.; Kavanagh, A.M. Socio-economic pathways to diet: Modelling the association between socio-economic position and food purchasing behaviour. Public Health Nutr. 2006, 9, 375–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roberts-Thomson, K.F.; Slade, G.D.; Bailie, R.S.; Endean, C.; Simmons, B.; Leach, A.J.; Raye, I.; Morris, P.S. A comprehensive approach to health promotion for the reduction of dental caries in remote Indigenous Australian children: A clustered randomised controlled trial. Int. Dent. J. 2010, 60, 245–249. [Google Scholar] [PubMed]
- Lawrence, H.P. Oral health interventions among Indigenous populations in Canada. Int. Dent. J. 2010, 60, 229–234. [Google Scholar] [PubMed]
- Duijster, D.; de Jong-Lenters, M.; Verrips, E.; van Loveren, C. Establishing oral health promoting behaviours in children: Parents’ views on barriers, facilitators and professional support: A qualitative study. BMC Oral. Health 2015, 15, 157. [Google Scholar] [CrossRef] [Green Version]
- Fulkerson, J.A.; Rydell, S.; Kubik, M.Y.; Lytle, L.; Boutelle, K.; Story, M.; Neumark-Sztainer, D.; Dudovitz, B.; Garwick, A. Healthy Home Offerings via the Mealtime Environment (HOME): Feasibility, Acceptability, and Outcomes of a Pilot Study. Obesity (Silver Spring Md.) 2010, 18, S69–S74. [Google Scholar] [CrossRef] [Green Version]
- Lewis, M.; Lee, A. Costing ‘healthy’ food baskets in Australia—A systematic review of food price and affordability monitoring tools, protocols and methods. Public Health Nutr. 2016, 19, 2872–2886. [Google Scholar] [CrossRef]
- Lee, A.; Lewis, M. Testing the Price of Healthy and Current Diets in Remote Aboriginal Communities to Improve Food Security: Development of the Aboriginal and Torres Strait Islander Healthy Diets ASAP (Australian Standardised Affordability and Pricing) Methods. Int. J. Environ. Res. Public Health 2018, 15, 2912. [Google Scholar] [CrossRef] [Green Version]
- Marshman, Z.; Ahern, S.M.; McEachan, R.R.C.; Rogers, H.J.; Gray-Burrows, K.A.; Day, P.F. Parents’ Experiences of Toothbrushing with Children: A Qualitative Study. JDR Clin. Trans. Res. 2016, 1, 122–130. [Google Scholar] [CrossRef] [Green Version]
- Durey, A.; McAullay, D.; Gibson, B.; Slack-Smith, L.M. Oral Health in Young Australian Aboriginal Children: Qualitative Research on Parents’ Perspectives. JDR Clin. Trans. Res. 2017, 2, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Butten, K.; Johnson, N.W.; Hall, K.K.; Toombs, M.; King, N.; O’Grady, K.-A.F. Impact of oral health on Australian urban Aboriginal and Torres Strait Islander families: A qualitative study. Int. J. Equity Health 2019, 18, 34. [Google Scholar] [CrossRef]
- Levin, A.; Sokal-Gutierrez, K.; Hargrave, A.; Funsch, E.; Hoeft, K.S. Maintaining Traditions: A Qualitative Study of Early Childhood Caries Risk and Protective Factors in an Indigenous Community. Int. J. Environ. Res. Public Health 2017, 14, 907. [Google Scholar] [CrossRef] [Green Version]
- Australian Government Department of Health. Poisons Standard; Australian Government Department of Health: Canberra, Australia, 2017; p. 667.
- Skinner, J.; Dimitropoulos, Y.; Rambaldini, B.; Calma, T.; Raymond, K.; Ummer-Christian, R.; Orr, N.; Gwynne, K. Costing the Scale-Up of a National Primary School-Based Fluoride Varnish Program for Aboriginal Children Using Dental Assistants in Australia. Int. J. Environ. Res. Public Health 2020, 17, 8774. [Google Scholar] [CrossRef] [PubMed]
- Nolan-Isles, D.; Macniven, R.; Hunter, K.; Gwynn, J.; Lincoln, M.; Moir, R.; Dimitropoulos, Y.; Taylor, D.; Agius, T.; Finlayson, H.; et al. Enablers and Barriers to Accessing Healthcare Services for Aboriginal People in New South Wales, Australia. Int. J. Environ. Res. Public Health 2021, 18, 3014. [Google Scholar] [CrossRef]
- Campbell, M.A.; Hunt, J.; Scrimgeour, D.J.; Davey, M.; Jones, V. Contribution of Aboriginal Community-Controlled Health Services to improving Aboriginal health: An evidence review. Aust. Health Rev. 2018, 42, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Jan, S.; Conaty, S.; Hecker, R.; Bartlett, M.; Delaney, S.; Capon, T. An holistic economic evaluation of an Aboriginal community-controlled midwifery programme in Western Sydney. J. Health Serv. Res. Policy 2004, 9, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Dimer, L.; Dowling, T.; Jones, J.; Cheetham, C.; Thomas, T.; Smith, J.; McManus, A.; Maiorana, A.J. Build it and they will come: Outcomes from a successful cardiac rehabilitation program at an Aboriginal Medical Service. Aust. Health Rev. 2013, 37, 79–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Socha, A. Addressing Institutional Racism Against Aboriginal and Torres Strait Islanders of Australia in Mainstream Health Services: Insights From Aboriginal Community Controlled Health Services. Int. J. Indig. Health 2020, 16, 291–303. [Google Scholar] [CrossRef]
- Tynan, A.; Walker, D.; Tucker, T.; Fisher, B.; Fisher, T. Factors influencing the perceived importance of oral health within a rural Aboriginal and Torres Strait Islander community in Australia. BMC Public Health 2020, 20, 514. [Google Scholar] [CrossRef]
- Senturia, K.; Fiset, L.; Hort, K.; Huebner, C.; Mallott, E.; Milgrom, P.; Nelson, L.; Parrish, C.; Cunha-Cruz, J. Dental health aides in Alaska: A qualitative assessment to improve paediatric oral health in remote rural villages. Community Dent. 2018, 46, 416–424. [Google Scholar] [CrossRef]
- Martin, D.; McNally, M.; Castleden, H.; Worden-Driscoll, I.; Clarke, M.; Wall, D.; Ley, M. Linking Inuit Knowledge and Public Health for Improved Child and Youth Oral Health in NunatuKavut. JDR Clin. Trans. Res. 2018, 3, 256–263. [Google Scholar] [CrossRef]
- Smith, L.; Blinkhorn, A.; Moir, R.; Brown, N.; Blinkhorn, F. Evaluation of an oral health education program for young aboriginal children: Feedback from parents, aboriginal health workers and managerial staff. Int. J. Health Promot. Educ. 2020, 58, 92–103. [Google Scholar] [CrossRef]
- Kong, A.C.; Sousa, M.S.; Ramjan, L.; Dickson, M.; Goulding, J.; Gwynne, K.; Talbot, F.; Jones, N.; Srinivas, R.; George, A. ”Got to build that trust”: The perspectives and experiences of Aboriginal health staff on maternal oral health. Int. J. Equity Health 2020, 19, 187. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.L.; Jack, S.M.; Ballantyne, M.; Gabel, C.; Bomberry, R.; Wahoush, O. Indigenous mothers’ experiences of using acute care health services for their infants. J. Clin. Nurs. 2019, 28, 3935–3948. [Google Scholar] [CrossRef]
- Kong, A.C.; Ramjan, L.; Sousa, M.S.; Gwynne, K.; Goulding, J.; Jones, N.; Srinivas, R.; Rambaldini, B.; Moir, R.; George, A. The oral health of Indigenous pregnant women: A mixed-methods systematic review. Women Birth J. Aust. Coll. Midwives 2020, 33, 311–322. [Google Scholar] [CrossRef]
- Jones, K.; Keeler, N.; Morris, C.; Brennan, D.; Roberts-Thompson, K.; Jamieson, L. Factors Relating to Access to Dental Care for Indigenous South Australians. J. Health Care Poor Underserved 2016, 27, 148–160. [Google Scholar] [CrossRef]
- Tsai, C.; Blinkhorn, A.; Irving, M. Oral Health Programmes in Indigenous Communities Worldwide—Lessons learned from the field: A qualitative systematic review. Community Dent. 2017, 45, 389–397. [Google Scholar] [CrossRef]
- Hayman, N.E.; White, N.E.; Spurling, G.K. Improving Indigenous patients’ access to mainstream health services: The Inala experience. Med. J. Aust. 2009, 190, 604–606. [Google Scholar] [CrossRef]
- Forsyth, C.; Irving, M.; Short, S.; Tennant, M.; Gilroy, J. Strengthening Indigenous cultural competence in dentistry and oral health education: Academic perspectives. Eur. J. Dent. Educ. 2019, 23, e37–e44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Neill, L.; O’Neill, L.; Fraser, T.; Fraser, T.; Kitchenham, A.; Kitchenham, A.; McDonald, V.; McDonald, V. Hidden Burdens: A Review of Intergenerational, Historical and Complex Trauma, Implications for Indigenous Families. J. Child Adolesc. Trauma 2018, 11, 173–186. [Google Scholar] [CrossRef] [PubMed]
- Viscogliosi, C.; Asselin, H.; Basile, S.; Borwick, K.; Couturier, Y.; Drolet, M.-J.; Gagnon, D.; Obradovic, N.; Torrie, J.; Zhou, D.; et al. Importance of Indigenous elders’ contributions to individual and community wellness: Results from a scoping review on social participation and intergenerational solidarity. Can. J. Public Health 2020, 111, 667–681. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kant, S.; Vertinsky, I.; Zheng, B.; Smith, P.M. Multi-Domain Subjective Wellbeing of Two Canadian First Nations Communities. World Dev. 2014, 64, 140–157. [Google Scholar] [CrossRef]
| Original Measures | Dichotomised | Categorisation |
|---|---|---|
| Health care card status | ||
| Yes | Yes | Low SEP |
| No | No | High SEP |
| Maternal education | ||
| No school | High school or less | Low SEP |
| Primary school | ||
| High school | Trade or University | High SEP |
| Trade/TAFE | ||
| University | ||
| Car ownership | ||
| Yes | Yes | High SEP |
| No | No | Low SEP |
| Difficulty paying AUD 100 dental bill | ||
| Not hard at all | Minimal difficulty (Not hard at all, Not very hard) | High SEP |
| Not very hard | ||
| A little bit hard | Some difficulty (A little bit hard, Very hard, Could not pay) | |
| Very hard | Low SEP | |
| Could not pay | ||
| Index of relative socioeconomic advantage and disadvantage (IRSAD) | ||
| Decile 1–10 | Decile 1–5 | Low SEP |
| Decile 6–10 | High SEP | |
| Measure | Overall Sample (N = 226) 1 N (%) |
|---|---|
| Health care card status | |
| Yes | 176 (80.0%) |
| No | 44 (20.0%) |
| Maternal education | |
| High school or less | 151 (67.7%) |
| Trade or University | 72 (32.3%) |
| Car ownership | |
| Yes | 122 (54.7%) |
| No | 101 (45.3%) |
| Difficulty paying AUD 100 dental bill | |
| Minimal difficulty | 49 (22.0%) |
| Some difficulty | 174 (78.0%) |
| IRSAD | |
| Decile 1–5 | 200 (90.9%) |
| Decile 6–10 | 20 (9.1%) |
| Socioeconomic Position (SEP) | |
| High SEP | 63 (28.9%) |
| Low SEP | 155 (71.1%) |
| Mean Maternal Age in Years (SD) | 28.5 (6.65) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poirier, B.F.; Hedges, J.; Smithers, L.G.; Moskos, M.; Jamieson, L.M. Child-, Family-, and Community-Level Facilitators for Promoting Oral Health Practices among Indigenous Children. Int. J. Environ. Res. Public Health 2022, 19, 1150. https://doi.org/10.3390/ijerph19031150
Poirier BF, Hedges J, Smithers LG, Moskos M, Jamieson LM. Child-, Family-, and Community-Level Facilitators for Promoting Oral Health Practices among Indigenous Children. International Journal of Environmental Research and Public Health. 2022; 19(3):1150. https://doi.org/10.3390/ijerph19031150
Chicago/Turabian StylePoirier, Brianna F., Joanne Hedges, Lisa G. Smithers, Megan Moskos, and Lisa M. Jamieson. 2022. "Child-, Family-, and Community-Level Facilitators for Promoting Oral Health Practices among Indigenous Children" International Journal of Environmental Research and Public Health 19, no. 3: 1150. https://doi.org/10.3390/ijerph19031150
APA StylePoirier, B. F., Hedges, J., Smithers, L. G., Moskos, M., & Jamieson, L. M. (2022). Child-, Family-, and Community-Level Facilitators for Promoting Oral Health Practices among Indigenous Children. International Journal of Environmental Research and Public Health, 19(3), 1150. https://doi.org/10.3390/ijerph19031150







