Effect of Treadmill Training with Visual Biofeedback on Selected Gait Parameters in Subacute Hemiparetic Stroke Patients
Abstract
1. Introduction
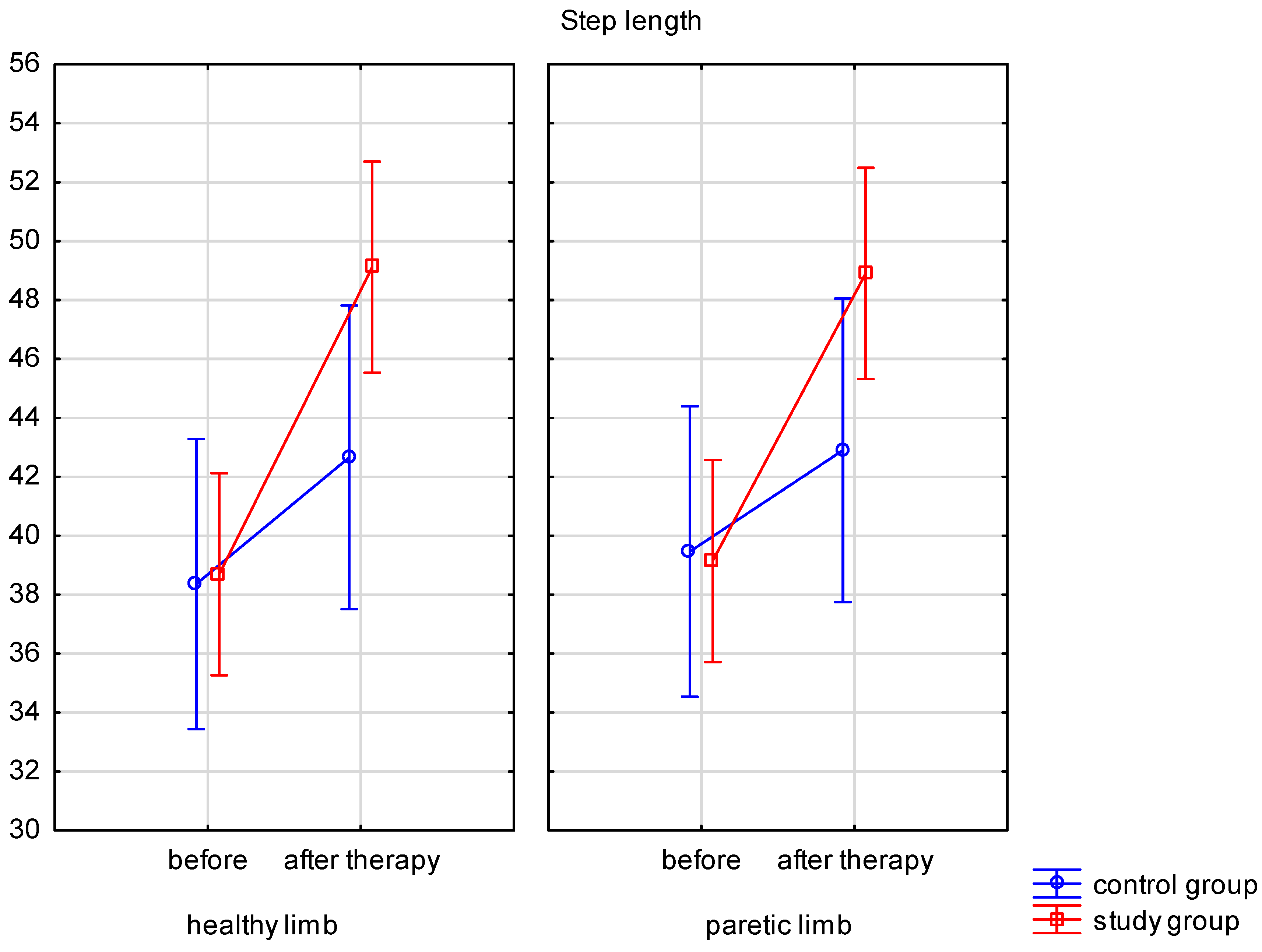
- Effects of the treadmill with visual feedback on the step length and load on paretic and healthy limbs.
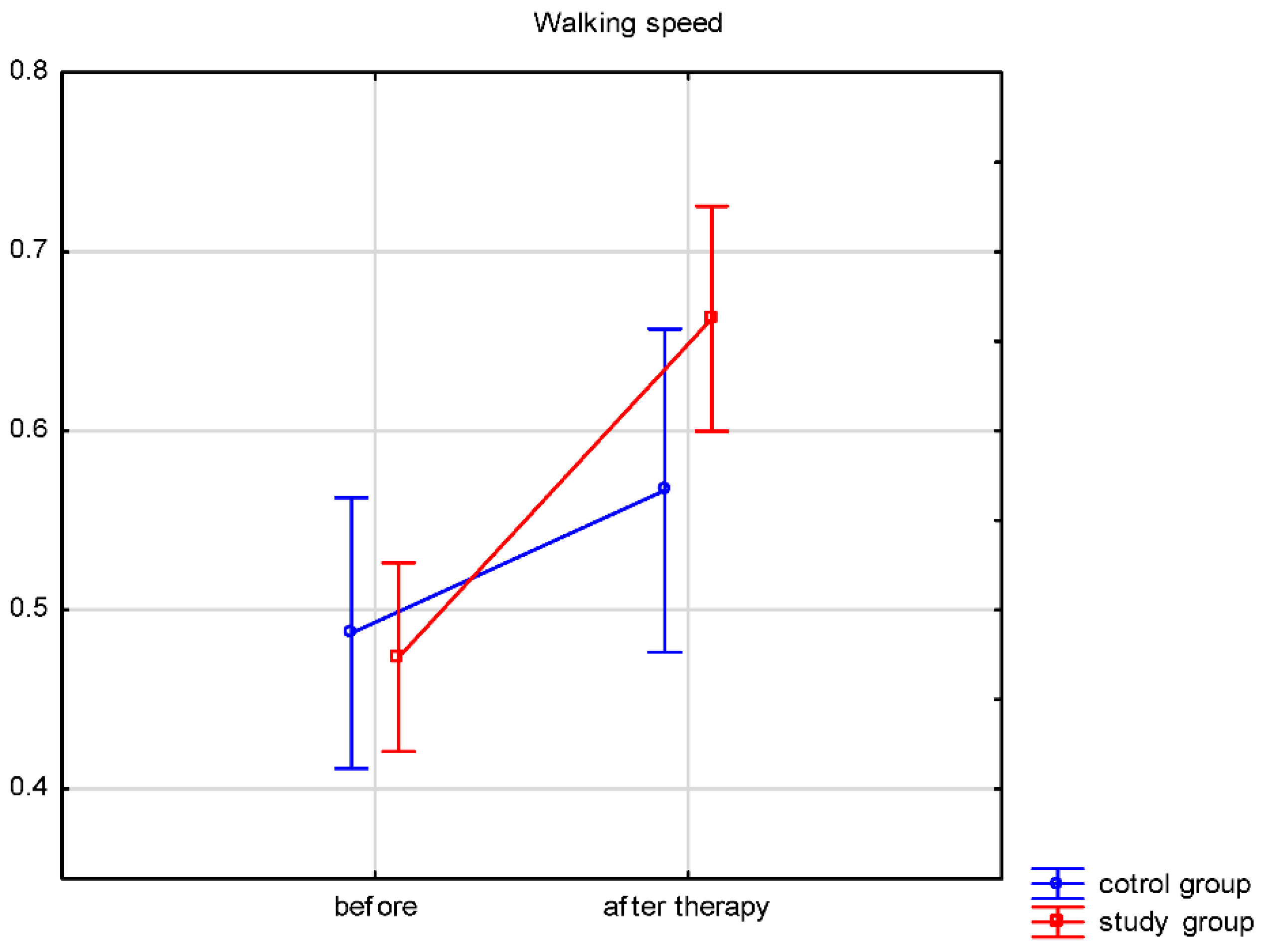
- Effects of the treadmill with visual feedback on walking speed.
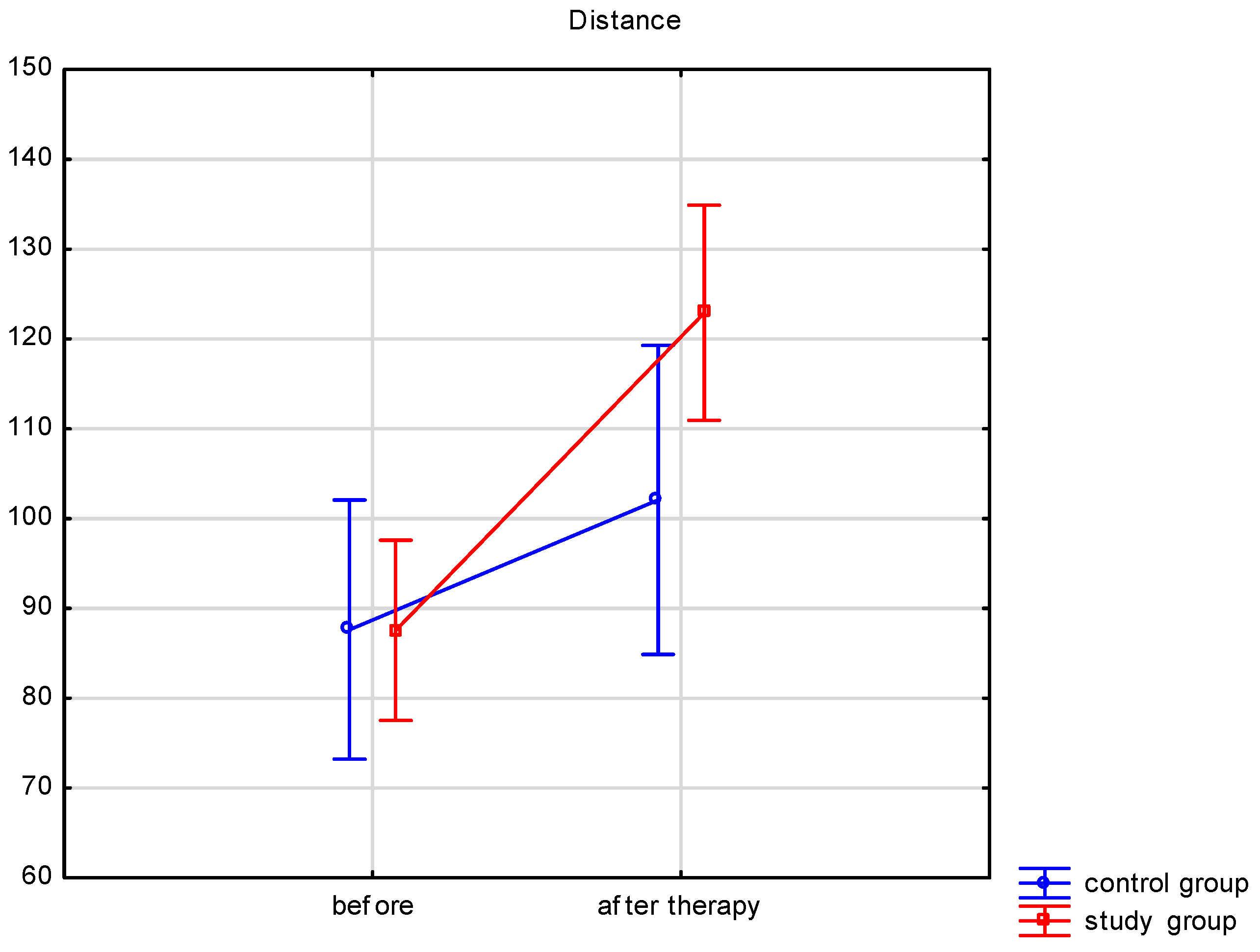
- Effects of the treadmill with visual feedback on improved functional gait variables, such as sense of balance and walking base, and decreasing the need for orthopedic aids.
2. Materials and Methods
2.1. Procedure and Instruments
- step length for the paretic and the healthy limb (cm)
- load on the paretic and the healthy limb (%)
- walking speed (km/h)
2.2. Protocol
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Step Length
4.2. Lower Limb Loading
4.3. Speed
4.4. Balance
4.5. Summary
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tanaka, H.; Nankaku, M.; Nishikawa, T.; Hosoe, T.; Yonezawa, H.; Mori, H.; Kikuchi, T.; Nishi, H.; Takagi, Y.; Miyamoto, S.; et al. Spatiotemporal gait characteristic changes with gait training using the hybrid assistive limb for chronic stroke patients. Gait Posture 2019, 71, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Thaut, M.H.; Leins, A.K.; Rice, R.R.; Argstatter, H.; Kenyon, G.P.; McIntosh, G.C.; Bolay, H.V.; Fetter, M. Rhythmic auditory stimulation improves gait more than NDT/Bobath training in near-ambulatory patients early poststroke: A single-blind, randomized trial. Neurorehabil. Neural Repair 2007, 21, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Park, S.G.; Lim, H.J.; Park, G.C.; Kim, M.H.; Lee, B.H. Effects of the combination of rhythmic auditory stimulation and task-oriented training on functional recovery of subacute stroke patients. J. Phys. Ther. Sci. 2012, 24, 1307–1313. [Google Scholar] [CrossRef]
- Li, S.; Francisco, G.E.; Zhou, P. Post-stroke hemiplegic gait: New perspective and insights. Front. Physiol. 2018, 9, 1021. [Google Scholar] [CrossRef]
- Oatis, C.A. Kinesiology: The Mechanics and Pathomechanics of Human Movement, 2nd ed.; Williams and Wilkins: Baltimore, MD, USA, 2009; pp. 896–911. [Google Scholar]
- Elsner, B.; Schöler, A.; Kon, T.; Mehrholz, J. Walking with rhythmic auditory stimulation in chronic patients after stroke: A pilot randomized controlled trial. Physiother. Res. Int. 2020, 25, e1800. [Google Scholar] [CrossRef] [PubMed]
- Sheng, Y.; Kan, S.; Wen, Z.; Chen, W.; Qi, Q.; Qu, Q.; Yu, B. Effect of Kinesio Taping on the Walking Ability of Patients with Foot Drop after Stroke. Evid.-Based Complement Altern Med. 2019, 2019, 1–7. [Google Scholar] [CrossRef]
- Hase, K.; Suzuki, E.; Matsumoto, M.; Fujiwara, T.; Liu, M. Effects of therapeutic gait training using a prosthesis and a treadmill for ambulatory patients with hemiparesis. Arch. Phys. Med. Rehabil. 2011, 92, 1961–1966. [Google Scholar] [CrossRef]
- Drużbicki, M.; Guzik, A.; Przysada, G.; Kwolek, A.; Brzozowska-Magoń, A.; Sobolewski, M. Changes in gait symmetry after training on a treadmill with biofeedback in chronic stroke patients: A 6-month follow-up from a randomized controlled trial. Med. Sci. Monit. 2016, 22, 4859–4868. [Google Scholar] [CrossRef]
- Druzbicki, M.; Guzik, A.; Przysada, G.; Kwolek, A.; Brzozowska-Magoń, A. Efficacy of gait training using a treadmill with and without visual biofeedback in patients after stroke: A randomized study. J. Rehabil. Med. 2015, 47, 419–425. [Google Scholar] [CrossRef]
- Drużbicki, M.; Przysada, G.; Guzik, A.; Brzozowska-Magoń, A.; Kołodziej, K.; Nieroda, A.W.; Majewska, J.; Kwolek, A. The efficacy of gait training using a body weight support treadmill and visual biofeedback in patients with subacute stroke: A randomized controlled trial. BioMed Res. Int. 2018, 2018, 3812602. [Google Scholar] [CrossRef]
- Samson, M.M.; Crowe, A.; de Vreede, P.L.; Dessens, J.A.G.; Duursma, S.A.; Verhaar, H.J.J. Differences in gait parameters at a preferred walking speed in healthy subjects due to age, height and body weight. Aging Clin. Exp. Res. 2001, 13, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Middleton, A.; Fritz, S.L.; Lusardi, M. Walking speed: The functional vital sign. J. Aging Phys. Act. 2015, 23, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Nigg, B.M.; Fisher, V.; Ronsky, J.L. Gait characteristics as a function of age and gender. Gait Posture 1994, 2, 213–220. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Wang, Y.C. Four-Meter Gait Speed: Normative Values and Reliability Determined for Adults Participating in the NIH Toolbox Study. Arch. Phys. Med. Rehabil. 2019, 100, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Rozanski, G.M.; Wong, J.S.; Inness, E.L.; Patterson, K.K.; Mansfield, A. Longitudinal change in spatiotemporal gait symmetry after discharge from inpatient stroke rehabilitation. Disabil. Rehabil. 2018, 42, 1–7. [Google Scholar] [CrossRef]
- Little, V.L.; Perry, L.A.; Mercado, M.W.V.; Kautz, S.A.; Patten, C. Gait asymmetry pattern following stroke determines acute response to locomotor task. Gait Posture 2020, 77, 300–307. [Google Scholar] [CrossRef]
- Ribeiro, T.; Silva, E.; Silva, S.; Regalado, I.; Lindquist, R. Effects of gait training with unilateral leg load on weight bearing asymmetry of individuals with stroke: A randomized clinical trial. Ann. Phys. Rehabil. Med. 2018, 61, e464. [Google Scholar] [CrossRef]
- Beyaert, C.; Vasa, R.; Frykberg, G.E. Gait post-stroke: Pathophysiology and rehabilitation strategies. Neurophysiol. Clin. 2015, 45, 335–355. [Google Scholar] [CrossRef]
- Patterson, K.K.; Nadkarni, N.K.; Black, S.E.; McIlroy, W.E. Gait symmetry and velocity differ in their relationship to age. Gait Posture 2012, 35, 590–594. [Google Scholar] [CrossRef]
- Hodt-Billington, C.; Helbostad, J.L.; Moe-Nilssen, R. Should trunk movement or footfall parameters quantify gait asymmetry in chronic stroke patients? Gait Posture 2008, 27, 552–558. [Google Scholar] [CrossRef]
- Begg, R.; Galea, M.P.; James, L.; Sparrow, W.A.T.; Levinger, P.; Khan, F.; Said, C.M. Real-time foot clearance biofeedback to assist gait rehabilitation following stroke: A randomized controlled trial protocol. Trials 2019, 20, 317. [Google Scholar] [CrossRef] [PubMed]
- Mohammed Gharib, N.; Ali Mohamed, R.; Professor, A. Isokinetic strength training in patients with stroke: Effects on muscle strength, gait and functional mobility. Orig. Res. Artic. 2017, 5, 1976–1986. [Google Scholar] [CrossRef]
- Singhal, S.; Pattnaik, M.; Mohanty, P. Comparison of isokinetic strengthening with functional strengthening of lower limb and their effect on gait in hemiparesis due to stroke. J. Neurol. Neurorehabil. Res. 2017, 2, 46–54. [Google Scholar] [CrossRef]
- Chlebuś, E.; Lisiński, P. Comparison of the effects of early neurological rehabilitation in patients after haemorrhagic or ischemic stroke. Issue Rehabil. Orthop. Neurophysiol. Sport Promot. 2017, 21, 21–33. [Google Scholar] [CrossRef]
- Gunning, E.; Uszynski, M.K. Effectiveness of the Proprioceptive Neuromuscular Facilitation Method on Gait Parameters in Patients With Stroke: A Systematic Review. Arch. Phys. Med. Rehabil. 2019, 100, 980–986. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Arribas, M.J.; Martín-Casas, P.; Cano-de-la-Cuerda, R.; Plaza-Manzano, G. Effectiveness of the Bobath concept in the treatment of stroke: A systematic review. Disabil. Rehabil. 2019, 42, 1636–1649. [Google Scholar] [CrossRef]
- Mikołajewska, E. Bobath and traditional approaches in post-stroke gait rehabilitation in adults. Biomed Hum. Kinet. 2017, 9, 27–33. [Google Scholar] [CrossRef]
- Kim, J.I.; Kang, H.W.; Ji, M.; Hwang, S.S.; Maeng, G.C. The Effect of Stabilizing Reversal and Rhythmic Stabilization in PNF on Walking and Balance in Patients with Stroke. PNF Mov. 2018, 16, 195–205. [Google Scholar] [CrossRef]
- Krukowska, J.; Bugajski, M.; Sienkiewicz, M.; Czernicki, J. The influence of NDT-Bobath and PNF methods on the field support and total path length measure foot pressure (COP) in patients after stroke. Neurol. Neurochir. Pol. 2016, 50, 449–454. [Google Scholar] [CrossRef]
- Yen, C.L.; Wang, R.Y.; Liao, K.K.; Huang, C.C.; Yang, Y.R. Gait training-induced change in corticomotor excitability in patients with chronic stroke. Neurorehabil. Neural Repair. 2008, 22, 22–30. [Google Scholar] [CrossRef]
- Baer, G.D.; Salisbury, L.G.; Smith, M.T.; Pitman, J.; Dennis, M. Treadmill training to improve mobility for people with sub-acute stroke: A phase II feasibility randomized controlled trial. Clin. Rehabil. 2018, 32, 201–212. [Google Scholar] [CrossRef] [PubMed]
- MacKay-Lyons, M.; McDonald, A.; Matheson, J.; Eskes, G.; Klus, M.A. Dual effects of body-weight supported treadmill training on cardiovascular fitness and walking ability early after stroke: A randomized controlled trial. Neurorehabil. Neural Repair 2013, 27, 644–653. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, A.; Taly, A.B.; Gupta, A.; Kumar, S.; Murali, T. Bodyweight-supported treadmill training for retraining gait among chronic stroke survivors: A randomized controlled study. Ann. Phys. Rehabil. Med. 2016, 59, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.-R.; Lo, W.L.; Lin, Q.; Li, L.; Xiao, X.; Raghavan, P.; Huang, D.-F. The Effect of Body Weight Support Treadmill Training on Gait Recovery, Proximal Lower Limb Motor Pattern, and Balance in Patients with Subacute Stroke. BioMed Res. Int. 2015, 2015, 1–10. [Google Scholar] [CrossRef]
- Spencer, J.; Wolf, S.W.; Kesar, T.M. Biofeedback for Post-stroke Gait Retraining: A Review of Current Evidence and Future Research Directions on the Context of Emerging Technologies. Front. Neurol. 2021, 12, 637199. [Google Scholar] [CrossRef]
- Giggins, O.M.; Persson, U.M.C.; Caulfield, B. Biofeedback in rehabilitation. J. Neuroeng. Rehabil. 2013, 10, 60. [Google Scholar] [CrossRef]
- Thikey, H.; Grealy, M.; van Wijck, F.; Barber, M.; Rowe, P. Augmented visual feedback of movement performance to enhance walking recovery after stroke: Study protocol for a pilot randomised controlled trial. Trials 2012, 13, 163. [Google Scholar] [CrossRef]
- Whittle, M.W.; Richards, J.L.D. Whittle’s Gait Analysis; Churchill Livingstone: London, UK, 2012; p. 70. [Google Scholar]
- Hodkinson, H.M. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972, 1, 233. [Google Scholar] [CrossRef]
- Gregson, J.M.; Leathley, M.J.; Moore, A.P.; Smith, T.L.; Sharma, A.K.; Watkins, C.L. Reliability of measurements of muscle tone and muscle power in stroke patients. Age Ageing 2000, 29, 223–228. [Google Scholar] [CrossRef]
- Cirstea, C.M. Gait Rehabilitation After Stroke Should We Re-Evaluate Our Practice? Stroke 2020, 51, 2892–2894. [Google Scholar] [CrossRef]
- Hidayat, A.A.; Arief, Z.; Yuniarti, H. LOVETT scalling with MYO armband for monitoring finger muscles therapy of post-stroke people. In Proceedings-2016 International Electronics Symposium, IES 2016; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2017; pp. 66–70. [Google Scholar] [CrossRef]
- Feigin, V.L.; Krishnamurthi, R.V.; Parmar, P.; Norrving, B.; Mensah, G.A.; Bennett, D.A.; Barker-Collo, S.; Moran, A.E.; Sacco, R.L.; Truelsen, T.; et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: The GBD 2013 study. Neuroepidemiology 2015, 45, 161–176. [Google Scholar] [CrossRef] [PubMed]
- Brewer, L.; Horgan, F.; Hibkey, A.; Williams, D. Stroke rehabilitation: Recent advances and future therapies. Q. J. Med. 2013, 106, 11–25. [Google Scholar] [CrossRef] [PubMed]
- Stanton, R.; Ada, L.; Dean, C.M.; Preston, E. Biofeedback improves performance in lower limb activities more than usual therapy in people following stroke: A systematic review. J. Physiother. 2017, 63, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Patterson, K.K.; Mansfield, A.; Biasin, L.; Brunton, K.; Inness, E.L.; McIlroy, W.E. Longitudinal changes in poststroke spatiotemporal gait asymmetry over inpatient rehabilitation. Neurorehabil. Neural Repair 2015, 29, 153–162. [Google Scholar] [CrossRef]
- Neumann, D.A. Kinesiology of Musculoskeletal System. Foundations for Rehabilitation; Elsevier Health Sciences: St. Louis, MO, USA, 2016; p. 527. [Google Scholar]
- Wang, Y.; Pan, W.-Y.; Li, F.; Ge, J.-S.; Zhang, X.; Luo, X.; Wang, Y.-L. Effect of Rhythm of Music Therapy on Gait in Patients with Stroke. J. Stroke Cerebrovasc. Dis. 2021, 30, 105544. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.A.; Fox, E.J.; Daly, J.J.; Rose, D.K.; Wu, S.S.; Christou, E.A.; Hawkins, K.A.; Otzel, D.M.; Butera, K.A.; Skinner, J.W.; et al. Interpreting prefrontal recruitment during walking after stroke: Influence of individual differences in mobility and cognitive function. Front. Hum. Neurosci. 2019, 13, 194. [Google Scholar] [CrossRef] [PubMed]
- Bishop, L.; Khan, M.; Martelli, D.; Quinn, L.; Stein, J.; Agrawal, S. Exploration of two training paradigms using forced induced weight shifting with the tethered pelvic assist device to reduce asymmetry in individuals after stroke case reports. Am. J. Phys. Med. Rehabil. 2017, 96, S135–S140. [Google Scholar] [CrossRef]
- Bonnyaud, C.; Pradon, D.; Zory, R.; Bussel, B.; Bensmail, D.; Vuillerme, N.; Roche, N. Effects of a gait training session combined with a mass on the non-paretic lower limb on locomotion of hemiparetic patients: A randomized controlled clinical trial. Gait Posture 2013, 37, 627–630. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, T.S.; Regalado, I.C.; da Silva, S.T.; de Oliveira Sousa, C.; de Figueiredo, K.M.; Lindquist, A.R. Effects of load addition during gait training on weight-bearing and temporal asymmetry after stroke. Am. J. Phys. Med. Rehabil. 2020, 99, 250–256. [Google Scholar] [CrossRef]
- Murtagh, E.M.; Mair, J.L.; Aguiar, E.; Tudor-Locke, C.; Murphy, M.H. Outdoor Walking Speeds of Apparently Healthy Adults: A Systematic Review and Meta-analysis. Sport Med. 2021, 51, 125–141. [Google Scholar] [CrossRef]
- Park, S.; Liu, C.; Sánchez, N.; Tilson, J.K.; Mulroy, S.J.; Finley, J.M. Using Biofeedback to Reduce Step Length Asymmetry Impairs Dynamic Balance in People Poststroke. Neurorehabil. Neural Repair 2021, 35, 738–749. [Google Scholar] [CrossRef] [PubMed]
- Regnaux, J.P.; Pradon, D.; Roche, N.; Robertson, J.; Bussel, B.; Dobkin, B. Effects of loading the unaffected limb for one session of locomotor training on laboratory measures of gait in stroke. Clin. Biomech. 2008, 23, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.H.; Lee, W.H. Virtual walking training program using a real-world video recording for patients with chronic stroke: A pilot study. Am. J. Phys. Med. Rehabil. 2013, 92, 371–380; quiz 380–382, 458. [Google Scholar] [CrossRef]
- Jonsdottir, J.; Cattaneo, D.; Recalcati, M.; Regola, A.; Rabuffetti, M.; Ferrarin, M.; Casiraghi, A. Task-oriented biofeedback to improve gait in individuals with chronic stroke: Motor learning approach. Neurorehabil. Neural Repair 2010, 24, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Park, E.C.; Hwangbo, G. The effects of action observation gait training on the static balance and walking ability of stroke patients. J. Phys. Ther. Sci. 2015, 27, 341–344. [Google Scholar] [CrossRef] [PubMed]
- Seo, K.C.; Park, S.H.; Park, K. The effects of stair gait training using proprioceptive neuromuscular facilitation on stroke patients’ dynamic balance ability. J. Phys. Ther. Sci. 2015, 27, 1459–1462. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, A.; Taly, A.B.; Gupta, A.; Kumar, S.; Murali, T. Post-stroke balance training: Role of force platform with visual feedback technique. J. Neurol. Sci. 2009, 287, 89–93. [Google Scholar] [CrossRef]
- Li, J.; Zhong, D.; Ye, J.; He, M.; Liu, X.; Zheng, H.; Jin, R.; Zhang, S.-L. Rehabilitation for balance impairment in patients after stroke: A protocol of a systematic review and network meta-analysis. BMJ Open 2019, 9, e026844. [Google Scholar] [CrossRef]
- Khallaf, M.E.; Gabr, A.M.; Fayed, E.E. Effect of Task Specific Exercises, Gait Training, and Visual Biofeedback on Equinovarus Gait among Individuals with Stroke: Randomized Controlled Study. Neurol Res Int. 2014, 2014, 693048. [Google Scholar] [CrossRef]
- Kim, N.; Park, Y.; Lee, B.H. Effects of community-based virtual reality treadmill training on balance ability in patients with chronic stroke. J. Phys. Ther. Sci. 2015, 27, 655–658. [Google Scholar] [CrossRef]
- Maciaszek, J. Effects of Posturographic Platform Biofeedback Training on the Static and Dynamic Balance of Older Stroke Patients. J. Stroke Cerebrovasc. Dis. 2018, 27, 1969–1974. [Google Scholar] [CrossRef] [PubMed]
- Jankowska, A.; Klimkiewicz, P.; Krukowska, S.; Woldańska-Okońska, M. Assessment of the Impact of Training on the Stabilometric Platform Using the Biofeedback Method on Improving Balance and Functional Efficiency of Patients After a Stroke. Acta Balneol. 2021, 62, 15–21. [Google Scholar] [CrossRef]
| Variable | Study Group | Control Group | |||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Median | Min–Max | Mean ± SD | Median | Min–Max | p | |
| age | 63.0 ± 10.9 | 65.0 | 27.0–85.0 | 61.9 ± 14.0 | 61.0 | 30.0–87.0 | 0.816 |
| height (m) | 1.69 ± 0.10 | 1.68 | 1.43–1.850 | 1.70 ± 0.014 | 1.70 | 1.43–2.10 | 0.705 |
| weight (kg) | 77.8 ± 14.8 | 78.0 | 53.0–110.0 | 77.5 ± 13.9 | 74.0 | 54.0–108.0 | 0.647 |
| BMI | 27.4 ± 4.7 | 26.8 | 18.3–42.4 | 26.9 ± 4.1 | 26.2 | 18.7–36.0 | 0.708 |
| Variables | Paretic Limb | Healthy Limb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study Group | Control Group | p between Groups | Study Group | Control Group | p between Groups | Main Effect p | Group × Time Interaction | |||
| Step length [cm] | Before | mean ± SD median range | 39.1 ± 12.6 38.5 15.0–67.0 | 39.5 ± 15.0 36.5 13.0–70.0 | 0.230 | 38.7 ± 13.0 37.0 10.0–64.0 | 38.4 ± 15.8 35.5 7.0–68.0 | 0.916 | <0.001 | 0.018 |
| After therapy | mean ± SD median range | 48.9 ± 13.3 50.0 12.0–67.0 | 42.9 ± 15.8 45.0 12.0–72.0 | 0.056 | 49.1 ± 13.1 51.5 19.0–71.0 | 42.7 ± 17.0 43.0 9.0–75.0 | 0.040 | |||
| p * | <0.001 | 0.023 | <0.001 | 0.005 | ||||||
| Limb loading (time on limb) [%] | Before | mean ± SD median range | 49.5 ± 3.5 50.0 37.0–59.0 | 49.5 ± 3.0 49.5 39.0–54.0 | 0.913 | 50.4 ± 3.5 50.0 41.0–63.0 | 51.1 ± 3.7 50.0 44.0–72.0 | 0.709 | 0.219 | 0.722 |
| After therapy | mean ± SD median range | 49.4 ± 4.0 50.0 28.0–65.0 | 49.4 ± 2.1 50.0 42.0–52.0 | 0.962 | 51.1 ± 3.7 50.0 44.0–72.0 | 50.7 ± 3.0 50.0 46.0–61.0 | 0.580 | |||
| p * | 0.869 | 0.946 | 0.385 | 0.919 | ||||||
| Variables | Study Group | Control Group | p between Groups | Main Effect p | Group × Time Interaction | ||
|---|---|---|---|---|---|---|---|
| Walking speed [m/s] | Before | mean ± SD median range | 0.47 ± 0.19 0.47 0.11–0.92 | 0.49 ± 0.25 0.47 0.14–1.31 | 0.642 | <0.001 | <0.001 |
| After therapy | mean ± SD median range | 0.66 ± 0.24 0.63 0.19–1.25 | 0.57 ± 0.27 0.56 0.17–1.33 | 0.023 | |||
| p * | <0.001 | <0.001 | |||||
| Distance traveled [m] | Before | mean ± SD median range | 87.5 ± 36.9 85.0 18.0–170.0 | 87.6 ± 45.2 84.0 25.0–237.0 | 0.768 | <0.001 | <0.001 |
| After therapy | mean ± SD median range | 122.9 ± 47.3 116.5 34.5–238.0 | 102.1 ± 47.8 100.0 30.0–240.0 | <0.001 | |||
| p * | <0.001 | <0.001 | |||||
| Variable | Group | Before Therapy | After Therapy | |||
|---|---|---|---|---|---|---|
| Abnormal | Normal | Abnormal | Normal | p | ||
| Romberg test | study | 47 (75.8%) | 15 (24.2%) | 20 (32.3%) | 42 (67.7%) | <0.001 |
| control | 19 (63.3%) | 11 (36.7%) | 8 (26.7%) | 22 (73.3%) | 0.006 | |
| Walking base | study | 44 (71.0%) | 18 (29.0%) | 27 (43.5%) | 35 (56.5%) | <0.001 |
| control | 20 (66.7%) | 10 (33.3%) | 25 (83.3%) | 5 (16.7%) | 0.074 | |
| Orthopedic aid * | study | 23 (37.1%) | 39 (62.9%) | 10 (16.1%) | 52 (83.9%) | 0.006 |
| control | 21 (70.0%) | 9 (30.0%) | 10 (33.3%) | 20 (66.7%) | 0.006 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaźmierczak, K.; Wareńczak-Pawlicka, A.; Miedzyblocki, M.; Lisiński, P. Effect of Treadmill Training with Visual Biofeedback on Selected Gait Parameters in Subacute Hemiparetic Stroke Patients. Int. J. Environ. Res. Public Health 2022, 19, 16925. https://doi.org/10.3390/ijerph192416925
Kaźmierczak K, Wareńczak-Pawlicka A, Miedzyblocki M, Lisiński P. Effect of Treadmill Training with Visual Biofeedback on Selected Gait Parameters in Subacute Hemiparetic Stroke Patients. International Journal of Environmental Research and Public Health. 2022; 19(24):16925. https://doi.org/10.3390/ijerph192416925
Chicago/Turabian StyleKaźmierczak, Katarzyna, Agnieszka Wareńczak-Pawlicka, Margaret Miedzyblocki, and Przemysław Lisiński. 2022. "Effect of Treadmill Training with Visual Biofeedback on Selected Gait Parameters in Subacute Hemiparetic Stroke Patients" International Journal of Environmental Research and Public Health 19, no. 24: 16925. https://doi.org/10.3390/ijerph192416925
APA StyleKaźmierczak, K., Wareńczak-Pawlicka, A., Miedzyblocki, M., & Lisiński, P. (2022). Effect of Treadmill Training with Visual Biofeedback on Selected Gait Parameters in Subacute Hemiparetic Stroke Patients. International Journal of Environmental Research and Public Health, 19(24), 16925. https://doi.org/10.3390/ijerph192416925






