A Rapid Review of the Factors That Influence Service User Involvement in Interprofessional Education, Practice, and Research
Abstract
1. Introduction
1.1. Review Aims
1.2. Review Questions
- What is the current status of service user involvement in interprofessional education, practice, and research?
- What are the enablers of and barriers to service user involvement in interprofessional education, practice, and research?
2. Materials and Methods
2.1. Needs Assessment
2.2. Protocol Development
2.3. Literature Search
2.3.1. Database Selection
2.3.2. Search Strategy
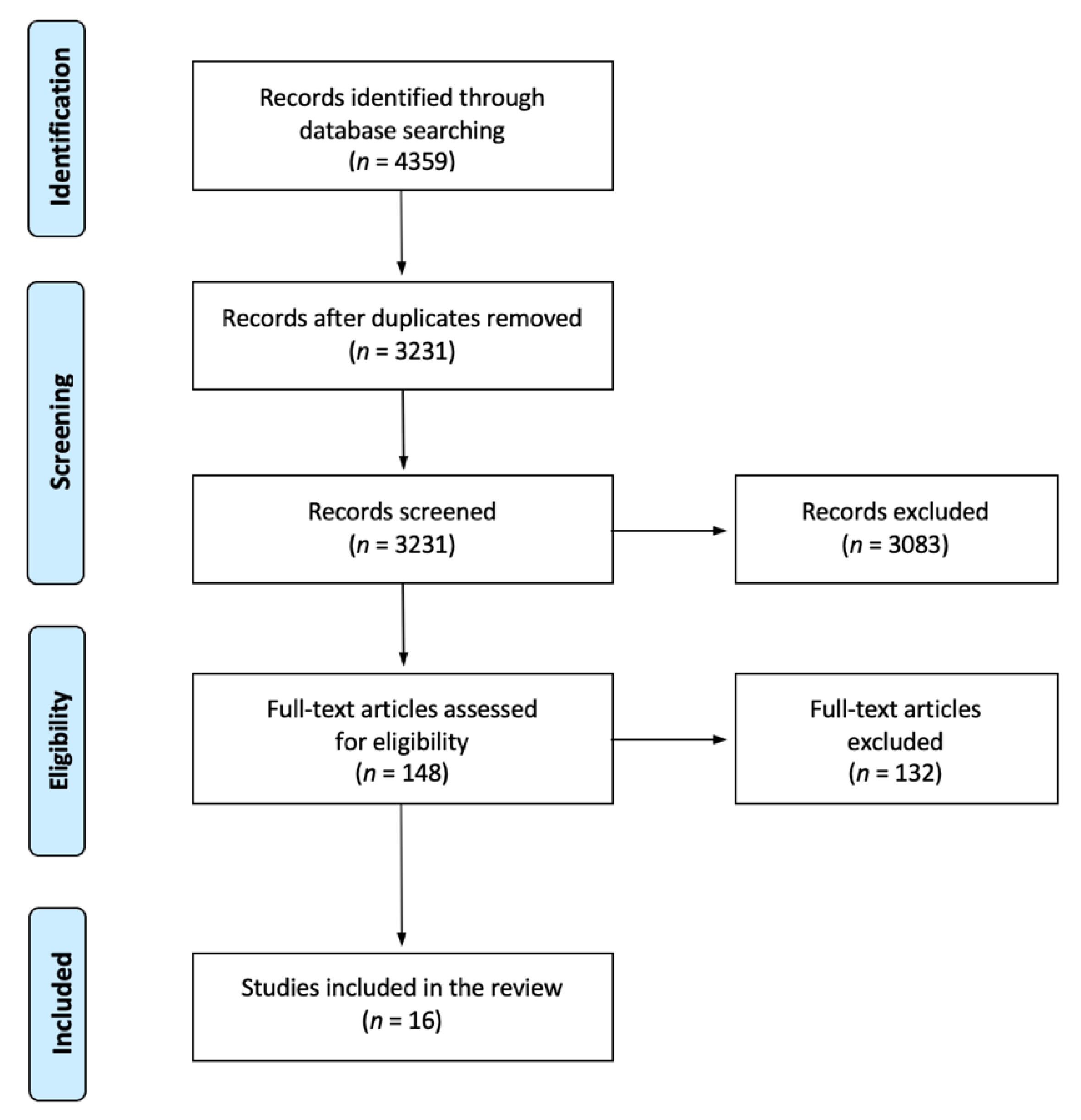
2.4. Screening and Study Selection
2.5. Data Extraction
2.6. Risk of Bias (Quality) Assessment
2.7. Knowledge Synthesis
3. Results
3.1. Methodological Quality
3.2. Service User Involvement in IPECP Education, Practice, and Research
3.2.1. Nature of Service User Involvement
3.2.2. Enablers
3.2.3. Barriers
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Australian Health Ministers. National Mental Health Policy 2008; Commonwealth of Australia: Canberra, Australia, 2009.
- House of Commons Health Committee. Patient and public involvement in the NHS. In HC-278-I; The Stationery Office: London, UK, 2007. [Google Scholar]
- Health & Care Professions Council. Standards of Conduct, Performance and Ethics; Health & Care Professions Council: London, UK, 2016. [Google Scholar]
- Happell, B.; Byrne, L.; McAllister, M.; Lampshire, D.; Roper, C.; Gaskin, C.J.; Martin, G.; Wynaden, D.; McKenna, B.; Lakeman, R.; et al. Consumer involvement in the tertiary-level education of mental health professionals: A systematic review. Int. J. Ment. Health Nurs. 2014, 23, 3–16. [Google Scholar] [CrossRef]
- Wiles, L.K.; Kay, D.; Luker, J.A.; Worley, A.; Austin, J.; Ball, A.; Bevan, A.; Cousins, M.; Dalton, S.; Hodges, E.; et al. Consumer engagement in health care policy, research and services: A systematic review and meta-analysis of methods and effects. PLoS ONE 2022, 17, e0261808. [Google Scholar] [CrossRef]
- Romme, S.; Bosveld, M.H.; Van Bokhoven, M.A.; De Nooijer, J.; Van den Besselaar, H.; Van Dongen, J.J.J. Patient involvement in interprofessional education: A qualitative study yielding recommendations on incorporating the patient’s perspective. Health Expect. 2020, 23, 943–957. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.B.; Norbye, B.; Dahlgren, M.A.; Iversen, A. Patient participation in interprofessional learning and collaboration with undergraduate health professional students in clinical placements: A scoping review. J. Interprofessional Educ. Pract. 2022, 27, 100494. [Google Scholar] [CrossRef]
- Lammers, J.; Happell, B. Mental health reforms and their impact on consumer and carer participation: A perspective from Victoria, Australia. Issues Ment. Health Nurs. 2004, 25, 261–276. [Google Scholar] [CrossRef]
- Towle, A.; Bainbridge, L.; Godolphin, W.; Katz, A.; Kline, C.; Lown, B.; Madularu, I.; Solomon, P.; Thistlethwaite, J. Active patient involvement in the education of health professionals. Med. Educ. 2010, 44, 64–74. [Google Scholar] [CrossRef]
- Repper, J.; Breeze, J. User and carer involvement in the training and education of health professionals: A review of the literature. Int. J. Nurs. Stud. 2007, 44, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Jones, C. Involving NHS service users in teaching advanced clinical skills. Br. J. Nurs. 2006, 15, 462–465. [Google Scholar] [CrossRef] [PubMed]
- Slattery, P.; Saeri, A.K.; Bragge, P. Research co-design in health: A rapid overview of reviews. Health Res. Policy Syst. 2020, 18, 17. [Google Scholar] [CrossRef]
- Hanley, B.; Bradburn, J.; Gorin, S.; Barnes, M.; Evans, C.; Goodare, H.; Kelson, M.; Kent, A.; Oliver, S.; Wallcraft, J. Involving Consumers in Research and Development in the NHS: Briefing Notes for Researchers; Consumers in NHS Research Support Unit: Hamshire, UK, 2000. [Google Scholar]
- World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Young, A.S.; Chinman, M.; Forquer, S.L.; Knight, E.L.; Vogel, H.; Miller, A.; Rowe, M.; Mintz, J. Use of a consumer-led intervention to improve provider competencies. Psychiatr. Serv. 2005, 56, 967–975. [Google Scholar] [CrossRef]
- Curran, V.; Heath, O.; Adey, T.; Callahan, T.; Craig, D.; Hearn, T.; White, H.; Hollett, A. An approach to integrating interprofessional education in collaborative mental health care. Acad. Psychiatry 2012, 36, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.; Carpenter, J.; Dickinson, C. The outcomes of partnerships with mental health service users in interprofessional education: A case study. Health Soc. Care Community 2006, 14, 426–435. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cooper, H.; Spencer-Dawe, E. Involving service users in interprofessional education narrowing the gap between theory and practice. J. Interprofessional Care 2006, 20, 603–617. [Google Scholar] [CrossRef]
- Carpenter, J.; Barnes, D.; Dickinson, C.; Wooff, D. Outcomes of interprofessional education for Community Mental Health Services in England: The longitudinal evaluation of a postgraduate programme. J. Interprofessional Care 2006, 20, 145–161. [Google Scholar] [CrossRef][Green Version]
- Kvarnström, S.; Hedberg, B.; Cedersund, E. The dual faces of service user participation: Implications for empowerment processes in interprofessional practice. J. Soc. Work. 2013, 13, 287–307. [Google Scholar] [CrossRef]
- Khalili, H.; Breitbach, A.; Jensen, G.; King, S.; Maxwell, B.; Nickol, D.; Pfeifle, A.; Gilbert, J. Global leadership in IPECP research: An intro to co-creation of best practice guidelines. J. Interprofessional Educ. Pract. 2021, 24, 100445. [Google Scholar] [CrossRef]
- Lackie, K.; Najjar, G.; El-Awaisi, A.; Frost, J.; Green, C.; Langlois, S.; Lising, D.; Pfeifle, A.L.; Ward, H.; Xyrichis, A.; et al. Interprofessional education and collaborative practice research during the COVID-19 pandemic: Considerations to advance the field. J. Interprofessional Care 2020, 34, 583–586. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. Statement on Consumer and Community Involvement in Health and Medical Research; National Health and Medical Research Council: Canberra, Australia, 2016.
- National Institute for Health and Care Research. It’s Time for Patients, Service Users and the Public to Lead Development of New Research Ideas. Available online: https://www.nihr.ac.uk/blog/its-time-for-patients-service-users-and-the-public-to-lead-development-of-new-research-ideas/29669 (accessed on 8 November 2022).
- Tricco, A.C.; Langlois, E.V.; Straus, S.E. Rapid Reviews to Strengthen Health Policy and Systems: A Practical Guide; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Garritty, C.; Gartlehner, G.; Nussbaumer-Streit, B.; King, V.J.; Hamel, C.; Kamel, C.; Affengruber, L.; Stevens, A. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J. Clin. Epidemiol. 2021, 130, 13–22. [Google Scholar] [CrossRef]
- Khalili, H.; Thistlethwaite, J.; El-Awaisi, A.; Pfeifle, A.; Gilbert, J.; Lising, D.; MacMillan, K.; Maxwell, B.; Grymonpre, R.; Rodrigues, F.; et al. Guidance on Global Interprofessional Education and Collaborative Practice Research: Discussion Paper; A joint publication by InterprofessionalResearch.Global & Interprofessional.Global; 2019. Available online: https://interprofessional.global/wp-content/uploads/2019/10/Guidance-on-Global-Interprofessional-Education-and-Collaborative-Practice-Research_Discussion-Paper_FINAL-WEB.pdf (accessed on 9 November 2022).
- Law, M.; Stewart, D.; Pollock, N.; Letts, L.; Bosch, J.; Westmorland, M. Critical Review Form—Quantitative Studies; McMaster University: Hamilton, ON, Canada, 1998. [Google Scholar]
- Letts, L.; Wilkins, S.; Law, M.; Stewart, D.; Bosch, J.; Westmorland, M. Critical Review Form—Qualitative Studies (Version 2.0); McMaster University: Hamilton, ON, Canada, 2007. [Google Scholar]
- Hong, Q.N.; Gonzalez-Reyes, A.; Pluye, P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J. Eval. Clin. Pract. 2018, 24, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme. Available online: https://www.lancaster.ac.uk/media/lancaster-university/contentassets/documents/fhm/dhr/chir/NSsynthesisguidance Version1-April2006.pdf (accessed on 9 November 2022).
- Metersky, K.; Orchard, C.; Adams, T.; Hurlock-Chorostecki, C. Patient roles in primary care interprofessional teams: A constructivist grounded theory of patient and health care provider perspectives. J. Interprofessional Care 2021, 36, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Valaitis, R.; Longaphy, J.; Ploeg, J.; Agarwal, G.; Oliver, D.; Nair, K.; Kastner, M.; Avilla, E.; Dolovich, L. Health TAPESTRY: Co-designing interprofessional primary care programs for older adults using the persona-scenario method. BMC Fam. Pract. 2019, 20, 122. [Google Scholar] [CrossRef] [PubMed]
- Worswick, L.; Little, C.; Ryan, K.; Carr, E. Interprofessional learning in primary care: An exploration of the service user experience leads to a new model for co-learning. Nurse Educ. Today 2015, 35, 283–287. [Google Scholar] [CrossRef] [PubMed]
- van Dongen, J.J.J.; de Wit, M.; Smeets, H.W.H.; Stoffers, E.; van Bokhoven, M.A.; Daniëls, R. “They are talking about me, but not with me”: A focus group study to explore the patient perspective on interprofessional team meetings in primary care. Patient 2017, 10, 429–438. [Google Scholar] [CrossRef]
- van Dongen, J.J.J.; Habets, I.G.J.; Beurskens, A.; van Bokhoven, M.A. Successful participation of patients in interprofessional team meetings: A qualitative study. Health Expect. 2017, 20, 724–733. [Google Scholar] [CrossRef]
- Molenaar, J.; Korstjens, I.; Hendrix, M.; de Vries, R.; Nieuwenhuijze, M. Needs of parents and professionals to improve shared decision-making in interprofessional maternity care practice: A qualitative study. Birth 2018, 45, 245–254. [Google Scholar] [CrossRef]
- Körner, M.; Ehrhardt, H.; Steger, A.-K. Designing an interprofessional training program for shared decision making. J. Interprofessional Care 2013, 27, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Koerner, M.; Wirtz, M.; Michaelis, M.; Ehrhardt, H.; Steger, A.-K.; Zerpies, E.; Bengel, J. A multicentre cluster-randomized controlled study to evaluate a train-the-trainer programme for implementing internal and external participation in medical rehabilitation. Clin. Rehabil. 2014, 28, 20–35. [Google Scholar] [CrossRef]
- Carr, E.C.; Worswick, L.; Wilcock, P.M.; Campion-Smith, C.; Hettinga, D. Improving services for back pain: Putting the patient at the centre of interprofessional education. Qual. Prim. Care 2012, 20, 345–353. [Google Scholar]
- Sitzia, J.; Cotterell, P.; Richardson, A. Interprofessional collaboration with service users in the development of cancer services: The Cancer Partnership Project. J. Interprofessional Care 2006, 20, 60–74. [Google Scholar] [CrossRef]
- Phillips, R.L.; Short, A.; Kenning, A.; Dugdale, P.; Nugus, P.; McGowan, R.; Greenfield, D. Achieving patient-centred care: The potential and challenge of the patient-as-professional role. Health Expect. 2015, 18, 2616–2628. [Google Scholar] [CrossRef]
- Sæbjørnsen, S.E.N.; Willumsen, E. Service user participation in interprofessional teams in child welfare in Norway: Vulnerable adolescents’ perceptions. Child Fam. Soc. Work. 2015, 22, 43–53. [Google Scholar] [CrossRef]
- Bolin, A. Children’s agency in interprofessional collaborative meetings in child welfare work. Child Fam. Soc. Work. 2014, 21, 502–511. [Google Scholar] [CrossRef]
- Schoeb, V.; Staffoni, L.; Keel, S. Influence of interactional structure on patient’s participation during interprofessional discharge planning meetings in rehabilitation centers. J. Interprofessional Care 2019, 33, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Tjia, J.; Clayton, M.; Chiriboga, G.; Staples, B.; Puerto, G.; Rappaport, L.; DeSanto-Madeya, S. Stakeholder-engaged process for refining the design of a clinical trial in home hospice. BMC Med. Res. Methodol. 2021, 21, 92. [Google Scholar] [CrossRef]
- Reeves, S.; McMillan, S.E.; Kachan, N.; Paradis, E.; Leslie, M.; Kitto, S. Interprofessional collaboration and family member involvement in intensive care units: Emerging themes from a multi-sited ethnography. J. Interprofessional Care 2015, 29, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Cancer Australia; Cancer Voices Australia. National Framework for Consumer Involvement in Cancer Control; Cancer Australia: Canberra, Australia, 2011.
- Olweny, C. The ethics and conduct of cross-cultural research in developing countries. Psycho-Oncol. 1994, 3, 11–20. [Google Scholar] [CrossRef]
- NSW Council of Social Service. Principles of Co-Design. Available online: https://www.ncoss.org.au/wp-content/uploads/2017/06/Codesign-principles.pdf (accessed on 11 August 2022).
- Kara, M.A. Applicability of the principle of respect for autonomy: The perspective of Turkey. Journal of Medical Ethics 2007, 33, 627. [Google Scholar] [CrossRef]
- Chalmers, I.; Glasziou, P. Avoidable waste in the production and reporting of research evidence. The Lancet 2009, 374, 86–89. [Google Scholar] [CrossRef]
- Glasziou, P.; Chalmers, I. Paul Glasziou and Iain Chalmers: Is 85% of health research really “wasted”? Available online: https://blogs.bmj.com/bmj/2016/01/14/paul-glasziou-and-iain-chalmers-is-85-of-health-research-really-wasted/ (accessed on 14 September 2022).
- Abayneh, S.; Lempp, H.; Hanlon, C. Participatory action research to pilot a model of mental health service user involvement in an Ethiopian rural primary healthcare setting: Study protocol. Research Involvement and Engagement 2020, 6, 2. [Google Scholar] [CrossRef]
- Hutchinson, A.; Lovell, A. Participatory action research: Moving beyond the mental health ‘service user’ identity. Journal of Psychiatric and Mental Health Nursing 2013, 20, 641–649. [Google Scholar] [CrossRef]
- Bigby, C.; Frawley, P.; Ramcharan, P. Conceptualizing inclusive research with people with intellectual disability. Journal of Applied Research in Intellectual Disabilities 2014, 27, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Chambers, E.; Gardiner, C.; Thompson, J.; Seymour, J. Patient and carer involvement in palliative care research: An integrative qualitative evidence synthesis review. Palliative Medicine 2019, 33, 969–984. [Google Scholar] [CrossRef] [PubMed]
- DeCamp, M.; Alasmar, A.; Fischer, S.; Kutner, J.S. Meeting ethical challenges with authenticity when engaging patients and families in end-of-life and palliative care research: A qualitative study. BMC Palliative Care 2022, 21, 74. [Google Scholar] [CrossRef] [PubMed]
- Lawson, W.B.; Carrington, S. Inclusive research practice: Engaging autistic individuals and their families in research. In Research Approaches to Supporting Students on the Autism Spectrum in Inclusive Schools: Outcomes, Challenges, and Impact; Carrington, S., Saggers, B., Harper-Hill, K., Whelan, M., Eds.; Routledge: Oxford, UK, 2021; pp. 17–31. [Google Scholar]
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population | Patients or service users who have received a healthcare service from a healthcare worker and/or their carer/s who have participated in an IPECP initiative with a healthcare worker | Patients or service users who were not involved in an IPECP initiative with a healthcare worker |
| Intervention or investigated phenomena | IPECP initiatives for entry-level and practicing professionals that involve healthcare workers from at least two professions working together with service user/s | Education, research, and practice activities that are labelled as multidisciplinary, interdisciplinary, or transdisciplinary |
| Comparator | No comparator | No comparator |
| Outcome | Description of the involvement of service users in the IPECP initiatives | Outcomes that are not attributed to the involvement of service users |
| Research designs | Primary research: quantitative, qualitative, and mixed methods designs | Secondary research (i.e., reviews), conference abstracts/posters, study protocols, editorials/commentaries, position papers |
| Other | English-language literature published from 2006 onwards | Unpublished literature (e.g., grey literature, theses, and dissertation manuscripts) |
| No. | Author/s and Year | Design | Country | Participants | Measures | Setting | |
|---|---|---|---|---|---|---|---|
| Professionals | Service Users | ||||||
| 1 | Bolin, 2014 [44] | Qualitative | Sweden | Social workers and professionals in child psychiatry | Children receiving social services (n = 28) | Attendance in collaborative meetings | Practice |
| 2 | Carr et al., 2012 [40] | Qualitative | United Kingdom | General practitioners, nurses, physiotherapists, and managers (n = 44) | Clients with back pain (n = 11) | Participation in workshops for quality | Education |
| 3 | Koerner et al., 2014 [39] | Quantitative | Germany | Physicians, nursing staff, physical therapists, sport teachers, masseurs, psychologists and other psychosocial therapists, dietitians, and social workers | Clients with chronic disease | Participation on a survey for a training program evaluation | Practice |
| 4 | Körner et al., 2013 [38] | Mixed methods | Germany | Physicians, nursing staff, physical therapists, sport teachers, masseurs, psychologists and other psychosocial therapists, dietitians, and social workers (n = 32) | Rehabilitation clients (n = 36) | Involvement in focus group discussions in developing a training program for health professionals | Practice |
| 5 | Metersky et al., 2021 [32] | Qualitative | Canada | Nurses, social workers, dietitians, pharmacists, a nurse practitioner, and a respiratory therapist (n = 10) | Clients with chronic disease diagnosis (n = 10) | Participation in group interviews for designing interprofessional teams | Practice/research |
| 6 | Molenaar et al., 2018 [37] | Qualitative | Netherlands | Primary care midwives, hospital-based midwives, obstetricians, obstetric nurses, and maternity care assistants | Pregnant women and their partners (n = 71) | Involvement in co-creating a shared decision-making model | Practice |
| 7 | Phillips et al., 2015 [42] | Qualitative | Australia | Nurses, physiotherapists, exercise physiologists, fitness instructors, social workers, and general practitioners (n = 14) | Clients with chronic disease and their carers (n = 55) | Participation in interviews to describe ‘patient as professional’ role | Practice |
| 8 | Reeves et al., 2015 [47] | Qualitative | USA and Canada | Nurses, doctors, pharmacists, and social workers | Clients from the intensive care unit | Involvement of family members in co-designing the treatment plan | Practice/education |
| 9 | Sæbjørnsen & Willumsen, 2015 [43] | Qualitative | Norway | Social workers, childcare specialists, and therapists | Children receiving social welfare services | Participation in children conferences | Practice |
| 10 | Schoeb et al., 2019 [45] | Qualitative | Switzerland | Doctors, nurses, physiotherapists, occupational therapists, social workers, psychologists, speech therapists, dieticians, and work rehabilitation staff | Clients with various conditions (n = 25) | Participation in interprofessional meetings for discharge planning | Practice |
| 11 | Sitzia et al., 2006 [41] | Qualitative | United Kingdom | Nurses, doctors, administrators, and managers | Clients with cancer (n = 59) | Involvement in project evaluation through interviews | Practice |
| 12 | Tjia et al., 2021 [46] | Qualitative | USA | Hospice administrator, nurses, physicians, pharmacists (n = 8) | Former family caregivers (n = 10) | Involvement in stakeholder panel meetings | Practice |
| 13 | Valaitis et al., 2019 [33] | Qualitative | Canada | Healthcare providers/community care providers (n = 29), community service providers (n = 12), volunteers (n = 14) | Clients with complex and chronic conditions (n = 70) | Involvement in designing a primary care service | Practice |
| 14 | van Dongen et al., 2017 [36] | Qualitative | Netherlands | Healthcare professionals (n = 8) | Clients with chronic conditions and their relatives (n = 11) | Participation in interprofessional meetings | Practice |
| 15 | Van Dongen et al., 2017 [35] | Qualitative | Netherlands | Family medicine and occupational therapist | Clients with chronic conditions (n = 7) | Participation in interprofessional team meetings | Practice/research |
| 16 | Worswick et al., 2015 [34] | Qualitative | Canada | Primary healthcare professionals | Clients with back pain (n = 11) | Participation in workshops | Practice/education |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sy, M.P.; Panotes, A.; Cho, D.; Pineda, R.C.; Martin, P. A Rapid Review of the Factors That Influence Service User Involvement in Interprofessional Education, Practice, and Research. Int. J. Environ. Res. Public Health 2022, 19, 16826. https://doi.org/10.3390/ijerph192416826
Sy MP, Panotes A, Cho D, Pineda RC, Martin P. A Rapid Review of the Factors That Influence Service User Involvement in Interprofessional Education, Practice, and Research. International Journal of Environmental Research and Public Health. 2022; 19(24):16826. https://doi.org/10.3390/ijerph192416826
Chicago/Turabian StyleSy, Michael Palapal, Arden Panotes, Daniella Cho, Roi Charles Pineda, and Priya Martin. 2022. "A Rapid Review of the Factors That Influence Service User Involvement in Interprofessional Education, Practice, and Research" International Journal of Environmental Research and Public Health 19, no. 24: 16826. https://doi.org/10.3390/ijerph192416826
APA StyleSy, M. P., Panotes, A., Cho, D., Pineda, R. C., & Martin, P. (2022). A Rapid Review of the Factors That Influence Service User Involvement in Interprofessional Education, Practice, and Research. International Journal of Environmental Research and Public Health, 19(24), 16826. https://doi.org/10.3390/ijerph192416826






