Patterns and Determinants of Multimorbidity in Older Adults: Study in Health-Ecological Perspective
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Variables
2.2.1. Outcome Variable
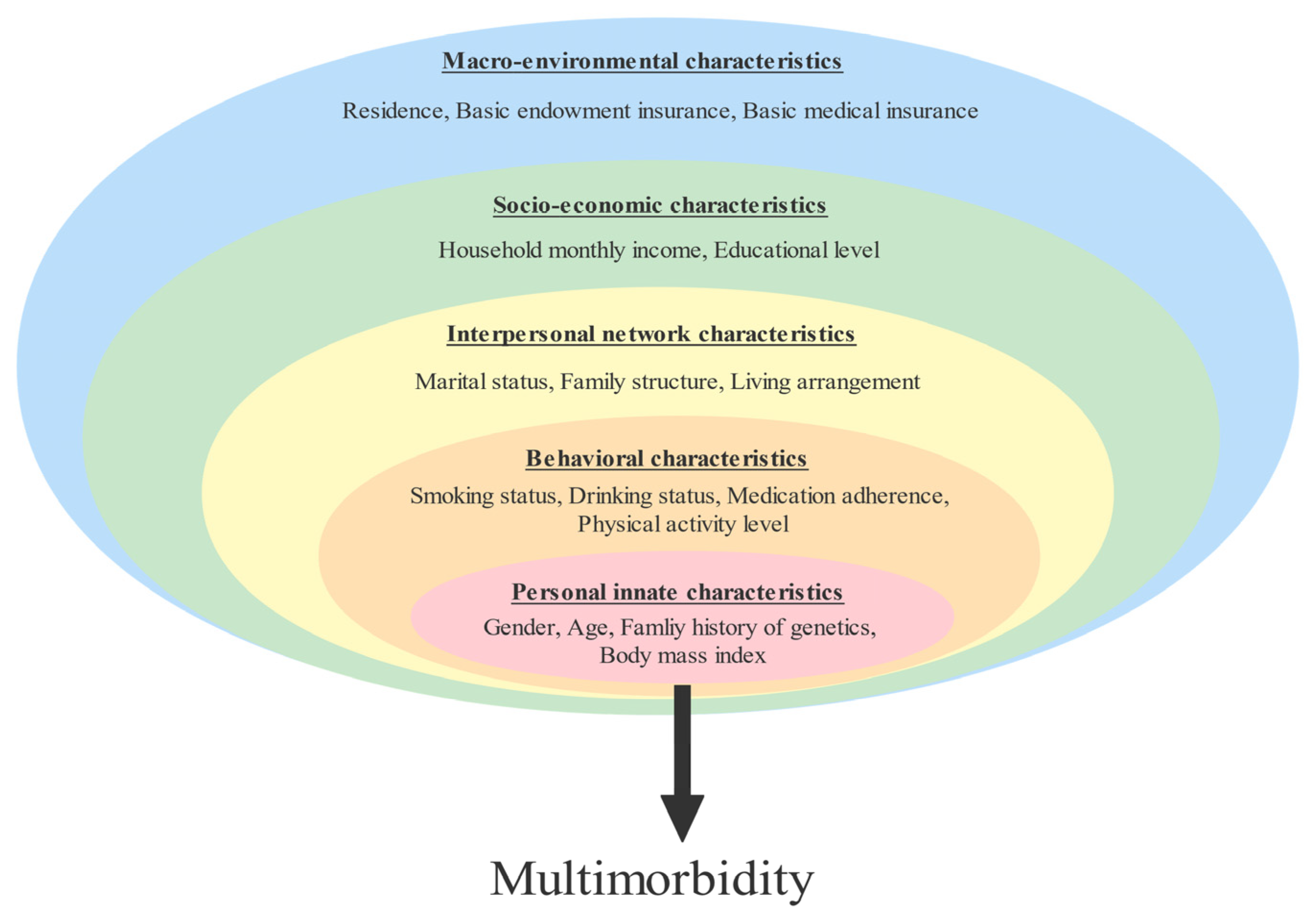
2.2.2. Independent Variable
2.3. Statistical Analysis
3. Results
3.1. The Prevalence of Chronic Disease and Multimorbidity in the Elderly
3.2. Patterns of Multimorbidity
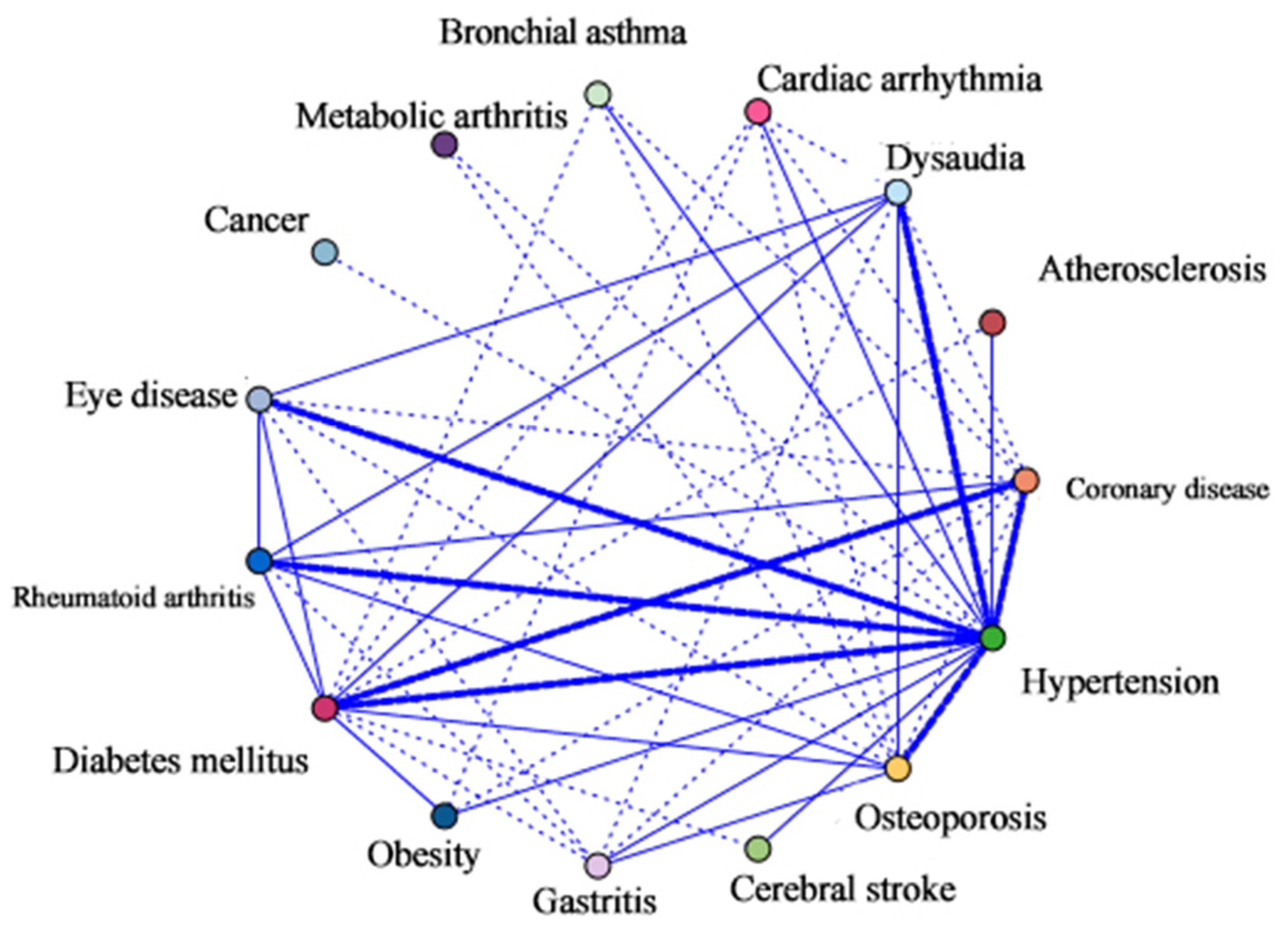
3.2.1. Network Analysis
3.2.2. Association Rules Mining Analysis
3.3. Univariate Analysis of Factors Underlying Multimorbidity
3.4. Hierarchical Multiple Logistic Regression Results
4. Discussion
4.1. Suggestions
4.2. Implications and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| HTN | Hypertension |
| DM | Diabetes mellitus |
| CAD | Coronary artery disease |
References
- Ofori-Asenso, R.; Chin, K.L.; Curtis, A.J.; Zomer, E.; Zoungas, S.; Liew, D. Recent Patterns of Multimorbidity Among Older Adults in High-Income Countries. Popul. Health Manag. 2019, 22, 127–137. [Google Scholar] [CrossRef]
- Zhao, Y.; Atun, R.; Oldenburg, B.; McPake, B.; Tang, S.; Mercer, S.W.; Cowling, T.E.; Sum, G.; Qin, V.M.; Lee, J.T. Physical Multimorbidity, Health Service Use, and Catastrophic Health Expenditure by Socioeconomic Groups in China: An Analysis of Population-Based Panel Data. Lancet Glob. Health 2020, 8, e840–e849. [Google Scholar] [CrossRef]
- National Bureau of Statistics Seventh National Census Bulletin (No. 5). Available online: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/202106/t20210628_1818824.html (accessed on 15 October 2022).
- Zhao, Y.W.; Haregu, T.N.; He, L.; Lu, S.; Katar, A.; Wang, H.; Yao, Z.; Zhang, L. The Effect of Multimorbidity on Functional Limitations and Depression amongst Middle-Aged and Older Population in China: A Nationwide Longitudinal Study. Age Ageing 2021, 50, 190–197. [Google Scholar] [CrossRef]
- Yoon, J.; Zulman, D.; Scott, J.Y.; Maciejewski, M.L. Costs Associated with Multimorbidity among VA Patients. Med. Care 2014, 52 (Suppl. S3), S31–S36. [Google Scholar] [CrossRef]
- Jankovic, J.; Mirkovic, M.; Jovic-Vranes, A.; Santric-Milicevic, M.; Terzic-Supic, Z. Association between Non-Communicable Disease Multimorbidity and Health Care Utilization in a Middle-Income Country: Population-Based Study. Public Health 2018, 155, 35–42. [Google Scholar] [CrossRef]
- Zhang, C.; Xiao, S.; Shi, L.; Xue, Y.; Zheng, X.; Dong, F.; Zhang, J.; Xue, B.; Lin, H.; Ouyang, P. Urban-Rural Differences in Patterns and Associated Factors of Multimorbidity Among Older Adults in China: A Cross-Sectional Study Based on Apriori Algorithm and Multinomial Logistic Regression. Front. Public Health 2021, 9, 707062. [Google Scholar] [CrossRef]
- Pearson-Stuttard, J.; Ezzati, M.; Gregg, E.W. Multimorbidity-a Defining Challenge for Health Systems. Lancet Public Health 2019, 4, e599–e600. [Google Scholar] [CrossRef]
- van den Akker, M.; Buntinx, F.; Metsemakers, J.F.; Roos, S.; Knottnerus, J.A. Multimorbidity in General Practice: Prevalence, Incidence, and Determinants of Co-Occurring Chronic and Recurrent Diseases. J. Clin. Epidemiol. 1998, 51, 367–375. [Google Scholar] [CrossRef]
- Garin, N.; Koyanagi, A.; Chatterji, S.; Tyrovolas, S.; Olaya, B.; Leonardi, M.; Lara, E.; Koskinen, S.; Tobiasz-Adamczyk, B.; Ayuso-Mateos, J.L.; et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2016, 71, 205–214. [Google Scholar] [CrossRef]
- Yao, S.-S.; Cao, G.-Y.; Han, L.; Chen, Z.-S.; Huang, Z.-T.; Gong, P.; Hu, Y.; Xu, B. Prevalence and Patterns of Multimorbidity in a Nationally Representative Sample of Older Chinese: Results From the China Health and Retirement Longitudinal Study. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 1974–1980. [Google Scholar] [CrossRef]
- Gu, J.; Chao, J.; Chen, W.; Xu, H.; Wu, Z.; Chen, H.; He, T.; Deng, L.; Zhang, R. Multimorbidity in the Community-Dwelling Elderly in Urban China. Arch. Gerontol. Geriatr. 2017, 68, 62–67. [Google Scholar] [CrossRef]
- Violan, C.; Foguet-Boreu, Q.; Flores-Mateo, G.; Salisbury, C.; Blom, J.; Freitag, M.; Glynn, L.; Muth, C.; Valderas, J.M. Prevalence, Determinants and Patterns of Multimorbidity in Primary Care: A Systematic Review of Observational Studies. PLoS ONE 2014, 9, e102149. [Google Scholar] [CrossRef]
- Quiñones, A.R.; Valenzuela, S.H.; Huguet, N.; Ukhanova, M.; Marino, M.; Lucas, J.A.; O’Malley, J.; Schmidt, T.D.; Voss, R.; Peak, K.; et al. Prevalent Multimorbidity Combinations Among Middle-Aged and Older Adults Seen in Community Health Centers. J. Gen. Intern. Med. 2022, 37, 3545–3553. [Google Scholar] [CrossRef]
- Wang, S.B.; D’Arcy, C.; Yu, Y.Q.; Li, B.; Liu, Y.W.; Tao, Y.C.; Wu, Y.H.; Zhang, Q.Q.; Xu, Z.Q.; Fu, Y.L.; et al. Prevalence and Patterns of Multimorbidity in Northeastern China: A Cross-Sectional Study. Public Health 2015, 129, 1539–1546. [Google Scholar] [CrossRef]
- Hunter, M.L.; Knuiman, M.W.; Musk, B.A.W.; Hui, J.; Murray, K.; Beilby, J.P.; Hillman, D.R.; Hung, J.; Newton, R.U.; Bucks, R.S.; et al. Prevalence and Patterns of Multimorbidity in Australian Baby Boomers: The Busselton Healthy Ageing Study. BMC Public Health 2021, 21, 1539. [Google Scholar] [CrossRef]
- Zacarias-Pons, L.; Vilalta-Franch, J.; Turro-Garriga, O.; Saez, M.; Garre-Olmo, J. Multimorbidity Patterns and Their Related Characteristics in European Older Adults: A Longitudinal Perspective. Arch. Gerontol. Geriatr. 2021, 95, 104428. [Google Scholar] [CrossRef]
- Kivimäki, M.; Strandberg, T.; Pentti, J.; Nyberg, S.T.; Frank, P.; Jokela, M.; Ervasti, J.; Suominen, S.B.; Vahtera, J.; Sipilä, P.N.; et al. Body-Mass Index and Risk of Obesity-Related Complex Multimorbidity: An Observational Multicohort Study. Lancet Diabetes Endocrinol. 2022, 10, 253–263. [Google Scholar] [CrossRef]
- Chudasama, Y.V.; Khunti, K.; Gillies, C.L.; Dhalwani, N.N.; Davies, M.J.; Yates, T.; Zaccardi, F. Healthy Lifestyle and Life Expectancy in People with Multimorbidity in the UK Biobank: A Longitudinal Cohort Study. PLoS Med. 2020, 17, e1003332. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of Multimorbidity and Implications for Health Care, Research, and Medical Education: A Cross-Sectional Study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Ingram, E.; Ledden, S.; Beardon, S.; Gomes, M.; Hogarth, S.; McDonald, H.; Osborn, D.P.; Sheringham, J. Household and Area-Level Social Determinants of Multimorbidity: A Systematic Review. J. Epidemiol. Community Health 2021, 75, 232–241. [Google Scholar] [CrossRef]
- Craig, L.S.; Cunningham-Myrie, C.A.; Hotchkiss, D.R.; Hernandez, J.H.; Gustat, J.; Theall, K.P. Social Determinants of Multimorbidity in Jamaica: Application of Latent Class Analysis in a Cross-Sectional Study. BMC Public Health 2021, 21, 1197. [Google Scholar] [CrossRef]
- Kamara, R.F.; Saunders, M.J.; Sahr, F.; Losa-Garcia, J.E.; Foray, L.; Davies, G.; Wingfield, T. Social and Health Factors Associated with Adverse Treatment Outcomes among People with Multidrug-Resistant Tuberculosis in Sierra Leone: A National, Retrospective Cohort Study. Lancet Glob. Health 2022, 10, e543–e554. [Google Scholar] [CrossRef]
- Poblador-Plou, B.; van den Akker, M.; Vos, R.; Calderón-Larrañaga, A.; Metsemakers, J.; Prados-Torres, A. Similar Multimorbidity Patterns in Primary Care Patients from Two European Regions: Results of a Factor Analysis. PLoS ONE 2014, 9, e100375. [Google Scholar] [CrossRef][Green Version]
- Vennu, V.; Abdulrahman, T.A.; Alenazi, A.M.; Bindawas, S.M. Associations between Social Determinants and the Presence of Chronic Diseases: Data from the Osteoarthritis Initiative. BMC Public Health 2020, 20, 1323. [Google Scholar] [CrossRef]
- Fisher, K.A.; Griffith, L.E.; Gruneir, A.; Upshur, R.; Perez, R.; Favotto, L.; Nguyen, F.; Markle-Reid, M.; Ploeg, J. Effect of Socio-Demographic and Health Factors on the Association between Multimorbidity and Acute Care Service Use: Population-Based Survey Linked to Health Administrative Data. BMC Health Serv. Res. 2021, 21, 62. [Google Scholar] [CrossRef]
- Lu, J.; Wang, Y.; Hou, L.; Zuo, Z.; Zhang, N.; Wei, A. Multimorbidity Patterns in Old Adults and Their Associated Multi-Layered Factors: A Cross-Sectional Study. BMC Geriatr. 2021, 21, 372. [Google Scholar] [CrossRef]
- Frohlich, K.L.; Corin, E.; Potvin, L. A Theoretical Proposal for the Relationship between Context and Disease. Sociol. Health Illn. 2001, 23, 776–797. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Toward an Experimental Ecology of Human Development. Am. Psychol. 1977, 32, 513–531. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Mahmudiono, T.; Segalita, C.; Rosenkranz, R.R. Socio-Ecological Model of Correlates of Double Burden of Malnutrition in Developing Countries: A Narrative Review. Int. J. Environ. Res. Public Health 2019, 16, 3730. [Google Scholar] [CrossRef]
- Chang, H.; Huang, Y.; Liu, X. Loneliness Status and Related Factors among the Hakka Elderly in Fujian, China: Based on the Health Ecological Model. J. Environ. Public Health 2022, 2022, 2633297. [Google Scholar] [CrossRef]
- Sun, Y.; Ma, Y.; Cao, M.; Hu, Z.; Lin, W.; Chen, M.; He, Y. Breast and Cervical Cancer Screening Adherence in Jiangsu, China: An Ecological Perspective. Front. Public Health 2022, 10, 967495. [Google Scholar] [CrossRef]
- Reifsnider, E.; Gallagher, M.; Forgione, B. Using Ecological Models in Research on Health Disparities. J. Prof. Nurs. 2005, 21, 216–222. [Google Scholar] [CrossRef]
- Chua, Y.P.; Xie, Y.; Lee, P.S.S.; Lee, E.S. Definitions and Prevalence of Multimorbidity in Large Database Studies: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 1673. [Google Scholar] [CrossRef]
- Fortin, M.; Stewart, M.; Poitras, M.-E.; Almirall, J.; Maddocks, H. A Systematic Review of Prevalence Studies on Multimorbidity: Toward a More Uniform Methodology. Ann. Fam. Med. 2012, 10, 142–151. [Google Scholar] [CrossRef]
- Sakib, M.N.; Shooshtari, S.; St John, P.; Menec, V. The Prevalence of Multimorbidity and Associations with Lifestyle Factors among Middle-Aged Canadians: An Analysis of Canadian Longitudinal Study on Aging Data. BMC Public Health 2019, 19, 243. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, Morbidity, and Risk Factors in China and Its Provinces, 1990-2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- Hsieh, P.-C.; Cheng, C.-F.; Wu, C.-W.; Tzeng, I.-S.; Kuo, C.-Y.; Hsu, P.-S.; Lee, C.-T.; Yu, M.-C.; Lan, C.-C. Combination of Acupoints in Treating Patients with Chronic Obstructive Pulmonary Disease: An Apriori Algorithm-Based Association Rule Analysis. Evid. Based Complement. Alternat. Med. 2020, 2020, 8165296. [Google Scholar] [CrossRef]
- Zemedikun, D.T.; Gray, L.J.; Khunti, K.; Davies, M.J.; Dhalwani, N.N. Patterns of Multimorbidity in Middle-Aged and Older Adults: An Analysis of the UK Biobank Data. Mayo Clin. Proc. 2018, 93, 857–866. [Google Scholar] [CrossRef]
- Dhungana, R.R.; Karki, K.B.; Bista, B.; Pandey, A.R.; Dhimal, M.; Maskey, M.K. Prevalence, Pattern and Determinants of Chronic Disease Multimorbidity in Nepal: Secondary Analysis of a National Survey. BMJ Open 2021, 11, e047665. [Google Scholar] [CrossRef]
- Hu, F.; Xu, L.; Zhou, J.; Zhang, J.; Gao, Z.; Hong, Z. Association between Overweight, Obesity and the Prevalence of Multimorbidity among the Elderly: Evidence from a Cross-Sectional Analysis in Shandong, China. Int. J. Environ. Res. Public Health 2020, 17, 8355. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [CrossRef]
- Gao, Y.; Ping, Z.; Pei, X.; Cai, Y.; Wang, J. Multi-correspondence analysis of the status and related factors of chronic diseases multimorbidity in middle-aged and elderly people in China in 2009. J. Hyg. Res. 2020, 49, 844–849. [Google Scholar]
- Zhang, C.; Cai, Y.; Xue, Y.; Zheng, X.; Yang, X.; Lu, J.; Hou, L.; Li, M. Exploring the Influencing Factors of Quality of Life among the Empty Nesters in Shanxi, China: A Structural Equation Model. Health Qual Life Outcomes 2021, 19, 156. [Google Scholar] [CrossRef]
- Pang, Y.; Yu, C.; Guo, Y.; Lyu, J.; Li, L. Associations of lifestyles with major chronic diseases in Chinese adults: Evidence from the China Kadoorie Biobank. Chin. J. Epidemiol. 2021, 42, 369–375. [Google Scholar]
- Vogeli, C.; Shields, A.E.; Lee, T.A.; Gibson, T.B.; Marder, W.D.; Weiss, K.B.; Blumenthal, D. Multiple Chronic Conditions: Prevalence, Health Consequences, and Implications for Quality, Care Management, and Costs. J. Gen. Intern. Med. 2007, 22 (Suppl. S3), 391–395. [Google Scholar] [CrossRef]
- Castro, J.P.; El-Atat, F.A.; McFarlane, S.I.; Aneja, A.; Sowers, J.R. Cardiometabolic Syndrome: Pathophysiology and Treatment. Curr. Hypertens. Rep. 2003, 5, 393–401. [Google Scholar] [CrossRef]
- Kovacic, J.C.; Castellano, J.M.; Fuster, V. The Links between Complex Coronary Disease, Cerebrovascular Disease, and Degenerative Brain Disease. In Evolving Challenges in Promoting Cardiovascular Health; Blackwell Science Publ: Oxford, UK, 2012; Volume 1254, pp. 99–105. ISBN 978-1-57331-859-4. [Google Scholar]
- Ho, H.-E.; Yeh, C.-J.; Wei, J.C.-C.; Chu, W.-M.; Lee, M.-C. Trends of Multimorbidity Patterns over 16 Years in Older Taiwanese People and Their Relationship to Mortality. Int. J. Environ. Res. Public Health 2022, 19, 3317. [Google Scholar] [CrossRef]
- Bayes-Marin, I.; Sanchez-Niubo, A.; Egea-Cortés, L.; Nguyen, H.; Prina, M.; Fernández, D.; Haro, J.M.; Olaya, B. Multimorbidity Patterns in Low-Middle and High Income Regions: A Multiregion Latent Class Analysis Using ATHLOS Harmonised Cohorts. BMJ Open 2020, 10, e034441. [Google Scholar] [CrossRef]
- Hien, H.; Berthé, A.; Drabo, M.K.; Meda, N.; Konaté, B.; Tou, F.; Badini-Kinda, F.; Macq, J. Prevalence and Patterns of Multimorbidity among the Elderly in Burkina Faso: Cross-Sectional Study. Trop. Med. Int. Health 2014, 19, 1328–1333. [Google Scholar] [CrossRef]
- Agrawal, S.; Agrawal, P. Association Between Body Mass Index and Prevalence of Multimorbidity in Low-and Middle-Income Countries: A Cross-Sectional Study. Int. J. Med. Public Health 2016, 6, 73. [Google Scholar] [CrossRef] [PubMed]
- Agborsangaya, C.; Ngwakongnwi, E.; Lahtinen, M.; Cooke, T.; Johnson, J.A. Multimorbidity Prevalence in the General Population: The Role of Obesity in Chronic Disease Clustering. BMC Public Health 2013, 13, 1161. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.-S.; Meng, X.; Cao, G.-Y.; Huang, Z.-T.; Chen, Z.-S.; Han, L.; Wang, K.; Su, H.-X.; Luo, Y.; Hu, Y.; et al. Associations between Multimorbidity and Physical Performance in Older Chinese Adults. Int. J. Environ. Res. Public Health 2020, 17, 4546. [Google Scholar] [CrossRef] [PubMed]
- Félix, I.B.; Henriques, A. Medication Adherence and Related Determinants in Older People with Multimorbidity: A Cross-Sectional Study. Nurs. Forum 2021, 56, 834–843. [Google Scholar] [CrossRef] [PubMed]
- Stafford, G.; Villén, N.; Roso-Llorach, A.; Troncoso-Mariño, A.; Monteagudo, M.; Violán, C. Combined Multimorbidity and Polypharmacy Patterns in the Elderly: A Cross-Sectional Study in Primary Health Care. Int. J. Environ. Res. Public Health 2021, 18, 9216. [Google Scholar] [CrossRef] [PubMed]
- Domino, M.E.; Beadles, C.A.; Lichstein, J.C.; Farley, J.F.; Morrissey, J.P.; Ellis, A.R.; Dubard, C.A. Heterogeneity in the Quality of Care for Patients With Multiple Chronic Conditions by Psychiatric Comorbidity. Med. Care 2014, 52, S101–S109. [Google Scholar] [CrossRef]
- Autenrieth, C.S.; Kirchberger, I.; Heier, M.; Zimmermann, A.-K.; Peters, A.; Döring, A.; Thorand, B. Physical Activity Is Inversely Associated with Multimorbidity in Elderly Men: Results from the KORA-Age Augsburg Study. Prev. Med. 2013, 57, 17–19. [Google Scholar] [CrossRef]
- Delpino, F.M.; de Lima, A.P.M.; da Silva, B.G.C.; Nunes, B.P.; Caputo, E.L.; Bielemann, R.M. Physical Activity and Multimorbidity Among Community-Dwelling Older Adults: A Systematic Review With Meta-Analysis. Am. J. Health Promot. 2022, 36, 1371–1385. [Google Scholar] [CrossRef]
- Wang, D.; Li, D.; Mishra, S.R.; Lim, C.; Dai, X.; Chen, S.; Xu, X. Association between Marital Relationship and Multimorbidity in Middle-Aged Adults: A Longitudinal Study across the US, UK, Europe, and China. Maturitas 2022, 155, 32–39. [Google Scholar] [CrossRef]
- Xue, B.; Xue, Y.; Dong, F.; Zheng, X.; Shi, L.; Xiao, S.; Zhang, J.; Ou, W.; Wang, Q.; Zhang, C. The Impact of Socioeconomic Status and Sleep Quality on the Prevalence of Multimorbidity in Older Adults. Front. Public Health 2022, 10, 959700. [Google Scholar] [CrossRef]
- Eyowas, F.A.; Schneider, M.; Alemu, S.; Getahun, F.A. Multimorbidity of Chronic Non-Communicable Diseases: Burden, Care Provision and Outcomes over Time among Patients Attending Chronic Outpatient Medical Care in Bahir Dar, Ethiopia-a Mixed Methods Study Protocol. BMJ Open 2021, 11, e051107. [Google Scholar] [CrossRef] [PubMed]
| Chronic Disease | Number of Cases | Types of Chronic Diseases [N (%)] | Multimorbidity | |||
|---|---|---|---|---|---|---|
| N (%) | 1 | 2 | 3 | ≥4 | N (%) | |
| All participants | 3637(100.0) | 1742 (47.90) | 522 (14.35) | 167 (4.59) | 73 (2.01) | 762 (20.95) |
| HTN | 1409 (38.7) | 855 (60.7) | 377 (26.8) | 122 (8.7) | 55 (3.9) | 554 (39.3) |
| DM | 481 (13.2) | 213 (44.3) | 165 (34.3) | 70 (14.6) | 33 (6.9) | 268 (55.7) |
| Rheumatoid arthritis | 226 (6.2) | 99 (43.8) | 65 (28.8) | 37 (16.4) | 25 (11.1) | 127 (56.2) |
| CAD | 223 (6.1) | 87 (39.0) | 72 (32.3) | 42 (18.8) | 22 (9.9) | 136 (61.0) |
| Hearing impairment | 213 (5.9) | 86 (40.4) | 59 (27.7) | 44 (20.7) | 24 (11.3) | 127 (59.6) |
| Eye disease | 199 (5.5) | 72 (36.2) | 67 (33.7) | 36 (18.1) | 24 (12.1) | 127 (63.8) |
| Osteoporosis | 163 (4.5) | 57 (35.0) | 43 (26.4) | 34 (20.9) | 29 (17.8) | 106 (65.0) |
| Gastritis | 114 (3.1) | 51 (44.7) | 27 (23.7) | 22 (19.3) | 14 (12.3) | 63 (55.3) |
| Obesity | 102 (2.8) | 46 (45.1) | 30 (29.4) | 13 (12.7) | 13 (12.7) | 56 (54.9) |
| Bronchial asthma | 77 (2.1) | 33 (42.9) | 22 (28.6) | 10 (13.0) | 12 (15.6) | 44 (57.1) |
| Order | Consequent | Antecedent | Support (%) | Confidence (%) | Lift |
|---|---|---|---|---|---|
| 1 | HTN | DM | 13.23 | 41.79 | 1.08 |
| 2 | DM | CAD | 6.13 | 45.71 | 1.18 |
| 3 | DM | Eye disease | 5.47 | 36.18 | 0.93 |
| 4 | HTN | Osteoporosis | 4.48 | 38.65 | 1.00 |
| 5 | HTN | Digestive system disease | 3.13 | 23.68 | 0.61 |
| 6 | HTN | Obesity | 2.81 | 31.38 | 0.81 |
| 7 | DM | CAD, HTN | 2.81 | 24.51 | 1.85 |
| 8 | Osteoporosis | rheumatoid arthritis, HTN | 2.26 | 21.95 | 4.90 |
| 9 | rheumatoid arthritis | Osteoporosis, HTN | 1.73 | 28.57 | 4.60 |
| 10 | Hearing impairment | Osteoporosis, HTN | 1.73 | 20.54 | 1.56 |
| 11 | DM | Osteoporosis, HTN | 1.73 | 20.54 | 1.56 |
| 12 | HTN | Arrhythmia | 1.60 | 34.48 | 0.89 |
| Multimorbidity | |||||
|---|---|---|---|---|---|
| Characteristics | N (n = 3637) | Yes (n = 762) | No (n = 2875) | χ2 | p Value |
| Personal innate characteristics: | |||||
| Gender | 3.680 | 0.055 | |||
| Male | 1864 (51.3) | 367 (48.2) | 1497 (52.1) | ||
| Female | 1773 (48.7) | 395 (51.8) | 1378 (47.9) | ||
| Age | 22.831 | <0.001 | |||
| 60~ | 1816 (49.9) | 322 (42.3) | 1494 (52.0) | ||
| 70~ | 1315 (36.2) | 315 (41.3) | 1000 (34.8) | ||
| 80 and above | 506 (13.9) | 125 (16.4) | 381 (13.3) | ||
| Family history | 40.472 | <0.001 | |||
| Yes | 308 (8.5) | 108 (14.2) | 200 (7.0) | ||
| No | 3329 (91.5) | 654 (85.8) | 2675 (93.0) | ||
| BMI | 9.457 | 0.009 | |||
| Lean (<18.6) | 265 (7.3) | 53 (7.0) | 212 (7.4) | ||
| Normal (18.5–23.9) | 2060 (56.6) | 398 (52.2) | 1662 (57.8) | ||
| Overweight (≥24) | 1312 (36.1) | 311 (40.8) | 1001 (34.8) | ||
| Behavioral characteristics: | |||||
| Smoking status | 0.208 | 0.648 | |||
| Yes | 936 (25.7) | 201 (26.4) | 735 (25.6) | ||
| No | 2701 (74.3) | 561 (73.6) | 2140 (74.4) | ||
| Drinking status | 0.014 | 0.907 | |||
| Yes | 798 (21.9) | 166 (21.8) | 632 (22.0) | ||
| No | 2839 (78.1) | 596 (78.2) | 2243 (78.0) | ||
| Physical activity levels | 23.694 | <0.001 | |||
| Low | 896 (24.6) | 222 (29.1) | 674 (23.4) | ||
| Moderate | 1505 (41.4) | 335 (44.0) | 1170 (40.7) | ||
| High | 1236 (34.0) | 205 (26.9) | 1031 (35.9) | ||
| Medication adherence | 120.971 | <0.001 | |||
| Low | 1064 (29.3) | 331 (43.4) | 733 (25.5) | ||
| Moderate | 1932 (53.1) | 277 (36.4) | 1655 (57.6) | ||
| High | 641 (17.6) | 154 (20.2) | 487 (16.9) | ||
| Interpersonal network: | |||||
| Marital status | 22.831 | <0.001 | |||
| Married | 2901(79.8) | 566 (74.3) | 2335 (81.2) | ||
| Single | 105(2.9) | 20 (2.6) | 85 (3.0) | ||
| Divorced | 42(1.2) | 4 (0.5) | 38 (1.3) | ||
| Widowed | 589(16.2) | 172 (22.6) | 417 (14.5) | ||
| Family structure | 1.871 | 0.171 | |||
| Empty nest | 1748 (48.0) | 383 (50.3) | 1365 (47.5) | ||
| Non-empty nest | 1889 (51.9) | 379 (49.7) | 1510 (52.5) | ||
| Living arrangement | 1.999 | 0.157 | |||
| Living alone | 657 (18.1) | 151 (19.8) | 506 (17.6) | ||
| Living with others | 2980 (81.9) | 611 (80.2) | 2369 (82.4) | ||
| Socioeconomic characteristics: | |||||
| Monthly income | 15.170 | 0.001 | |||
| <1000 RMB | 582 (16. 0) | 154 (13.6) | 434 (15.1) | ||
| 1000~3000 RMB | 1666 (45.8) | 529 (46.7) | 1302 (45.3) | ||
| >3000 RMB | 1389 (38.1) | 250 (32.8) | 1139 (39.6) | ||
| Educational level | 41.573 | <0.001 | |||
| Elementary education and below | 1376 (37.8) | 365 (47.9) | 1011 (35.2) | ||
| Secondary education | 1791 (49.3) | 316 (41.5) | 1475 (51.3) | ||
| Higher education and above | 470 (12.9) | 81 (10.6) | 389 (13.5) | ||
| Macro-environmental characteristics: | |||||
| Residence | 29.772 | <0.001 | |||
| Urban | 2124(58.4) | 379 (49.7) | 1745 (60.7) | ||
| Rural | 1513(41.6) | 383 (50.3) | 1130 (39.3) | ||
| Basic endowment Insurance | 48.418 | <0.001 | |||
| Uninsured | 1250 (34.4) | 343 (45.0) | 907 (31.5) | ||
| Insured | 2387 (65.6) | 419 (55.0) | 1968 (68.5) | ||
| Basic medical insurance | 4.433 | 0.035 | |||
| Uninsured | 365 (10.0) | 92 (12.1) | 273 (9.5) | ||
| Insured | 3272 (90.0) | 670 (87.9) | 2602 (90.5) | ||
| Factors | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | OR (95% CI) | β | OR (95% CI) | β | OR (95% CI) | β | OR (95% CI) | β | OR (95% CI) | |
| Personal innate characteristics: | ||||||||||
| Age (Ref. 60–69) | ||||||||||
| 70–79 | 0.38 | 1.46 (1.22–1.74) *** | 0.37 | 1.45 (1.21–1.74) *** | 0.30 | 1.35 (1.13–1.63) ** | 0.32 | 1.38 (1.15–1.66) ** | 0.33 | 1.39 (1.15–1.68) *** |
| 80 and above | 0.45 | 1.56 (1.23–1.99) *** | 0.40 | 1.49 (1.17–1.91) ** | 0.27 | 1.32 (1.02–1.70) * | 0.31 | 1.36 (1.05–1.76) * | 0.34 | 1.41 (1.08–1.83) ** |
| Family history (Ref. No) | ||||||||||
| Yes | 0.80 | 2.22 (1.73–2.86) *** | 0.68 | 1.98 (1.53–2.56) *** | 0.72 | 2.05 (1.58–2.66) ** | 0.74 | 2.09 (1.61–2.71) *** | 0.75 | 2.11 (1.62–2.74) *** |
| BMI (Ref. Normal) | ||||||||||
| Lean | 0.02 | 1.02 (0.74–1.41) | −0.05 | 0.94 (0.67–1.31) | −0.08 | 0.91 (0.65–1.27) | −0.15 | 0.86 (0.62–1.21) | −0.20 | 0.82 (0.58–1.14) |
| Overweight | 0.23 | 1.26 (1.06–1.50) ** | 0.23 | 1.26 (1.06–1.49) ** | 0.23 | 1.26 (1.05–1.50) ** | 0.22 | 1.24 (1.04–1.48) * | 0.22 | 1.24 (1.04–1.48) * |
| Behavioral characteristics: | ||||||||||
| Physical activity levels (Ref. High) | ||||||||||
| Low | 0.43 | 1.54 (1.23–1.92) *** | 0.41 | 1.51 (1.21–1.89) *** | 0.38 | 1.46 (1.16–1.83) ** | 0.34 | 1.41 (1.12–1.78) ** | ||
| Moderate | 0.34 | 1.42 (1.16–1.73) ** | 0.32 | 1.38 (1.12–1.68) ** | 0.32 | 1.38 (1.13–1.68) ** | 0.29 | 1.34 (1.09–1.64) ** | ||
| Medication adherence (Ref. High) | ||||||||||
| Low | 0.35 | 1.42 (1.13–1.79) ** | 0.34 | 1.41 (1.12–1.78) ** | 0.29 | 1.34 (1.06–1.69) * | 0.28 | 1.32 (1.05–1.68) * | ||
| Moderate | −0.58 | 0.56 (0.45–0.69) *** | −0.58 | 0.55 (0.44–0.69) *** | −0.62 | 0.54 (0.43–0.68) *** | −0.62 | 0.54 (0.43–0.68) *** | ||
| Family and social network: | ||||||||||
| Marital status (Ref. Married) | ||||||||||
| Unmarried | −0.09 | 0.91 (0.54–1.55) | −0.11 | 0.89 (0.53–1.54) | −0.09 | 0.91 (0.53–1.55) | ||||
| Divorced | −0.87 | 0.42 (0.15–1.21) | −0.87 | 0.42 (0.15–1.21) | −0.84 | 0.43 (0.15–1.25) | ||||
| Widowed | 0.43 | 1.54 (1.23–1.93) *** | 0.35 | 1.42 (1.12–1.78) ** | 0.35 | 1.42 (1.13–1.79) ** | ||||
| Living arrangement (Ref. Living with others) | ||||||||||
| Living alone | −0.01 | 0.99 (0.79–1.24) | −0.05 | 0.95 (0.76–1.19) | −0.05 | 0.95 (0.76–1.19) | ||||
| Socioeconomic characteristics: | ||||||||||
| Educational level (Ref. Higher education and above) | ||||||||||
| Elementary education and below | 0.35 | 1.42 (1.05–1.92) * | 0.39 | 1.48 (1.05–2.12) * | ||||||
| Secondary education | −0.05 | 0.95 (0.71–1.26) | −0.08 | 0.92 (0.69–1.23) | ||||||
| Monthly income (Ref. >3000 RMB) | ||||||||||
| <1000 RMB | 0.22 | 1.24 (0.95–1.62) | −0.01 | 0.99 (0.74–1.32) | ||||||
| 1000–3000 RMB | 0.19 | 1.22 (0.99–1.48) | 0.13 | 1.14 (0.93–1.39) | ||||||
| Macro-environmental characteristics: | ||||||||||
| Residence (Ref. Urban) | ||||||||||
| Rural | 0.08 | 1.08 (0.87–1.35) | ||||||||
| Basic endowment Insurance (Ref. Uninsured) | ||||||||||
| Insured | −0.27 | 0.76 (0.55–1.06) | ||||||||
| Basic medical insurance (Ref. Uninsured) | ||||||||||
| Insured | −0.12 | 0.89 (0.61–1.28) | ||||||||
| −2 Loglikelihood | 3657.751 | 3533.541 | 3514.315 | 3483.096 | 3464.779 | |||||
| χ2 | 68.411 | 192.620 | 211.846 | 243.065 | 261.382 | |||||
| Sig | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |||||
| Nagelkerke R2 | 0.029 | 0.081 | 0.088 | 0.101 | 0.108 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.; Shi, L.; Zheng, X.; Yang, J.; Xue, Y.; Xiao, S.; Xue, B.; Zhang, J.; Li, X.; Lin, H.; et al. Patterns and Determinants of Multimorbidity in Older Adults: Study in Health-Ecological Perspective. Int. J. Environ. Res. Public Health 2022, 19, 16756. https://doi.org/10.3390/ijerph192416756
Chen Y, Shi L, Zheng X, Yang J, Xue Y, Xiao S, Xue B, Zhang J, Li X, Lin H, et al. Patterns and Determinants of Multimorbidity in Older Adults: Study in Health-Ecological Perspective. International Journal of Environmental Research and Public Health. 2022; 19(24):16756. https://doi.org/10.3390/ijerph192416756
Chicago/Turabian StyleChen, Yiming, Lei Shi, Xiao Zheng, Juan Yang, Yaqing Xue, Shujuan Xiao, Benli Xue, Jiachi Zhang, Xinru Li, Huang Lin, and et al. 2022. "Patterns and Determinants of Multimorbidity in Older Adults: Study in Health-Ecological Perspective" International Journal of Environmental Research and Public Health 19, no. 24: 16756. https://doi.org/10.3390/ijerph192416756
APA StyleChen, Y., Shi, L., Zheng, X., Yang, J., Xue, Y., Xiao, S., Xue, B., Zhang, J., Li, X., Lin, H., Ma, C., & Zhang, C. (2022). Patterns and Determinants of Multimorbidity in Older Adults: Study in Health-Ecological Perspective. International Journal of Environmental Research and Public Health, 19(24), 16756. https://doi.org/10.3390/ijerph192416756







