Prevalence of Depression, Anxiety, and Stress in Junior High School Students in Guadalajara, Mexico: A Cross-Sectional Survey Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Aims
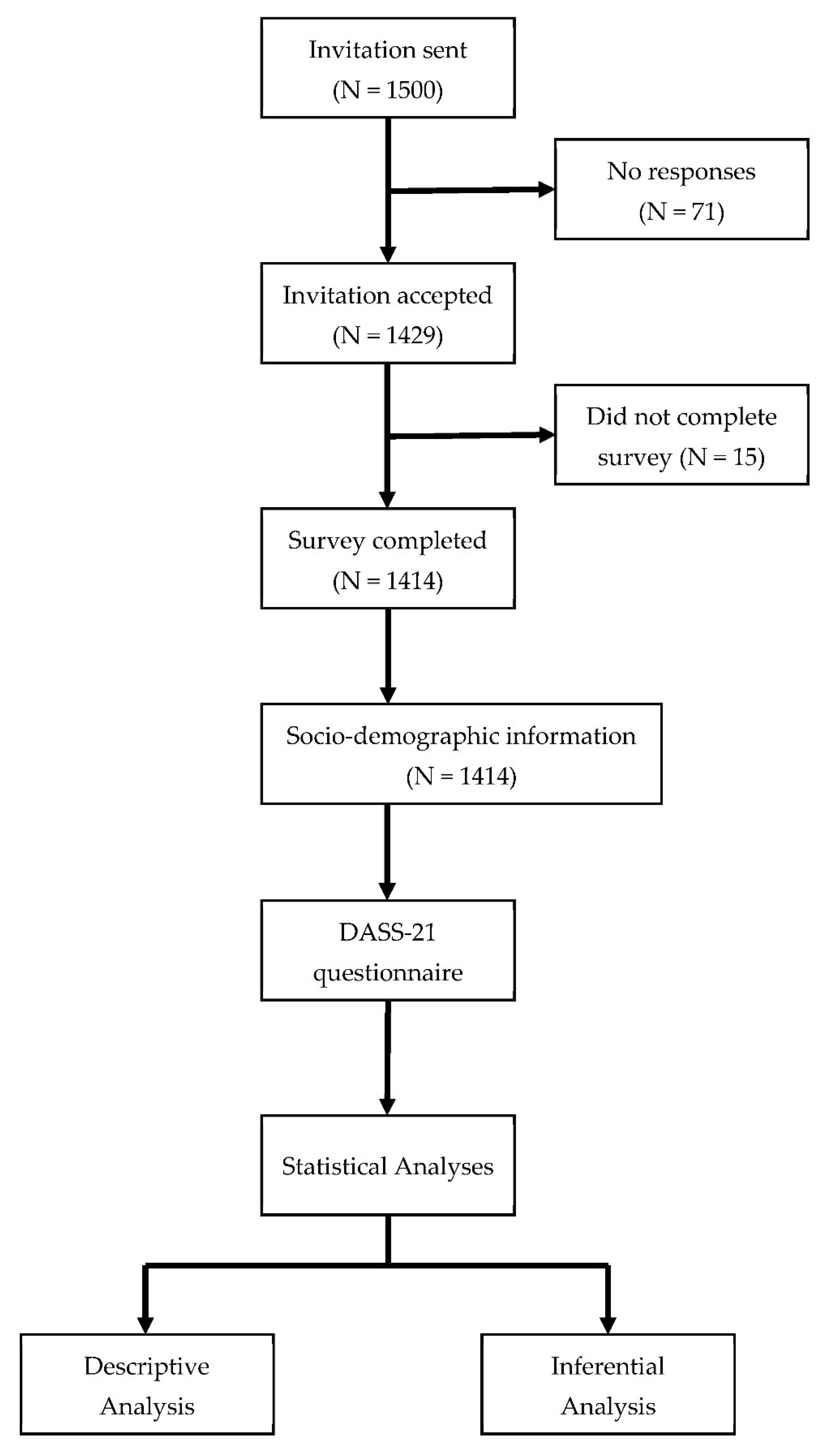
2.2. Design
2.3. Instrument
2.4. Participants
2.5. Sample Size
2.6. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aguilar-Gaxiola, S.; Deeb-Sossa, N. La investigación en epidemiología psiquiátrica y la encuesta mundial de salud mental de la organización mundial de la salud en américa latina y el caribe. [Research in psychiatric epidemiology and the world mental health survey of the world health organization in Latin America and the Caribbean]. In Epidemiología de los Trastornos Mentales en América Latina y el Caribe; Rodríguez, J.J., Kohn, R., Aguilar-Gaxiola, S., Eds.; OPS: Washington, DC, USA, 2009; Volume 1, pp. 35–53. [Google Scholar]
- Berenzon, S.; Asunción Lara, M.; Robles, R.; Elena Medina-Mora, M. Depresión: Estado del conocimiento y la necesidad de políticas públicas y planes de acción en México [Depression: State of knowledge and the need for public policies and action plans in Mexico]. Salud Pública Mex 2013, 55, 74–80. Available online: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0036-36342013000100011&lng=es&nrm=iso&tlng=es (accessed on 2 January 2022). [CrossRef] [PubMed][Green Version]
- Hasin, D.S.; Sarvet, A.L.; Meyers, J.L.; Saha, T.D.; Ruan, W.J.; Stohl, M.; Grant, B.F. Epidemiology of Adult DSM-5 Major Depressive Disorder and its specifiers in the United States. JAMA Psychiatry 2018, 75, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Bandelow, B.; Michaelis, S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin. Neurosci. 2015, 17, 327. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Radua, J.; Olivola, M.; Croce, E.; Soardo, L.; Salazar de Pablo, G.; Il Shin, J.; Kirkbride, J.B.; Jones, P.; Kim, J.H.; et al. Age at onset of mental disorders worldwide: Large-scale meta-analysis of 192 epidemiological studies. Mol. Psychiatry 2022, 27, 281–295. [Google Scholar] [CrossRef]
- Özdin, S.; Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Mucci, F.; Mucci, N.; Diolaiuti, F. Lockdown and isolation: Psychological aspects of COVID-19 pandemic in the general population. Clin. Neuropsychiatry J. Treat. Eval. 2020, 17, 63–64. Available online: https://psycnet.apa.org/record/2020-27302-004 (accessed on 13 March 2022).
- Zhang, C.; Ye, M.; Fu, Y.; Yang, M.; Luo, F.; Yuan, J.; Tao, Q. The psychological impact of the COVID-19 pandemic on teenagers in China. J. Adolesc. Health 2020, 67, 747. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Román Mella, F.; Vinet, E.V.; Alarcón Muñoz, A.M. Escalas de Depresión, Ansiedad y Estrés (DASS-21): Adaptación y propiedades psicométricas en estudiantes secundarios de temuco. Rev. Argent. De Clínica Psicológica 2014, 23, 179–190. Available online: https://www.redalyc.org/exportarcita.oa?id=281943265009 (accessed on 7 March 2022).
- Dapieve-Patias, N.; de Lara-Machado, W.; Ruschel-Bandeira, D.; Dalbosco-Dell’Aglio, D. Depression Anxiety and Stress Scale (DASS-21)—Short Form: Adaptation and validation for Brazilian adolescents. Psico-USF 2016, 21, 459–469. [Google Scholar] [CrossRef]
- Camacho, Á.; Cordero, E.D.; Perkins, T. Psychometric properties of the DASS-21 among latina/o college students by the US-Mexico Border. J. Immigr. Minor. Health 2016, 18, 1017–1023. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112. [Google Scholar] [CrossRef] [PubMed]
- Brumby, S.; Chandrasekara, A.; McCoombe, S.; Torres, S.; Kremer, P.; Lewandowski, P. Reducing psychological distress and obesity in Australian farmers by promoting physical activity. BMC Public Health 2011, 11, 362. [Google Scholar] [CrossRef]
- WHO. Adolescent Mental Health. World Health Organization. 17 November 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed on 7 March 2022).
- Palacio-Ortiz, J.D.; Londoño-Herrera, J.P.; Nanclares-Márquez, A.; Robledo-Rengifo, P.; Quintero-Cadavid, C.P. Trastornos psiquiátricos en los niños y adolescentes en tiempo de la pandemia por COVID-19. Rev. Colomb. Psiquiatría 2020, 49, 279–288. [Google Scholar] [CrossRef]
- UNICEF. La familia y la escuela: Factores clave de la resiliencia. In Salud Mental e Infancia En el Escenario de la COVID-19 Propuestas de UNICEF España; UNICEF, Ed.; UNICEF: Madrid, Spain, 2020; Volume 1, pp. 8–17. [Google Scholar]
- De la Concepción Galiano Ramírez, M.; Prado Rodríguez, R.F.; Mustelier Bécquer, R.G. Salud mental en la infancia y adolescencia durante la pandemia de COVID-19. Rev. Cuba. Pediatría 2021, 92. Available online: http://revpediatria.sld.cu/index.php/ped/article/view/1342/769 (accessed on 10 February 2022).
- Alamolhoda, S.H.; Zare, E.; HakimZadeh, A.; Zalpour, A.; Vakili, F.; Chermahini, R.M.; Ebadifard, R.; Masoumi, M.; Khaleghi, N.; Nasiri, M. Adolescent mental health during covid-19 pandemics: A systematic review. Int. J. Adolesc. Med. Health 2022. [Google Scholar] [CrossRef]
- Andrade da Silva, H.; Pereira Dos Passos, M.H.; Alves de Oliveira, V.M.; Cabral Palmeira, A.; Rodarti Pitangui, A.C.; Cappato de Araújo, R. Short version of the Depression Anxiety Stress Scale-21: Is it valid for Brazilian adolescents? Einstein 2016, 14, 486. [Google Scholar] [CrossRef]
- Le, M.T.H.; Tran, T.D.; Holton, S.; Nguyen, H.T.; Wolfe, R.; Fisher, J. Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PLoS ONE 2017, 12, e0180557. [Google Scholar] [CrossRef] [PubMed]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
| Normal | Mild | Moderate | Severe | Extremely Severe | |
|---|---|---|---|---|---|
| Depression | <9 | 10–13 | 14–20 | 21–27 | >28 |
| Anxiety | <7 | 8–9 | 10–14 | 15–19 | >20 |
| Stress | <14 | 15–18 | 19–25 | 26–33 | >34 |
| Age (years), (Mean ± SD) | 13.39 ± 0.99 |
| Sex, n (%) | |
| Female | 779 (55.1%) |
| Male | 635 (44.9%) |
| Age group (years) | n (%) |
| 12–13 | 788 (55.7%) |
| 14–16 | 626 (44.3%) |
| Type of school | n (%) |
| Public | 1076 (76.1%) |
| Private | 338 (23.9%) |
| School shift | n (%) |
| Morning shift | 1188 (84%) |
| Evening shift | 226 (16%) |
| School grade | n (%) |
| 1st grade | 552 (39%) |
| 2nd grade | 450 (31.8%) |
| 3rd grade | 412 (29.1%) |
| Type of family | n (%) |
| Nuclear family | 763 (54%) |
| Extended family | 353 (25%) |
| Single-parent family | 235 (16.6%) |
| Unipersonal family | 63 (4.5%) |
| Age Group | Depression Mean Scores | p-Value | Anxiety Mean Scores | p-Value | Stress Mean Scores | p-Value |
|---|---|---|---|---|---|---|
| 12–13 | 6.27 ± 5.6 | 0.21 * | 5.9 ± 5.2 | 0.95 * | 8.09 ± 5.3 | 0.29 * |
| 14–16 | 6.01 ± 5.5 | 5.8 ± 5.1 | 8.07 ± 5.4 | |||
| Sex | ||||||
| Female | 7.37 ± 5.9 | 0.001 * | 7.07 ± 5.5 | 0.001 * | 9.41 ± 5.4 | 0.001 * |
| Male | 4.66 ± 4.7 | 4.38 ± 4.3 | 6.45 ± 4.7 | |||
| Type of school | ||||||
| Public | 6.39 ± 5.6 | 6.02 ± 5.1 | 8.11 ± 5.3 | |||
| Private | 5.41 ± 5.3 | 0.004 * | 5.36 ± 5.3 | 0.95 * | 7.99 ± 5.3 | 0.91 * |
| School grade | ||||||
| 1st grade | 5.76 ± 5.4 | 0.073 † | 5.54 ± 4.9 | 0.167 † | 7.82 ± 5.1 | 0.207 † |
| 2nd grade | 6.25 ± 5.7 | 6.15 ± 5.4 | 8.44 ± 5.56 | |||
| 3rd grade | 6.58 ± 6.61 | 5.86 ± 5.21 | 8.08 ± 5.3 | |||
| School shift | ||||||
| Morning shift | 5.88 ± 5.4 | 0.001 * | 5.65 ± 5.1 | 0.001 * | 7.90 ± 5.3 | 0.37 * |
| Evening shift | 7.59 ± 6.0 | 6.98 ± 5.6 | 9.03 ± 5.5 | |||
| Type of family | ||||||
| Nuclear family | 5.59 ± 5.5 | 0.001 † | 5.34 ± 5.0 | 0.001 † | 7.76 ± 5.2 | 0.026 † |
| Extended family | 6.58 ± 5.7 | 6.19 ± 5.2 | 8.13 ± 5.3 | |||
| Single-parent family | 7.0 ± 5.69 | 6.91 ± 5.5 | 8.72 ± 5.4 | |||
| Unipersonal family | 7.44 ± 5.6 | 6.41 ± 5.3 | 9.28 ± 5.7 | |||
| Parental work | ||||||
| Only one parent works | 5.98 ± 5.6 | 0.70 * | 5.68 ± 5.3 | 0.21 * | 7.96 ± 5.5 | 0.12 * |
| Both parents work | 6.24 ± 5.5 | 5.96 ± 5.1 | 8.15 ± 5.2 | |||
| Infected family member | ||||||
| Yes | 6.39 ± 5.7 | 0.13 * | 6.19 ± 5.3 | 0.004 * | 8.52 ± 5.4 | 0.10 * |
| No | 5.81 ± 5.4 | 5.39 ± 5 | 7.43 ± 5.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maciel-Saldierna, M.; Elizondo-Hernández, E.; Cervantes-Guevara, G.; Cervantes-Pérez, E.; Cervantes-Cardona, G.A.; Guzmán-Ramírez, B.G.; Brancaccio-Pérez, I.V.; Chejfec-Ciociano, J.M.; Guzmán-Ruvalcaba, M.J.; Cifuentes-Andrade, L.R.; et al. Prevalence of Depression, Anxiety, and Stress in Junior High School Students in Guadalajara, Mexico: A Cross-Sectional Survey Study. Int. J. Environ. Res. Public Health 2022, 19, 15463. https://doi.org/10.3390/ijerph192315463
Maciel-Saldierna M, Elizondo-Hernández E, Cervantes-Guevara G, Cervantes-Pérez E, Cervantes-Cardona GA, Guzmán-Ramírez BG, Brancaccio-Pérez IV, Chejfec-Ciociano JM, Guzmán-Ruvalcaba MJ, Cifuentes-Andrade LR, et al. Prevalence of Depression, Anxiety, and Stress in Junior High School Students in Guadalajara, Mexico: A Cross-Sectional Survey Study. International Journal of Environmental Research and Public Health. 2022; 19(23):15463. https://doi.org/10.3390/ijerph192315463
Chicago/Turabian StyleMaciel-Saldierna, Manuel, Emmanuel Elizondo-Hernández, Gabino Cervantes-Guevara, Enrique Cervantes-Pérez, Guillermo Alonso Cervantes-Cardona, Bertha Georgina Guzmán-Ramírez, Irma Valeria Brancaccio-Pérez, Jonathan Matías Chejfec-Ciociano, Mario Jesús Guzmán-Ruvalcaba, Luis Rodrigo Cifuentes-Andrade, and et al. 2022. "Prevalence of Depression, Anxiety, and Stress in Junior High School Students in Guadalajara, Mexico: A Cross-Sectional Survey Study" International Journal of Environmental Research and Public Health 19, no. 23: 15463. https://doi.org/10.3390/ijerph192315463
APA StyleMaciel-Saldierna, M., Elizondo-Hernández, E., Cervantes-Guevara, G., Cervantes-Pérez, E., Cervantes-Cardona, G. A., Guzmán-Ramírez, B. G., Brancaccio-Pérez, I. V., Chejfec-Ciociano, J. M., Guzmán-Ruvalcaba, M. J., Cifuentes-Andrade, L. R., Cueto-Valadez, A. E., Cueto-Valadez, T. A., Ibarra-Camargo, S. A., Mellado-Tellez, M. P., Barbosa-Camacho, F. J., Fuentes-Orozco, C., & González-Ojeda, A. (2022). Prevalence of Depression, Anxiety, and Stress in Junior High School Students in Guadalajara, Mexico: A Cross-Sectional Survey Study. International Journal of Environmental Research and Public Health, 19(23), 15463. https://doi.org/10.3390/ijerph192315463






