Do Community Home-Based Elderly Care Services Improve Life Satisfaction of Chinese Older Adults? An Empirical Analysis Based on the 2018 CLHLS Dataset
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Variable Description
2.2.1. Dependent Variable
2.2.2. Independent Variables
2.2.3. Control Variables
2.3. Methodology
3. Results
3.1. Descriptive Statistics
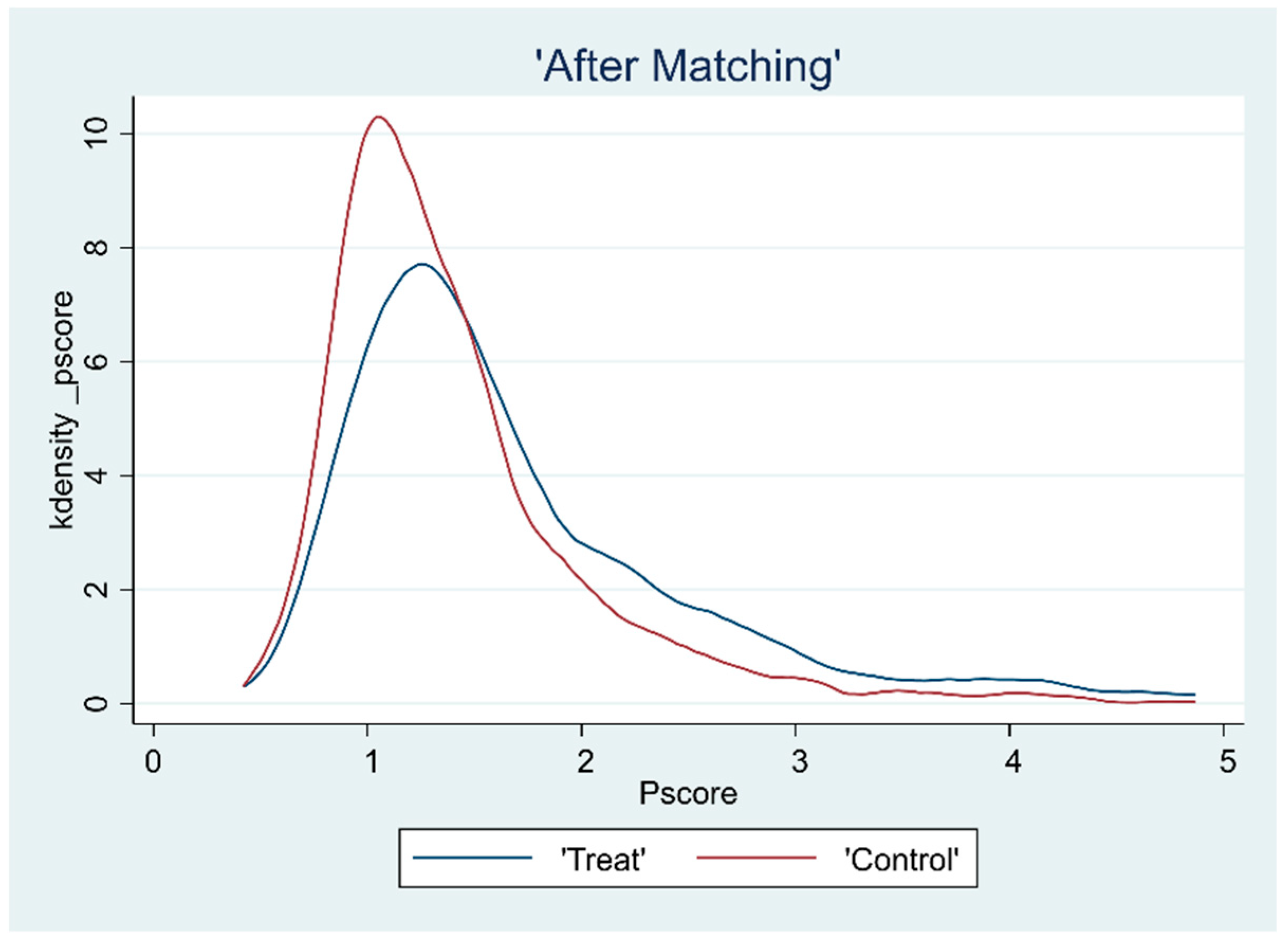
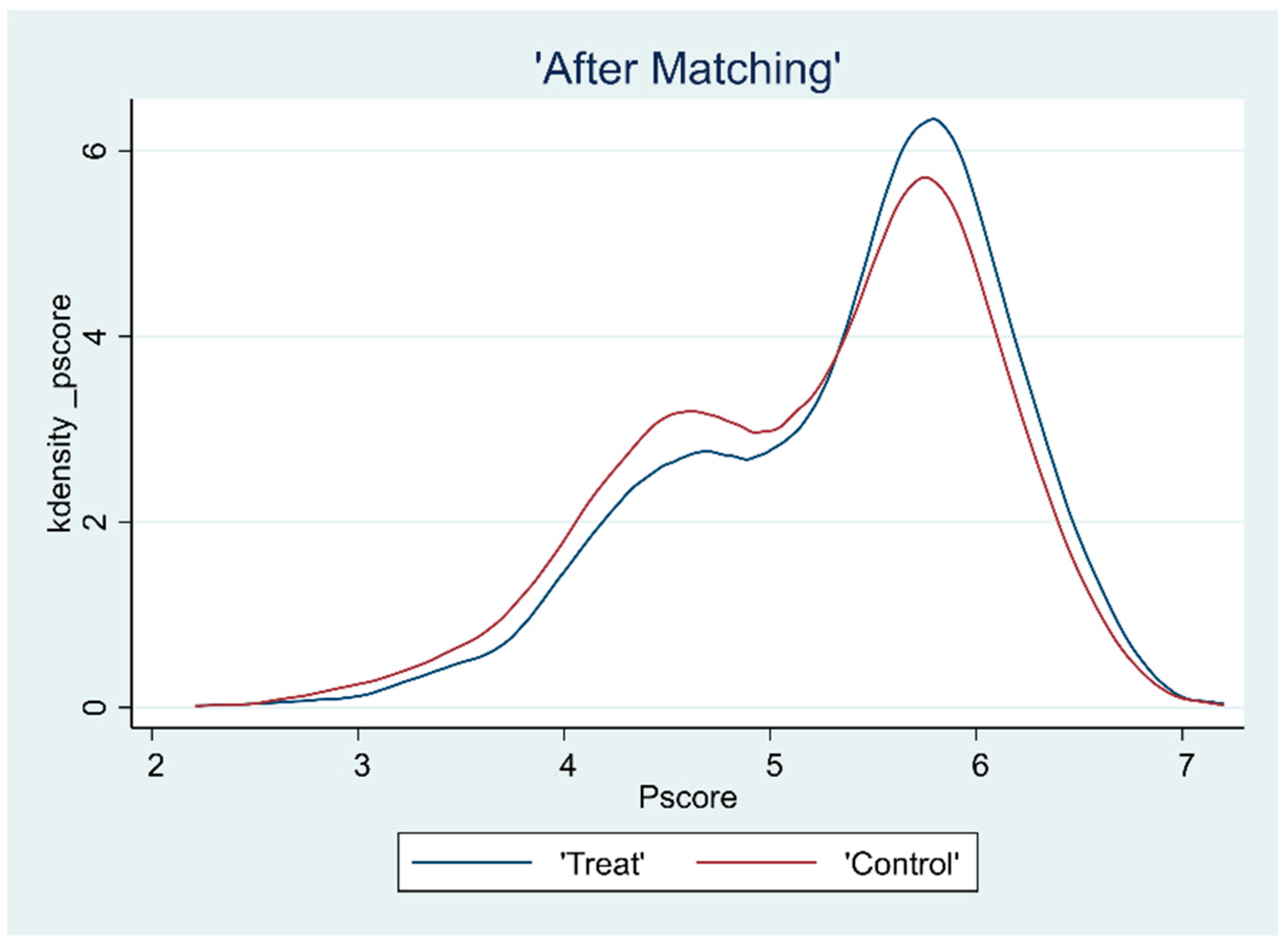
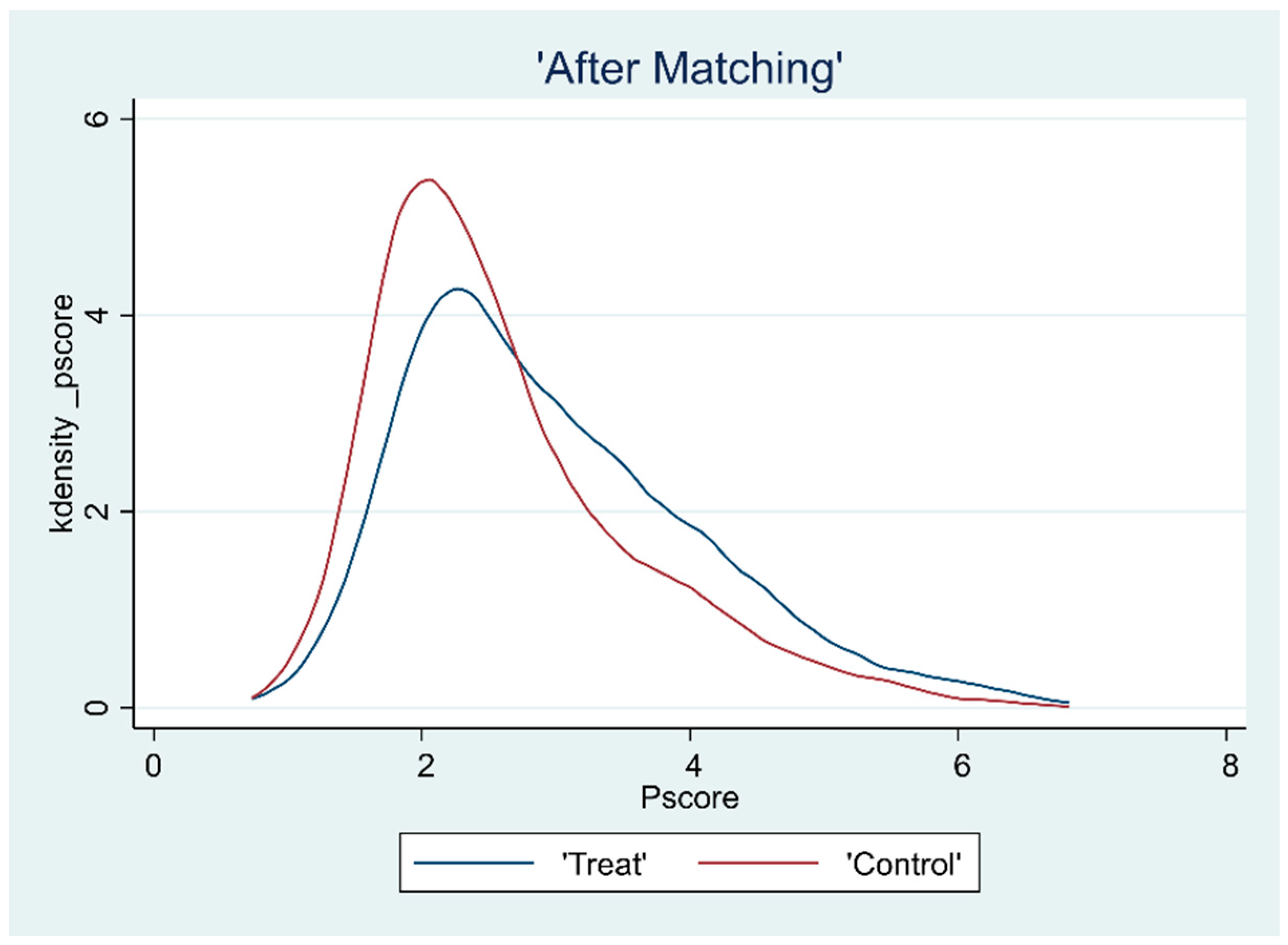
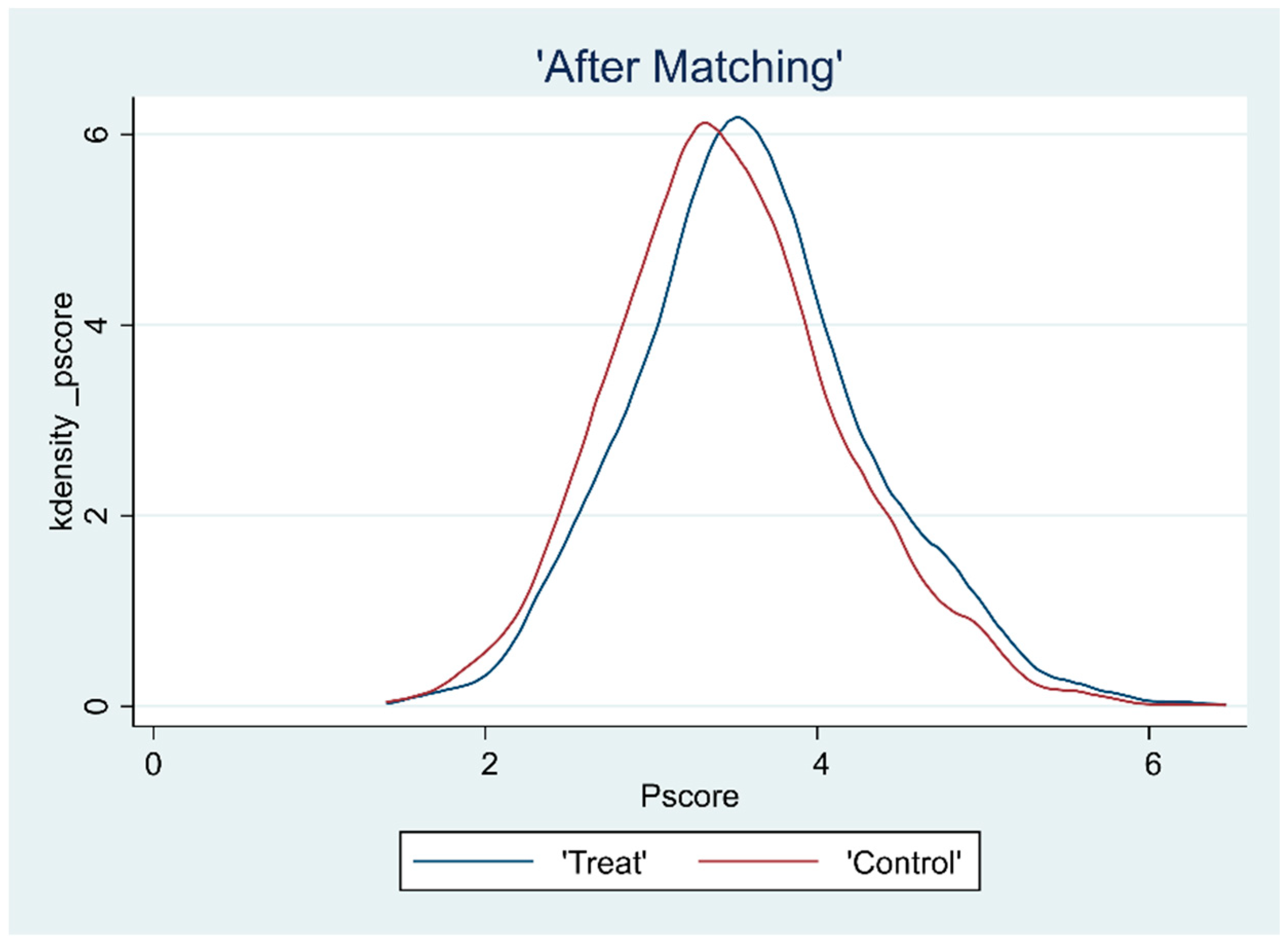
3.2. Overlap Test
3.3. Balance Test
3.4. Average Effect Analysis
3.5. Heterogeneous Effect Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shin, D.C.; Johnson, D.M. Avowed Happiness as an Overall Assessment of the Quality of Life. Soc. Indic. Res. 1978, 5, 475–492. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Personal. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Blanchflower, D.G. Unhappiness and Age. J. Econ. Behav. Organ. 2020, 176, 461–488. [Google Scholar] [CrossRef]
- Barnay, T.; Juin, S. Does Home Care for Dependent Elderly People Improve Their Mental Health? J. Health Econ. 2016, 45, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Macbride, A. Retirement as a Life Crisis: Myth or Reality? A Review. Can. Psychiatr. Assoc. J. 1976, 21, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Fast, J.E.; Williamson, D.L.; Keating, N.C. The Hidden Costs of Informal Elder Care. J. Fam. Econ. Issues 1999, 20, 301–326. [Google Scholar] [CrossRef]
- Rakowski, W.; Clark, N.M. Future Outlook, Caregiving, and Care-Receiving in the Family Context. The Gerontologist 1985, 25, 618–623. [Google Scholar] [CrossRef]
- Han, J.; Lee, S.; Kwon, Y. Can Social Capital Improve the Quality of Life Satisfaction for Older Adults? Focusing on the 2016 Quality of Life Survey in Gyeonggi Province, Korea. Cities 2022, 130, 103853. [Google Scholar] [CrossRef]
- Zapata-Lamana, R.; Poblete-Valderrama, F.; Ledezma-Dames, A.; Pavón-León, P.; Leiva, A.M.; Fuentes-Alvarez, M.T.; Cigarroa, I.; Parra-Rizo, M.A. Health, Functional Ability, and Environmental Quality as Predictors of Life Satisfaction in Physically Active Older Adults. Soc. Sci. 2022, 11, 265. [Google Scholar] [CrossRef]
- Akimov, A.V.; Gemueva, K.A.; Semenova, N.K. The Seventh Population Census in the PRC: Results and Prospects of the Country’s Demographic Development. Her. Russ. Acad. Sci. 2021, 91, 724–735. [Google Scholar] [CrossRef]
- Chu, L.-W.; Chi, I. Nursing Homes in China. J. Am. Med. Dir. Assoc. 2008, 9, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, P.; Sun, W.; Wang, C. Well-Being Loss in Informal Care for the Elderly People: Empirical Study from China National Baseline CHARLS. Asia Pac. Psychiatry 2019, 11, e12336. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Chow, J.C. Exploring the Community-Based Service Delivery Model: Elderly Care in China. Int. Soc. Work 2011, 54, 374–387. [Google Scholar] [CrossRef]
- Gao, Y. Problems and Countermeasures in Building an Age-Friendly Society in China. Chin. Public Adm. Nistration 2022, 9, 74–79. [Google Scholar] [CrossRef]
- Bilgili, N.; Arpacı, F. Quality of Life of Older Adults in Turkey. Arch. Gerontol. Geriatr. 2014, 59, 415–421. [Google Scholar] [CrossRef]
- Cheung, J.C.K.; Kwan, A.Y.H.; Chan, S.S.C.; Ngan, R.M.H.; Ng, S.H.; Leung, E.M.F.; Lau, A. Quality of Life in Older Adults: Benefits from Caring Services in Hong Kong. Soc. Indic. Res. 2005, 71, 291–334. [Google Scholar] [CrossRef]
- Zhou, H.; Chen, X.; Dong, Y. The Impact of Community Home-based Elderly Care Services on the Health of Urban Elderly. Stat. Decis. 2018, 34, 98–101. [Google Scholar] [CrossRef]
- Shen, Y.; Yeatts, D.E. Social Support and Life Satisfaction among Older Adults in China: Family-Based Support versus Community-Based Support. Int. J. Aging Hum. Dev. 2013, 77, 189–209. [Google Scholar] [CrossRef]
- Su, S.-W.; Wang, D. Health-Related Quality of Life and Related Factors among Elderly Persons under Different Aged Care Models in Guangzhou, China: A Cross-Sectional Study. Qual. Life Res. 2019, 28, 1293–1303. [Google Scholar] [CrossRef]
- Hellström, Y.; Persson, G.; Hallberg, I.R. Quality of Life and Symptoms among Older People Living at Home. J. Adv. Nurs. 2004, 48, 584–593. [Google Scholar] [CrossRef]
- Gu, L.; Cheng, Y.; Phillips, D.R.; Rosenberg, M. Understanding the Wellbeing of the Oldest-Old in China: A Study of Socio-Economic and Geographical Variations Based on CLHLS Data. Int. J. Environ. Res. Public Health 2019, 16, 601. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.; Jia, G.; Liu, K. Health-Related Quality of Life and Related Factors among Elderly People in Jinzhou, China: A Cross-Sectional Study. Public Health 2015, 129, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Song, W.; Ye, C.; Wang, Z. Family Networks, Social Networks, and Life Satisfaction of Older Adults in China. Healthcare 2022, 10, 1568. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Hao, Y. A Study on the Effect of Community Old-age Service on the Mental Health Improvement of the Elderly. Northwest Popul. J. 2020, 41, 79–91. [Google Scholar] [CrossRef]
- Yao, X.; Su, Q.; Zhu, M.; Ji, L. The Adoption of Smart Senior Care Services and Health of the Elderly under the “Silver Wave”. J. Soc. Dev. 2021, 8, 181–195 + 242–243. [Google Scholar]
- Thielke, S.; Harniss, M.; Thompson, H.; Patel, S.; Demiris, G.; Johnson, K. Maslow’s Hierarchy of Human Needs and the Adoption of Health-Related Technologies for Older Adults. Ageing Int 2012, 37, 470–488. [Google Scholar] [CrossRef]
- Taormina, R.J.; Gao, J.H. Maslow and the Motivation Hierarchy: Measuring Satisfaction of the Needs. Am. J. Psychol. 2013, 126, 155–177. [Google Scholar] [CrossRef]
- Zhang, C.; Lan, X. Community Support and Elderly Health Promotion. World Surv. Res. 2021, 1, 74–81. [Google Scholar] [CrossRef]
- Pinto, J.M.; Fontaine, A.M.; Neri, A.L. The Influence of Physical and Mental Health on Life Satisfaction Is Mediated by Self-Rated Health: A Study with Brazilian Elderly. Arch. Gerontol. Geriatr. 2016, 65, 104–110. [Google Scholar] [CrossRef]
- Xu, J.; Qiu, J.; Chen, J.; Zou, L.; Feng, L.; Lu, Y.; Wei, Q.; Zhang, J. Lifestyle and Health-Related Quality of Life: A Cross-Sectional Study among Civil Servants in China. BMC Public Health 2012, 12, 330. [Google Scholar] [CrossRef]
- Tao, Y.; Shen, Y. The Influence of Social Support on the Physical and Mental Health of the Rural Elderly. Popul. Econ. 2014, 3, 3–14. [Google Scholar]
- Idler, E.L.; Benyamini, Y. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. J. Health Soc. Behav. 1997, 38, 21–37. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Wang, X.; Zheng, C. The Impact of Health Insurance on Medical Expenditure and Health of the Elderly. J. Financ. Econ. 2014, 40, 65–75. [Google Scholar] [CrossRef]
- Steiner, P.M.; Cook, T.D.; Shadish, W.R. On the Importance of Reliable Covariate Measurement in Selection Bias Adjustments Using Propensity Scores. J. Educ. Behav. Stat. 2011, 36, 213–236. [Google Scholar] [CrossRef]
- Caliendo, M.; Kopeinig, S. Some Practical Guidance for the Implementation of Propensity Score Matching. J. Econ. Surv. 2008, 22, 31–72. [Google Scholar] [CrossRef]
- Lian, Y.; Su, Z.; Gu, Y. Evaluating the Effects of Equity Incentives Using PSM: Evidence from China. Front. Bus. Res. China 2011, 2, 266–290. [Google Scholar] [CrossRef]
- Gu, T.; Yuan, J.; Li, L.; Shao, Q.; Zheng, C. Demand for Community-Based Care Services and Its Influencing Factors among the Elderly in Affordable Housing Communities: A Case Study in Nanjing City. BMC Health Serv. Res. 2020, 20, 241. [Google Scholar] [CrossRef]
- Lv, X.; Zhang, X. The Influence of Community Home-based Elderly Care on the Health of the Elderly Population. Chin. J. Popul. Sci. 2022, 3, 111–125+128. [Google Scholar]
- Lin, W. The Relationship between Formal and Informal Care among Chinese Older Adults: Based on the 2014 CLHLS Dataset. BMC Health Serv. Res. 2019, 19, 323. [Google Scholar] [CrossRef]
- Zimmer, Z.; Kwong, J. Family Size and Support of Older Adults in Urban and Rural China: Current Effects and Future Implications. Demography 2003, 40, 23–44. [Google Scholar] [CrossRef] [PubMed]
- Duan, H.; Zhang, Y.; Hou, Y.; Ma, L. Research on the Influence of the Policy of Medical Alliance on the Service Ability of Primary Community Medical and Health Institutions—A Quasi Experimental Study from the Perspective of Organizational Alliance Theory. J. Gansu Adm. Inst. 2020, 4, 4–16+124. [Google Scholar]
- Fang, E.F.; Xie, C.; Schenkel, J.A.; Wu, C.; Long, Q.; Cui, H.; Aman, Y.; Frank, J.; Liao, J.; Zou, H.; et al. A Research Agenda for Ageing in China in the 21st Century (2nd Edition): Focusing on Basic and Translational Research, Long-Term Care, Policy and Social Networks. Ageing Res. Rev. 2020, 64, 101174. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Wei, X. Analysis Framework, Concept, and Pathways of Digital Divide Governance for Older Adults: From the Perspective of Digital Divide and Knowledge Gap Theory. Popul. Res. 2021, 45, 17–30. [Google Scholar]
- Su, H.; Zhou, Y.; Sun, Y.; Cai, Y. The Relationship between Depression and Subjective Cognitive Decline in Older Adults of China: The Mediating Role of General Self-Efficacy. Psychol. Health Med. 2022, 1–11. [Google Scholar] [CrossRef]
- Tsai, F.J.; Motamed, S.; Rougemont, A. The Protective Effect of Taking Care of Grandchildren on Elders’ Mental Health? Associations between Changing Patterns of Intergenerational Exchanges and the Reduction of Elders’ Loneliness and Depression between 1993 and 2007 in Taiwan. BMC Public Health 2013, 13, 567. [Google Scholar] [CrossRef]
| Where to Live | Services Provider | Cost | |
|---|---|---|---|
| Family elderly care model | Home | Family members | Low |
| Institutional elderly care model | Institutions | Professional nursing staff | High |
| Community home-based elderly care model | Home | Family members and professional nursing staff | Relatively low |
| Variable Category | Variable | Min. | Max. | Mean | S.D. |
|---|---|---|---|---|---|
| Dependent variable | Life satisfaction | 1 | 5 | 3.946 | 0.804 |
| Independent variables | Life care services (LCS) | 0 | 1 | 0.141 | 0.348 |
| Medical care services (MCS) | 0 | 1 | 0.523 | 0.500 | |
| Spiritual and cultural services (SCS) | 0 | 1 | 0.262 | 0.440 | |
| Reconciliation and legal services (RLS) | 0 | 1 | 0.346 | 0.476 | |
| Personal characteristics | Gender | 0 | 1 | 0.471 | 0.499 |
| Age | 60 | 117 | 83.212 | 11.299 | |
| Household registration | 0 | 1 | 0.179 | 0.383 | |
| Years of education | 0 | 18 | 3.796 | 4.364 | |
| Relative economic level | 1 | 5 | 3.135 | 0.652 | |
| Whether to live with spouse | 0 | 1 | 0.463 | 0.499 | |
| Whether to live with family | 0 | 1 | 0.835 | 0.371 | |
| Availability of commercial insurance and social security | 0 | 1 | 0.074 | 0.261 | |
| Living habits | Sleep quality | 1 | 5 | 3.552 | 1.004 |
| Smoking or not | 0 | 1 | 0.166 | 0.372 | |
| Drinking or not | 0 | 1 | 0.162 | 0.369 | |
| Whether to exercise regularly | 0 | 1 | 0.382 | 0.486 | |
| Whether annual medical examination | 0 | 1 | 0.693 | 0.462 | |
| Level of physical and mental health | Self-assessed health level | 1 | 5 | 3.495 | 0.913 |
| ADL | 1 | 3 | 2.611 | 0.632 | |
| Illness | 0 | 24 | 1.490 | 1.598 | |
| Depression level | 6 | 30 | 22.718 | 3.929 | |
| Personality–emotion | 13 | 35 | 27.078 | 3.435 | |
| Family support | Family financial support | 0 | 1 | 0.621 | 0.485 |
| Family health support | 0 | 1 | 0.933 | 0.250 | |
| Family emotional support | 0 | 1 | 0.916 | 0.277 |
| Variables | Sample Matching | LCS | MCS | SCS | RLS | ||||
|---|---|---|---|---|---|---|---|---|---|
| Deviation | t-Value | Deviation | t-Value | Deviation | t-Value | Deviation | t-Value | ||
| Gender | Unmatched | −0.005 | −0.20 | 0.014 | 0.84 | 0.010 | 0.56 | 0.003 | 0.15 |
| Matched | 0.001 | 0.04 | 0.006 | 0.38 | −0.001 | −0.07 | 0.004 | 0.22 | |
| Age | Unmatched | 0.014 | 0.03 | −0.161 | −0.44 | −0.596 | −1.43 | −0.644 | −1.67 * |
| Matched | −0.095 | −0.14 | 0.031 | 0.09 | −0.004 | −0.01 | −0.043 | −0.10 | |
| Household registration | Unmatched | 0.103 | 5.78 *** | 0.010 | 0.77 | 0.124 | 8.83 *** | 0.056 | 4.26 *** |
| Matched | 0.020 | 0.74 | 0.002 | 0.18 | 0.015 | 0.75 | 0.013 | 0.83 | |
| Years of education | Unmatched | 1.045 | 5.15 *** | 0.203 | 1.43 | 1.447 | 9.09 *** | 0.668 | 4.50 *** |
| Matched | 0.239 | 0.81 | 0.039 | 0.28 | 0.133 | 0.62 | 0.138 | 0.78 | |
| Relative economic level | Unmatched | 0.172 | 5.68 *** | 0.080 | 3.79 *** | 0.152 | 6.37 *** | 0.093 | 4.19 *** |
| Matched | 0.027 | 0.64 | 0.027 | 1.31 | 0.020 | 0.67 | 0.017 | 0.66 | |
| Whether to live with spouse | Unmatched | −0.010 | −0.43 | 0.021 | 1.28 | 0.034 | 1.85 * | 0.038 | 2.21 ** |
| Matched | 0.001 | 0.03 | −0.000 | −0.01 | −0.001 | −0.04 | 0.004 | 0.21 | |
| Whether to live with family | Unmatched | 0.016 | 0.91 | 0.027 | 2.21 ** | 0.032 | 2.31 | 0.012 | 0.91 |
| Matched | 0.008 | 0.35 | 0.001 | 0.11 | 0.003 | 0.17 | −0.001 | −0.09 | |
| Availability of commercial insurance and social security | Unmatched | 0.010 | 0.81 | −0.027 | −3.15 *** | −0.001 | −0.07 | −0.016 | −1.83 * |
| Matched | 0.002 | 0.15 | −0.001 | −0.12 | −0.001 | −0.04 | 0.000 | 0.03 | |
| Sleep quality | Unmatched | 0.036 | 0.77 | 0.031 | 0.96 | 0.090 | 2.43 ** | 0.031 | 0.91 |
| Matched | 0.003 | 0.04 | 0.013 | 0.40 | −0.006 | −0.14 | 0.006 | 0.16 | |
| Smoking or not | Unmatched | −0.010 | −0.58 | −0.029 | −2.43 ** | −0.040 | −2.88 *** | −0.031 | −2.47 ** |
| Matched | −0.004 | −0.16 | −0.002 | −0.13 | −0.004 | −0.23 | 0.001 | 0.06 | |
| Drinking or not | Unmatched | 0.003 | 0.17 | 0.010 | 0.84 | 0.010 | 0.76 | 0.006 | 0.46 |
| Matched | 0.002 | 0.07 | 0.005 | 0.47 | 0.002 | 0.10 | 0.002 | 0.15 | |
| Whether to exercise regularly | Unmatched | 0.095 | 4.18 *** | 0.012 | 0.78 | 0.109 | 6.12 | 0.052 | 3.12 *** |
| Matched | 0.020 | 0.64 | 0.001 | 0.04 | −0.002 | −0.09 | 0.005 | 0.26 | |
| Whether receiving an annual medical examination | Unmatched | 0.049 | 2.27 ** | 0.114 | 7.66 *** | 0.023 | 1.38 | 0.053 | 3.35 *** |
| Matched | 0.007 | 0.26 | 0.001 | 0.05 | −0.002 | −0.11 | 0.003 | 0.16 | |
| Self-assessed health level | Unmatched | 0.113 | 2.66 ** | 0.064 | 2.15 ** | 0.084 | 2.50 ** | 0.078 | 2.50 ** |
| Matched | 0.009 | 0.16 | 0.020 | 0.70 | −0.015 | −0.38 | 0.006 | 0.17 | |
| ADL | Unmatched | −0.002 | −0.08 | −0.010 | −0.47 | −0.014 | −0.58 | 0.022 | 1.02 |
| Matched | −0.003 | −0.07 | −0.012 | −0.61 | −0.004 | −0.14 | −0.002 | −0.07 | |
| Illness | Unmatched | 0.192 | 2.57 ** | 0.082 | 1.58 | 0.372 | 6.35 *** | 0.211 | 3.88 *** |
| Matched | 0.047 | 0.46 | 0.023 | 0.45 | 0.019 | 0.24 | 0.045 | 0.70 | |
| Depression level | Unmatched | 0.426 | 2.32 ** | 0.083 | 0.65 | 0.141 | 0.97 | 0.055 | 0.41 |
| Matched | 0.074 | 0.31 | −0.020 | −0.16 | −0.021 | −0.12 | 0.000 | 0.00 | |
| Personality–emotion | Unmatched | 0.490 | 3.06 *** | 0.120 | 1.08 | 0.533 | 4.22 *** | 0.225 | 1.93 * |
| Matched | 0.072 | 0.35 | 0.027 | 0.24 | −0.014 | −0.09 | 0.002 | 0.01 | |
| Family financial support | Unmatched | −0.044 | −1.96 | 0.026 | 1.65 * | −0.031 | −1.73 ** | 0.029 | 1.77 * |
| Matched | −0.006 | −0.21 | 0.007 | 0.42 | −0.002 | −0.07 | 0.000 | 0.00 | |
| Family health Support | Unmatched | −0.077 | −6.61 *** | 0.008 | 1.01 | −0.025 | −2.71 ** | 0.008 | 0.95 |
| Matched | −0.013 | −0.66 | −0.004 | −0.51 | −0.005 | −0.37 | −0.001 | −0.11 | |
| Family emotional support | Unmatched | −0.037 | −2.90 | 0.027 | 2.96 *** | 0.002 | 0.19 | 0.022 | 2.36 ** |
| Matched | −0.003 | −0.13 | −0.002 | −0.27 | 0.000 | 0.02 | 0.001 | 0.07 | |
| Service Category | Matching Method | Treatment Group | Control Group | ATT | S.D. | t-Value |
|---|---|---|---|---|---|---|
| LCS | K-nearest neighbor matching | 4.062 | 4.055 | 0.007 | 0.043 | 0.15 |
| Radius matching | 4.058 | 4.030 | 0.028 | 0.039 | 0.74 | |
| Kernel matching | 4.062 | 4.017 | 0.045 | 0.038 | 1.17 | |
| Mean | 4.061 | 4.034 | 0.027 | 0.040 | ||
| MCS | K-nearest neighbor matching | 3.992 | 3.945 | 0.047 | 0.029 | 1.63 |
| Radius matching | 3.992 | 3.953 | 0.039 | 0.027 | 1.43 | |
| Kernel matching | 3.992 | 3.946 | 0.046 | 0.027 | 1.72 * | |
| Mean | 3.992 | 3.948 | 0.044 | 0.028 | ||
| SCS | K-nearest neighbor matching | 4.076 | 4.016 | 0.060 | 0.034 | 1.79 * |
| Radius matching | 4.076 | 4.019 | 0.057 | 0.031 | 1.88 ** | |
| Kernel matching | 4.076 | 4.012 | 0.064 | 0.030 | 2.13 ** | |
| Mean | 4.076 | 4.016 | 0.060 | 0.032 | ||
| RLS | K-nearest neighbor matching | 4.039 | 3.948 | 0.091 | 0.030 | 2.99 *** |
| Radius matching | 4.039 | 3.966 | 0.068 | 0.028 | 2.66 ** | |
| Kernel matching | 4.039 | 3.962 | 0.077 | 0.028 | 2.79 *** | |
| Mean | 4.039 | 3.959 | 0.080 | 0.029 |
| Service Category | Matching Method | ADL | Depression Level | Whether to Live with Families | |||
|---|---|---|---|---|---|---|---|
| Restricted | Unrestricted | CES-D > 20 | CES-D ≤ 20 | Yes | No | ||
| LCS | K-nearest neighbor matching | 0.027 (0.34) | 0.049 (0.99) | 0.004 (0.08) | 0.030 (0.34) | −0.059 (−0.51) | 0.043 (0.95) |
| Radius matching | 0.010 (0.14) | 0.042 (0.91) | 0.013 (0.30) | 0.080 (1.02) | −0.074 (−0.70) | 0.051 (1.23) | |
| Kernel matching | 0.013 (0.17) | 0.053 (1.16) | 0.026 (0.62) | 0.083 (1.06) | −0.058 (−0.54) | 0.071 * (1.74) | |
| Mean | 0.016 | 0.048 | 0.014 | 0.065 | −0.064 | 0.055 | |
| MCS | K-nearest neighbor matching | −0.042 (−0.76) | 0.064 * (1.86) | 0.041 (1.28) | 0.040 (0.69) | 0.047 (0.58) | 0.033 (1.05) |
| Radius matching | −0.028 (−0.54) | 0.062 ** (1.98) | 0.037 (1.26) | 0.057 (1.06) | 0.025 (0.35) | 0.041 (1.42) | |
| Kernel matching | −0.015 (−0.30) | 0.067 ** (2.12) | 0.039 (1.31) | 0.060 (1.12) | 0.033 (0.45) | 0.045 (1.54) | |
| Mean | −0.028 | 0.064 | 0.039 | 0.053 | 0.035 | 0.040 | |
| SCS | K-nearest neighbor matching | 0.013 (0.21) | 0.080 ** (2.05) | 0.083 ** (2.32) | −0.028 (−0.40) | −0.06 (−0.66) | 0.065 * (1.82) |
| Radius matching | −0.003 (−0.05) | 0.090 ** (2.55) | 0.080 ** (2.46) | 0.004 (0.05) | −0.06 (−0.69) | 0.079 ** (2.41) | |
| Kernel matching | −0.000 (−0.00) | 0.095 ** (2.72) | 0.084 ** (2.60) | 0.003 (0.05) | −0.06 (−0.72) | 0.083 ** (2.55) | |
| Mean | 0.004 | 0.088 | 0.082 | −0.007 | −0.06 | 0.075 | |
| RLS | K-nearest neighbor matching | −0.050 (−0.87) | 0.1153 *** (3.24) | 0.052 (1.56) | 0.050 (0.82) | −0.023 (−0.28) | 0.078 ** (2.41) |
| Radius matching | −0.023 (−0.43) | 0.114 *** (3.50) | 0.064 ** (2.11) | 0.066 (1.19) | 0.037 (0.50) | 0.085 *** (2.86) | |
| Kernel matching | −0.014 (−0.26) | 0.120 *** (3.70) | 0.070 ** (2.31) | 0.073 (1.34) | 4.072 (−0.03) | 0.089 *** (3.03) | |
| Mean | −0.029 | 0.116 | 0.062 | 0.063 | 0.004 | 0.084 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Z.; Mao, Y.; Shui, Y.; Deng, R.; Hu, Y. Do Community Home-Based Elderly Care Services Improve Life Satisfaction of Chinese Older Adults? An Empirical Analysis Based on the 2018 CLHLS Dataset. Int. J. Environ. Res. Public Health 2022, 19, 15462. https://doi.org/10.3390/ijerph192315462
Zhang Z, Mao Y, Shui Y, Deng R, Hu Y. Do Community Home-Based Elderly Care Services Improve Life Satisfaction of Chinese Older Adults? An Empirical Analysis Based on the 2018 CLHLS Dataset. International Journal of Environmental Research and Public Health. 2022; 19(23):15462. https://doi.org/10.3390/ijerph192315462
Chicago/Turabian StyleZhang, Zhao, Yihua Mao, Yueyao Shui, Ruyu Deng, and Yuchen Hu. 2022. "Do Community Home-Based Elderly Care Services Improve Life Satisfaction of Chinese Older Adults? An Empirical Analysis Based on the 2018 CLHLS Dataset" International Journal of Environmental Research and Public Health 19, no. 23: 15462. https://doi.org/10.3390/ijerph192315462
APA StyleZhang, Z., Mao, Y., Shui, Y., Deng, R., & Hu, Y. (2022). Do Community Home-Based Elderly Care Services Improve Life Satisfaction of Chinese Older Adults? An Empirical Analysis Based on the 2018 CLHLS Dataset. International Journal of Environmental Research and Public Health, 19(23), 15462. https://doi.org/10.3390/ijerph192315462





