Study Regarding the Optimal Dimension of Intraoral Bitewing Radiographs in Patients with Primary Dentition
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population, Selection Criteria, and Sample Size
2.2. Data Collection, Research Systematics, and Study Variables
2.2.1. Phase I: Determining Tooth Dimensions by Radiographic Analysis after the Bitewing Technique
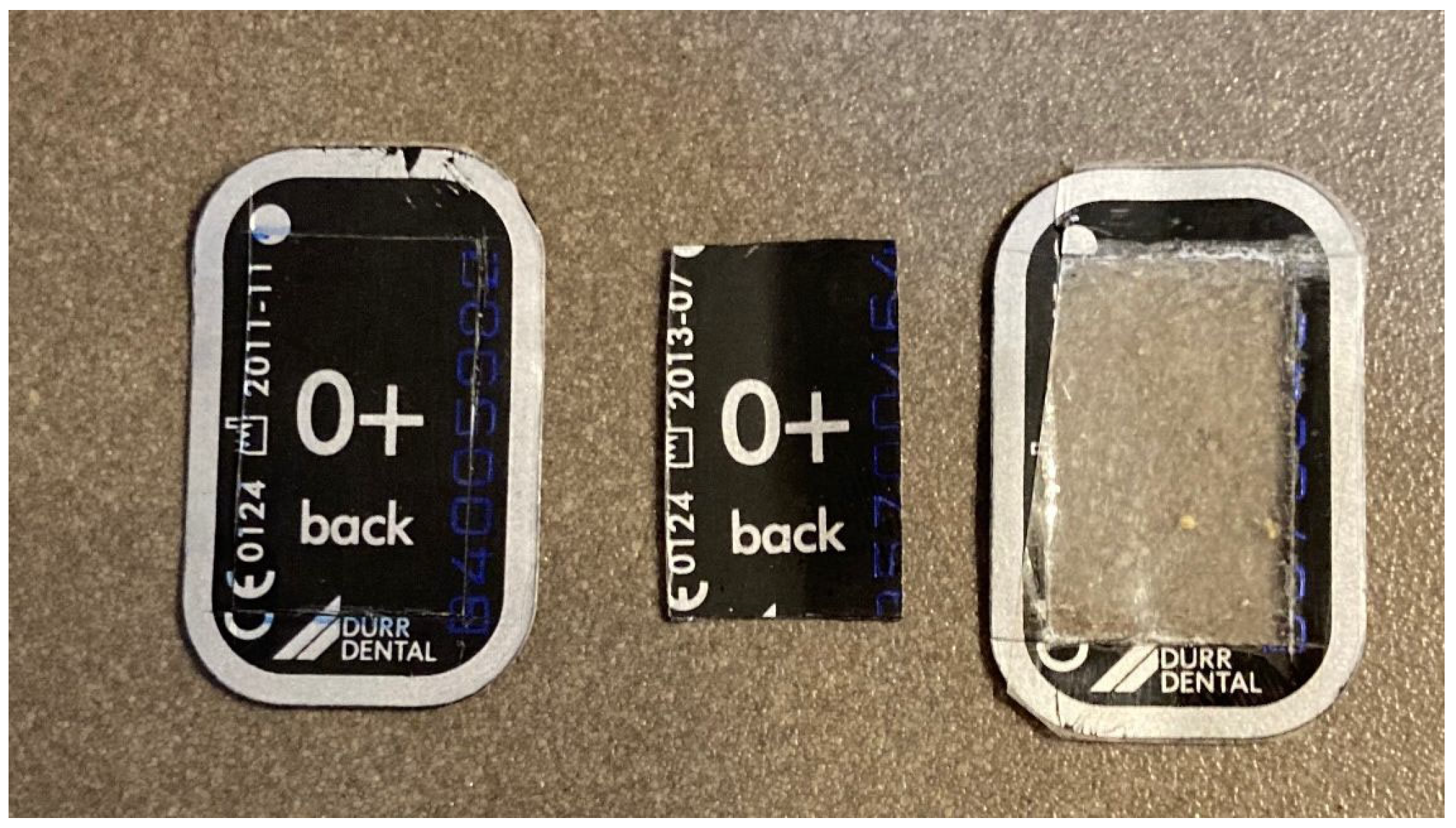
2.2.2. Phase II: Determining the Suitability of the Trimmed Plate
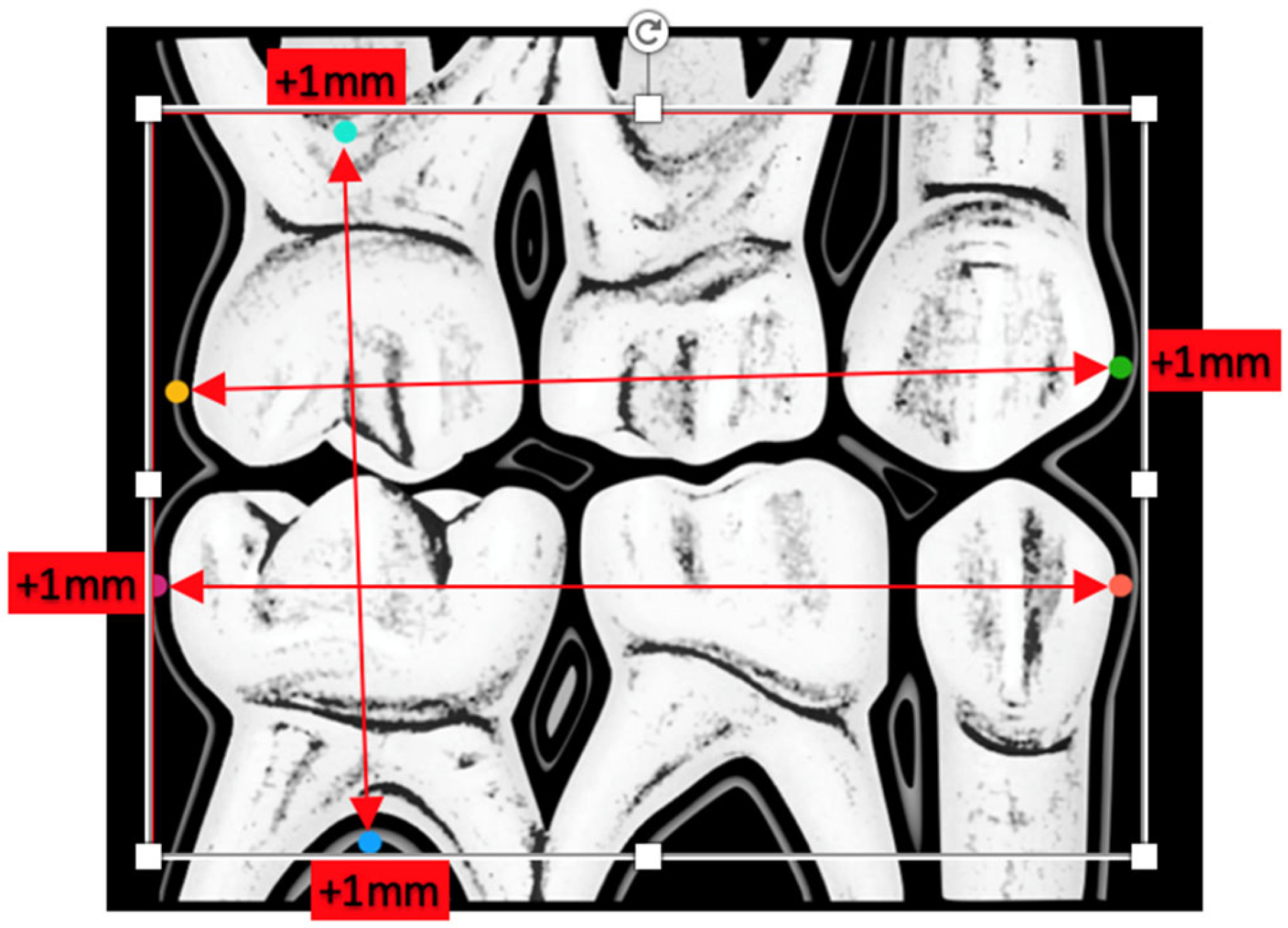
- Anatomical dimensions of the following teeth 55, 54, 53, 63, 64, 65, 75, 74, 73, 83, 84, and 85, as shown in Figure 1. The measurements of the radiographic variables were carried out in duplicate, thus calculating the intraclass correlation coefficient between both measurements to evaluate the intraobserver reproducibility (phase I);
- Visualization of the coronal portion of the teeth under study and furcation of all primary molars (phase I vs. phase II);
- Presence of ischemia in the areas close to the radiographic plate (phase I vs. phase II);
- Presence or absence of gag reflex (phase I vs. phase II);
- Acceptance/refusal of the radiographic technique by the pediatric patient (phase I vs. phase II).
2.3. Statistical Analysis
3. Results
3.1. Optimal Radiographic Plate Size
3.2. Comparison of Phase I vs. II
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sabbadini, G.D. A Review of Pediatric Radiology. J. Calif. Dent. Assoc. 2013, 41, 575–581. [Google Scholar] [PubMed]
- Anwar, A.; Keightley, A.J.; Roebuck, E.M.; Turner, S. The Value of Bitewing Radiographs in the Management of Carious Primary Molars. Br. Dent. J. 2021, 231, 575–579. [Google Scholar] [CrossRef]
- Kühnisch, J.; Anttonen, V.; Duggal, M.S.; Spyridonos, M.L.; Rajasekharan, S.; Sobczak, M.; Stratigaki, E.; Van Acker, J.W.E.; Aps, J.K.M.; Horner, K.; et al. Best Clinical Practice Guidance for Prescribing Dental Radiographs in Children and Adolescents: An EAPD Policy Document. Eur. Arch. Paediatr. Dent. 2020, 21, 375–386. [Google Scholar] [CrossRef]
- Ashkenazi, M.; Bijaoui, E.; Blumer, S.; Gordon, M. Common Mistakes, Negligence and Legal Offences in Paediatric Dentistry: A Self-Report. Eur. Arch. Paediatr. Dent. 2011, 12, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Katsouda, M.; Coolidge, T.; Simos, G.; Kotsanos, N.; Arapostathis, K.N. Factors Associated with Gagging during Radiographic and Intraoral Photographic Examinations in 4–12-Year-Old Children. Eur. Arch. Paediatr. Dent. 2021, 22, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Mesut, E.; Önjen, T.; Ülkü, Ş.E.; Can, K.; Kubilay, E. The Use of Low-Level Laser Therapy for Controlling the Gag Reflex in Children during Intraoral Radiography. Lasers Med. Sci. 2016, 3, 355–361. [Google Scholar]
- Rahul, K.; Neha, K.; Ekta, P. Extraoral Periapical Radiography: An Alternative Approach to Intraoral Periapical Radiography. Imaging Sci. Dent. 2011, 41, 161–165. [Google Scholar]
- Schwartz, S. Radiographic Techniques for the Pediatric Patient. J. Contemp. Dent. Pract. 2000, 1, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Abu-Saad, H. Assessing Children’s Responses to Pain. Pain 1984, 19, 163–171. [Google Scholar] [CrossRef]
- Herman, H.D.; Ashkenazi, M. Quality of Bitewing Radiographs in Children in Relation to the Type of Film Holder Used. Eur. Arch. Paediatr. Dent. 2013, 14, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Pierro, V.S.; Barcelos, R.; de Souza, I.P.; Raymundo, R.J. Pediatric Bitewing Film Holder: Preschoolers’ Acceptance and Radiographs’ Diagnostic Quality. Pediatr. Dent. 2008, 30, 342–347. [Google Scholar] [PubMed]
- Ozdemir, S.; Parlakyıldız Gokce, A.; Unver, T. Simulation of Three Intraoral Radiographic Techniques in Pediatric Dental Patients: Subjective Comfort Assessment Using the VAS and Wong-Baker FACES Pain Raiting Scale. BMC Oral Health 2020, 20, 33. [Google Scholar] [CrossRef] [PubMed]
- Katsouda, M.; Coolidge, T.; Simos, G.; Kotsanos, N. Gagging and Cooperation in 4–12-year-old Children over a Series of Dental Appointments. Eur. Arch. Paediatr. Dent. 2021, 22, 937–946. [Google Scholar] [CrossRef] [PubMed]
- Katsouda, M.; Provatenou, E.; Arapostathis, K.; Coolidge, T.; Kotsanos, N. The Greek Version of the Gagging Assessment Scale in Children and Adolescents: Psychometric Properties, Prevalence of Gagging, and the Association between Gagging and Dental Fear. Int. J. Paediatr. Dent. 2017, 27, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Goel, H.; Mathur, S.; Sandhu, M.; Jhingan, P.; Sachdev, V. Effect of Low-Level LASER Therapy on P6 Acupoint to Control Gag Reflex in Children: A Clinical Trial. Acupunct. Meridian Stud. 2017, 10, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Ateet, K.; Sarah, S.A.; Reem, A.A.; Eman, I.A.; Afnan, M.A. Knowledge on Patient Gag Reflex among Pedodontists in Saudi Arabia. J. Adv. Med. Dent. Sci. Res. 2020, 8, 9–10. [Google Scholar]
- Eachempati, P.; Kumbargere, N.S.; Kiran, K.; Krishanappa, S.; George, R.P.; Soe, H.H.K.; Karanth, L. Management of Gag Reflex for Patients Undergoing Dental Treatment. Cochrane Database Syst. Rev. 2019, 11, CD011116. [Google Scholar]
- Behavior Guidance for the Pediatric Dental Patient. Pediatr. Dent. 2017, 39, 246–259.
| Category | Height | Width |
|---|---|---|
| n | 40 | 40 |
| Mean | 18.16 | 24.04 |
| Standard deviation (SD) | 1.49 | 1.62 |
| Minimum | 13.45 | 20.75 |
| p25 | 17.47 | 23.15 |
| p50 | 18.37 | 23.85 |
| p75 | 18.75 | 25.07 |
| p90 | 19.47 | 26.3 |
| Maximum | 22.5 | 27.6 |
| p normality test | 0.0156 | 0.2907 |
| Optimal dimension 1 | 19.48 | 27.27 |
| Visualization of Dental Tissues on the Left | Visualization of Dental Tissues on the Right | ||||||
|---|---|---|---|---|---|---|---|
| Total | |||||||
| Category | n | % | IC 95% | Category | n | % | IC 95% |
| No | 10 | 12.5 | No | 17 | 21.25 | ||
| Yes | 70 | 87.5 | 80.25–94.75 | Yes | 63 | 78.75 | 69.79–87.71 |
| Total | 80 | 100 | Total | 80 | 100 | ||
| Phase I | |||||||
| Category | n | % | IC 95% | Category | n | % | IC 95% |
| No | 5 | 12.5 | No | 10 | 25 | ||
| Yes | 35 | 87.5 | 77.25–97.75 | Yes | 30 | 75 | 61.58–88.42 |
| Total | 40 | 100 | Total | 40 | 100 | ||
| Phase II | |||||||
| Category | n | % | IC 95% | Category | n | % | IC 95% |
| No | 5 | 12.5 | No | 7 | 17.5 | ||
| Yes | 35 | 87.5 | 77.25–97.75 | Yes | 33 | 82.5 | 70.72–94.28 |
| Total | 40 | 100 | Total | 40 | 100 | ||
| Chi-square test (p = 1) | Chi-square test (p = 0.412) | ||||||
| Total | |||
|---|---|---|---|
| Category | n | % | IC 95% |
| No | 42 | 52.5 | |
| Yes | 38 | 47.5 | 36.56–58.44 |
| Total | 80 | 100 | |
| Phase I | |||
| Category | n | % | IC 95% |
| No | 2 | 5 | |
| Yes | 38 | 95 | 88.25–100 |
| Phase II | |||
| Category | n | % | IC 95% |
| No | 40 | 100 | |
| Yes | 0 | 0 | 0–0 |
| Chi-square test (p < 0.001) | |||
| Total | |||
|---|---|---|---|
| Category | n | % | IC 95% |
| No | 44 | 55 | |
| Yes | 36 | 45 | 34.10–55.90 |
| Total | 80 | 100 | |
| Phase I | |||
| Category | n | % | IC 95% |
| No | 4 | 10 | |
| Yes | 36 | 90 | 80.70–99.30 |
| Phase II | |||
| Category | n | % | IC 95% |
| No | 40 | 100 | |
| Yes | 0 | 0 | 0–0 |
| Chi-square test (p < 0.001) | |||
| Total | |||
|---|---|---|---|
| Category | n | % | IC 95% |
| No | 42 | 52.5 | |
| Yes | 38 | 47.5 | 36.56–58.44 |
| Total | 80 | 100 | |
| Phase I | |||
| Category | n | % | IC 95% |
| No | 2 | 5 | |
| Yes | 38 | 95 | 88.25–100.00 |
| Phase II | |||
| Category | n | % | IC 95% |
| No | 40 | 100 | |
| Yes | 0 | 0 | 0–0 |
| Chi-square test (p < 0.001) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diéguez-Pérez, M.; Lacalle-Muñoz de Cuerva, C.; Costa-Ferrer, F.; Muñoz-Corcuera, M. Study Regarding the Optimal Dimension of Intraoral Bitewing Radiographs in Patients with Primary Dentition. Int. J. Environ. Res. Public Health 2022, 19, 15413. https://doi.org/10.3390/ijerph192215413
Diéguez-Pérez M, Lacalle-Muñoz de Cuerva C, Costa-Ferrer F, Muñoz-Corcuera M. Study Regarding the Optimal Dimension of Intraoral Bitewing Radiographs in Patients with Primary Dentition. International Journal of Environmental Research and Public Health. 2022; 19(22):15413. https://doi.org/10.3390/ijerph192215413
Chicago/Turabian StyleDiéguez-Pérez, Montserrat, Concepción Lacalle-Muñoz de Cuerva, Fernando Costa-Ferrer, and Marta Muñoz-Corcuera. 2022. "Study Regarding the Optimal Dimension of Intraoral Bitewing Radiographs in Patients with Primary Dentition" International Journal of Environmental Research and Public Health 19, no. 22: 15413. https://doi.org/10.3390/ijerph192215413
APA StyleDiéguez-Pérez, M., Lacalle-Muñoz de Cuerva, C., Costa-Ferrer, F., & Muñoz-Corcuera, M. (2022). Study Regarding the Optimal Dimension of Intraoral Bitewing Radiographs in Patients with Primary Dentition. International Journal of Environmental Research and Public Health, 19(22), 15413. https://doi.org/10.3390/ijerph192215413






