What Is Next for Public Health after COVID-19 in Italy? Adopting a Youth-Centred Care Approach in Mental Health Services
Abstract
1. Introduction
2. Materials and Methods
3. Results
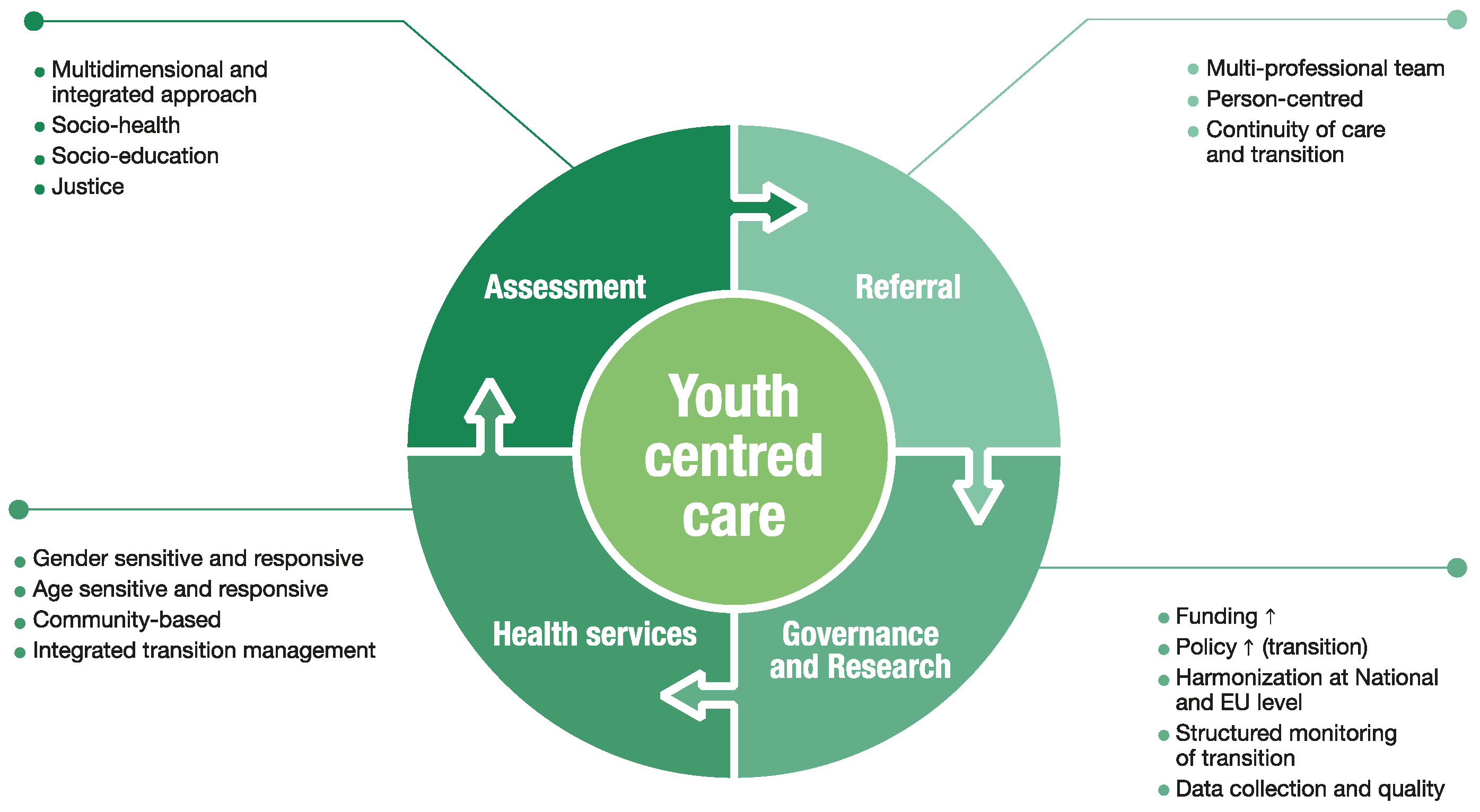
Addressing Mental Health Gaps among Young People in a Post-COVID-19 Era
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sawyer, S.M.; Azzopardi, P.S.; Wickremarathne, D.; Patton, G.C. The age of adolescence. Lancet Child Adolesc. Health 2018, 2, 223–228. [Google Scholar] [CrossRef]
- Castelpietra, G.; Knudsen, A.K.S.; Agardh, E.E.; Armocida, B.; Beghi, M.; Iburg, K.M.; Logroscino, G.; Ma, R.; Starace, F.; Steel, N.; et al. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990–2019: Findings from the Global Burden of Disease Study 2019. Lancet Reg. Health Eur. 2022, 16, 100341. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Armocida, B.; Monasta, L.; Sawyer, S.; Bustreo, F.; Segafredo, G.; Castelpietra, G.; Ronfani, L.; Pasovic, M.; Hay, S.; Perel, P.; et al. Burden of non-communicable diseases among adolescents aged 10–24 years in the EU, 1990–2019: A systematic analysis of the Global Burden of Diseases Study 2019. Lancet Child Adolesc. Health 2022, 6, 367–383. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for Europe. WHO European Framework for Action on Mental Health (EFAMH) 2021–2025. Available online: https://www.who.int/europe/publications/i/item/9789289057813 (accessed on 10 November 2022).
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef] [PubMed]
- Presidenza del Consiglio dei Ministri. Conferenza Unificata. Linee di Indirizzo per i Disturbi Neuropsichici Dell’età Evolutiva. 25 July 2019. Available online: https://www.salute.gov.it/imgs/C_17_pagineAree_5621_0_file.pdf (accessed on 10 November 2022).
- Petruzzelli, M.G.; Furente, F.; Colacicco, G.; Annecchini, F.; Margari, A.; Gabellone, A.; Margari, L.; Matera, E. Implication of COVID-19 Pandemic on Adolescent Mental Health: An Analysis of the Psychiatric Counseling from the Emergency Room of an Italian University Hospital in the Years 2019–2021. J. Clin. Med. 2022, 11, 6177. [Google Scholar] [CrossRef] [PubMed]
- Malerba, A.; Iannattone, S.; Casano, G.; Lauriola, M.; Bottesi, G. The Trap of the COVID-19 Pandemic: Italian Adolescents Fare Well at First, Maybe Thanks to Protective Trait Expression. Children 2022, 9, 1631. [Google Scholar] [CrossRef]
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet Psychiatry 2021, 9, 137–150. [Google Scholar]
- Amendola, S. Burden of mental health and substance use disorders among Italian young people aged 10–24 years: Results from the Global Burden of Disease 2019 Study. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 683–694. [Google Scholar] [CrossRef] [PubMed]
- Hafstad, G.S.; Augusti, E.-M. A lost generation? COVID-19 and adolescent mental health. Lancet Psychiatry 2021, 8, 640–641. [Google Scholar] [CrossRef]
- Kilicel, D.; De Crescenzo, F.; Barbe, R.; Edan, A.; Curtis, L.; Singh, S.; Micali, N.; Aubry, J.-M.; Mégevand, J.; Eliez, S.; et al. Mapping Child and Adolescent Mental Health Services and the Interface During Transition to Adult Services in Six Swiss Cantons. Front. Psychiatry 2022, 13, 814147. [Google Scholar] [CrossRef] [PubMed]
- Moitra, M.; Santomauro, D.; Degenhardt, L.; Collins, P.Y.; Whiteford, H.; Vos, T.; Ferrari, A. Estimating the risk of suicide associated with mental disorders: A systematic review and meta-regression analysis. J. Psychiatr. Res. 2021, 137, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Lorenzoni, G.; Azzolina, D.; Maresio, E.; Gallipoli, S.; Ghidina, M.; Baldas, S.; Berchialla, P.; Giron, M.C.; Silano, M.; Gregori, D. Impact of the COVID-19 lockdown on psychological health and nutritional habits in Italy: Results from the #PRESTOinsieme study. BMJ Open 2022, 12, e048916. [Google Scholar] [CrossRef] [PubMed]
- Bonus Psicologo 2022, Come Richiederlo, a Chi Spetta e Come Funziona. Available online: https://www.agendadigitale.eu/documenti/bonus-psicologo-cose-come-funziona-e-come-ottenere-i-600-euro/ (accessed on 10 November 2022).
- “Aiutamente Giovani”: 10,9 Mln per Tutela Salute Mentale e Prevenzione Disagio Psichico. Available online: https://www.regione.lazio.it/notizie/Aiutamente%20giovani-10-9-mln-tutela-salute-mentale-prevenzione-disagio-psichico (accessed on 10 November 2022).
- Il Friuli Venezia Giulia Introduce lo Psicologo di Base. Available online: https://www.udinetoday.it/politica/fvg-psicologo-base-servizio-pubblico.html (accessed on 10 November 2022).
- Bonus Psicologo: Contributi per Uscire dalle Difficoltà Create dalla Pandemia. Available online: https://www.regione.lombardia.it/wps/portal/istituzionale/HP/DettaglioRedazionale/istituzione/delegazioni/roma/bonus-psicologo-pandemia/bonus-psicologo-pandemia (accessed on 10 November 2022).
- D.A. n. 662 Dell’ 8 July 2021. Available online: https://www.regione.sicilia.it/istituzioni/servizi-informativi/decreti-e-direttive/n-662-08072021 (accessed on 10 November 2022).
- Presidenza del Consiglio dei Ministri. Dipartimento per le Politiche della Famiglia. 5° Piano Nazionale di Azione e di Interventi per la Tutela dei Diritti e lo Sviluppo dei Soggetti in Età Evolutiva 2022–2023 Educazione, Equità, Empowerment. May 2021. Available online: https://famiglia.governo.it/media/2636/v-piano-nazionale-infanzia-e-adolescenza-gennaio-2022.pdf (accessed on 10 November 2022).
- Otto Italiani su 10 a Favore dello Psicologo Obbligatorio in Ogni Scuola. Available online: https://www.ilsole24ore.com/art/otto-italiani-10-favore-psicologo-obbligatorio-ogni-scuola-AE7vGdp?refresh_ce=1 (accessed on 10 November 2022).
- Ministero della Salute. Piano di Azioni Nazionale per la Salute Mentale 2013–2020. 24 January 2013. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_1905_allegato.pdf (accessed on 10 November 2022).
- Salute Mentale. Pronte le Nuove Linee D’indirizzo del Ministero. Ecco gli Obiettivi per le Regioni. Available online: https://www.quotidianosanita.it/governo-e-parlamento/articolo.php?articolo_id=103208 (accessed on 10 November 2022).
- Muzi, S.; Sansò, A.; Pace, C.S. What’s Happened to Italian Adolescents During the COVID-19 Pandemic? A Preliminary Study on Symptoms, Problematic Social Media Usage, and Attachment: Relationships and Differences with Pre-pandemic Peers. Front. Psychiatry 2021, 12, 590543. [Google Scholar] [CrossRef] [PubMed]
- Signorini, G.; Singh, S.P.; Marsanic, V.B.; Dieleman, G.; Dodig-Ćurković, K.; Franic, T.; Gerritsen, S.E.; Griffin, J.; Maras, A.; McNicholas, F.; et al. The interface between child/adolescent and adult mental health services: Results from a European 28-country survey. Eur. Child Adolesc. Psychiatry 2018, 27, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.P.; Tuomainen, H.; Warwick, J.; de Girolamo, G.; Maras, A.; Santosh, P.; McNicholas, F.; Schulze, U.; Purper-Ouakil, D.; Tremmery, S.; et al. Protocol for a cohort study of adolescent mental health service users with a nested cluster-randomised controlled trial to assess the clinical and cost effectiveness of managed transition in improving transitions from child to adult mental health services (The MILESTONE study). BMJ Open 2017, 7, e016055. [Google Scholar] [PubMed]
- Patton, G.C.; Sawyer, S.M.; Santelli, J.S.; Ross, D.A.; Afifi, R.; Allen, N.B.; Arora, M.; Azzopardi, P.; Baldwin, W.; Bonell, C.; et al. Our future: A Lancet commission on adolescent health and wellbeing. Lancet 2016, 387, 2423–2478. [Google Scholar] [CrossRef]
- Il Piano Nazionale di Ripresa e Resilienza (PNRR). Available online: https://temi.camera.it/leg18/temi/piano-nazionale-di-ripresa-e-resilienza.html (accessed on 10 November 2022).
- Indirizzi e Indicazioni per le Aziende Ulss del Veneto per L’implementazione del Servizio “Unità Funzionale Distrettuale Adolescenti–UFDA”. L. n. 106 Del 23 luglio. 2021. Available online: https://bur.regione.veneto.it/BurvServices/Pubblica/DettaglioDgr.aspx?id=457329 (accessed on 10 November 2022).
- Lepiece, B.; Patigny, P.; Dubois, T.; Jacques, D.; Zdanowicz, N. Improving Transition from Child and Adolescent Mental Health Services to Adult Mental Health Services for Adolescents in Transition to Young Adulthood: A Literature Review. Psychiatr. Danub. 2020, 32, 153–157. [Google Scholar] [PubMed]
- Dunn, V. Young people, mental health practitioners and researchers co-produce a Transition Preparation Programme to improve outcomes and experience for young people leaving Child and Adolescent Mental Health Services (CAMHS). BMC Health Serv. Res. 2017, 17, 293. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ussai, S.; Castelpietra, G.; Mariani, I.; Casale, A.; Missoni, E.; Pistis, M.; Monasta, L.; Armocida, B. What Is Next for Public Health after COVID-19 in Italy? Adopting a Youth-Centred Care Approach in Mental Health Services. Int. J. Environ. Res. Public Health 2022, 19, 14937. https://doi.org/10.3390/ijerph192214937
Ussai S, Castelpietra G, Mariani I, Casale A, Missoni E, Pistis M, Monasta L, Armocida B. What Is Next for Public Health after COVID-19 in Italy? Adopting a Youth-Centred Care Approach in Mental Health Services. International Journal of Environmental Research and Public Health. 2022; 19(22):14937. https://doi.org/10.3390/ijerph192214937
Chicago/Turabian StyleUssai, Silvia, Giulio Castelpietra, Ilaria Mariani, Andrea Casale, Eduardo Missoni, Marco Pistis, Lorenzo Monasta, and Benedetta Armocida. 2022. "What Is Next for Public Health after COVID-19 in Italy? Adopting a Youth-Centred Care Approach in Mental Health Services" International Journal of Environmental Research and Public Health 19, no. 22: 14937. https://doi.org/10.3390/ijerph192214937
APA StyleUssai, S., Castelpietra, G., Mariani, I., Casale, A., Missoni, E., Pistis, M., Monasta, L., & Armocida, B. (2022). What Is Next for Public Health after COVID-19 in Italy? Adopting a Youth-Centred Care Approach in Mental Health Services. International Journal of Environmental Research and Public Health, 19(22), 14937. https://doi.org/10.3390/ijerph192214937






