Schizophrenia Assessment, Referral and Awareness Training for Health Auxiliaries (SARATHA): Protocol for a Mixed-Methods Pilot Study in Rural India
Abstract
1. Introduction
Study Objectives
2. Methods
2.1. Setting
2.2. Participants for the Training Program
2.3. Study Design
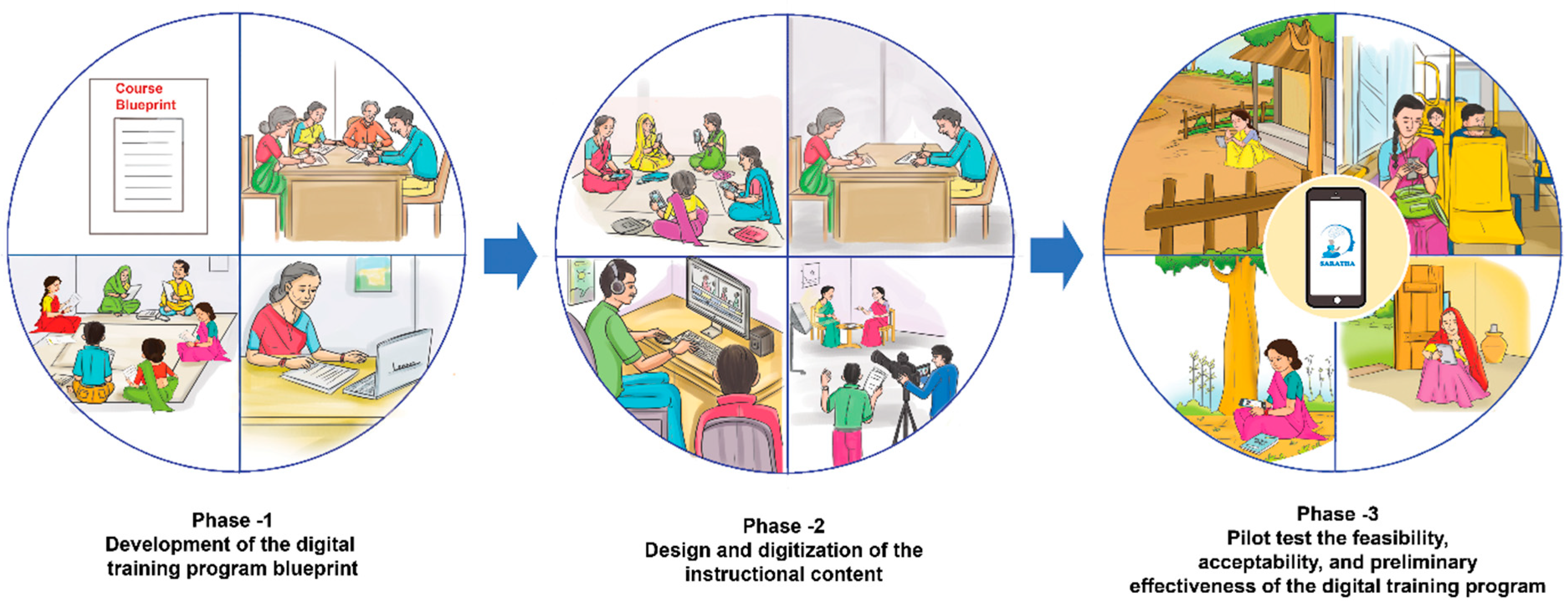
2.3.1. Phase 1—Development of the Digital Training Program Curriculum
2.3.2. Phase 2—Design and Digitization of the Instructional Content
2.3.3. Phase 3—Pilot Test the Feasibility, Acceptability, and Preliminary Effectiveness of the Digital Training Program
2.4. Evidence-Based Content to Adapt for the Training Program
2.5. Ethical Approval
3. Discussion
Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gautham, M.S.; Gururaj, G.; Varghese, M.; Benegal, V.; Rao, G.N.; Kokane, A.; Chavan, B.S.; Dalal, P.K.; Ram, D.; Pathak, K.; et al. The National Mental Health Survey of India (2016): Prevalence, socio-demographic correlates and treatment gap of mental morbidity. Int. J. Soc. Psychiatry 2020, 66, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Kokane, A.; Pakhare, A.; Gururaj, G.; Varghese, M.; Benegal, V.; Rao, G.N.; Arvind, B.; Shukla, M.; Mitra, A.; Yadav, K.; et al. Mental health issues in Madhya Pradesh: Insights from national mental health survey of India 2016. Healthcare 2019, 7, 53. [Google Scholar] [CrossRef] [PubMed]
- Sagar, R.; et al. The burden of mental disorders across the states of India: The Global Burden of Disease Study 1990–2017. Lancet Psychiatry 2020, 7, 148–161. [Google Scholar] [CrossRef]
- Walker, E.R.; McGee, R.E.; Druss, B.G. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry 2015, 72, 334–341. [Google Scholar] [CrossRef]
- Liu, N.H.; Daumit, G.L.; Dua, T.; Aquila, R.; Charlson, F.; Cuijpers, P.; Druss, B.; Dudek, K.; Freeman, M.; Fujii, C.; et al. Excess mortality in persons with severe mental disorders: A multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry 2017, 16, 30–40. [Google Scholar] [CrossRef]
- Koschorke, M.; Padmavati, R.; Kumar, S.; Cohen, A.; Weiss, H.A.; Chatterjee, S.; Pereira, J.; Naik, S.; John, S.; Dabholkar, H.; et al. Experiences of stigma and discrimination faced by family caregivers of people with schizophrenia in India. Soc. Sci. Med. 2017, 178, 66–77. [Google Scholar] [CrossRef]
- Keshavan, M.S.; Shrivastava, A.; Gangadhar, B.N. Gangadhar, Early intervention in psychotic disorders: Challenges and relevance in the Indian context. Indian J. Psychiatry 2010, 52, S153. [Google Scholar] [CrossRef]
- Raviola, G.; Naslund, J.A.; Smith, S.L.; Patel, V. Innovative models in mental health delivery systems: Task sharing care with non-specialist providers to close the mental health treatment gap. Curr. Psychiatry Rep. 2019, 21, 1–13. [Google Scholar] [CrossRef]
- Barnett, M.L.; Gonzalez, A.; Miranda, J.; Chavira, D.A.; Lau, A.S. Mobilizing community health workers to address mental health disparities for underserved populations: A systematic review. Adm. Policy Ment. Health Ment. Health Serv. Res. 2018, 45, 195–211. [Google Scholar] [CrossRef]
- Singla, D.R.; Kohrt, B.A.; Murray, L.K.; Anand, A.; Chorpita, B.F.; Patel, V. Psychological treatments for the world: Lessons from low- and middle-income countries. Annu. Rev. Clin. Psychol. 2017, 13, 149–181. [Google Scholar] [CrossRef]
- World Health Organization. mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme (mhGAP); World Health Organization (WHO): Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization. Community-Based Rehabilitation: CBR Guidelines; World Health Organization (WHO): Geneva, Switzerland, 2010; p. 67. [Google Scholar]
- Asher, L.; Patel, V.; De Silva, M.J. Community-based psychosocial interventions for people with schizophrenia in low and middle-income countries: Systematic review and meta-analysis. BMC Psychiatry 2017, 17, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, S.; Naik, S.; John, S.; Dabholkar, H.; Balaji, M.; Koschorke, M.; Varghese, M.; Thara, R.; Weiss, H.A.; Williams, P.; et al. Effectiveness of a community-based intervention for people with schizophrenia and their caregivers in India (COPSI): A randomised controlled trial. Lancet 2014, 383, 1385–1394. [Google Scholar] [CrossRef]
- Chatterjee, S.; Leese, M.; Koschorke, M.; McCrone, P.; Naik, S.; John, S.; Dabholkar, H.; Goldsmith, K.; Balaji, M.; Varghese, M.; et al. Collaborative community based care for people and their families living with schizophrenia in India: Protocol for a randomised controlled trial. Trials 2011, 12, 1–14. [Google Scholar] [CrossRef]
- Asher, L.; Hanlon, C.; Birhane, R.; Habtamu, A.; Eaton, J.; Weiss, H.A.; Patel, V.; Fekadu, A.; De Silva, M. Community-based rehabilitation intervention for people with schizophrenia in Ethiopia (RISE): A 12 month mixed methods pilot study. BMC Psychiatry 2018, 18, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Asher, L.; Birhane, R.; Weiss, H.A.; Medhin, G.; Selamu, M.; Patel, V.; De Silva, M.; Hanlon, C.; Fekadu, A. Community-based rehabilitation intervention for people with schizophrenia in Ethiopia (RISE): Results of a 12-month cluster-randomised controlled trial. Lancet Glob. Health 2022, 10, e530–e542. [Google Scholar] [CrossRef]
- Merchant, R.; Torous, J.; Rodriguez-Villa, E.; Naslund, J.A. Digital Technology for Management of Severe Mental Disorders in Low-and Middle-Income Countries. Curr. Opin. Psychiatry 2020, 33, 501. [Google Scholar] [CrossRef] [PubMed]
- Naslund, J.A.; Gonsalves, P.P.; Gruebner, O.; Pendse, S.R.; Smith, S.L.; Sharma, A.; Raviola, G. Digital innovations for global mental health: Opportunities for data science, task sharing, and early intervention. Curr. Treat. Options Psychiatry 2019, 6, 337–351. [Google Scholar] [CrossRef]
- Xu, D.R.; Xiao, S.; He, H.; Caine, E.D.; Gloyd, S.; Simoni, J.; Hughes, J.P.; Nie, J.; Lin, M.; He, W.; et al. Lay health supporters aided by mobile text messaging to improve adherence, symptoms, and functioning among people with schizophrenia in a resource-poor community in rural China (LEAN): A randomized controlled trial. PLoS Med. 2019, 16, e1002785. [Google Scholar] [CrossRef]
- Lilford, P.; Rajapakshe, O.B.W.; Singh, S.P. A systematic review of care pathways for psychosis in low-and middle-income countries. Asian J. Psychiatry 2020, 54, 102237. [Google Scholar] [CrossRef]
- Carter, H.; Araya, R.; Anjur, K.; Deng, D.; Naslund, J.A. The emergence of digital mental health in low-income and middle-income countries: A review of recent advances and implications for the treatment and prevention of mental disorders. J. Psychiatr. Res. 2021, 133, 223–246. [Google Scholar] [CrossRef]
- Naslund, J.A.; Aschbrenner, K.A.; Araya, R.; Marsch, L.A.; Unützer, J.; Patel, V.; Bartels, S.J. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: A narrative review of the literature. Lancet Psychiatry 2017, 4, 486–500. [Google Scholar] [CrossRef]
- Naslund, J.A.; Shidhaye, R.; Patel, V. Digital technology for building capacity of non-specialist health workers for task-sharing and scaling up mental health care globally. Harv. Rev. Psychiatry 2019, 27, 181. [Google Scholar] [CrossRef] [PubMed]
- Census Organization of India. Madhya Pradesh Population 2011–2022. 2011. Available online: https://www.census2011.co.in/census/state/madhya+pradesh.html (accessed on 29 September 2022).
- Suryanarayana, M.H.; Agrawal, A.; Seeta Prabhu, K. Inequality-Adjusted Human Development Index for India’s States 2011; United Nations Development Programme: New Delhi, India, 2011; Available online: https://www.undp.org/india/publications/inequality-adjusted-human-development-index-india%E2%80%99s-states (accessed on 8 November 2022).
- Menon, P.; Deolalikar, A.B.; Bhaskar, A. The India State Hunger Index: Comparisons of Hunger Across States; Welthungerhilfe: Bonn, Germany, 2008. [Google Scholar]
- Shidhaye, R.; Baron, E.; Murhar, V.; Rathod, S.; Khan, A.; Singh, A.; Shrivastava, S.; Muke, S.; Shrivastava, R.; Lund, C.; et al. Community, facility and individual level impact of integrating mental health screening and treatment into the primary healthcare system in Sehore district, Madhya Pradesh, India. BMJ Glob. Health 2019, 4, e001344. [Google Scholar] [CrossRef]
- Shidhaye, R.; Murhar, V.; Muke, S.; Shrivastava, R.; Khan, A.; Singh, A.; Breuer, E. Delivering a complex mental health intervention in low-resource settings: Lessons from the implementation of the PRIME mental healthcare plan in primary care in Sehore district, Madhya Pradesh, India. BJPsych Open 2019, 5, e63. [Google Scholar] [CrossRef]
- Naslund, J.A.; Tugnawat, D.; Anand, A.; Cooper, Z.; Dimidjian, S.; Fairburn, C.G.; Hollon, S.D.; Joshi, U.; Khan, A.; Lu, C.; et al. Digital training for non-specialist health workers to deliver a brief psychological treatment for depression in India: Protocol for a three-arm randomized controlled trial. Contemp. Clin. Trials 2021, 102, 106267. [Google Scholar] [CrossRef]
- Rodriguez-Villa, E.; Mehta, U.M.; Naslund, J.; Tugnawat, D.; Gupta, S.; Thirtalli, J.; Bhan, A.; Patel, V.; Chand, P.K.; Rozatkar, A.; et al. Smartphone Health Assessment for Relapse Prevention (SHARP): A digital solution toward global mental health. BJPsych Open 2021, 7, e29. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Villa, E.; Naslund, J.; Keshavan, M.; Patel, V.; Torous, J. Making mental health more accessible in light of COVID-19: Scalable digital health with digital navigators in low and middle-income countries. Asian J. Psychiatry 2020, 54, 102433. [Google Scholar] [CrossRef]
- Rodriguez-Villa, E.; Rozatkar, A.R.; Kumar, M.; Patel, V.; Bondre, A.; Naik, S.S.; Dutt, S.; Mehta, U.M.; Nagendra, S.; Tugnawat, D.; et al. Cross cultural and global uses of a digital mental health app: Results of focus groups with clinicians, patients and family members in India and the United States. Glob. Ment. Health 2021, 8, e30. [Google Scholar] [CrossRef]
- Bondre, A.P.; Shrivastava, R.; Raghuram, H.; Tugnawat, D.; Khan, A.; Gupta, S.; Kumar, M.; Mehta, U.M.; Keshavan, M.; Lakhtakia, T.; et al. A qualitative exploration of perceived needs and barriers of individuals with schizophrenia, caregivers and clinicians in using mental health applications in Madhya Pradesh, India. SSM-Ment. Health 2022, 2, 100063. [Google Scholar] [CrossRef]
- Lakhtakia, T.; Bondre, A.; Chand, P.K.; Chaturvedi, N.; Choudhary, S.; Currey, D.; Dutt, S.; Khan, A.; Kumar, M.; Gupta, S.; et al. Smartphone digital phenotyping, surveys, and cognitive assessments for global mental health: Initial data and clinical correlations from an international first episode psychosis study. Digit. Health 2022, 8, 1–18. [Google Scholar] [CrossRef]
- Scott, K.; George, A.S.; Ved, R.R. Taking stock of 10 years of published research on the ASHA programme: Examining India’s national community health worker programme from a health systems perspective. Health Res. Policy Syst. 2019, 17, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Shrivastava, R.; Tugnawat, D.; Singh, A.; Dimidjian, S.; Patel, V.; Bhan, A.; Naslund, J.A. Design and development of a digital program for training non-specialist health workers to deliver an evidence-based psychological treatment for depression in primary care in India. J. Technol. Behav. Sci. 2020, 5, 402–415. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Morrison, L.; Bradbury, K.; Muller, I. The person-based approach to intervention development: Application to digital health-related behavior change interventions. J. Med. Internet Res. 2015, 17, e4055. [Google Scholar] [CrossRef] [PubMed]
- Kruse, K. Introduction to instructional design and the ADDIE model. Retrieved Jan. 2002, 26, 2005. [Google Scholar]
- Shelton, K.; Saltsman, G. Applying the ADDIE Model to Online Instruction, in Instructional Design: Concepts, Methodologies, Tools and Applications; IGI Global: Hershey, PA, USA, 2011; pp. 566–582. [Google Scholar]
- Chatterjee, S. A Manual for Working with People with Schizophrenia and Their Families; COPSI: Community Care for People with Schizophrenia in India; Sangath: Goa, India, 2012; Available online: http://www.sangath.in/wp-content/uploads/2018/03/COPSI_Manual_Nov_19.pdf (accessed on 20 June 2022).
- Department of Empowerment of Persons with Disabilities (Divyangjan). 2022. Available online: https://disabilityaffairs.gov.in/ (accessed on 30 September 2022).
- Chowdhary, N.; Dabholkar, H.; Velleman, R.; Dimidjian, S.; Fairburn, C.; Patel, V. The Premium Counselling Relationship Manual. 2013. Available online: https://www.sangath.in/wp-content/uploads/2018/03/Counselling-Relationship_Manual.pdf (accessed on 5 October 2021).
- Basavarajappa, C.; Ahamed, A.; Desai, G.; Chaturvedi, S. Nuts and Bolts of Starting and Running Psychiatric Rehabilitation Services; National Institute of Mental Health and Neurosciences (NIMHANS): Bengaluru, India, 2016. [Google Scholar]
- Joshi, U.; Khan, A.; Muke, S.; Choubey, S.; Tugnawat, D.; Naslund, J.A.; Bhan, A. Development and implementation of COVID-19 safety protocols for conducting a randomized trial in global mental health: Field report from Central India. Asian J. Psychiatry 2021, 63, 102750. [Google Scholar] [CrossRef]
- Muke, S.S.; Shrivastava, R.D.; Mitchell, L.M.; Khan, A.; Murhar, V.; Tugnawat, D.; Shidhaye, R.; Patel, V.; Naslund, J.A. Acceptability and feasibility of digital technology for training community health workers to deliver brief psychological treatment for depression in rural India. Asian J. Psychiatry 2019, 45, 99–106. [Google Scholar] [CrossRef]
- Muke, S.; Tugnawat, D.; Joshi, U.; Anand, A.; Khan, A.; Shrivastava, R.; Singh, A.; Restivo, J.; Bhan, A.; Patel, V.; et al. Digital training for non-specialist health workers to deliver a brief psychological treatment for depression in primary care in India: Findings from a randomized pilot study. Int. J. Environ. Res. Public Health 2020, 17, 6368. [Google Scholar] [CrossRef]
- Restivo, J.L.; Mitchell, L.; Joshi, U.; Anand, A.; Gugiu, P.C.; Singla, D.R.; Hollon, S.D.; Patel, V.; Naslund, J.A.; Cooper, Z. Assessing health worker competence to deliver a brief psychological treatment for depression: Development and validation of a scalable measure. J. Behav. Cogn. Ther. 2020, 30, 253–266. [Google Scholar] [CrossRef]
- National Health Mission. Update on ASHA Programme. 2017. Available online: https://nhsrcindia.org/sites/default/files/2021-06/ASHA%20Update%20January-2017.pdf (accessed on 22 September 2022).
- Zhang, M.; Wang, M.; Li, J.; Phillips, M.R. Randomised-control trial of family intervention for 78 first-episode male schizophrenic patients: An 18-month study in Suzhou, Jiangsu. Br. J. Psychiatry 1994, 165, 96–102. [Google Scholar] [CrossRef]
- Vasfi, M.G.; Moradi-Lakeh, M.; Esmaeili, N.; Soleimani, N.; Hajebi, A. Efficacy of aftercare services for people with severe mental disorders in Iran: A randomized controlled trial. Psychiatr. Serv. 2015, 66, 373–380. [Google Scholar] [CrossRef]
- SCARF India. Schizophrenia Research Foundation (SCARF India). 2022. Available online: https://www.scarfindia.org/ (accessed on 30 September 2022).
- Thara, R.; Padmavati, R.; Lakshmi, A.; Karpagavalli, P. Family education in schizophrenia: A comparison of two approaches. Indian J. Psychiatry 2005, 47, 218. [Google Scholar] [CrossRef] [PubMed]
- Kulhara, P.; Chakrabarti, S.; Avasthi, A.; Sharma, A.; Sharma, S. Psychoeducational intervention for caregivers of Indian patients with schizophrenia: A randomised-controlled trial. Acta Psychiatr. Scand. 2009, 119, 472–483. [Google Scholar] [CrossRef] [PubMed]
- Walia, T.S.; Verma, P.K.; Chaudhury, S.; Srivastava, S. Family psychoeducation with caregivers of schizophrenia patients: Impact on perceived quality of life. Ind. Psychiatry J. 2019, 28, 19. [Google Scholar] [CrossRef] [PubMed]
- Sivakumar, T.; Thirthalli, J.; Kumar, C.N.; Basavarajappa, C. Community-based rehabilitation for persons with severe mental illness in a rural community of Karnataka: Methodology of a randomized controlled study. Indian J. Psychol. Med. 2020, 42, S73–S79. [Google Scholar] [CrossRef]
- Patel, V.; Naslund, J.A.; Wood, S.; Patel, A.; Chauvin, J.J.; Agrawal, R.; Bhan, A.; Joshi, U.; Amara, M.; Kohrt, B.A.; et al. EMPOWER: Toward the Global Dissemination of Psychosocial Interventions. Focus 2022, 20, 301–306. [Google Scholar] [CrossRef]
- Rössler, W. The stigma of mental disorders: A millennia-long history of social exclusion and prejudices. EMBO Rep. 2016, 17, 1250–1253. [Google Scholar] [CrossRef]
- Stangl, A.L.; Earnshaw, V.A.; Logie, C.H.; Van Brakel, W.; Simbayi, L.C.; Barré, I.; Dovidio, J.F. The Health Stigma and Discrimination Framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019, 17, 1–13. [Google Scholar] [CrossRef]
- Naheed, M.; Akter, K.A.; Tabassum, F.; Mawla, R.; Rahman, M. Factors contributing the outcome of schizophrenia in developing and developed countries: A brief review. Int. Curr. Pharm. J. 2012, 1, 81–85. [Google Scholar] [CrossRef]
| Module No. | Module | Learning Objectives | Learning Outcomes |
|---|---|---|---|
| 1 | Introduction to Schizophrenia | To learn about schizophrenia and its symptoms To dispel misconceptions associated with schizophrenia To know the issue of stigma and discrimination To know the potential risk with schizophrenia cases To know the available treatments of schizophrenia To know the physical comorbidities in schizophrenia To know the phases of illness | Understand schizophrenia and its symptoms Have a clear understanding of facts, stigma and discrimination related to schizophrenia Clarity on available treatments of schizophrenia Able to recognise different phases of the illness |
| 2 | Disability and Rehabilitation | To understand rehabilitation and its need To know about disability To know about various disability schemes and benefits | Understand the importance of rehabilitation to improve the quality of life of the individual living with schizophrenia Understand the concept of disability and various schemes by the government. Skilled in the process of obtaining Disability Certificates and able to support patients and their families in obtaining the disability card |
| 3 | Understanding of COVID-19 | To develop a basic understanding of COVID-19 To learn about vaccines To know how COVID-19 may impact persons living with schizophrenia and their Family | Understanding COVID-19 and its impact on persons living with schizophrenia and their families and regarding vaccination for COVID-19 |
| 4 | Identifying Schizophrenia in the community | To know the schizophrenia symptom profile checklist/screening tool To learn how to identify schizophrenia in community | Skilled in recognizing schizophrenia cases in community Skilled in detecting patients with the help of screening tool |
| 5 | Mental Health First Aid (MHFA) | How to respond to and involve a family member or caregivers Managing suicide risk in schizophrenia To learn about Mental Health First Aid (MHFA) and how to deliver MHFA | Skilled in communicating with family members and providing mental health first aid. Able to assess suicide risk and its management |
| 6 | Making a referral | Understand the referral process How and whom to refer How to coordinate with clinicians and caregivers or family member How to do documentation and reporting Post referral follow-up | Skilled in referring cases from the community and communicating with clinicians and caregivers Able to educate family members/caregiver about the importance of referral Able to maintain a record of community processes and reporting |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naslund, J.A.; Tyagi, V.; Khan, A.; Siddiqui, S.; Kakra Abhilashi, M.; Dhurve, P.; Mehta, U.M.; Rozatkar, A.; Bhatia, U.; Vartak, A.; et al. Schizophrenia Assessment, Referral and Awareness Training for Health Auxiliaries (SARATHA): Protocol for a Mixed-Methods Pilot Study in Rural India. Int. J. Environ. Res. Public Health 2022, 19, 14936. https://doi.org/10.3390/ijerph192214936
Naslund JA, Tyagi V, Khan A, Siddiqui S, Kakra Abhilashi M, Dhurve P, Mehta UM, Rozatkar A, Bhatia U, Vartak A, et al. Schizophrenia Assessment, Referral and Awareness Training for Health Auxiliaries (SARATHA): Protocol for a Mixed-Methods Pilot Study in Rural India. International Journal of Environmental Research and Public Health. 2022; 19(22):14936. https://doi.org/10.3390/ijerph192214936
Chicago/Turabian StyleNaslund, John A., Vidhi Tyagi, Azaz Khan, Saher Siddiqui, Minal Kakra Abhilashi, Pooja Dhurve, Urvakhsh Meherwan Mehta, Abhijit Rozatkar, Urvita Bhatia, Anil Vartak, and et al. 2022. "Schizophrenia Assessment, Referral and Awareness Training for Health Auxiliaries (SARATHA): Protocol for a Mixed-Methods Pilot Study in Rural India" International Journal of Environmental Research and Public Health 19, no. 22: 14936. https://doi.org/10.3390/ijerph192214936
APA StyleNaslund, J. A., Tyagi, V., Khan, A., Siddiqui, S., Kakra Abhilashi, M., Dhurve, P., Mehta, U. M., Rozatkar, A., Bhatia, U., Vartak, A., Torous, J., Tugnawat, D., & Bhan, A. (2022). Schizophrenia Assessment, Referral and Awareness Training for Health Auxiliaries (SARATHA): Protocol for a Mixed-Methods Pilot Study in Rural India. International Journal of Environmental Research and Public Health, 19(22), 14936. https://doi.org/10.3390/ijerph192214936








