Psychometric Analysis of the Quarantine Coping Strategies Scale (Q-COPE) in the Spanish Language
Abstract
1. Introduction
Coping Quarantine
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Instrument
2.4. Validation by Judges
2.5. Statistical Analysis
3. Results
3.1. Content Validity
3.2. Descriptive Statistics of the Q-COPE Items
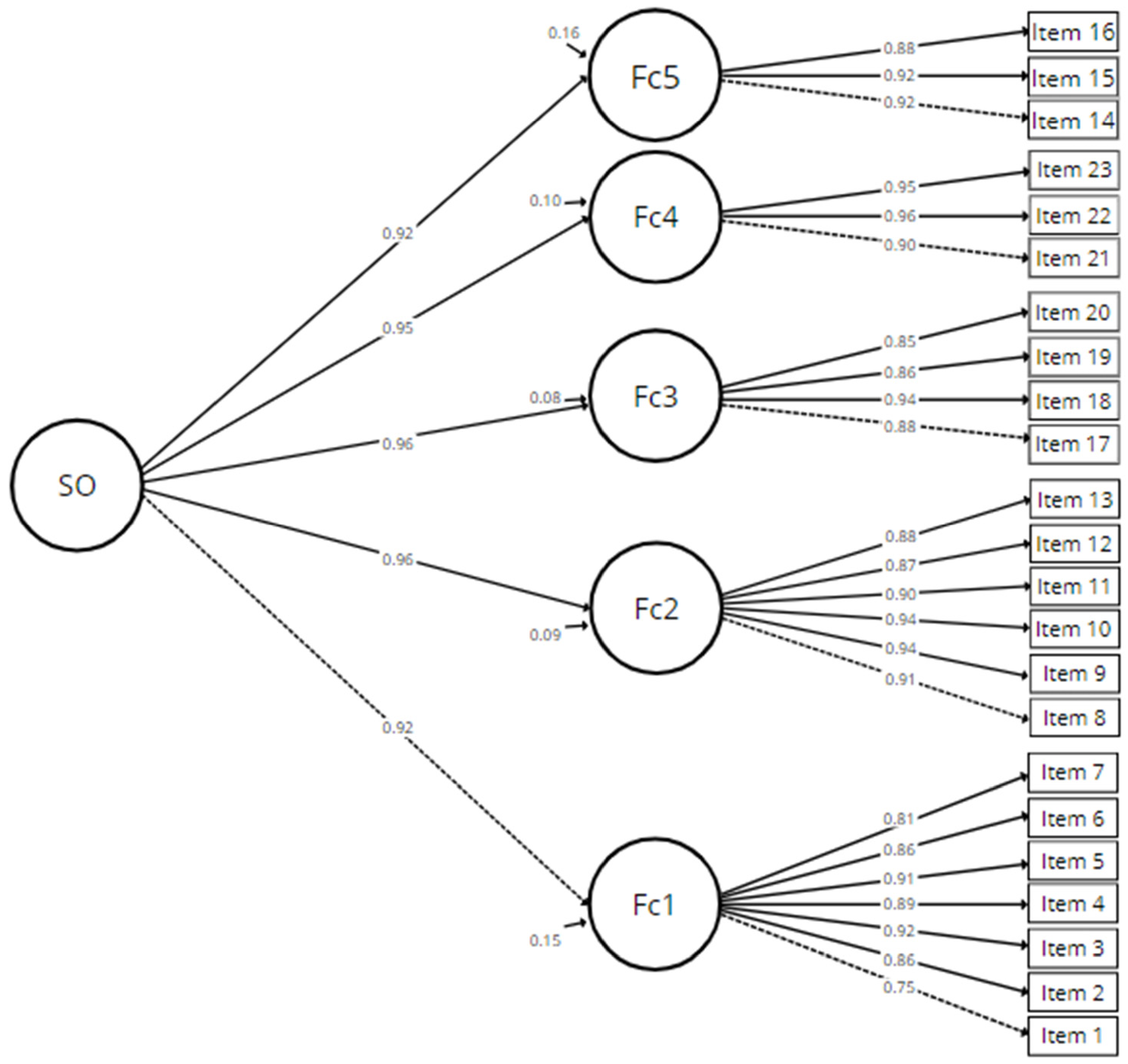
3.3. Evidence of Validity of the Internal Structure
3.4. Internal Consistency
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Rolling Updates on Coronavirus Disease (COVID-19). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed on 14 May 2022).
- Violant-Holz, V.; Gallego-Jiménez, M.G.; González-González, C.S.; Muñoz-Violant, S.; Rodríguez, M.J.; Sansano-Nadal, O.; Guerra-Balic, M. Psychological Health and Physical Activity Levels during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 9419. [Google Scholar] [CrossRef]
- Brodeur, A.; Clark, A.E.; Fleche, S.; Powdthavee, N. COVID-19, lockdowns and well-being: Evidence from Google Trends. J. Public Econ. 2021, 193, 104346. [Google Scholar] [CrossRef] [PubMed]
- Ramiz, L.; Contrand, B.; Rojas Castro, M.Y.; Dupuy, M.; Lu, L.; Sztal-Kutas, C.; Lagarde, E. A longitudinal study of mental health before and during COVID-19 lockdown in the French population. Glob. Health 2021, 17, 29. [Google Scholar] [CrossRef] [PubMed]
- Shukla, J.; Manohar Singh, R. Psychological Health amidst COVID-19: A Review of existing literature in the Indian Context. Clin. Epidemiol. Glob. Health 2021, 11, 100736. [Google Scholar] [CrossRef]
- Singh, R.K.; Bajpai, R.; Kaswan, P. COVID-19 pandemic and psychological wellbeing among health care workers and general population: A systematic-review and meta-analysis of the current evidence from India. Clin. Epidemiol. Glob. Health 2021, 11, 100737. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, R.; Sweta; Singh, B.; Singh, U. Psychological impact of quarantine period on asymptomatic individuals with COVID-19. Soc. Sci. Humanit. Open 2020, 2, 100061. [Google Scholar] [CrossRef]
- Di Cagno, A.; Buonsenso, A.; Baralla, F.; Grazioli, E.; Di Martino, G.; Lecce, E.; Calcagno, G.; Fiorilli, G. Psychological Impact of the Quarantine-Induced Stress during the Coronavirus (COVID-19) Outbreak among Italian Athletes. Int. J. Environ. Res. Public Health 2020, 17, 8867. [Google Scholar] [CrossRef]
- Bueno-Notivol, J.; Gracia-García, P.; Olaya, B.; Lasheras, I.; López-Antón, R.; Santabárbara, J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021, 21, 100196. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
- Jin, Y.; Sun, T.; Zheng, P.; An, J. Mass quarantine and mental health during COVID-19: A meta-analysis. J. Affect. Disord. 2021, 295, 1335–1346. [Google Scholar] [CrossRef]
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. QJM Int. J. Med. 2020, 113, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Sun, X.; Xie, F.; Chen, B.; Wang, L.; Hu, L.; Dai, Q. Impact of COVID-19 on psychological wellbeing. Int. J. Clin. Health Psychol. 2021, 21, 100252. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Riyu, P.; Xiaoyang, W.; Yilin, T.; Linkang, X.; Cyrus, S.H.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Medda, E.; Gigantesco, A.; Picardi, A.; Carluccio, E.; D’Ippolito, C.; Ferri, M.; Brescianini, S.; Toccaceli, V.; Stazi, M.A. The COVID-19 pandemic in Italy: The impact on social life and mental health. Riv. Psichiatr. 2021, 56, 182–188. [Google Scholar] [PubMed]
- Bonati, M.; Campi, R.; Zanetti, M.; Cartabia, M.; Scarpellini, F.; Clavenna, A.; Segre, G. Psychological distress among Italians during the 2019 coronavirus disease (COVID-19) quarantine. BMC Psychiatry 2021, 21, 20. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Yao, M.; Deng, C.; Marsiglia, F.F.; Duan, W. Social Isolation and Anxiety Disorder During the COVID-19 Pandemic and Lockdown in China. J. Affect. Disord. 2021, 294, 10–16. [Google Scholar] [CrossRef]
- Saurabh, K.; Ranjan, S. Compliance and Psychological Impact of Quarantine in Children and Adolescents due to Covid-19 Pandemic. Indian J. Pediatr. 2020, 87, 532–536. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Demaria, F.; Vicari, S. COVID-19 quarantine: Psychological impact and support for children and parents. Ital. J. Pediatr. 2021, 47, 58. [Google Scholar] [CrossRef]
- Brailovskaia, J.; Margraf, J. Predicting adaptive and maladaptive responses to the Coronavirus (COVID-19) outbreak: A prospective longitudinal study. Int. J. Clin. Health Psychol. 2020, 20, 183–191. [Google Scholar] [CrossRef]
- Rosa-Alcázar, Á.; García-Hernández, M.D.; Parada-Navas, J.L.; Olivares-Olivares, P.J.; Martínez-Murillo, S.; Rosa-Alcázar, A.I. Coping strategies in obsessive-compulsive patients during Covid-19 lockdown. Int. J. Clin. Health Psychol. 2021, 21, 100223. [Google Scholar] [CrossRef] [PubMed]
- Zager Kocjan, G.; Kavčič, T.; Avsec, A. Resilience matters: Explaining the association between personality and psychological functioning during the COVID-19 pandemic. Int. J. Clin. Health Psychol. 2021, 21, 100198. [Google Scholar] [CrossRef]
- Jiang, R. Knowledge, attitudes and mental health of university students during the COVID-19 pandemic in China. Child. Youth Serv. Rev. 2020, 119, 105494. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Jacob, L.; Yakkundi, A.; McDermott, D.; Armstrong, N.C.; Barnett, Y.; López-Sánchez, G.F.; Martin, S.; Butler, L.; Tully, M.A. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: A cross-sectional study of UK-based respondents. Psychiatry Res. 2020, 291, 113138. [Google Scholar] [CrossRef]
- Reynolds, D.L.; Garay, J.R.; Deamond, S.L.; Moran, M.K.; Gold, W.; Styra, R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2008, 136, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- Marjanovic, Z.; Greenglass, E.R.; Coffey, S. The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: An online questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 991–998. [Google Scholar] [CrossRef]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS Control and Psychological Effects of Quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef]
- Manuell, M.E.; Cukor, J. Mother Nature versus human nature: Public compliance with evacuation and quarantine. Disasters 2011, 35, 417–442. [Google Scholar] [CrossRef] [PubMed]
- Braunack-Mayer, A.; Tooher, R.; Collins, J.E.; Street, J.M.; Marshall, H. Understanding the school community’s response to school closures during the H1N1 2009 influenza pandemic. BMC Public Health 2013, 13, 344. [Google Scholar] [CrossRef]
- Caleo, G.; Duncombe, J.; Jephcott, F.; Lokuge, K.; Mills, C.; Looijen, E.; Theoharaki, F.; Kremer, R.; Kleijer, K.; Squire, J.; et al. The factors affecting household transmission dynamics and community compliance with Ebola control measures: A mixed-methods study in a rural village in Sierra Leone. BMC Public Health 2018, 18, 248. [Google Scholar] [CrossRef]
- DiGiovanni, C.; Conley, J.; Chiu, D.; Zaborski, J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur. Bioterror. 2004, 2, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Pellecchia, U.; Crestani, R.; Decroo, T.; Van Den Bergh, R.; Al-Kourdi, Y. Social consequences of ebola containment measures in Liberia. PLoS ONE 2015, 10, e0143036. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Hershenfield, K.; Grace, S.L.; Stewart, D.E. The psychosocial effects of being quarantined following exposure to SARS: A qualitative study of Toronto health care workers. Can. J. Psychiatry 2004, 49, 403–407. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- VandenBos, G.R.; American Psychological Association. APA Dictionary of Psychology, 2nd ed.; VandenBos, G.R., Association, A.P., Eds.; American Psychological Association: Washington, DC, USA, 2015. [Google Scholar]
- Endler, N.S.; Parker, J.D.A. Multidimensional Assessment of Coping: A Critical Evaluation. J. Personal. Soc. Psychol. 1990, 58, 844–854. [Google Scholar] [CrossRef]
- Skinner, E.A.; Edge, K.; Altman, J.; Sherwood, H. Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychol. Bull. 2003, 129, 216–269. [Google Scholar] [CrossRef]
- Zheng, S. Quarantine Life Is Stillness and Dialogue: A Reflective Autoethnography During a Global Pandemic. Qual. Inq. 2021, 27, 829–834. [Google Scholar] [CrossRef]
- Luo, X.; Estill, J.; Wang, Q.; Lv, M.; Liu, Y.; Liu, E.; Chen, Y. The psychological impact of quarantine on coronavirus disease 2019 (COVID-19). Psychiatry Res. 2020, 291, 113193. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Mahamid, F.A.; Veronese, G.; Bdier, D. Fear of coronavirus (COVID-19) and mental health outcomes in Palestine: The mediating role of social support. Curr. Psychol. 2021, 1–10. [Google Scholar] [CrossRef]
- Munawar, K.; Choudhry, F.R. Exploring stress coping strategies of frontline emergency health workers dealing Covid-19 in Pakistan: A qualitative inquiry. Am. J. Infect. Control. 2021, 49, 286–292. [Google Scholar] [CrossRef]
- Baghcheghi, N.; Koohestani, H.R. Designing and psychometric properties of coping strategies scale for family caregivers of hemodialysis patients. Acta Fac. Med. Naissensis 2021, 38, 257–269. [Google Scholar] [CrossRef]
- Mesekaa, L.; Mungai, L.; Rutjens, B.T.; Van Lissa, C.J.; Farias, M. The psychological impact of threat and lockdowns during the COVID-19 pandemic: Exacerbating factors and mitigati ng actions. Transl. Behav. Med. 2021, 11, 1318–1329. [Google Scholar] [CrossRef]
- Hsieh, K.Y.; Kao, W.T.; Li, D.J.; Lu, W.C.; Tsai, K.Y.; Chen, W.J.; Chou, L.S.; Huang, J.J.; Hsu, S.T.; Chou, F.H.C. Mental health in biological disasters: From SARS to COVID-19. Int. J. Soc. Psychiatry 2021, 67, 576–586. [Google Scholar] [CrossRef] [PubMed]
- Chandu, V.C.; Marella, Y.; Panga, G.S.; Pachava, S.; Vadapalli, V. Measuring the Impact of COVID-19 on Mental Health: A Scoping Review of the Existing Scales. Indian J. Psychol. Med. 2020, 42, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Kato, T. Frequently used coping scales: A meta-analysis. Stress Health 2015, 31, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Noreen, K.; Umar, M.; Sabir, S.A.; Rehman, R. Outbreak of coronavirus disease 2019 (COVID-19) in Pakistan: Psychological impact and coping strategies of health care professionals. Pak. J. Med. Sci. 2020, 36, 1478–1483. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, C.; Pan, W.; Zheng, J.; Gao, J.; Huang, X.; Cai, S.; Zhai, Y.; Latour, J.M.; Zhu, C. Stress, Burnout, and Coping Strategies of Frontline Nurses During the COVID-19 Epidemic in Wuhan and Shanghai, China. Front. Psychiatry 2020, 11, 1154. [Google Scholar] [CrossRef]
- Singh, N.; Kumar, S.; Rathore, P.; Vig, S.; Vallath, N.; Mohan, A.; Bhatnagar, S. Concerns and coping strategies of persons under institutional quarantine during SARS-CoV-2 pandemic. Indian J. Palliat. Care 2020, 26, S99–S105. [Google Scholar] [CrossRef]
- Shousha, H.I.; Madbouly, N.; Afify, S.; Asem, N.; Fouad, E.; Maher, R.; Moussa, S.S.; Abdelazeem, A.; Youssif, E.M.; Harhira, K.Y.; et al. Anxiety, depression and coping strategies among chronic medical patients with coronavirus disease-2019: A multicenter follow-up cohort study. J. Ment. Health 2021, 1–9. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Ato, M.; López, J.J.; Benavente, A. Un sistema de clasificación de los diseños de investigación en psicología. Ann. Psychol. 2013, 29, 1038–1059. [Google Scholar] [CrossRef]
- Lazarus, R.S. From Psychological Stress to the Emotions: A History of Changing Outlooks. Annu. Rev. Psychol. 1993, 44, 1–22. [Google Scholar] [CrossRef]
- Navas, M.J. Los instrumentos de investigación psicológica. I: Construcción y aplicación. In Métodos, Diseños y Técnicas de Investigación Psicológica; Navas, M.J., Ed.; Universidad Nacional de Educación a Distancia: Madrid, Spain, 2001. [Google Scholar]
- Muñiz, J.; Fonseca-Pedrero, E. Ten steps for test development. Psicothema 2019, 31, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Aiken, L.R. Three coefficients for analyzing the reliability and validity of ratings. Educ. Psychol. Meas. 1985, 45, 131–142. [Google Scholar] [CrossRef]
- Sireci, S.; Faulkner-Bond, M. Evidencia de validez basada en el contenido del test. Psicothema 2014, 26, 100–107. [Google Scholar] [CrossRef]
- Penfield, R.D.; Giacobbi, P.R. Applying a score confidence interval to Aiken’s item content-relevance index. Meas. Phys. Educ. Exerc. Sci. 2004, 8, 213–225. [Google Scholar] [CrossRef]
- Gravetter, F.; Wallnau, L. Essentials of Statistics for the Behavioral Sciences; Cengage Learning: Wadsworth, OH, USA, 2014. [Google Scholar]
- Pérez, E.R.; Medrano, L. Análisis Factorial Exploratorio: Bases Conceptuales y Metodológicas Artículo de Revisión. Rev. Argent. Cienc. Comport. 2010, 2, 58–66. [Google Scholar]
- Lewis, N.D. 100 Statistical Tests in R: What to Choose, How to Easily Calculate, with Over 300 Illustrations and Examples; Heather Hills Press: Bowie, MD, USA, 2013. [Google Scholar]
- Bandalos, D.L.; Finney, S.J. Factor Analysis: Exploratory and Confirmatory. In Reviewer’s Guide to Quantitative Methods in the Social Sciences; Hancock, G.R., Stapleton, L.M., Mueller, R.O., Eds.; Routledge: New York, NY, USA, 2019; pp. 1–376. [Google Scholar]
- Kaiser, H.F. An index of factorial simplicity. Psychometrika 1974, 39, 31–36. [Google Scholar] [CrossRef]
- Martínez-Arias, M.R.; Hernández-Lloreda, M.V.; Hernández-Lloreda, M.J. Psicometría; Alianza Editorial S.A.: Madrid, Spain, 2014. [Google Scholar]
- Watkins, M.W. Exploratory Factor Analysis: A Guide to Best Practice. J. Black Psychol. 2018, 44, 219–246. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with Amos; Tercerda, E., Ed.; Routledge: New York, NY, USA, 2016. [Google Scholar]
- Gould, S.J. Second Order Confirmatory Factor Analysis: An Example. In Developments in Marketing Science: Proceedings of the Academy of Marketing Science; Springer: Cham, Switzerland, 2015; pp. 488–490. [Google Scholar]
- Finney, S.J.; DiStefano, C. Nonnormal and categorial data in structural equation modeling. In Structural Equation Modeling: A Second Course; Information Age Publishing Inc.: Charlotte, NC, USA, 2013. [Google Scholar]
- Hancock, G.R.; Mueller, R.O. Rethinking Construct Reliability within Latent Variable Systems. In Structural Equation Modeling: Present and Future—A Festschrift in Honor of Karl Joreskog; Cudeck, R., Toit, S.D., Soerbom, D., Eds.; Scientific Software International: Lincolnwood, IL, USA, 2001; pp. 195–216. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 8th ed.; Cengage Learning: North Way, AK, USA, 2019. [Google Scholar]
- Schumacker, R.E.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modeling, 4th ed.; Taylor & Francis: New York, NY, USA, 2016. [Google Scholar]
- Dominguez-Lara, S. Propuesta de puntos de corte para cargas factoriales: Una perspectiva de fiabilidad de constructo. Enfermería Clínica 2018, 28, 401–402. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Structural Equation Models with Unobservable Variables and Measurement Error: Algebra and Statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Hunsley, J.; Marsh, E.J. Developing criteria for evidence-based assessment: An introduction to assessment that work. In A guide to Assessments That Work; Hunsley, J., Marsh, E.J., Eds.; Oxford University Press: Oxford, UK, 2008; pp. 3–14. [Google Scholar]
- Ponterotto, J.G.; Charter, R.A. Statistical extensions of ponterotto and ruckdeschel’s (2007) reliability matrix for estimating the adequacy of internal consistency coefficients. Percept. Mot. Ski. 2009, 108, 878–886. [Google Scholar] [CrossRef] [PubMed]
- Revelle, W. Psych: Procedures for Psychological, Psychometric, and Personality Research. 2019. Available online: https://CRAN.R-project.org/package=psych (accessed on 1 November 2022).
- Lloret-Segura, S.; Ferreres-Traver, A.; Hernández-Baeza, A.; Tomás-Marco, I. Exploratory Item Factor Analysis: A practical guide revised and updated. An. Psicol. 2014, 30, 1151–1169. [Google Scholar] [CrossRef]
- Costello, A.B.; Osborne, J.W. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2005, 10, 7. [Google Scholar] [CrossRef]
- Velicer, W.F.; Fava, J.L. Effects of Variable and Subject Sampling on Factor Pattern Recovery. Psychol. Methods 1998, 3, 231–251. [Google Scholar] [CrossRef]
- Mason, C.H.; Perreault, W.D. Collinearity, Power, and Interpretation of Multiple Regression Analysis. J. Mark. Res. 1991, 28, 268–280. [Google Scholar] [CrossRef]
- Eignor, D.R. The Standards for Educational and Psychological Testing; Geisinger, K.F., Bracken, B.A., Carlson, J.F., Hansen, J.-I.C., Kuncel, N.R., Reise, S.P., Rodriguez, M.C., Eds.; American Psychological Association: Washington, DC, USA, 2013. [Google Scholar]
- Schwarz, C.; Schwarz, A.; Black, W.C. Examining the Impact of Multicollinearity in Discovering Higher-Order Factor Models. Commun. Assoc. Inf. Syst. 2014, 34, 1191–1208. [Google Scholar] [CrossRef]
- Reise, S.P.; Scheines, R.; Widaman, K.F.; Haviland, M.G. Multidimensionality and Structural Coefficient Bias in Structural Equation Modeling: A Bifactor Perspective. Educ. Psychol. Meas. 2013, 73, 5–26. [Google Scholar] [CrossRef]
- Chen, D.; Song, F.; Tang, L.; Zhang, H.; Shao, J.; Qiu, R.; Wang, X.; Ye, Z. Quarantine experience of close contacts of COVID-19 patients in China: A qualitative descriptive study. Gen. Hosp. Psychiatry 2020, 66, 81–88. [Google Scholar] [CrossRef]
- Reise, S.P. The Rediscovery of Bifactor Measurement Models. Multivar. Behav. Res. 2012, 47, 667–696. [Google Scholar] [CrossRef]
- Martínez-García, J.; Martínez-Caro, L. Discriminant Validity as a Scale Evaluation Criterion: Theory or Statistics? Univ. Psychol. 2009, 8, 27–36. [Google Scholar]
- Borsboom, D.; Mellenbergh, G.J.; van Heerden, J. The concept of validity. Psychol. Rev. 2004, 111, 1061–1071. [Google Scholar] [CrossRef] [PubMed]
- Dunn, T.J.; Baguley, T.; Brunsden, V. From alpha to omega: A practical solution to the pervasive problem of internal consistency estimation. Br. J. Psychol. 2014, 105, 399–412. [Google Scholar] [CrossRef] [PubMed]
- Goes, M.; Lopes, M.; Marôco, J.; Oliveira, H.; Fonseca, C. Psychometric properties of the WHOQOL-BREF(PT) in a sample of elderly citizens. Health Qual. Life Outcomes 2021, 19, 146. [Google Scholar] [CrossRef]
- Lucero-Perez, M.R.; Sabastizagal, I.; Astete-Cornejo, J.; Burgos, M.A.; Villarreal-Zegarra, D.; Moncada, S. Validation of the medium and short version of CENSOPAS-COPSOQ: A psychometric study in the Peruvian population. BMC Public Health 2022, 22, 910. [Google Scholar] [CrossRef]
- Lee, E.Y.; Shin, Y.J.; Choi, B.Y.; Cho, H.S.M. Reliability and validity of a scale for health-promoting schools. Health Promot. Int. 2014, 29, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Wolf, E.J.; Harrington, K.M.; Clark, S.L.; Miller, M.W. Sample Size Requirements for Structural Equation Models: An Evaluation of Power, Bias, and Solution Propriety. Educ. Psychol. Meas. 2013, 73, 913–934. [Google Scholar] [CrossRef]
- Kyriazos, T.A.; Kyriazos, T.A. Applied Psychometrics: Sample Size and Sample Power Considerations in Factor Analysis (EFA, CFA) and SEM in General. Psychology 2018, 9, 2207–2230. [Google Scholar] [CrossRef]

| V [IC 95%] | M1 | M2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Item | M | DE | g1 | g2 | M | DE | g1 | g2 | |
| Item1 | 0.92 [0.74; 0.98] | 3.58 | 1.30 | −0.74 | −0.56 | 3.56 | 1.33 | −0.74 | −0.62 |
| Item2 | 0.79 [0.60; 0.91] | 3.48 | 1.16 | −0.40 | −0.81 | 3.51 | 1.20 | −0.48 | −0.79 |
| Item3 * | 0.67 [0.47; 0.82] | 3.34 | 1.18 | −0.23 | −0.95 | 3.35 | 1.19 | −0.36 | −0.84 |
| Item4 * | 0.67 [0.47; 0.82] | 3.05 | 1.26 | 0.07 | −1.14 | 3.05 | 1.31 | 0.09 | −1.20 |
| Item5 | 0.75 [0.55; 0.88] | 3.17 | 1.31 | −0.08 | −1.20 | 3.20 | 1.32 | −0.13 | −1.25 |
| Item6 | 0.96 [0.80; 0.99] | 3.71 | 1.27 | −0.93 | −0.19 | 3.76 | 1.28 | −1.01 | −0.08 |
| Item7 | 0.96 [0.80; 0.99] | 3.87 | 1.29 | −1.13 | 0.16 | 3.90 | 1.27 | −1.11 | 0.15 |
| Item8 | 0.71 [0.51; 0.85] | 3.42 | 1.16 | −0.31 | −0.80 | 3.49 | 1.18 | −0.47 | −0.66 |
| Item9 | 1.00 [0.86; 1.00] | 3.72 | 1.22 | −0.89 | −0.14 | 3.76 | 1.27 | −0.98 | −0.07 |
| Item10 | 0.96 [0.80; 0.99] | 3.79 | 1.28 | −1.00 | −0.04 | 3.81 | 1.29 | −1.04 | −0.01 |
| Item11 | 0.96 [0.80; 0.99] | 3.63 | 1.26 | −0.81 | −0.34 | 3.68 | 1.29 | −0.83 | −0.38 |
| Item12 | 0.75 [0.55; 0.88] | 3.69 | 1.14 | −0.66 | −0.39 | 3.72 | 1.18 | −0.67 | −0.47 |
| Item13 | 0.71 [0.51; 0.85] | 3.30 | 1.17 | −0.22 | −0.84 | 3.40 | 1.22 | −0.28 | −0.91 |
| Item14 | 0.79 [0.60; 0.91] | 3.34 | 1.18 | −0.26 | −0.83 | 3.39 | 1.23 | −0.27 | −0.95 |
| Item15 | 1.00 [0.86; 1.00] | 3.50 | 1.29 | −0.65 | −0.62 | 3.53 | 1.26 | −0.73 | −0.45 |
| Item16 | 1.00 [0.86; 1.00] | 3.18 | 1.24 | −0.02 | −1.13 | 3.08 | 1.30 | 0.03 | −1.22 |
| Item17 | 0.96 [0.80; 0.99] | 3.86 | 1.28 | −1.16 | 0.27 | 3.89 | 1.27 | −1.12 | 0.17 |
| Item18 | 0.92 [0.74; 0.98] | 3.87 | 1.28 | −1.17 | 0.28 | 3.92 | 1.29 | −1.20 | 0.31 |
| Item19 | 0.88 [0.69; 0.96] | 3.83 | 1.27 | −1.13 | 0.24 | 3.84 | 1.27 | −1.11 | 0.16 |
| Item20 | 1.00 [0.86; 1.00] | 3.39 | 1.14 | −0.30 | −0.81 | 3.40 | 1.25 | −0.32 | −0.98 |
| Item21 | 1.00 [0.86; 1.00] | 3.69 | 1.24 | −0.96 | −0.07 | 3.77 | 1.26 | −1.02 | 0.02 |
| Item22 | 0.96 [0.80; 0.99] | 3.62 | 1.24 | −0.89 | −0.18 | 3.67 | 1.25 | −0.91 | −0.15 |
| Item23 | 1.00 [0.86; 1.00] | 3.54 | 1.24 | −0.78 | −0.37 | 3.60 | 1.21 | −0.73 | −0.39 |
| Item24 | 0.96 [0.80; 0.99] | 3.80 | 1.25 | −1.10 | 0.19 | 3.81 | 1.27 | −1.07 | 0.09 |
| Item25 | 1.00 [0.86; 1.00] | 3.57 | 1.26 | −0.81 | −0.40 | 3.65 | 1.26 | −0.85 | −0.30 |
| Item26 | 1.00 [0.86; 1.00] | 3.63 | 1.24 | −0.90 | −0.20 | 3.68 | 1.28 | −0.91 | −0.27 |
| Item27 | 1.00 [0.86; 1.00] | 3.57 | 1.25 | −0.80 | −0.35 | 3.59 | 1.26 | −0.79 | −0.41 |
| Item28 * | 0.63 [0.43; 0.79] | 2.64 | 1.15 | 0.18 | −0.82 | 2.68 | 1.25 | 0.26 | −0.92 |
| Item29 * | 0.63 [0.43; 0.79] | 2.75 | 1.15 | 0.12 | −0.89 | 2.77 | 1.22 | 0.12 | −0.97 |
| Item30 | 0.92 [0.74; 0.98] | 3.05 | 1.24 | 0.13 | −1.04 | 2.98 | 1.30 | 0.12 | −1.12 |
| Item31 * | 0.54 [0.35; 0.72] | 3.49 | 1.12 | −0.39 | −0.69 | 3.42 | 1.20 | −0.33 | −0.85 |
| Item32 | 0.71 [0.51; 0.85] | 3.20 | 1.21 | −0.27 | −0.91 | 3.24 | 1.24 | −0.33 | −0.89 |
| Item33 | 0.96 [0.80; 0.99] | 3.48 | 1.26 | −0.75 | −0.51 | 3.55 | 1.22 | −0.80 | −0.35 |
| Item34 | 0.96 [0.80; 0.99] | 3.63 | 1.33 | −0.76 | −0.61 | 3.72 | 1.29 | −0.88 | −0.37 |
| Item35 | 0.92 [0.74; 0.98] | 3.67 | 1.27 | −0.94 | −0.17 | 3.72 | 1.24 | −1.00 | 0.05 |
| Item36 | 1.00 [0.86; 1.00] | 3.52 | 1.26 | −0.66 | −0.66 | 3.54 | 1.28 | −0.70 | −0.59 |
| Item37 | 1.00 [0.86; 1.00] | 3.63 | 1.29 | −0.81 | −0.48 | 3.69 | 1.23 | −0.94 | −0.05 |
| Item38 | 0.96 [0.80; 0.99] | 3.59 | 1.24 | −0.88 | −0.15 | 3.65 | 1.21 | −0.88 | −0.11 |
| Item39 | 1.00 [0.86; 1.00] | 3.49 | 1.28 | −0.64 | −0.69 | 3.54 | 1.26 | −0.70 | −0.54 |
| Item40 | 1.00 [0.86; 1.00] | 3.69 | 1.29 | −0.93 | −0.23 | 3.74 | 1.25 | −0.95 | −0.09 |
| Item41 | 1.00 [0.86; 1.00] | 3.84 | 1.29 | −1.06 | 0.00 | 3.89 | 1.29 | −1.14 | 0.17 |
| Item42 | 1.00 [0.86; 1.00] | 3.82 | 1.31 | −1.06 | −0.05 | 3.88 | 1.28 | −1.14 | 0.22 |
| Item43 | 0.96 [0.80; 0.99] | 2.60 | 1.30 | 0.54 | −0.85 | 2.54 | 1.31 | 0.58 | −0.84 |
| EFA | CFA | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Initial Numbering | F1 | F2 | F3 | F4 | F5 | h2 | F1 (λ) | F2 (λ) | F3 (λ) | F4 (λ) | F5 (λ) | Final Numbering |
| 1 | 0.48 | 0.610 | 0.75 | 1 | ||||||||
| 6 | 0.75 | 0.728 | 0.86 | 2 | ||||||||
| 7 | 0.84 | 0.814 | 0.92 | 3 | ||||||||
| 9 | 0.92 | 0.810 | 0.89 | 4 | ||||||||
| 10 | 0.93 | 0.842 | 0.91 | 5 | ||||||||
| 11 | 0.85 | 0.751 | 0.86 | 6 | ||||||||
| 15 | 0.53 | 0.599 | 0.81 | 7 | ||||||||
| 17 | 0.84 | 0.869 | 0.91 | 8 | ||||||||
| 18 | 0.89 | 0.927 | 0.94 | 9 | ||||||||
| 19 | 0.67 | 0.857 | 0.94 | 10 | ||||||||
| 21 | 0.61 | 0.807 | 0.90 | 11 | ||||||||
| 22 | 0.56 | 0.740 | 0.87 | 12 | ||||||||
| 24 | 0.40 | 0.848 | 0.88 | 13 | ||||||||
| 25 | 0.73 | 0.802 | 0.92 | 14 | ||||||||
| 26 | 0.64 | 0.797 | 0.92 | 15 | ||||||||
| 27 | 0.69 | 0.769 | 0.88 | 16 | ||||||||
| 34 | 0.75 | 0.756 | 0.88 | 17 | ||||||||
| 35 | 0.73 | 0.853 | 0.94 | 18 | ||||||||
| 36 | 0.77 | 0.740 | 0.86 | 19 | ||||||||
| 39 | 0.66 | 0.726 | 0.85 | 20 | ||||||||
| 40 | 0.63 | 0.813 | 0.90 | 21 | ||||||||
| 41 | 0.83 | 0.921 | 0.96 | 22 | ||||||||
| 42 | 0.92 | 0.932 | 0.95 | 23 | ||||||||
| % variance | 22.6 | 18.4 | 14.4 | 12.6 | 11.6 | Complete scale | Complete scale | |||||
| α | 0.95 | 0.97 | 0.93 | 0.96 | 0.92 | 0.98 | 0.95 | 0.97 | 0.93 | 0.95 | 0.93 | 0.98 |
| ω | 0.95 | 0.97 | 0.93 | 0.96 | 0.92 | 0.98 | 0.95 | 0.97 | 0.94 | 0.95 | 0.93 | 0.98 |
| - | - | - | - | - | - | - | 0.95 | 0.97 | 0.93 | 0.95 | 0.93 | Ordinalα |
| - | - | - | - | - | - | - | 0.96 | 0.97 | 0.94 | 0.96 | 0.94 | H |
| - | - | - | - | - | - | - | 0.74 | 0.82 | 0.78 | 0.88 | 0.82 | AVE |
| - | - | - | - | - | - | - | 0.74 | 0.82 | 0.78 | 0.88 | 0.82 | F1 |
| - | - | - | - | - | - | - | 1 | 0.79 | 0.76 | 0.77 | 0.71 | F2 |
| - | - | - | - | - | - | - | 0.89 | 1 | 0.83 | 0.81 | 0.77 | F3 |
| - | - | - | - | - | - | - | 0.87 | 0.9 | 1 | 0.85 | 0.79 | F4 |
| - | - | - | - | - | - | - | 0.87 | 0.9 | 0.91 | 1 | 0.72 | F5 |
| Model | χ2 (df) | p-Valor | χ2/df | SRMR | CFI | TLI | RMSEA [90% CI] |
|---|---|---|---|---|---|---|---|
| First Order | 489.048 (220) | 0.000 | 2.223 | 0.025 | 0.969 | 0.965 | 0.047 [0.043; 0.051] |
| Second Order | 499.674 (225) | 0.000 | 2.221 | 0.026 | 0.969 | 0.965 | 0.047 [0.043; 0.051] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cunza-Aranzábal, D.F.; Morales-García, W.C.; Saintila, J.; Huancahuire-Vega, S.; Ruiz Mamani, P.G. Psychometric Analysis of the Quarantine Coping Strategies Scale (Q-COPE) in the Spanish Language. Int. J. Environ. Res. Public Health 2022, 19, 14847. https://doi.org/10.3390/ijerph192214847
Cunza-Aranzábal DF, Morales-García WC, Saintila J, Huancahuire-Vega S, Ruiz Mamani PG. Psychometric Analysis of the Quarantine Coping Strategies Scale (Q-COPE) in the Spanish Language. International Journal of Environmental Research and Public Health. 2022; 19(22):14847. https://doi.org/10.3390/ijerph192214847
Chicago/Turabian StyleCunza-Aranzábal, Denis Frank, Wilter C. Morales-García, Jacksaint Saintila, Salomón Huancahuire-Vega, and Percy G. Ruiz Mamani. 2022. "Psychometric Analysis of the Quarantine Coping Strategies Scale (Q-COPE) in the Spanish Language" International Journal of Environmental Research and Public Health 19, no. 22: 14847. https://doi.org/10.3390/ijerph192214847
APA StyleCunza-Aranzábal, D. F., Morales-García, W. C., Saintila, J., Huancahuire-Vega, S., & Ruiz Mamani, P. G. (2022). Psychometric Analysis of the Quarantine Coping Strategies Scale (Q-COPE) in the Spanish Language. International Journal of Environmental Research and Public Health, 19(22), 14847. https://doi.org/10.3390/ijerph192214847










