Burden of Malaria in Sao Tome and Principe, 1990–2019: Findings from the Global Burden of Disease Study 2019
Abstract
1. Introduction
2. Methods
2.1. Study Context
2.2. Data Sources
2.3. Indicators of Disease Burden Analysis
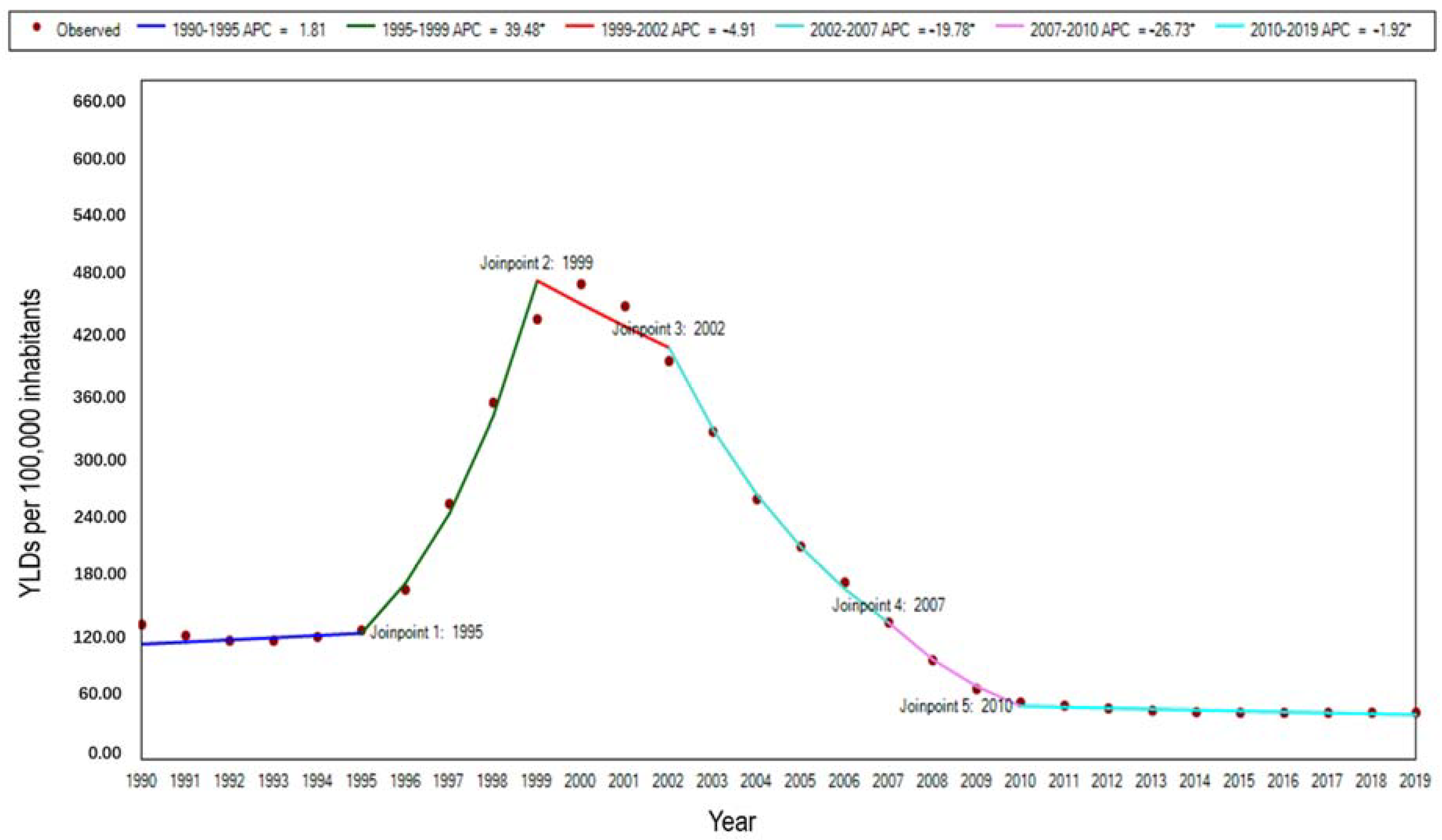
2.4. Statistical Analysis
3. Results
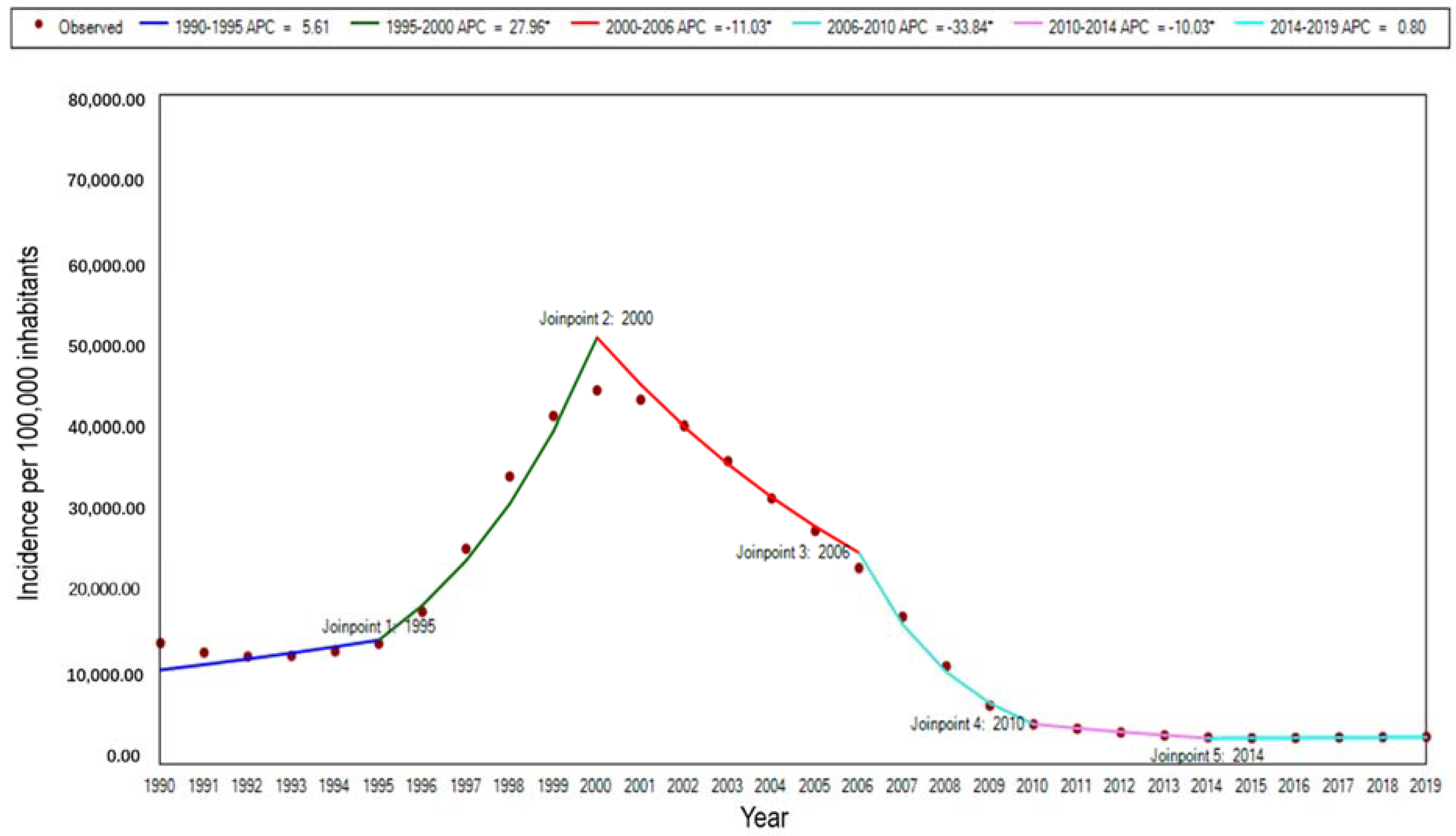
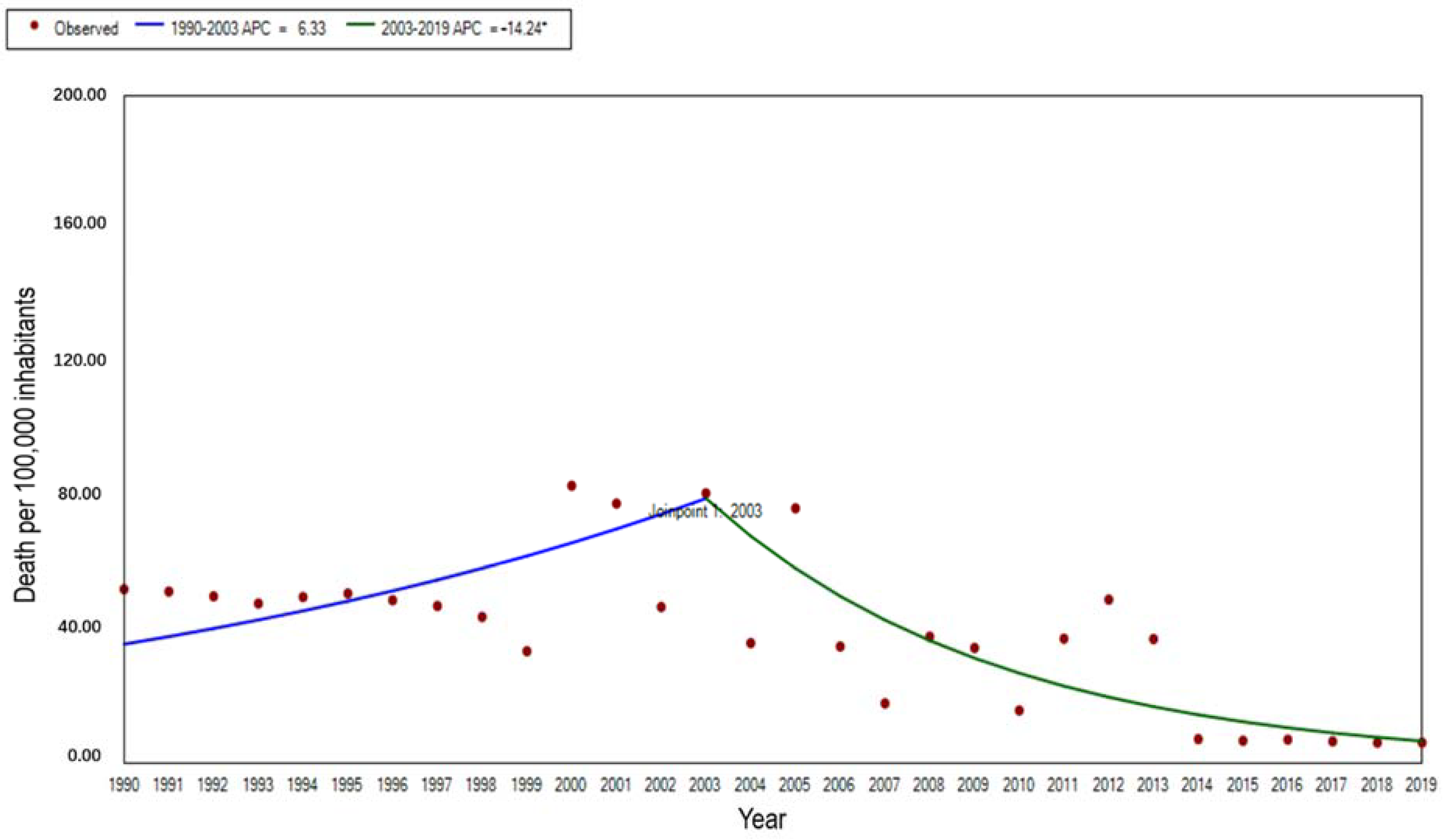
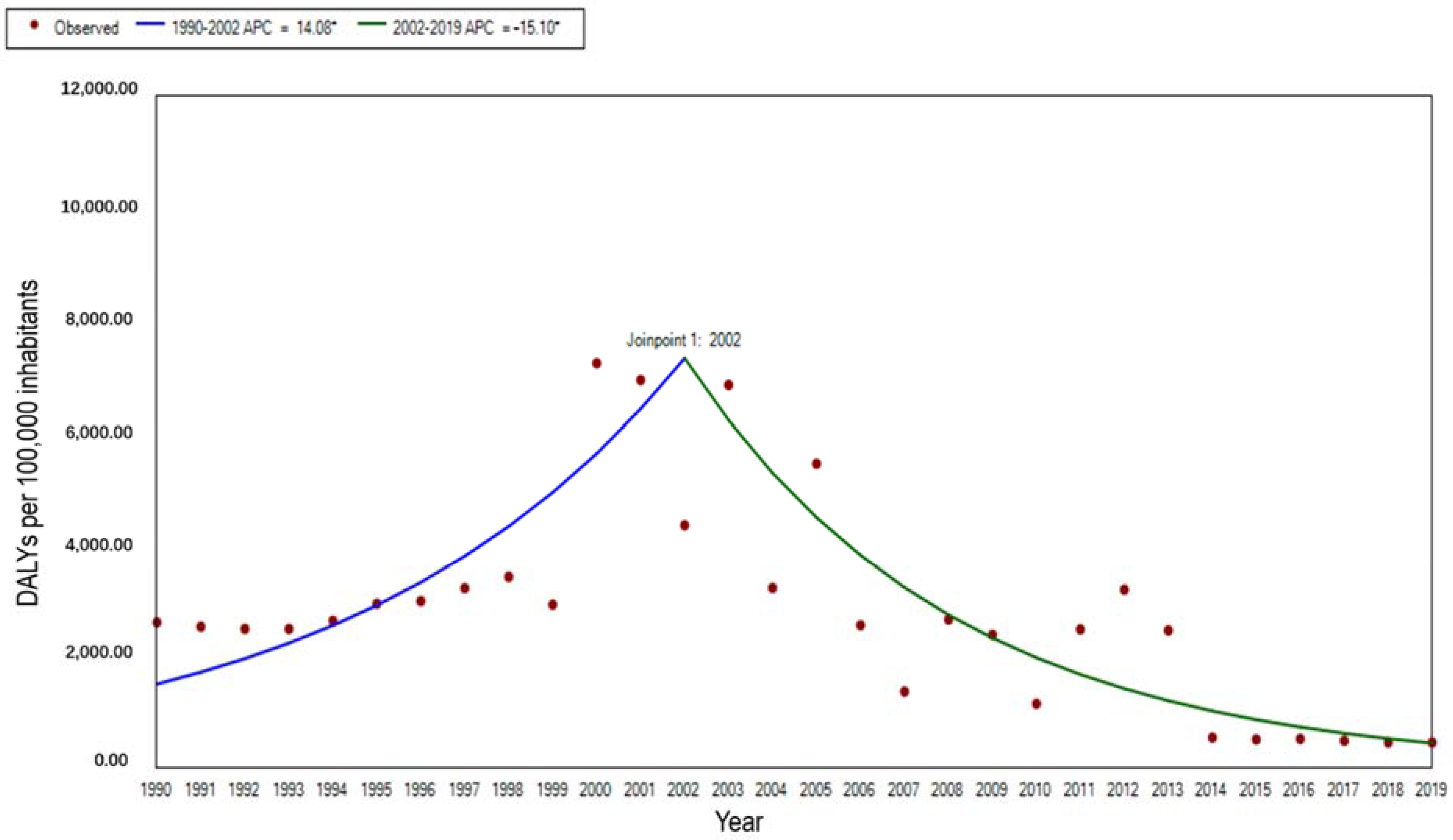
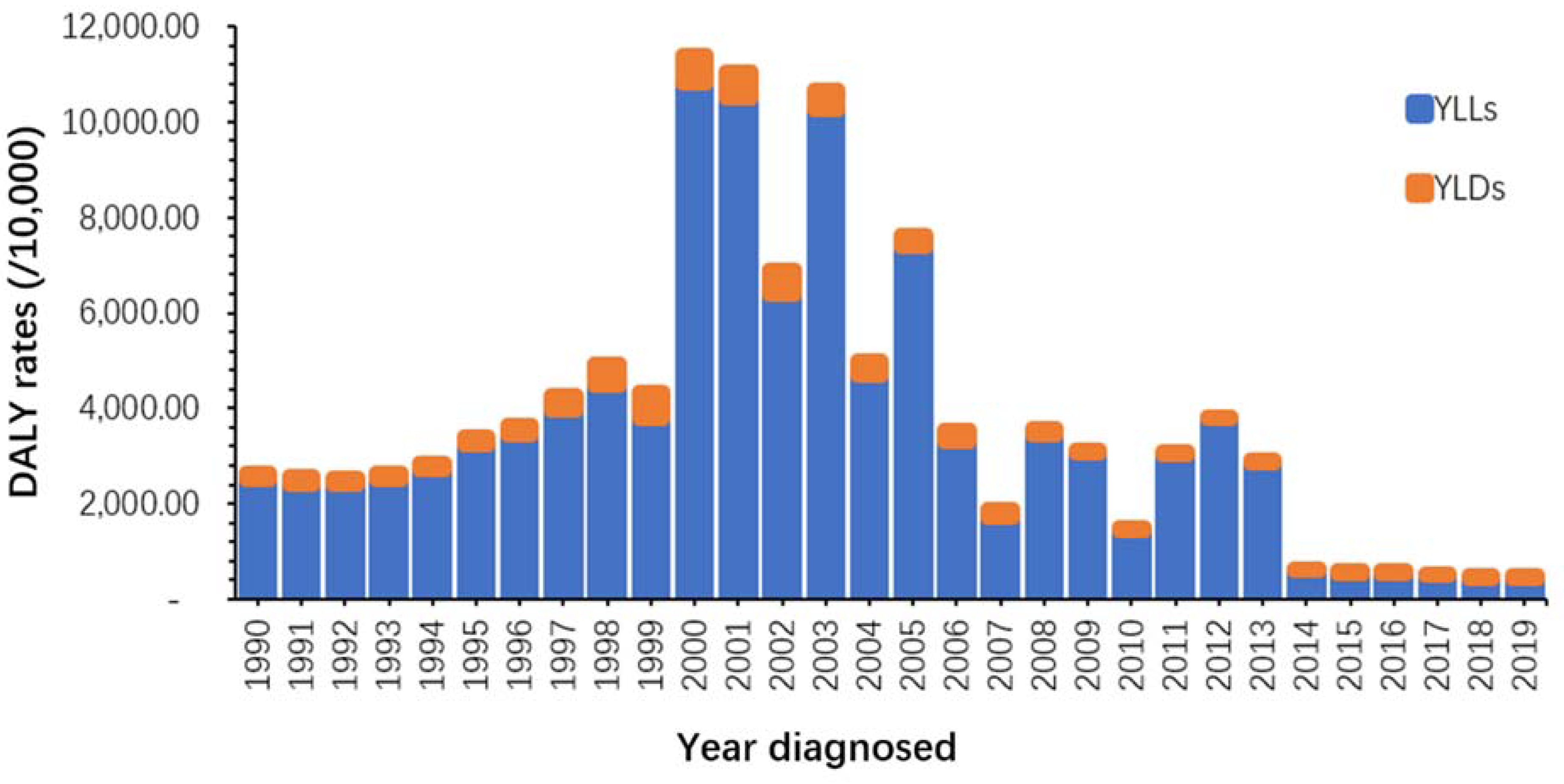
3.1. Descriptive Analysis of Incidence, Mortality, and DALY Rate, 1990–2019
3.2. The Changes in the Burden of Malaria by Gender and Age Groups
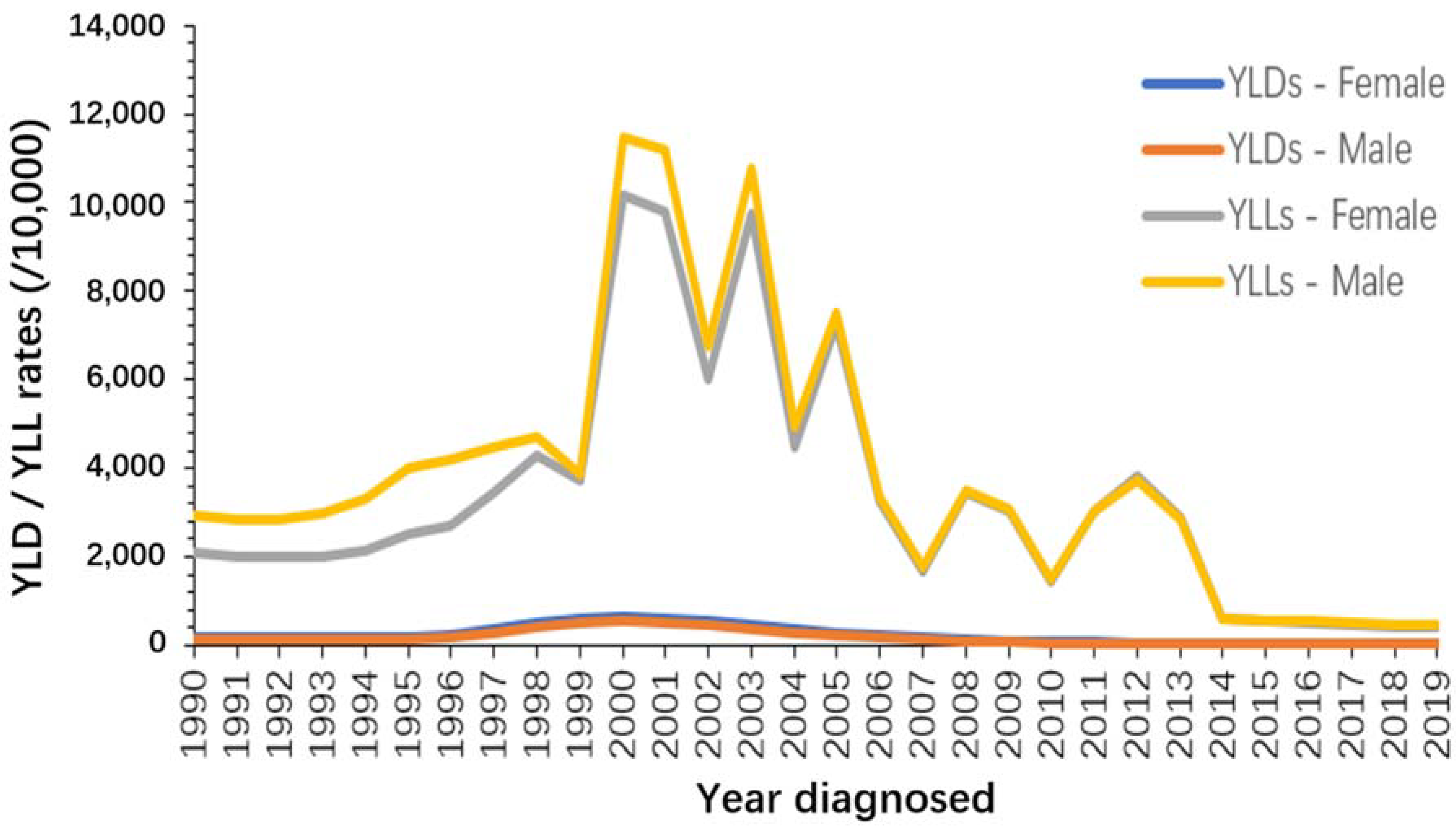
3.2.1. Changes by Gender
3.2.2. Changes by Age
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACT | Artemisinin-combination therapy |
| DALY | Disability-adjusted life years lost |
| YLD | Years of life with disability |
| YLL | Years of life lost due to mortality |
| GBD | Global burden of diseases; GTS: Global technical strategy for malaria |
| IPTp | Intermittent preventive treatment for pregnant women |
| IRS | Indoor residual spray |
| LLNTs | Long-lasting insecticide-treated nets |
| WHO | World Health Organization |
| MDA | Mass drug administration |
| CIR | Crude incidence rate |
| CMR | Crude mortality rate |
| ASIR | Age-standardized incidence rate |
| ASMR | Age-standardized mortality rate |
| ASDR | Age-tandardized DALY rate |
| CNE | Centro Nacional de Endemias |
References
- WHO. World Malaria Report 2020; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2020/ (accessed on 5 December 2021).
- WHO. Health in 2015, from MDG to SDG; World Health Organization: Geneva, Switzerland, 2015; Available online: http://apps.who.int/iris/bitstream/handle/10665/200009/9789241565110_eng.pdf;jsessionid=215780A8419B31A384FE24F8AB927DD7?sequence=1 (accessed on 5 December 2021).
- WHO. Global Technical Strategy for Malaria 2016–2030; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/i/item/9789240031357 (accessed on 5 March 2022).
- WHO. World Malaria Report 2019; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/publications/i/item/9789241565721 (accessed on 17 December 2021).
- Deribew, A.; Dejene, T.; Kebede, B.; Tessema, G.A.; Melaku, Y.A.; Misganaw, A.; Gebre, T.; Hailu, A.; Biadgilign, S.; Amberbir, A.; et al. Incidence, prevalence and mortality rates of malaria in Ethiopia from 1990 to 2015: Analysis of the global burden of diseases 2015. Malar. J. 2017, 16, 271. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde. Anuário Estatístico da Saúde 2020; Ministério da Saúde: Lisbon, Portugal, 2020; unpublished work. [Google Scholar]
- Centro Nacional de Endemias. Protocolos ou Gestão de Casos de Paludismo; Centro Nacional de Endemias: Lisbon, Portugal, 2018; unpublished work. [Google Scholar]
- Badirzadeh, A.; Naderimagham, S.; Asadgol, Z.; Mokhayeri, Y.; Khosravi, A.; Tohidnejad, E.; Vosoogh-Moghaddam, A.; Khoshdel, A.; Rezaei, N.; Kompani, F. Burden of Malaria in Iran, 1990–2010: Findings from the Global Burden of Disease Study 2010. Arch Iran Med. 2016, 19, 241–247. [Google Scholar] [PubMed]
- Gunda, R.; Chimbari, M.J.; Mukaratirwa, S. Assessment of Burden of Malaria in Gwanda District, Zimbabwe, Using the Disability Adjusted Life Years. Int. J. Environ. Res. Public Health 2016, 13, 244. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.L.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- Diseases, G.B.D.; Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar]
- Murray, C.J. Quantifying the burden of disease: The technical basis for disability-adjusted life years. Bull. World Health Organ. 1994, 72, 429–445. [Google Scholar] [PubMed]
- Jha, R.P.; Shri, N.; Patel, P.; Dhamnetiya, D.; Bhattacharyya, K.; Singh, M. Trends in the diabetes incidence and mortality in India from 1990 to 2019: A joinpoint and age-period-cohort analysis. J. Diabetes Metab. Disord. 2021, 20, 1725–1740. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-S.; Zeichner, S.; Anderson, R.N.; Espey, D.K.; Kim, H.-J.; Feuer, E.J. The Joinpoint-Jump and Joinpoint-Comparability Ratio Model for Trend Analysis with Applications to Coding Changes in Health Statistics. J. Off. Stat. 2020, 36, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Centro Nacional de Endemias. Revisão dos Programas Nacionais de Luta Contra o Paludismo, Componente de Gestão do Programa; Centro Nacional de Endemias: Lisbon, Portugal, 2011; unpublished work. [Google Scholar]
- Chen, Y.A.; Lien, J.C.; Tseng, L.F.; Cheng, C.F.; Lin, W.Y.; Wang, H.Y.; Tsai, K.H. Effects of indoor residual spraying and outdoor larval control on Anopheles coluzzii from Sao Tome and Principe, two islands with pre-eliminated malaria. Malar. J. 2019, 18, 405. [Google Scholar] [CrossRef] [PubMed]
- Teklehaimanot, H.D.; Kiszewski, A.; Teklehaimanot, A.; Rampao, H.S.; Sachs, J.D. Malaria in Sao Tome and principe: On the brink of elimination after three years of effective antimalarial measures. Am. J. Trop. Med. Hyg. 2009, 80, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Centro Nacional de Endemias. Revisão do Programa Nacional de Luta Contra o Paludismo; Centro Nacional de Endemias: Lisbon, Portugal, 2016; unpublished work. [Google Scholar]
- Lee, P.-W.; Liu, C.-T.; Rosario, V.E.D.; de Sousa, B.; Rampao, H.S.; Shaio, M.-F. Potential threat of malaria epidemics in a low transmission area, as exemplified by Sao Tome and Principe. Malar. J. 2010, 9, 264. [Google Scholar] [CrossRef]
- Centro Nacional de Endemias. Nálise da Situação Epidemiologica do Paludismo em São Tomé e Principe; Centro Nacional de Endemias: Lisbon, Portugal, 2022; unpublished work. [Google Scholar]
- Liu, Q.; Jing, W.; Kang, L.; Liu, J.; Liu, M. Trends of the global, regional and national incidence of malaria in 204 countries from 1990 to 2019 and implications for malaria prevention. J. Travel Med. 2021, 28, taab046. [Google Scholar] [CrossRef]
- Centro Nacional de Endemias. Relatório Anual das Actividades do Programa Nacional de Luta Contra o Paludismo; Centro Nacional de Endemias: Lisbon, Portugal, 2022; unpublished work. [Google Scholar]
- Li, M.; Tuo, F.; Tan, R.; Zhang, H.; Zheng, S.; Wang, Q.; Xu, Q.; Yu, X.; Lu, F.; Wu, Z.; et al. Mass Drug Administration With Artemisinin-Piperaquine for the Elimination of Residual Foci of Malaria in Sao Tome Island. Front. Med. 2021, 8, 617195. [Google Scholar] [CrossRef] [PubMed]
- Weiss, D.J.; Lucas, T.C.; Nguyen, M.; Nandi, A.K.; Bisanzio, D.; Battle, K.E.; Cameron, E.; Twohig, K.A.; Pfeffer, D.A.; Rozier, J.A.; et al. Mapping the global prevalence, incidence, and mortality of Plasmodium falciparum, 2000–2017: A spatial and temporal modelling study. Lancet 2019, 394, 322–331. [Google Scholar] [CrossRef]



| 1990 | 1995 | 2000 | 2005 | 2010 | 2015 | 2019 | 1990–2019 | |
|---|---|---|---|---|---|---|---|---|
| Relative Change (%) | ||||||||
| CIR | 18,089.54 | 17,248.51 | 63,243.40 | 36,205.95 | 4799.02 | 3098.04 | 3281.93 | −81.86 |
| CMR | 43.11 | 49.26 | 128.54 | 95.45 | 18.60 | 7.19 | 6.03 | −86.02 |
| DALY Rate | 2655.12 | 3397.66 | 11,394.78 | 7643.16 | 1504.96 | 597.26 | 490.85 | −81.51 |
| ASIR | 14,512.31 | 14,438.51 | 44,647.26 | 27,896.06 | 4819.97 | 3183.65 | 3325.66 | −77.08 |
| ASMR | 52.20 | 50.93 | 83.24 | 76.47 | 15.95 | 6.89 | 6.35 | −87.84 |
| ASDR | 2601.49 | 2934.76 | 7220.89 | 5436.51 | 1152.30 | 518.42 | 462.92 | −82.21 |
| 1990 | 1995 | 2000 | 2005 | 2010 | 2015 | 2019 | APC (%) | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Ages | |||||||||
| <5 years | 33,546.98 | 27,378.15 | 157,419.85 | 76,221.54 | 4330.17 | 2262.33 | 2457.29 | −8.4 a | (−10.8, −6) |
| 5–14 years | 20,656.17 | 17,679.31 | 91,584.68 | 43,317.22 | 3979.95 | 2395.90 | 2536.42 | −6.8 a | (−8.9, −4.6) |
| 15–49 years | 13,595.59 | 16,125.09 | 24,514.12 | 24,987.67 | 5483.41 | 3662.17 | 3812.33 | −4.2 a | (−4.7, −3.7) |
| 50–69 years | 5665.86 | 5820.32 | 5882.16 | 6285.00 | 4472.32 | 3248.68 | 3349.68 | −1.8 a | (−2, −1.7) |
| ≥70 years | 3691.91 | 3140.14 | 1645.66 | 1596.39 | 1924.98 | 3020.50 | 3097.37 | −0.6 a | (−1.2, −0.1) |
| Both | 18,089.54 | 17,248.51 | 63,243.40 | 36,205.95 | 4799.02 | 3098.04 | 3281.93 | −5.6 | (−6.9, −4.2) |
| 1990 | 1995 | 2000 | 2005 | 2010 | 2015 | 2019 | APC (%) | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Ages | |||||||||
| <5 years | 61.74 | 106.42 | 669.65 | 404.65 | 88.88 | 37.75 | 33.22 | −0.9 | (−4.4, 2.6) |
| 5–14 years | 5.10 | 3.62 | 17.45 | 4.93 | 0.40 | 0.14 | 0.12 | −12.4 | (−28.9, 7.9) |
| 15–49 years | 44.73 | 52.17 | 25.46 | 46.69 | 7.53 | 3.12 | 2.67 | −8.9 a | (−11.3, −6.5) |
| 50–69 years | 94.56 | 67.97 | 17.06 | 59.75 | 14.58 | 6.44 | 6.15 | −12 a | (−18.9, −4.6) |
| ≥70 years | 141.97 | 92.27 | 15.98 | 79.96 | 16.72 | 7.44 | 11.42 | −10.8 | (−22.6, 2.9) |
| Both | 52.20 | 50.93 | 83.24 | 76.47 | 15.95 | 6.89 | 6.35 | −6.2 a | (−9.6, −2.6) |
| 1990 | 1995 | 2000 | 2005 | 2010 | 2015 | 2019 | APC (%) | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Ages | |||||||||
| <5 years | 5599.56 | 9504.15 | 59,194.34 | 35,690.86 | 7827.09 | 3340.23 | 2939.79 | −1 | (−4.5, 2.5) |
| 5–14 years | 608.33 | 458.09 | 2277.93 | 736.05 | 99.58 | 67.11 | 65.17 | −8.1 | (−15.8, 0.4) |
| 15–49 years | 2882.10 | 3429.81 | 2062.17 | 3141.75 | 536.33 | 249.84 | 221.46 | −8.5 a | (−10.5, −6.5) |
| 50–69 years | 2903.33 | 2087.28 | 671.10 | 1901.75 | 486.91 | 231.44 | 220.92 | −11 a | (−17.1, −4.5) |
| ≥70 years | 2346.76 | 1587.78 | 436.33 | 1407.74 | 318.93 | 146.98 | 204.38 | −10.7 a | (−16.8, −4.3) |
| Both | 2655.12 | 3397.66 | 11,394.78 | 7643.16 | 1504.96 | 597.26 | 490.85 | −5 a | (−8.3, −1.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Li, M.; Guo, W.; Deng, C.; Zou, G.; Song, J. Burden of Malaria in Sao Tome and Principe, 1990–2019: Findings from the Global Burden of Disease Study 2019. Int. J. Environ. Res. Public Health 2022, 19, 14817. https://doi.org/10.3390/ijerph192214817
Wang Y, Li M, Guo W, Deng C, Zou G, Song J. Burden of Malaria in Sao Tome and Principe, 1990–2019: Findings from the Global Burden of Disease Study 2019. International Journal of Environmental Research and Public Health. 2022; 19(22):14817. https://doi.org/10.3390/ijerph192214817
Chicago/Turabian StyleWang, Yuxin, Mingqiang Li, Wenfeng Guo, Changsheng Deng, Guanyang Zou, and Jianping Song. 2022. "Burden of Malaria in Sao Tome and Principe, 1990–2019: Findings from the Global Burden of Disease Study 2019" International Journal of Environmental Research and Public Health 19, no. 22: 14817. https://doi.org/10.3390/ijerph192214817
APA StyleWang, Y., Li, M., Guo, W., Deng, C., Zou, G., & Song, J. (2022). Burden of Malaria in Sao Tome and Principe, 1990–2019: Findings from the Global Burden of Disease Study 2019. International Journal of Environmental Research and Public Health, 19(22), 14817. https://doi.org/10.3390/ijerph192214817





