Psychometric Properties of the Brazilian Version of GOHAI among Community-Dwelling Elderly People
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Ethics
2.2. The GOHAI Instrument
2.3. Brazilian Version of GOHAI
2.4. Data Collection and Measures
2.5. Statistical Analysis
2.5.1. Descriptive
2.5.2. Dimensional Structure and Adequacy of Components
2.5.3. Reliability
2.5.4. Validity
3. Results
3.1. Descriptive
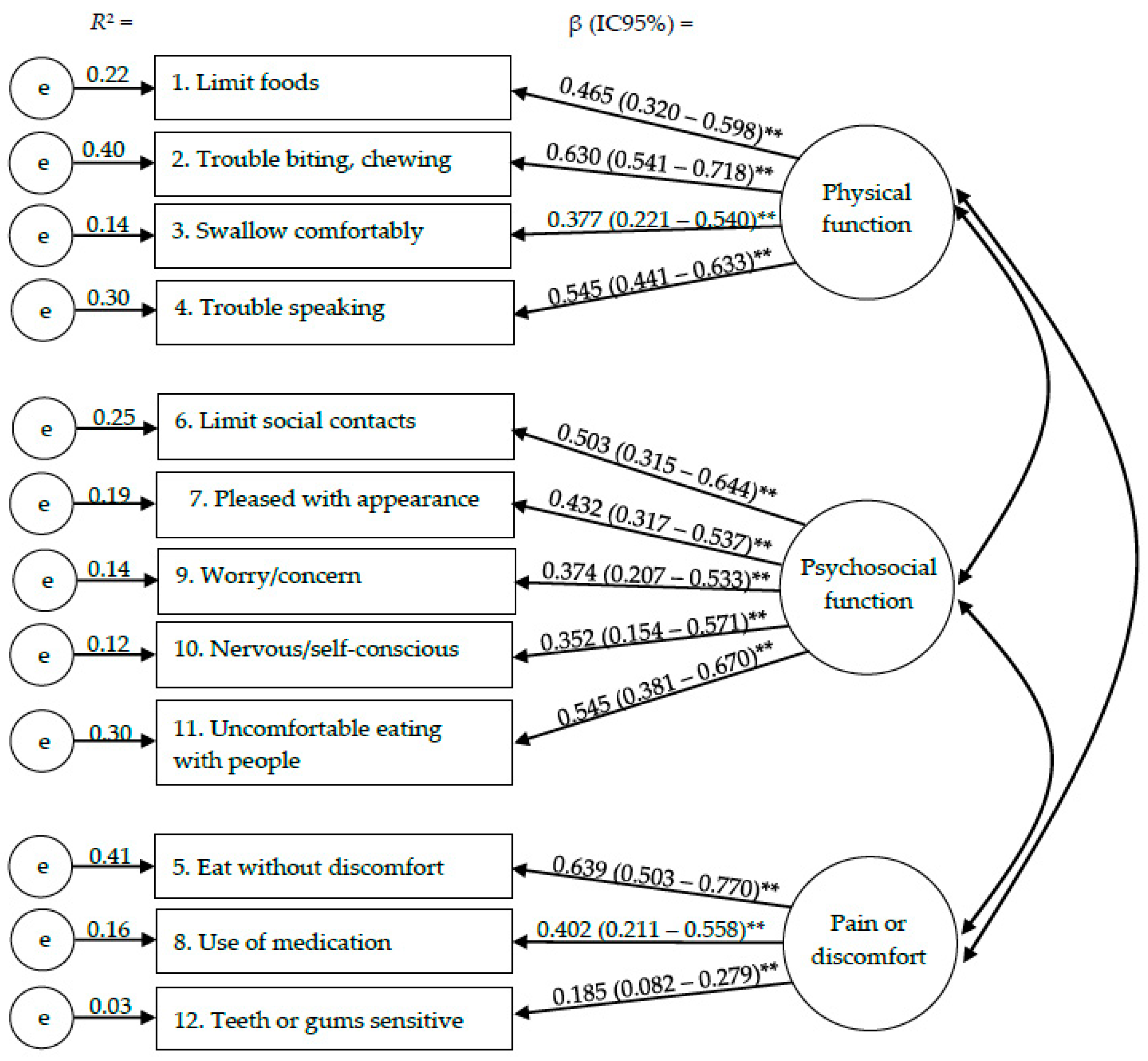
3.2. Dimensional Structure and Adequacy of Components
3.3. Reliability
3.4. Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Institute on Ageing; National Institutes of Health. No 07-6134. Why Population Aging Matters: A Global Perspective. 2007. Available online: https://www.nia.nih.gov/sites/default/files/2017-06/WPAM.pdf (accessed on 10 September 2022).
- Powell, J.L.; Cook, I.G. Global ageing in comparative perspective: A critical discussion. Int. J. Sociol. Social Policy 2009, 29, 388–400. [Google Scholar] [CrossRef]
- GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef]
- Petersen, P.E.; Kandelman, D.; Arpin, S.; Ogawa, H. Global oral health of older people-call for public health action. Community Dent. Health 2010, 27, 257S–267S. [Google Scholar] [CrossRef]
- Sischo, L.; Broder, H.L. Oral Health-related Quality of Life: What, Why, How, and Future Implications. J. Dent. Res. 2011, 90, 1264–1270. [Google Scholar] [CrossRef]
- Locker, D.; Allen, F. What do measures of ‘oral health related quality of life’ measure? Comm. Dent. Oral Epidemiol. 2007, 35, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Gift, H. Oral health outcomes research—Challenges and opportunities. In Measuring Oral Health and Quality of Life; Slade, G.D., Ed.; University of North Carolina, Dental Ecology: Chapel Hill, NC, USA, 1997; pp. 25–46. [Google Scholar]
- Atchison, K.A.; Dolan, T.A. Development of the Geriatric Oral Health Assessment Index. J. Dent. Educ. 1990, 54, 680–687. [Google Scholar] [CrossRef]
- Atchison, K.A. The general oral health assessment index (The Geriatric Oral Health Assessment Index). In Measuring Oral Health and Quality of Life; Slade, G.D., Ed.; University of North Carolina, Dental Ecology: Chapel Hill, NC, USA, 1997; pp. 71–80. [Google Scholar]
- Arnaiz, A.; Zumárraga, M.; Díez-Altuna, I.; Uriarte, J.J.; Moro, J.; Pérez-Ansorena, M.A. Oral health and the symptoms of schizophrenia. Psychiatry Res. 2011, 188, 24–28. [Google Scholar] [CrossRef]
- Hägglin, C.; Berggren, U.; Lundgren, J. A Swedish version of the GOHAI index Psychometric properties and validation. Swed. Dent. J. 2005, 29, 113–124. [Google Scholar]
- Atieh, M.A. Arabic version of the geriatric oral health assessment Index. Gerodontology 2008, 25, 34–41. [Google Scholar] [CrossRef]
- Hassel, A.J.; Rolko, C.; Koke, U.; Leisen, J.; Rammelsberg, P. A German version of the GOHAI. Comm. Dent. Oral Epidemiol. 2008, 36, 34–42. [Google Scholar] [CrossRef]
- Niesten, D.; Witter, D.; Bronkhorst, E.; Creugers, N. Validation of a Dutch version of the Geriatric Oral Health Assessment Index (GOHAI-NL) in care-dependent and care-independent older people. BMC Geriatr. 2016, 16, 53. [Google Scholar] [CrossRef] [PubMed]
- Denis, F.; Hamad, M.; Trojak, B.; Tubert-Jeannin, S.; Rat, C.; Pelletier, J.; Rude, N. Psychometric characteristics of the “General Oral Health Assessment Index (GOHAI) » in a French representative sample of patients with schizophrenia. BMC Oral Health 2017, 17, 75. [Google Scholar] [CrossRef] [PubMed]
- Aguirre-Bustamante, J.; Barón-López, F.J.; Carmona-González, F.J.; Pérez-Farinós, N.; Wärnberg, J. Validation of a modified version of the Spanish Geriatric Oral Health Assessment Index (GOHAI-SP) for adults and elder People. BMC Oral Health 2020, 20, 61. [Google Scholar] [CrossRef] [PubMed]
- Silva, S.R.C. Autopercepção das Condições Bucais em Pessoas com 60 anos e mais de Idade. Ph.D. Thesis, Faculdade de Saúde Pública, Universidade de São Paulo, São Paulo, Brazil, 1999. [Google Scholar]
- Silva, S.R.; Fernandes, R.A.C. Self-perception of oral health status by the elderly. Rev. Saude Publica 2001, 35, 349–355. [Google Scholar] [CrossRef][Green Version]
- Silva, D.D.; Sousa, M.L.R.; Wada, R.S. Self-perception and oral health conditions in an elderly population. Cad. Saúde Pública 2005, 21, 1251–1259. [Google Scholar] [CrossRef][Green Version]
- Rebelo, M.A.B.; Cardoso, E.M.; Robinson, P.G.; Vettore, M.V. Demographics, social position, dental status and oral health-related quality of life in community-dwelling older adults. Qual. Life Res. 2016, 25, 1735–1742. [Google Scholar] [CrossRef]
- Souza, R.F.; Terada, A.S.S.D.; Vecchia, M.P.D.; Regis, R.R.; Zanini, A.P.; Compagnoni, M.A. Validation of the Brazilian versions of two inventories for measuring oral health-related quality of life of edentulous subjects. Gerodontology 2012, 29, e88–e95. [Google Scholar] [CrossRef]
- Cardoso, A.M.; Parente, R.C.P.; Vettore, M.V.; Rebelo, M.A.B. Oral health conditions of older residents in the city of Manaus, Amazonas: Estimates by sex oral health. Rev. Bras. Epidemiol. 2011, 14, 1–10. [Google Scholar] [CrossRef][Green Version]
- Brucki, S.M.D.; Malheiros, S.M.F.; Okamoto, I.H.; Bertolucci, P.H.F. Dados normativos para o teste de fluência verbal: Categorias animais em nosso meio. Arq. Neuropsiquiatr. 1997, 55, 56–61. [Google Scholar] [CrossRef]
- Ministério da Saúde, Coordenação Nacional de Saúde Bucal. Condições de Saúde Bucal da População Brasileira 2002–2003 Resultados Principais; Editora MS; Ministério da Saúde, Coordenação Nacional de Saúde Bucal: Rio de Janeiro, Brazil, 2004.
- Jensen, M.P.; Karoly, P.; Braver, S. The measurement of clinical pain intensity: A comparison of six methods. Pain 1986, 27, 117–126. [Google Scholar] [CrossRef]
- WHO (World Health Organization). Oral Health Surveys, Basic Methods, 4th ed.; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Sheiham, A.; Steele, J.G.; Marcenes, W.; Finch, W.; Walls, A.W. The impact of oral health on stated ability to eat certain foods; findings from the National Diet and Nutrition Survey of Older People in Great Britain. Gerodontology 1999, 16, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Ainamo, J.; Barmes, D.; Beagrie, G.; Cutress, T.; Martin, J.; Sardo-Infirri, J. Development of the World Health Organization (WHO) community periodontal index of treatment needs (CPITN). Int. Dent. J. 1982, 32, 281–291. [Google Scholar]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Clark, L.A.; Watson, D. Constructing validity: Basic issues in objective scale development. Psychol. Assess. 1995, 7, 307–319. [Google Scholar] [CrossRef]
- Cronbach, L. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Cronbach’s alpha. BMJ 1997, 314, 572. [Google Scholar] [CrossRef]
- Fleiss, J. The Design and Analysis of Clinical Experiments; John Wiley & Sons: New York, NY, USA, 1986; pp. 1–32. [Google Scholar] [CrossRef]
- Allison, P.; Lockerm, D.; Jocovik, A.; Slade, G. A Cross-cultural Study of Oral Health Values. J. Dent. Res. 1999, 78, 643–649. [Google Scholar] [CrossRef]
- Bastos, R.S.; Sá, L.M.; Velasco, S.R.M.; Teixeira, D.F.; Oaino, L.S.; Vettore, M.V. Frailty and oral health-related quality of life in community-dwelling older adults: A cross-sectional study. Braz. Oral Res. 2021, 35, e139. [Google Scholar] [CrossRef]
- Osta, N.E.; Haddad, E.; Fakhouri, J.; Saad, R.; Osta, L.E. Comparison of psychometric properties of GOHAI, OHIP-14 and OHIP-EDENT as measures of oral health in complete edentulous patients aged 60 years and more. Qual. Life Res. 2021, 30, 1199–1213. [Google Scholar] [CrossRef]
- Nelson, S.; Albert, J.M.; Liu, Y.; Selvaraj, D.; Curtan, S.; Ryan, K.; Pinto, A.; Ejaz, F.; Milgrom, P.; Riedy, C. The psychometric properties of a new oral health illness perception measure for adults aged 62 years and older. PLoS ONE 2019, 14, e0214082. [Google Scholar] [CrossRef]
| Item | Dimension | In the Past Three Months (Nos últimos três meses) | (1) A (S) | (2) S (AV) | (3) N (N) |
|---|---|---|---|---|---|
| 1 | Physical function | How often did you limit the kinds or amounts of food you eat because of problems with your teeth or denture? | 13 (2.1) | 43 (7.0) | 557 (90.9) |
| Você diminuiu a quantidade de alimentos ou mudou o tipo de alimentação por causa de seus dentes? | |||||
| 2 | Physical function | How often did you have trouble biting or chewing any kinds of food, such as a firm meat or apples? | 33 (5.4) | 113 (18.4) | 467 (76.2) |
| Você teve problemas para mastigar os alimentos? | |||||
| 3 | Physical function | How often were you able to swallow comfortably? | 6 (1.0) | 30 (4.9) | 577 (94.1) |
| Você teve dor ou desconforto para engolir alimentos? | |||||
| 4 | Physical function | How often have your teeth or dentures prevented you from speaking the way you wanted? | 25 (4.1) | 89 (14.5) | 499 (81.4) |
| Você mudou o jeito de falar por causa dos problemas em sua boca? | |||||
| 5 | Pain or discomfort | How often were you able to eat anything without feeling discomfort? | 16 (2.6) | 91 (14.8) | 506 (82.5) |
| Você sentiu algum desconforto ao comer algum alimento? | |||||
| 6 | Psychosocial function | How often did you limit contacts with people because of the condition of your teeth or dentures? | 1 (0.2) | 18 (2.9) | 594 (96.9) |
| Você deixou de se encontrar com outras pessoas por causa de sua boca? | |||||
| 7 | Psychosocial function | How often were you pleased or happy with the appearance of your teeth, gums or dentures? | 460 (75.0) | 71 (11.6) | 82 (13.4) |
| Você se sentiu satisfeito ou feliz com a aparência de sua boca? | |||||
| 8 | Pain or discomfort | How often did you use medication to relieve pain or discomfort around your mouth? | 3 (0.5) | 33 (5.4) | 577 (94.1) |
| Você teve que tomar remédio para passar a dor ou desconforto de sua boca? | |||||
| 9 | Psychosocial function | How often were you worried or concerned about the problems with your teeth, gums or dentures? | 19 (3.1) | 50 (8.2) | 544 (88.7) |
| Você teve algum problema na boca que o deixou preocupado? | |||||
| 10 | Psychosocial function | How often did you feel nervous or self-conscious because of problems with your teeth, gums or dentures? | 4 (0.7) | 26 (4.2) | 583 (95.1) |
| Você chegou a se sentir nervoso por causa de problemas na boca? | |||||
| 11 | Psychosocial function | How often did you feel uncomfortable eating in front of people because of problems with your teeth or dentures? | 20 (3.3) | 33 (5.4) | 560 (91.4) |
| Você evitou comer junto com outras pessoas por causa dos problemas na sua boca? | |||||
| 12 | Pain or discomfort | How often were your teeth or gums sensitive to hot, cold or sweet foods? | 96 (15.7) | 52 (8.5) | 465 (75.9) |
| Você sentiu seus dentes ou a gengiva ficarem sensíveis a alimentos líquidos? |
| Item | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Limit foods | 1 | |||||||||||
| 2. Trouble biting, chewing | 0.330 ** | 1 | ||||||||||
| 3. Swallow comfortably | 0.259 ** | 0.169 ** | 1 | |||||||||
| 4. Trouble speaking | 0.225 ** | 0.347 ** | 0.195 ** | 1 | ||||||||
| 5. Eat without discomfort | 0.273 ** | 0.442 ** | 0.289 ** | 0.413 ** | 1 | |||||||
| 6. Limit social contacts | 0.272 ** | 0.268 ** | 0.201 ** | 0.215 ** | 0.227 ** | 1 | ||||||
| 7. Pleased with appearance | 0.162 ** | 0.284 ** | 0.111 ** | 0.216 ** | 0.229 ** | 0.201 ** | 1 | |||||
| 8. Use of medication | 0.191 ** | 0.283 ** | 0.136 ** | 0.210 ** | 0.271 ** | 0.124 ** | 0.149 ** | 1 | ||||
| 9. Worry/concern | 0.162 ** | 0.185 ** | 0.039 | 0.165 ** | 0.208 ** | 0.165 ** | 0.156 ** | 0.279 ** | 1 | |||
| 10. Nervous/self-conscious | 0.121 ** | 0.115 ** | 0.147 ** | 0.155 ** | 0.224 ** | 0.235 ** | 0.116 ** | 0.238 ** | 0.417 ** | 1 | ||
| 11. Uncomfortable eating with people | 0.218 ** | 0.287 ** | 0.219 ** | 0.238 ** | 0.295 ** | 0.289 ** | 0.240 ** | 0.155 ** | 0.216 ** | 0.169 ** | 1 | |
| 12. Teeth or gums sensitive | 0.096 * | 0.136 ** | 0.048 | 0.133 ** | 0.048 | 0.083 * | 0.085 * | 0.154 ** | 0.122 ** | 0.047 | 0.069 | 1 |
| GOHAI dimensions | ||||||||||||
| Physical function | 0.641 ** | 0.772 ** | 0.489 ** | 0.710 ** | 0.542 * | 0.354 ** | 0.308 ** | 0.317 ** | 0.225 ** | 0.205 ** | 0.360 ** | 0.162 ** |
| Psychosocial function | 0.283 ** | 0.380 ** | 0.207 ** | 0.319 ** | 0.375 ** | 0.460 ** | 0.748 ** | 0.297 ** | 0.609 ** | 0.501 ** | 0.613 ** | 0.134 ** |
| Pain or discomfort | 0.249 ** | 0.381 ** | 0.205 ** | 0.345 ** | 0.570 ** | 0.200 ** | 0.208 ** | 0.504 ** | 0.261 ** | 0.201 ** | 0.229 ** | 0.809 ** |
| Internal Consistency | Stability | ||
|---|---|---|---|
| Item | Item–Scale Correlation a | Cronbach Alpha If Item Deleted | Test–Retest Correlation b |
| 1. Limit foods | 0.369 ** | 0.680 | 0.536 ** |
| 2. Trouble biting, chewing | 0.612 ** | 0.655 | 0.690 ** |
| 3. Swallow comfortably | 0.305 ** | 0.693 | 0.794 ** |
| 4. Trouble speaking | 0.526 ** | 0.668 | 1.000 ** |
| 5. Eat without discomfort | 0.538 ** | 0.661 | 0.717 ** |
| 6. Limit social contacts | 0.272 ** | 0.692 | 1.000 ** |
| 7. Pleased with appearance | 0.560 ** | 0.694 | 0.917 ** |
| 8. Use of medication | 0.326 ** | 0.686 | 0.833 ** |
| 9. Worry/concern | 0.410 ** | 0.685 | 0.981 ** |
| 10. Nervous/self-conscious | 0.292 ** | 0.693 | 0.646 ** |
| 11. Uncomfortable eating with people | 0.385 ** | 0.677 | 0.864 ** |
| 12. Teeth or gums sensitive | 0.433 ** | 0.733 | 0.881 ** |
| GOHAI | |||
| GOHAI total | |||
| ADD-score | – | – | 0.822 ** |
| SC-score | – | – | 0.881 ** |
| Physical function | |||
| ADD-score | – | – | 0.776 ** |
| SC-score | – | – | 0.760 ** |
| Psychosocial function | |||
| ADD-score | – | – | 0.946 ** |
| SC-score | – | – | 0.955 ** |
| Pain or discomfort | |||
| ADD-score | – | – | 0.859 ** |
| SC-score | – | – | 0.713 ** |
| Total Score | Physical Function | Psychosocial Function | Pain or Discomfort | |||||
|---|---|---|---|---|---|---|---|---|
| Additive Score | Simple Count | Additive Score | Simple Count | Additive Score | Simple Count | Additive Score | Simple Count | |
| Dental pain scale | −0.259 ** | 0.277 ** | −0.171 ** | 0.187 ** | −0.234 ** | 0.236 ** | −0.202 ** | 0.243 ** |
| Self-rated oral health | 0.326 ** | −0.314 ** | 0.162 ** | −0.159 ** | 0.374 ** | −0.348 ** | 0.225 ** | −0.242 ** |
| Self-perceived treatment needs | 0.258 ** | −0.274 ** | 0.167 ** | −0.180 ** | 0.293 ** | −0.292 ** | 0.126 ** | −0.171 ** |
| Self-perceived dental appearance | 0.299 ** | −0.295 ** | 0.229 ** | −0.220 ** | 0.314 ** | −0.288 ** | 0.139 ** | −0.183 ** |
| Self-perceived masticatory function | 0.439 ** | −0.453 ** | 0.437 ** | −0.448 ** | 0.345 ** | −0.326 ** | 0.241 ** | −0.285 ** |
| Self-perceived speaking function | 0.367 ** | −0.378 ** | 0.414 ** | −0.418 ** | 0.265 ** | −0.255 ** | 0.160 ** | −0.202 ** |
| Self-perceived social function | −0.250 ** | 0.244 ** | −0.174 ** | 0.162 ** | −0.263 ** | 0.255 | −0.131 ** | 0.155 ** |
| GOHAI Total Score | GOHAI Physical Function | GOHAI Psychosocial Function | GOHAI Pain or Discomfort | |
|---|---|---|---|---|
| Need of total dental prosthesis | ||||
| None | Ref | Ref | Ref | Ref |
| Upper or lower total dental prosthesis | 0.007 (−0.009/0.022) | 0.001 (−0.021/0.022) | 0.009 (−0.007/0.025) | 0.010 (−0.015/0.035) |
| Upper and lower total dental prosthesis | −0.021 (−0.038/−0.004) * | −0.029 (−0.052/−0.006) * | −0.024 (−0.043/−0.005) * | −0.005 (−0.028/0.019) |
| Functional dentition | ||||
| No (<20 teeth) | Ref | Ref | Ref | Ref |
| Yes (≥20 teeth) | 0.046 (0.016/0.076) ** | 0.048 (0.024/0.071) ** | 0.044 (0.001/0.087) * | 0.045 (−0.005/0095) |
| Number of decayed teeth | −0.007 (−0.012/0.003) ** | −0.006 (−0.010/−0.001) * | −0.009 (−0.015/−0.004) ** | −0.006 (−0.013/0.001) |
| Number of sextants with bleeding on probing | ||||
| 0 | −0.007 (−0.039/0.025) | 0.017 (−0.046/0.081) | −0.002 (−0.047/0.043) | −0.025 (−0.080/0.029) |
| 1 | 0.008 (−0.054/0.071) | 0.001 (−0.029/0.029) | −0.028 (−0.146/0.090) | 0.053 (−0.031/0.136) |
| 2 | Ref | Ref | Ref | Ref |
| Number of sextants with dental calculus | ||||
| 0 | 0.081 (0.055/0.107) ** | 0.057 (0.037/0.076) ** | 0.072 (0.004/0.141) * | 0.130 (0.070/0.191) ** |
| 1 | 0.069 (0.028/0.113) ** | 0.071 (0.054/0.089) ** | 0.057 (−0.011/0.126) | 0.126 (0.006/0.187) ** |
| 2 | 0.069 (0.025/0.113) ** | 0.032 (−0.033/0.097) | 0.050 (−0.028/0.127) | 0.152 (0.074/0.230) ** |
| 3 | 0.072 (0.011/0.134) * | 0.059 (0.005/0.112) * | 0.049 (−0.041/0.139) | 0.131 (0.024/0.237) * |
| 4 | Ref | Ref | Ref | Ref |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vettore, M.V.; Rebelo, M.A.B.; Rebelo Vieira, J.M.; Cardoso, E.M.; Birman, D.; Leão, A.T.T. Psychometric Properties of the Brazilian Version of GOHAI among Community-Dwelling Elderly People. Int. J. Environ. Res. Public Health 2022, 19, 14725. https://doi.org/10.3390/ijerph192214725
Vettore MV, Rebelo MAB, Rebelo Vieira JM, Cardoso EM, Birman D, Leão ATT. Psychometric Properties of the Brazilian Version of GOHAI among Community-Dwelling Elderly People. International Journal of Environmental Research and Public Health. 2022; 19(22):14725. https://doi.org/10.3390/ijerph192214725
Chicago/Turabian StyleVettore, Mario Vianna, Maria Augusta Bessa Rebelo, Janete Maria Rebelo Vieira, Evangeline Maria Cardoso, Dina Birman, and Anna Thereza Thomé Leão. 2022. "Psychometric Properties of the Brazilian Version of GOHAI among Community-Dwelling Elderly People" International Journal of Environmental Research and Public Health 19, no. 22: 14725. https://doi.org/10.3390/ijerph192214725
APA StyleVettore, M. V., Rebelo, M. A. B., Rebelo Vieira, J. M., Cardoso, E. M., Birman, D., & Leão, A. T. T. (2022). Psychometric Properties of the Brazilian Version of GOHAI among Community-Dwelling Elderly People. International Journal of Environmental Research and Public Health, 19(22), 14725. https://doi.org/10.3390/ijerph192214725





