The Prevalence, Indications, Outcomes of the Most Common Major Gynecological Surgeries in Kazakhstan and Recommendations for Potential Improvements into Public Health and Clinical Practice: Analysis of the National Electronic Healthcare System (2014–2019)
Abstract
1. Introduction
2. Materials and Methods
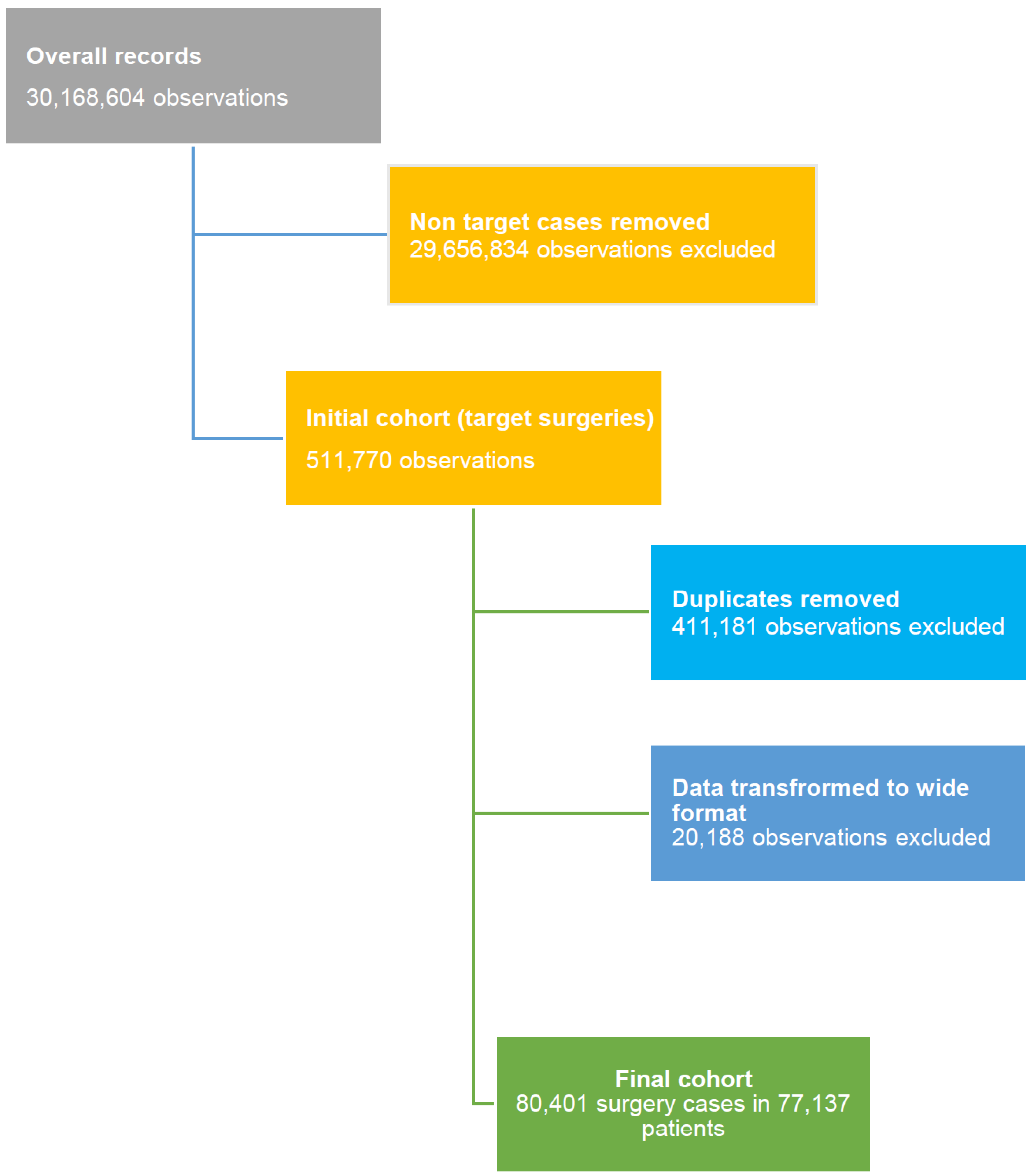
2.1. Study Population and Data Sources
2.2. Patients Selection and Definitions
2.3. Ethical Approval
2.4. Statistical Analysis
3. Results
3.1. Study Subjects Description
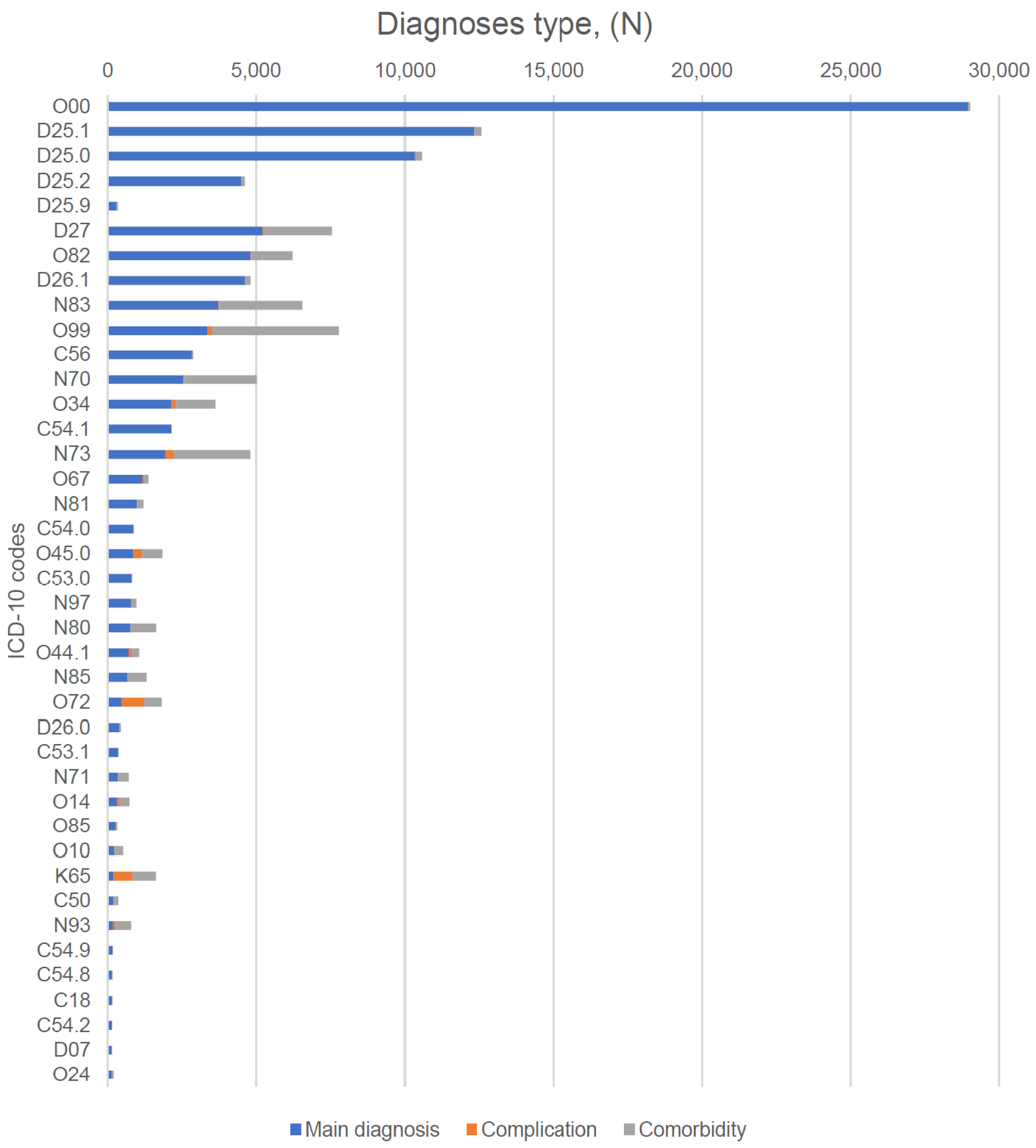
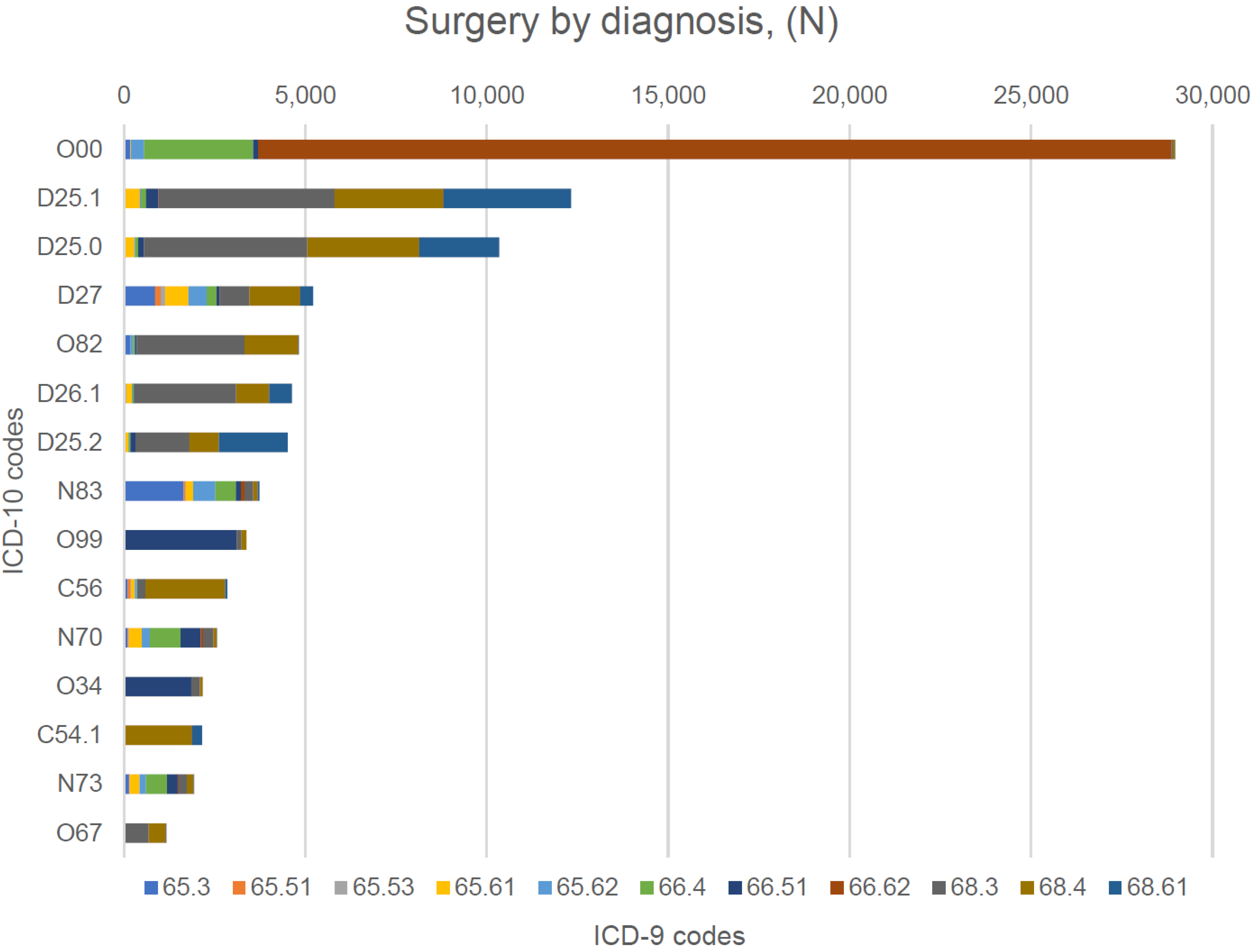
3.2. Analysis of the Surgical Procedures by Type, Indications, and Approach
3.3. Mortality Rates among the Study Population and Cox Regression Analysis of the Mortality
4. Discussion
4.1. Public Health Implications for Healthcare Improvements in Kazakhstan
4.2. Outcomes of the Gynecological Surgeries in Kazakhstan and Recommendations for Potential Improvements
4.3. Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ortiz-Martínez, R.A.; Betancourt-Cañas, A.J.; Bolaños-Náñez, D.M.; Cardona-Narváez, T.; Portilla, E.D.; Flórez-Victoria, O. Prevalence of surgical complications in gynecological surgery at the Hospital Universitario San José in Popayán, Colombia. 2015. Rev. Fac. Med. 2018, 66, 529–535. [Google Scholar] [CrossRef]
- Ramdhan, R.C.; Loukas, M.; Tubbs, R.S. Anatomical complications of hysterectomy: A review. Clin. Anat. 2017, 30, 946–952. [Google Scholar] [CrossRef] [PubMed]
- Harnod, T.; Chen, W.; Wang, J.-H.; Lin, S.-Z.; Ding, D.-C. Hysterectomies Are Associated with an Increased Risk of Depression: A Population-Based Cohort Study. J. Clin. Med. 2018, 7, 366. [Google Scholar] [CrossRef] [PubMed]
- Orhan, A.; Ozerkan, K.; Kasapoglu, I.; Ocakoglu, G.; Demir, B.C.; Gunaydin, T.; Uncu, G. Laparoscopic hysterectomy trends in challenging cases (1995–2018). J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Clarke-Pearson, D.L.; Geller, E.J. Complications of hysterectomy. Obstet. Gynecol. 2013, 121, 654–673. [Google Scholar] [CrossRef]
- Dedden, S.J.; Geomini, P.M.; Huirne, J.A.; Bongers, M.Y. Vaginal and Laparoscopic hysterectomy as an outpatient procedure: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 216, 212–223. [Google Scholar] [CrossRef]
- Lozada, Y.; Bhagavath, B. A Review of Laparoscopic Salpingo-Oophorectomy: Technique and Perioperative Considerations. J. Minim. Invasive Gynecol. 2017, 24, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Aarts, J.W.; E Nieboer, T.; Johnson, N.; Tavender, E.; Garry, R.; Mol, B.W.J.; Kluivers, K.B. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst. Rev. 2015, 2015, CD003677. [Google Scholar] [CrossRef]
- Lycke, K.D.; Kahlert, J.; Damgaard, R.; Mogensen, O.; Hammer, A. Trends in Hysterectomy Incidence Rates During 2000–2015 in Denmark: Shifting from Abdominal to Minimally Invasive Surgical Procedures. Clin. Epidemiol. 2021, 13, 407–416. [Google Scholar] [CrossRef]
- Jacoby, V.L.; Autry, A.; Jacobson, G.; Domush, R.; Nakagawa, S.; Jacoby, A. Nationwide Use of Laparoscopic Hysterectomy Compared With Abdominal and Vaginal Approaches. Obstet. Gynecol. 2009, 114, 1041–1048. [Google Scholar] [CrossRef]
- Fortin, C.; Hur, C.; Falcone, T. Impact of Laparoscopic Hysterectomy on Quality of Life. J. Minim. Invasive Gynecol. 2019, 26, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Brummer, T.H.; Jalkanen, J.; Fraser, J.; Heikkinen, A.M.; Kauko, M.; Mäkinen, J.; Seppälä, T.; Sjöberg, J.; Tomás, E.; Härkki, P. FINHYST, a prospective study of 5279 hysterectomies: Complications and their risk factors. Hum. Reprod. 2011, 26, 1741–1751. [Google Scholar] [CrossRef] [PubMed]
- McPherson, K.; Metcalfe, M.; Herbert, A.; Maresh, M.; Casbard, A.; Hargreaves, J.; Bridgman, S.; Clarke, A. Severe complications of hysterectomy: The VALUE study. BJOG 2004, 111, 688–694. [Google Scholar] [CrossRef]
- English, E.M.; Bell, S.; Kamdar, N.S.; Swenson, C.W.; Wiese, H.; Morgan, D.M. Importance of Estimated Blood Loss in Resource Utilization and Complications of Hysterectomy for Benign Indications. Obstet. Gynecol. 2019, 133, 650–657. [Google Scholar] [CrossRef] [PubMed]
- Ellinides, A.; Manolopoulos, P.P.; Hajymiri, M.; Sergentanis, T.N.; Trompoukis, P.; Ntourakis, D. Outpatient Hysterectomy versus Inpatient Hysterectomy: A Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2022, 29, 23–40.e7. [Google Scholar] [CrossRef]
- Uccella, S.; Zorzato, P.C.; Kho, R.M. Incidence and Prevention of Vaginal Cuff Dehiscence after Laparoscopic and Robotic Hysterectomy: A Systematic Review and Meta-analysis. J. Minim. Invasive Gynecol. 2021, 28, 710–720. [Google Scholar] [CrossRef]
- Ozcan, M.C.; Wilson, J.R.; Frishman, G.N. A Systematic Review and Meta-analysis of Surgical Treatment of Ectopic Pregnancy with Salpingectomy versus Salpingostomy. J. Minim. Invasive Gynecol. 2021, 28, 656–667. [Google Scholar] [CrossRef]
- Matulonis, U.A.; Sood, A.K.; Fallowfield, L.; Howitt, B.; Sehouli, J.; Karlan, B.Y. Ovarian cancer. Nat. Rev. Dis. Prim. 2016, 2, 16061. [Google Scholar] [CrossRef]
- Bergsten, T.M.; Burdette, J.E.; Dean, M. Fallopian tube initiation of high grade serous ovarian cancer and ovarian metastasis: Mechanisms and therapeutic implications. Cancer Lett. 2020, 476, 152–160. [Google Scholar] [CrossRef]
- Dilley, S.; Straughn, J.M.; Leath, C.A. The Evolution of and Evidence for Opportunistic Salpingectomy. Obstet. Gynecol. 2017, 130, 814–824. [Google Scholar] [CrossRef]
- ACOG Committee Opinion No. 774: Opportunistic Salpingectomy as a Strategy for Epithelial Ovarian Cancer Prevention. Obstet. Gynecol. 2019, 133, e279–e284. [CrossRef]
- Kotsopoulos, J.; Narod, S.A. Prophylactic salpingectomy for the prevention of ovarian cancer: Who should we target? Int. J. Cancer 2020, 147, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Mills, K.; Marchand, G.; Sainz, K.; Azadi, A.; Ware, K.; Vallejo, J.; Anderson, S.; King, A.; Osborn, A.; Ruther, S.; et al. Salpingectomy vs tubal ligation for sterilization: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2021, 224, 258–265.e4. [Google Scholar] [CrossRef] [PubMed]
- Kyo, S.; Ishikawa, N.; Nakamura, K.; Nakayama, K. The fallopian tube as origin of ovarian cancer: Change of diagnostic and preventive strategies. Cancer Med. 2020, 9, 421–431. [Google Scholar] [CrossRef]
- Evans, E.C.; Matteson, K.A.; Orejuela, F.J.; Alperin, M.; Balk, E.M.; El-Nashar, S.; Gleason, J.L.; Grimes, C.; Jeppson, P.; Mathews, C.; et al. Salpingo-oophorectomy at the Time of Benign Hysterectomy: A Systematic Review. Obstet. Gynecol. 2016, 128, 476–485. [Google Scholar] [CrossRef] [PubMed]
- Kotlyar, A.; Gingold, J.; Shue, S.; Falcone, T. The Effect of Salpingectomy on Ovarian Function. J. Minim. Invasive Gynecol. 2017, 24, 563–578. [Google Scholar] [CrossRef]
- Noventa, M.; Gizzo, S.; Saccardi, C.; Borgato, S.; Vitagliano, A.; Quaranta, M.; Litta, P.; Gangemi, M.; Ambrosini, G.; D’Antona, D.; et al. Salpingectomy before assisted reproductive technologies: A systematic literature review. J. Ovarian Res. 2016, 9, 1–18. [Google Scholar] [CrossRef]
- Luo, J.; Shi, Y.; Liu, D.; Yang, D.; Wu, J.; Cao, L.; Geng, L.; Hou, Z.; Lin, H.; Zhang, Q.; et al. The effect of salpingectomy on the ovarian reserve and ovarian response in ectopic pregnancy: A systematic review and meta-analysis. Medicine 2019, 98, e17901. [Google Scholar] [CrossRef]
- Eleje, G.U.; Eke, A.C.; Ezebialu, I.U.; Ikechebelu, J.I.; Ugwu, E.O.; Okonkwo, O.O. Risk-reducing bilateral salpingo-oophorectomy in women with BRCA1 or BRCA2 mutations. Cochrane Database Syst. Rev. 2018, 8, CD012464. [Google Scholar] [CrossRef]
- The World Bank Country Classification by Income. Available online: https://data.worldbank.org/country (accessed on 18 April 2022).
- Aimagambetova, G.; Sakko, Y.; Gusmanov, A.; Issanov, A.; Ukybassova, T.; Bapayeva, G.; Marat, A.; Nurpeissova, A.; Gaipov, A. The Prevalence, Incidence, Indications and Outcomes of Peripartum Hysterectomy in Kazakhstan: Data from Unified Nationwide Electronic Healthcare System 2014–2018. Int. J. Womens Health 2022, 14, 267–278. [Google Scholar] [CrossRef]
- World Population Review. Kazakhstan. Available online: https://worldpopulationreview.com/countries/kazakhstan-population (accessed on 22 June 2022).
- Kamalbekova, G.; Kalieva, M. Evidence-based medicine Training: Kazakhstan experience. Int. J. Risk Saf. Med. 2015, 27, S95–S96. [Google Scholar] [CrossRef]
- Aketayeva, A.; Khamidullina, Z.; Akhmetova, Z.; Baubekova, A.; Khismetova, Z.; Dudnik, Y.; Aitbaeva, Z. Diagnosis and Treatment of Female Infertility Is One of the Major Problems in Modern Gynecology. Iran. J. Public Health 2018, 47, 135–137. [Google Scholar] [PubMed]
- StataCorp LLC. Stata Statistical Software, Release 16; StataCorp LLC: College Station, TX, USA, 2019. [Google Scholar]
- International Trade Administration. Kazakhstan—Country Commercial Guide. Available online: https://www.trade.gov/country-commercial-guides/kazakhstan-healthcare (accessed on 21 June 2022).
- Ng, K.Y.B.; Cheong, Y. Hydrosalpinx—Salpingostomy, salpingectomy or tubal occlusion. Best Pract. Res. Clin. Obstet. Gynaecol. 2019, 59, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Bapayeva, G.; Aimagambetova, G.; Issanov, A.; Terzic, S.; Ukybassova, T.; Aldiyarova, A.; Utepova, G.; Daribay, Z.; Bekbossinova, G.; Balykov, A.; et al. The Effect of Stress, Anxiety and Depression on In Vitro Fertilization Outcome in Kazakhstani Public Clinical Setting: A Cross-Sectional Study. J. Clin. Med. 2021, 10, 937. [Google Scholar] [CrossRef]
- Issanov, A.; Aimagambetova, G.; Terzic, S.; Bapayeva, G.; Ukybassova, T.; Baikoshkarova, S.; Utepova, G.; Daribay, Z.; Bekbossinova, G.; Balykov, A.; et al. Impact of governmental support to the IVF clinical pregnancy rates: Differences between public and private clinical settings in Kazakhstan—A prospective cohort study. BMJ Open 2022, 12, e049388. [Google Scholar] [CrossRef]
- Ödesjö, E.; Bergh, C.; Strandell, A. Surgical methods for tubal pregnancy—Effects on ovarian response to controlled stimulation during IVF. Acta Obstet. Gynecol. Scand. 2015, 94, 1322–1326. [Google Scholar] [CrossRef] [PubMed]
- Gay, C.; Perrin, J.; Courbiere, B.; Bretelle, F.; Agostini, A. Impact of salpingectomy for ectopic pregnancy on the ovarian response during IVF stimulation. J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 727–730. [Google Scholar] [CrossRef] [PubMed]
- Aimagambetova, G.; Issanov, A.; Terzic, S.; Bapayeva, G.; Ukybassova, T.; Baikoshkarova, S.; Aldiyarova, A.; Shauyen, F.; Terzic, M. The effect of psychological distress on IVF outcomes: Reality or speculations? PLoS ONE 2020, 15, e0242024. [Google Scholar] [CrossRef] [PubMed]
- Committee on Practice Bulletins—Gynecology ACOG Practice Bulletin No. 191: Tubal Ectopic Pregnancy. Obstet. Gynecol. 2018, 131, e65–e77. [CrossRef] [PubMed]
- Elson, C.J.; Salim, R.; Potdar, N.; Chetty, M.; Ross, J.A.; Kirk, E.J. on behalf of the Royal College of Obstetricians and Gynaecologists. Diagnosis and management of ectopic pregnancy. BJOG 2016, 123, e15–e55. [Google Scholar]
- Hsu, J.; Chen, L.; Gumer, A.R.; Tergas, A.I.; Hou, J.Y.; Burke, W.M.; Ananth, C.V.; Hershman, D.L.; Wright, J.D. Disparities in the management of ectopic pregnancy. Am. J. Obstet. Gynecol. 2017, 217, 49.e1–49.e10. [Google Scholar] [CrossRef] [PubMed]
- Gingold, J.A.; Janmey, I.; Gemmell, L.; Mei, L.; Falcone, T. Effect of Methotrexate on Salpingostomy Completion Rate for Tubal Ectopic Pregnancy: A Retrospective Cohort Study. J. Minim. Invasive Gynecol. 2021, 28, 1334–1342.e3. [Google Scholar] [CrossRef]
- Polen-De, C.; Meganathan, K.; Lang, P.; Hohmann, S.; Jackson, A.; Whiteside, J.L. Nationwide salpingectomy rates for an indication of permanent contraception before and after published practice guidelines. Contraception 2019, 100, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.J.; Barberio, A.; Berens, P.; Chen, H.-Y.; Gants, S.; Swilinski, L.; Acholonu, U.; Chang-Jackson, S.-C. The Trend, Feasibility, and Safety of Salpingectomy as a form of Permanent Sterilization. J. Minim. Invasive Gynecol. 2019, 26, 1363–1368. [Google Scholar] [CrossRef] [PubMed]
- Yerezhepbayeva, M.; Terzic, M.; Aimagambetova, G.; Crape, B. Comparison of two invasive non-surgical treatment options for uterine myomas: Uterine artery embolization and magnetic resonance guided high intensity focused ultrasound—Systematic review. BMC Womens Health 2022, 22, 55. [Google Scholar] [CrossRef]
- Arnreiter, C.; Oppelt, P. A Systematic Review of the Treatment of Uterine Myomas Using Transcervical Ultrasound-Guided Radiofrequency Ablation with the Sonata System. J. Minim. Invasive Gynecol. 2021, 28, 1462–1469. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Chung, Y.-J.; Kim, H.-K.; Hwang, H.; Park, J.Y.; Shin, I.; Kim, C.; Cho, H.-H.; Kim, M.; Jung, C.Y.; et al. Estimated Prevalence and Incidence of Uterine Leiomyoma, and Its Treatment Trend in South Korean Women for 12 years: A National Population-Based Study. J. Women’s Health 2021, 30, 1038–1046. [Google Scholar] [CrossRef]
- Tuesley, K.M.; Protani, M.M.; Webb, P.M.; Dixon-Suen, S.C.; Wilson, L.F.; Stewart, L.M.; Jordan, S.J. Hysterectomy with and without oophorectomy and all-cause and cause-specific mortality. Am. J. Obstet. Gynecol. 2020, 223, 723.e1–723.e16. [Google Scholar] [CrossRef]
| Procedure 1, (N) | Procedure 2, (N) | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| None | 65.3 | 65.51 | 65.53 | 65.61 | 65.62 | 66.4 | 66.51 | 66.62 | 68.3 | 68.4 | 68.61 | ||
| 65.3 | 3101 | 0 | 0 | 0 | 0 | 1 | 25 | 10 | 34 | 25 | 12 | 1 | 3209 |
| 65.51 | 322 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 5 | 2 | 0 | 331 |
| 65.53 | 307 | 0 | 0 | 0 | 0 | 1 | 0 | 6 | 0 | 2 | 0 | 33 | 349 |
| 65.61 | 1410 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 148 | 182 | 10 | 1751 |
| 65.62 | 1912 | 0 | 0 | 0 | 0 | 0 | 19 | 2 | 5 | 14 | 11 | 1 | 1964 |
| 66.4 | 5076 | 34 | 1 | 0 | 0 | 17 | 0 | 0 | 6 | 46 | 34 | 10 | 5224 |
| 66.51 | 3020 | 21 | 3 | 1 | 0 | 5 | 1 | 0 | 2 | 96 | 116 | 4 | 3269 |
| 66.62 | 23,530 | 22 | 0 | 0 | 0 | 5 | 13 | 8 | 0 | 2 | 0 | 0 | 23,580 |
| 68.3 | 15,376 | 23 | 6 | 5 | 176 | 18 | 36 | 75 | 4 | 0 | 16 | 2 | 15,737 |
| 68.4 | 13,978 | 8 | 2 | 0 | 187 | 7 | 30 | 98 | 0 | 9 | 0 | 1 | 14,320 |
| 68.61 | 8828 | 1 | 0 | 18 | 10 | 0 | 20 | 4 | 0 | 0 | 1 | 0 | 8882 |
| Total | 76,860 | 109 | 12 | 24 | 373 | 54 | 146 | 204 | 51 | 347 | 374 | 62 | 78,616 |
| Variables | Median (IQR) or N (%) | Procedures, N (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 65.3 | 65.51 | 65.53 | 65.61 | 65.62 | 66.4 | 66.51 | 66.62 | 68.3 | 68.4 | 68.61 | ||
| Age | 40 (31; 49) | |||||||||||
| Age Group | ||||||||||||
| <18 | 278 (0.4) | 149 (4.5) | 3 (0.9) | 1 (0.3) | 3 (0.1) | 52 (2.6) | 21 (0.4) | 3 (0.1) | 34 (0.1) | 3 (0.0) | 7 (0.1) | 2 (0.0) |
| 18–34 | 27,527 (34.2) | 1545 (46.4) | 61 (17.7) | 15 (4.0) | 186 (8.8) | 827 (40.9) | 3047 (56.7) | 1470 (42.3) | 17,153 (72.6) | 1663 (10.3) | 1437 (9.8) | 123 (1.4) |
| 35–44 | 21,600 (26.9) | 928 (27.9) | 66 (19.2) | 34 (9.1) | 462 (21.8) | 671 (33.2) | 1749 (32.6) | 1437 (41.3) | 6356 (26.9) | 5092 (31.7) | 2874 (19.6) | 1931 (21.6) |
| 45–50 | 14,627 (18.2) | 345 (10.4) | 52 (15.1) | 43 (11.5) | 494 (23.3) | 233 (11.5) | 396 (7.4) | 427 (12.3) | 83 (0.4) | 5618 (34.9) | 3759 (25.6) | 3177 (35.5) |
| 51+ | 16,369 (20.4) | 360 (10.8) | 162 (47.1) | 280 (75.1) | 979 (46.1) | 237 (11.7) | 159 (3.0) | 141 (4.1) | 6 (0.0) | 3712 (23.1) | 6621 (45.1) | 3712 (41.5) |
| Ethnicity | ||||||||||||
| Kazakh | 48,974 (61.2) | 2162 (65.3) | 200 (58.3) | 157 (42.3) | 1033 (48.8) | 1254 (62.5) | 3425 (64.1) | 2242 (64.8) | 15,950 (68.0) | 9750 (60.9) | 8216 (56.1) | 4585 (51.4) |
| Other | 12,309 (15.4) | 504 (15.2) | 61 (17.8) | 72 (19.4) | 315 (14.9) | 290 (14.5) | 775 (14.5) | 563 (16.3) | 3082 (13.1) | 2524 (15.8) | 2393 (16.3) | 1730 (19.4) |
| Russian | 18,709 (23.4) | 644 (19.5) | 82 (23.9) | 142 (38.3) | 770 (36.4) | 461 (23.0) | 1142 (21.4) | 653 (18.9) | 4441 (18.9) | 3739 (23.4) | 4037 (27.6) | 2598 (29.2) |
| Residence | ||||||||||||
| Rural | 27,942 (34.8) | 1560 (46.9) | 84 (24.4) | 71 (19.0) | 689 (32.4) | 799 (39.6) | 1900 (35.4) | 1539 (44.3) | 7939 (33.6) | 6468 (40.2) | 4402 (30.0) | 2491 (27.9) |
| Urban | 52,459 (65.3) | 1767 (53.1) | 260 (75.6) | 302 (81.0) | 1435 (67.6) | 1221 (60.5) | 3472 (64.6) | 1939 (55.8) | 15,693 (66.4) | 9620 (59.8) | 10,296 (70.1) | 6454 (72.2) |
| Region | ||||||||||||
| Akmola region | 2458 (3.1) | 113 (3.4) | 23 (6.7) | 3 (0.8) | 95 (4.5) | 69 (3.4) | 209 (3.9) | 128 (3.7) | 985 (4.2) | 512 (3.2) | 295 (2.0) | 26 (0.3) |
| Aktobe region | 3039 (3.8) | 206 (6.2) | 10 (2.9) | 10 (2.7) | 25 (1.2) | 56 (2.8) | 175 (3.3) | 18 (0.5) | 1197 (5.1) | 922 (5.7) | 331 (2.3) | 89 (1.0) |
| Almaty city | 11,048 (13.7) | 180 (5.4) | 16 (4.7) | 16 (4.3) | 67 (3.2) | 91 (4.5) | 468 (8.7) | 1773 (51.0) | 3049 (12.9) | 595 (3.7) | 2562 (17.4) | 2231 (24.9) |
| Almaty region | 8360 (10.4) | 494 (14.9) | 17 (4.9) | 3 (0.8) | 42 (2.0) | 446 (22.1) | 525 (9.8) | 60 (1.7) | 3726 (15.8) | 2053 (12.8) | 878 (6.0) | 116 (1.3) |
| Astana (capital city) | 5287 (6.6) | 96 (2.9) | 40 (11.6) | 25 (6.7) | 84 (4.0) | 62 (3.1) | 181 (3.4) | 176 (5.1) | 1319 (5.6) | 776 (4.8) | 848 (5.8) | 1680 (18.8) |
| Atyrau region | 1505 (1.9) | 36 (1.1) | 2 (0.6) | 5 (1.3) | 22 (1.0) | 20 (1.0) | 78 (1.5) | 13 (0.4) | 609 (2.6) | 261 (1.6) | 193 (1.3) | 266 (3.0) |
| East Kazakhstan region | 10,534 (13.1) | 375 (11.3) | 53 (15.4) | 31 (8.3) | 588 (27.7) | 196 (9.7) | 548 (10.2) | 625 (18.0) | 3277 (13.9) | 2010 (12.5) | 2184 (14.9) | 647 (7.2) |
| Karaganda region | 7425 (9.2) | 309 (9.3) | 18 (5.2) | 223 (59.8) | 400 (18.8) | 229 (11.3) | 593 (11.0) | 205 (5.9) | 1938 (8.2) | 1774 (11.0) | 1319 (9.0) | 417 (4.7) |
| Kostanay region | 4650 (5.8) | 141 (4.2) | 6 (1.7) | 10 (2.7) | 291 (13.7) | 151 (7.5) | 374 (7.0) | 75 (2.2) | 1305 (5.5) | 1424 (8.9) | 710 (4.8) | 163 (1.8) |
| Kyzylorda region | 2547 (3.2) | 151 (4.5) | 10 (2.9) | 3 (0.8) | 22 (1.0) | 65 (3.2) | 156 (2.9) | 32 (0.9) | 893 (3.8) | 796 (5.0) | 312 (2.1) | 107 (1.2) |
| Mangystau region | 669 (0.8) | 16 (0.5) | 0 (0.0) | 3 (0.8) | 1 (0.1) | 10 (0.5) | 29 (0.5) | 7 (0.2) | 94 (0.4) | 116 (0.7) | 54 (0.4) | 339 (3.8) |
| North Kazakhstan region | 2546 (3.2) | 121 (3.6) | 15 (4.4) | 14 (3.8) | 141 (6.6) | 51 (2.5) | 183 (3.4) | 83 (2.4) | 236 (1.0) | 627 (3.9) | 578 (3.9) | 497 (5.6) |
| Pavlodar region | 3885 (4.8) | 127 (3.8) | 16 (4.7) | 8 (2.1) | 59 (2.8) | 108 (5.4) | 197 (3.7) | 71 (2.0) | 635 (2.7) | 1041 (6.5) | 565 (3.8) | 1058 (11.8) |
| Shymkent city | 4207 (5.2) | 126 (3.8) | 78 (22.7) | 1 (0.3) | 21 (1.0) | 22 (1.1) | 615 (11.5) | 12 (0.4) | 1156 (4.9) | 354 (2.2) | 1003 (6.8) | 819 (9.2) |
| Turkestan region | 5247 (6.5) | 491 (14.8) | 17 (4.9) | 4 (1.1) | 21 (1.0) | 243 (12.0) | 407 (7.6) | 32 (0.9) | 1697 (7.2) | 1383 (8.6) | 805 (5.5) | 147 (1.6) |
| West Kazakhstan region | 2491 (3.1) | 36 (1.1) | 7 (2.0) | 5 (1.3) | 124 (5.8) | 24 (1.2) | 318 (5.9) | 100 (2.9) | 496 (2.1) | 291 (1.8) | 882 (6.0) | 208 (2.3) |
| Zhambyl region | 4503 (5.6) | 309 (9.3) | 16 (4.7) | 9 (2.4) | 121 (5.7) | 177 (8.8) | 316 (5.9) | 68 (2.0) | 1020 (4.3) | 1153 (7.2) | 1179 (8.0) | 135 (1.5) |
| Admission | ||||||||||||
| Planned | 37,066 (46.1) | 1190 (35.8) | 248 (72.1) | 340 (91.2) | 1179 (55.5) | 627 (31.0) | 1041 (19.4) | 2307 (66.3) | 259 (1.1) | 10,825 (67.3) | 11,094 (75.5) | 7956 (88.9) |
| Emergency | 43,335 (53.9) | 2137 (64.2) | 96 (27.9) | 33 (8.9) | 945 (44.5) | 1393 (69.0) | 4331 (80.6) | 1171 (33.7) | 23,373 (98.9) | 5263 (32.7) | 3604 (24.5) | 989 (11.1) |
| Outcome of stay | ||||||||||||
| Discharge | 79,603 (99.0) | 3299 (99.2) | 342 (99.4) | 372 (99.7) | 2090 (98.4) | 1995 (98.8) | 5325 (99.1) | 3414 (98.2) | 23,511 (99.5) | 15,836 (98.4) | 14,484 (98.5) | 8935 (99.9) |
| Transfer | 521 (0.7) | 12 (0.4) | 0 (0.0) | 1 (0.3) | 16 (0.8) | 15 (0.7) | 27 (0.5) | 52 (1.5) | 58 (0.3) | 204 (1.3) | 130 (0.9) | 6 (0.1) |
| Voluntary discharge | 104 (0.1) | 5 (0.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (0.3) | 12 (0.2) | 4 (0.1) | 63 (0.3) | 6 (0.0) | 9 (0.1) | 0 (0.0) |
| Death | 172 (0.2) | 11 (0.3) | 2 (0.6) | 0 (0.0) | 18 (0.9) | 5 (0.3) | 8 (0.2) | 8 (0.2) | 0 (0.0) | 41 (0.3) | 75 (0.5) | 4 (0.0) |
| Outcome of treatment | ||||||||||||
| Without changes | 343 (0.4) | 6 (0.2) | 12 (3.5) | 0 (0.0) | 4 (0.2) | 4 (0.2) | 6 (0.1) | 2 (0.1) | 16 (0.1) | 102 (0.6) | 191 (1.3) | 0 (0.0) |
| Recovery | 50,578 (62.9) | 2140 (64.3) | 156 (45.4) | 301 (80.7) | 1531 (72.1) | 1431 (70.8) | 3901 (72.6) | 1378 (39.6) | 14,668 (62.1) | 11,694 (72.7) | 7427 (50.5) | 5951 (66.5) |
| Improvement | 29,271 (36.4) | 1166 (35.1) | 173 (50.3) | 72 (19.3) | 571 (26.9) | 580 (28.7) | 1455 (27.1) | 2088 (60.0) | 8947 (37.9) | 4242 (26.4) | 6988 (47.6) | 2,989 (33.4) |
| Deterioration | 36 (0.0) | 4 (0.1) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (0.0) | 2 (0.1) | 1 (0.0) | 9 (0.1) | 16 (0.1) | 1 (0.0) |
| Total, N (%) | 80,401 (100%) | 3327 (4.14%) | 344 (0.43%) | 373 (0.46%) | 2124 (2.64%) | 2020 (2.51%) | 5372 (6.68%) | 3478 (4.33%) | 23,632 (29.39%) | 16,088 (20.01%) | 14,698 (18.28%) | 8945 (11.13%) |
| Variables | Outcomes | ||
|---|---|---|---|
| Alive, N (%) | Deceased, N (%) | Total, N | |
| Age Group | |||
| <18 | 277 (99.64%) | 1 (0.36%) | 278 |
| 18–34 | 27,446 (99.71%) | 81 (0.29%) | 27,527 |
| 35–44 | 21,532 (99.69%) | 68 (0.31%) | 21,600 |
| 45–50 | 14,605 (99.85%) | 22 (0.15%) | 14,627 |
| >51 | 16,208 (99.02%) | 161 (0.98%) | 16,369 |
| Social status | |||
| Disabled | 528 (98.88%) | 6 (1.12%) | 534 |
| Employed | 33,309 (99.83%) | 58 (0.17%) | 33,367 |
| Retiree | 5682 (98.3%) | 98 (1.7%) | 5780 |
| Unemployed | 32,989 (99.64%) | 120 (0.36%) | 33,109 |
| Other | 7560 (99.33%) | 51 (0.67%) | 7611 |
| Region | |||
| Akmola region | 2452 (99.76%) | 6 (0.24%) | 2458 |
| Aktobe region | 3035 (99.87%) | 4 (0.13%) | 3039 |
| Almaty city | 11,007 (99.63%) | 41 (0.37%) | 11,048 |
| Almaty region | 8322 (99.55%) | 38 (0.45%) | 8360 |
| Astana (capital city) | 5254 (99.38%) | 33 (0.62%) | 5287 |
| Atyrau region | 1503 (99.87%) | 2 (0.13%) | 1505 |
| East Kazakhstan region | 10,477 (99.46%) | 57 (0.54%) | 10,534 |
| Karaganda region | 7394 (99.58%) | 31 (0.42%) | 7425 |
| Kostanay region | 4636 (99.7%) | 14 (0.3%) | 4650 |
| Kyzylorda region | 2536 (99.57%) | 11 (0.43%) | 2547 |
| Mangystau region | 662 (98.95%) | 7 (1.05%) | 669 |
| North Kazakhstan region | 2530 (99.37%) | 16 (0.63%) | 2546 |
| Pavlodar region | 3866 (99.51%) | 19 (0.49%) | 3885 |
| Shymkent city | 4196 (99.74%) | 11 (0.26%) | 4207 |
| Turkestan region | 5226 (99.6%) | 21 (0.4%) | 5247 |
| West Kazakhstan region | 2483 (99.68%) | 8 (0.32%) | 2491 |
| Zhambyl region | 4489 (99.69%) | 14 (0.31%) | 4503 |
| Surgery (ICD-9 code) | |||
| Unilateral oophorectomy (65.3) | 3308 (99.43%) | 19 (0.57%) | 3327 |
| Other removal of both ovaries at the same operative episode (65.51) | 334 (97.09%) | 10 (2.91%) | 344 |
| Laparoscopic removal of both ovaries at the same operative episode (65.53) | 373 (100%) | 0 (0%) | 373 |
| Other removal of both ovaries and tubes at the same operative episode (65.61) | 2095 (98.63%) | 29 (1.37%) | 2124 |
| Other removal of remaining ovary and tube (65.62) | 2011 (99.55%) | 9 (0.45%) | 2020 |
| Total unilateral salpingectomy (66.4) | 5359 (99.76%) | 13 (0.24%) | 5372 |
| Removal of both tubes (66.51) | 3467 (99.68%) | 11 (0.32%) | 3478 |
| Salpingectomy with removal of tubal pregnancy (66.62) | 23,630 (99.99%) | 2 (0.01%) | 23,632 |
| Subtotal abdominal hysterectomy (68.3) | 16,007 (99.5%) | 81 (0.5%) | 16,088 |
| Total abdominal hysterectomy (68.4) | 14,548 (98.98%) | 150 (1.02%) | 14,698 |
| Laparoscopic radical abdominal hysterectomy (68.61) | 8936 (99.9%) | 9 (0.1%) | 8945 |
| Total | 80,068 (99.59%) | 333 (0.41%) | 80,401 |
| Variables | Crude HR | Crude p-Value | 95% CI | Adjusted HR | Adjusted p-Value | 95% CI |
|---|---|---|---|---|---|---|
| Age group | ||||||
| <18 | 1.45 | 0.71 | (0.20–10.45) | 0.65 | 0.68 | (0.09–4.79) |
| 18–34 | Ref. | Ref. | ||||
| 35–44 | 1.05 | 0.79 | (0.74–1.49) | 0.71 | 0.07 | (0.49–1.02) |
| 45–50 | 0.55 | 0.02 | (0.34–0.91) | 0.31 | 0.00 | (0.18–0.52) |
| 51+ | 3.84 | 0.00 | (2.89–5.11) | 2.05 | 0.00 | (1.44–2.92) |
| Ethnicity | ||||||
| Kazakh | Ref. | Ref. | ||||
| Other | 1.02 | 0.92 | (0.73–1.42) | 0.94 | 0.72 | (0.67–1.32) |
| Russian | 1.39 | 0.01 | (1.07–1.79) | 1.08 | 0.60 | (0.82–1.43) |
| Residence | ||||||
| Rural | 0.86 | 0.21 | (0.67–1.09) | 0.89 | 0.40 | (0.68–1.16) |
| Urban | Ref. | Ref. | ||||
| Region | ||||||
| Akmola region | 0.26 | 0.01 | (0.09–0.74) | 0.21 | 0.00 | (0.08–0.61) |
| Aktobe region | 0.21 | 0.00 | (0.07–0.59) | 0.19 | 0.00 | (0.07–0.54) |
| Almaty city | 0.57 | 0.02 | (0.36–0.90) | 0.52 | 0.01 | (0.33–0.83) |
| Almaty region | 0.61 | 0.05 | (0.38–1.00) | 0.66 | 0.11 | (0.39–1.10) |
| Astana (capital city) | Ref. | Ref. | ||||
| Atyrau region | 0.11 | 0.03 | (0.01–0.78) | 0.13 | 0.04 | (0.02–0.93) |
| East Kazakhstan region | 0.81 | 0.33 | (0.52–1.25) | 0.54 | 0.01 | (0.34–0.85) |
| Karaganda region | 0.58 | 0.04 | (0.35–0.97) | 0.39 | 0.00 | (0.23–0.66) |
| Kostanay region | 0.45 | 0.01 | (0.24–0.85) | 0.33 | 0.00 | (0.17–0.63) |
| Kyzylorda region | 0.63 | 0.20 | (0.31–1.28) | 0.66 | 0.25 | (0.32–1.35) |
| Mangystau region | 1.45 | 0.41 | (0.61–3.45) | 1.52 | 0.35 | (0.63–3.67) |
| North Kazakhstan region | 0.95 | 0.86 | (0.51–1.74) | 0.58 | 0.09 | (0.31–1.09) |
| Pavlodar region | 0.70 | 0.23 | (0.39–1.26) | 0.60 | 0.09 | (0.33–1.09) |
| Shymkent city | 0.38 | 0.01 | (0.19–0.77) | 0.33 | 0.00 | (0.16–0.66) |
| Turkestan region | 0.52 | 0.03 | (0.29–0.93) | 0.40 | 0.00 | (0.22–0.74) |
| West Kazakhstan region | 0.32 | 0.02 | (0.13–0.82) | 0.22 | 0.00 | (0.09–0.58) |
| Zhambyl region | 0.50 | 0.03 | (0.27–0.93) | 0.38 | 0.00 | (0.20–0.71) |
| Admission | ||||||
| Planned/elective | 0.92 | 0.45 | (0.73–1.15) | 0.29 | 0.00 | (0.22–0.37) |
| Urgent | Ref. | Ref. | ||||
| Surgery (ICD-9) | ||||||
| Unilateral oophorectomy (65.3) | 1.29 | 0.34 | (0.77–2.16) | 0.91 | 0.73 | (0.53–1.56) |
| Other removal of both ovaries at the same operative episode (65.51) | 3.33 | 0.00 | (1.71–6.46) | 2.69 | 0.00 | (1.36–5.29) |
| Other removal of both ovaries and tubes at the same operative episode (65.61) | 3.05 | 0.00 | (1.95–4.76) | 2.12 | 0.00 | (1.33–3.37) |
| Other removal of remaining ovary and tube (65.62) | 1.06 | 0.87 | (0.53–2.13) | 0.68 | 0.28 | (0.34–1.38) |
| Total unilateral salpingectomy (66.4) | 0.53 | 0.04 | (0.29–0.98) | 0.35 | 0.00 | (0.18–0.66) |
| Removal of both tubes (66.51) | 0.62 | 0.17 | (0.31–1.23) | 0.62 | 0.19 | (0.30–1.27) |
| Salpingectomy with removal of tubal pregnancy (66.62) | 0.02 | 0.00 | (0.00–0.08) | 0.01 | 0.00 | (0.00–0.04) |
| Subtotal abdominal hysterectomy (68.3) | Ref. | Ref. | ||||
| Total abdominal hysterectomy (68.4) | 2.19 | 0.00 | (1.64–2.94) | 1.87 | 0.00 | (1.38–2.54) |
| Laparoscopic radical abdominal hysterectomy (68.61) | 0.24 | 0.00 | (0.12–0.48) | 0.21 | 0.00 | (0.10–0.43) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakko, Y.; Aimagambetova, G.; Terzic, M.; Ukybassova, T.; Bapayeva, G.; Gusmanov, A.; Zhakhina, G.; Zhantuyakova, A.; Gaipov, A. The Prevalence, Indications, Outcomes of the Most Common Major Gynecological Surgeries in Kazakhstan and Recommendations for Potential Improvements into Public Health and Clinical Practice: Analysis of the National Electronic Healthcare System (2014–2019). Int. J. Environ. Res. Public Health 2022, 19, 14679. https://doi.org/10.3390/ijerph192214679
Sakko Y, Aimagambetova G, Terzic M, Ukybassova T, Bapayeva G, Gusmanov A, Zhakhina G, Zhantuyakova A, Gaipov A. The Prevalence, Indications, Outcomes of the Most Common Major Gynecological Surgeries in Kazakhstan and Recommendations for Potential Improvements into Public Health and Clinical Practice: Analysis of the National Electronic Healthcare System (2014–2019). International Journal of Environmental Research and Public Health. 2022; 19(22):14679. https://doi.org/10.3390/ijerph192214679
Chicago/Turabian StyleSakko, Yesbolat, Gulzhanat Aimagambetova, Milan Terzic, Talshyn Ukybassova, Gauri Bapayeva, Arnur Gusmanov, Gulnur Zhakhina, Almira Zhantuyakova, and Abduzhappar Gaipov. 2022. "The Prevalence, Indications, Outcomes of the Most Common Major Gynecological Surgeries in Kazakhstan and Recommendations for Potential Improvements into Public Health and Clinical Practice: Analysis of the National Electronic Healthcare System (2014–2019)" International Journal of Environmental Research and Public Health 19, no. 22: 14679. https://doi.org/10.3390/ijerph192214679
APA StyleSakko, Y., Aimagambetova, G., Terzic, M., Ukybassova, T., Bapayeva, G., Gusmanov, A., Zhakhina, G., Zhantuyakova, A., & Gaipov, A. (2022). The Prevalence, Indications, Outcomes of the Most Common Major Gynecological Surgeries in Kazakhstan and Recommendations for Potential Improvements into Public Health and Clinical Practice: Analysis of the National Electronic Healthcare System (2014–2019). International Journal of Environmental Research and Public Health, 19(22), 14679. https://doi.org/10.3390/ijerph192214679








