Relationship between Pain, Fear of Falling and Physical Performance in Older People Residents in Long-Stay Institutions: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Eligibility Criteria
2.4. Procedures
2.4.1. Sociodemographic Variables
2.4.2. Body Mass Index (BMI)
2.4.3. Use of Psychotropic and/or Hypnotic Drugs
2.4.4. Perceived Health
2.4.5. Depression
2.4.6. Pain
2.4.7. Fear of Falling
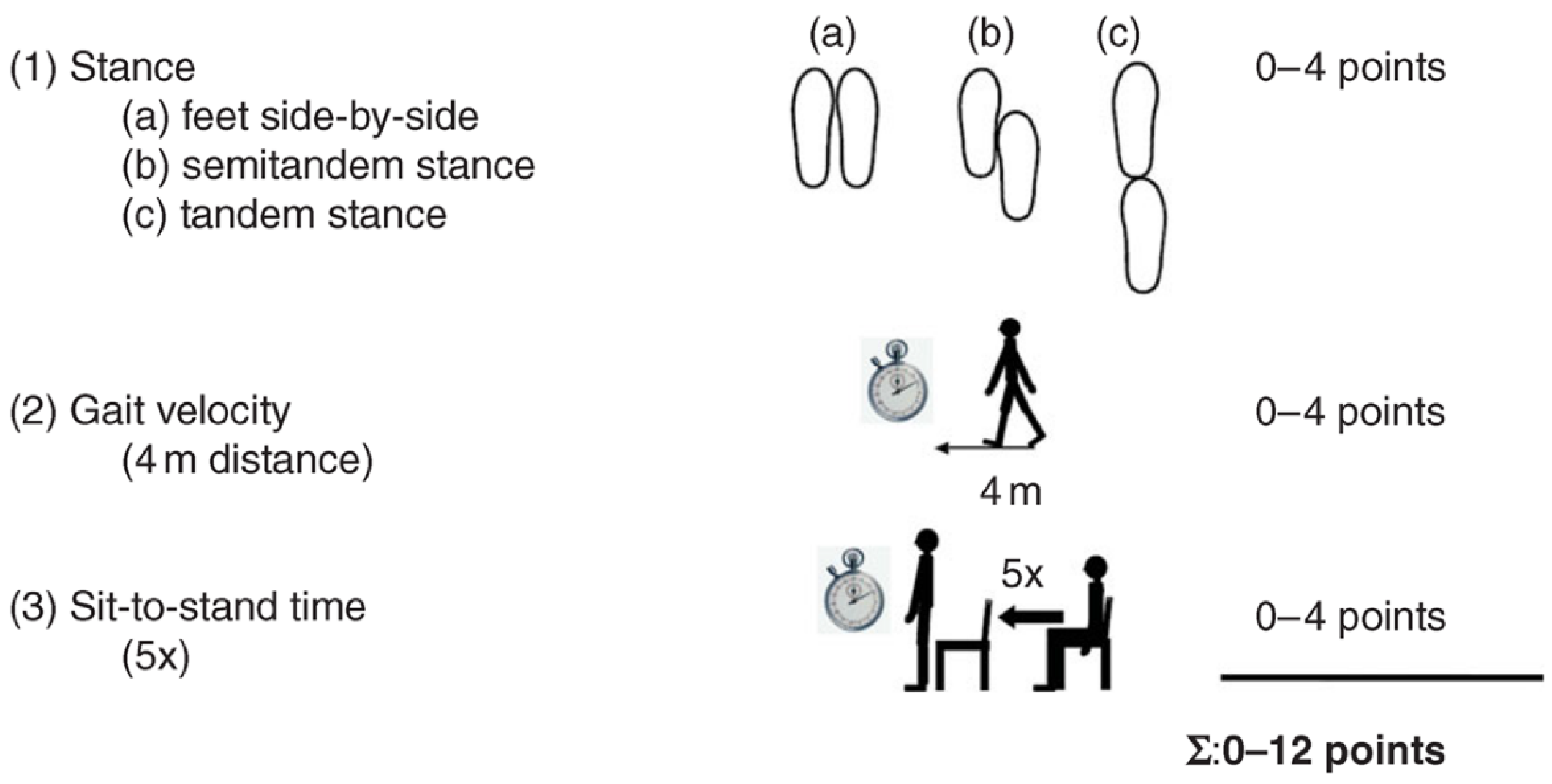
2.4.8. Short Physical Performance Battery
2.5. Ethical Aspects
2.6. Data Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Veras, R.P.; Oliveira, M. Envelhecer no Brasil: A construção de um modelo de cuidado. Ciência Saúde Coletiva 2018, 23, 1929–1936. [Google Scholar] [CrossRef]
- Cavalcanti, P.C.S.; Oliveira, A.V.; Sousa, M.F. Quais são os desafios para a qualificação da Atenção Básica na visão dos gestores municipais? Saúde Em Debate 2015, 39, 323–336. [Google Scholar] [CrossRef]
- Alves-Silva, J.D.; Scorsolini-Comin, F.; Santos, M.A. Idosos em instituições de longa permanência: Desenvolvimento, condições de vida e saúde. Psicol. Reflexão E Crítica 2013, 26, 820–830. [Google Scholar] [CrossRef]
- Bell, B.B.; Andrade, V.S.; Paulin, G.S.T.; Patrizzi, L.J. Uso de restrições físicas em instituições de longa permanência para idosos: Percepção de profissionais de saúde e cuidadores de idosos. Estud. Interdiscip. Sobre O Envelhec. 2016, 21, 9. [Google Scholar] [CrossRef]
- Manso, M.E.G.; Góes, L.G.; Concone, M.H.V.B. Idosos e doenças crônico-degenerativas: Por que eu, e por que agora? Kairós-Gerontol. 2019, 22, 379–393. [Google Scholar] [CrossRef]
- Bonafé, M.; Jorge, M.S.G.; Portella, M.R.; Doring, M.; Scortegagna, S.A.; Wibelinger, L.M. Factors related to chronic pain in institutionalized elderly. Braz. J. Pain 2020, 3, 314–317. [Google Scholar] [CrossRef]
- Barbosa, M.H.; Silva, L.C.; Andrade, É.V.; Luiz, R.B.; Bolina, A.F.; Mattia, A.L.D. Avaliação da dor crônica em idosos institucionalizados. Rev. Min. Enfer. 2012, 16, 63–68. Available online: https://www.reme.org.br/artigo/detalhes/501 (accessed on 15 August 2022).
- Dellaroza, M.S.G.; Pimenta, C.A.M.; Duarte, Y.A.; Lebrão, M.L. Dor crônica em idosos residentes em São Paulo, Brasil: Prevalência, características e associação com capacidade funcional e mobilidade (Estudo SABE). Cad. Saúde Pública 2013, 29, 325–334. [Google Scholar] [CrossRef]
- Pagotto, V.; Silva, V.A.P.; Pereira, L.V.; Santos, D.P.M.A. Comparação da funcionalidade de idosos residentes em duas modalidades institucionais. Rev. Eletr. Enferm. 2016, 18, 1–10. [Google Scholar] [CrossRef][Green Version]
- Antes, D.L.; Schneider, I.J.C.; Benedetti, T.R.B.; d’Orsi, E. Medo de queda recorrente e fatores associados em idosos de Florianópolis, Santa Catarina, Brasil. Cad. Saúde Pública 2013, 29, 758–768. [Google Scholar] [CrossRef]
- Tomita, Y.; Arima, K.; Kanagae, M.; Okabe, T.; Mizukami, S.; Nishimura, T.; Abe, Y.; Goto, H.; Horiguchi, I.; Aoyagi, K. Association of Physical Performance and Pain with Fear of Falling Among Community-Dwelling Japanese Women Aged 65 Years and Older. Medicine 2015, 94, e1449. [Google Scholar] [CrossRef]
- Magnani, C.A.L.P.; Moraes, J.F.; Zanca, G.G. Medo de cair em idosos com e sem dor crônica musculoesquelética. Colloq. Health Educ. 2021, 1, e011. [Google Scholar] [CrossRef]
- Malta, M.; Cardoso, L.O.; Bastos, F.I.; Magnanini, M.M.; Silva, C.M. STROBE initiative: Guidelines on reporting observational studies. Rev. Saúde Publica 2010, 44, 559–565. [Google Scholar] [CrossRef]
- Silva, S.L.A.; Neri, A.L.; Ferrioli, E.; Lourenço, R.A.; Dias, R.C. Fenótipo de fragilidade: Influência de cada item na determinação da fragilidade em idosos comunitários—Rede Fibra. Ciência Saúde Coletiva 2016, 21, 3483–3492. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; Mchugh, P.R. Mini-mental state. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Bertolucci, P.H.F.; Brucki, S.M.D.; Campacci, S.R.; Juliano, Y. O Mini-Exame do Estado Mental em uma população geral: Impacto da escolaridade. Arq. Neuro Psiquiatr. 1994, 52, 1–7. [Google Scholar] [CrossRef]
- Nóbrega, P.V.N.; Maciel, Á.C.C.; Almeida, H.C.M.; Guerra, R.O.; Araújo, J.F. Sleep and frailty syndrome in elderly residents of long-stay institutions: A cross-sectional study. Geriatr. Gerontol. Int. 2013, 14, 605–612. [Google Scholar] [CrossRef]
- Sheikh, J.I.; Yesavage, J.A. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter versio. Clin. Gerontol. J. Ment. Health Aging 1986, 5, 165–173. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiat. Res. 1983, 17, 37–49. [Google Scholar] [CrossRef]
- Feher, E.P.; Larrabee, G.J.; Crook, T.H. Factors attenuating the validity of the Geriatric Depression Scale in a dementia populatio. J. Am. Geriatr. Soc. 1992, 40, 906–909. [Google Scholar] [CrossRef]
- Stoppe, A. Aspectos Clínicos da depressão em idosos. Rev. Psiquiatr. Clín. 1994, 21, 121–128. [Google Scholar]
- Guimarães, L.A.; Brito, T.A.; Pithon, K.R.; Jesus, C.S.; Souto, C.S.; Souza, S.J.N.; Santos, T.S. Sintomas depressivos e fatores associados em idosos residentes em instituição de longa permanência. Ciência Saúde Coletiva 2019, 24, 3275–3282. [Google Scholar] [CrossRef]
- Motta, T.S.D.A.; Gambaro, R.C.; Santos, F.C. Pain measurement in the elderly: Evaluation of psychometric properties of the Geriatric Pain Measure—Portuguese version. Rev. Dor. 2015, 16, 560. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Powell, L. Fear of falling and low self-efficacy: A case of dependence in elderly persons. J. Gerontol. 1993, 48, 35–38. [Google Scholar] [CrossRef]
- Delbaere, K.; Close, J.T.; Mikolaizak, A.S.; Sachdev, P.S.; Brodaty, H.; Lord, S.R. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age Ageing 2010, 2, 210–216. [Google Scholar] [CrossRef]
- Borges, C.L.; Silva, M.J.; Clares, J.W.B.; Nogueira, J.M.; Freitas, M.C. Características sociodemográficas e clínicas de idosos institucionalizados: Contribuições para o cuidado de enfermagem. Rev. Enferm. UERJ 2015, 23, 381–387. [Google Scholar] [CrossRef]
- Marchon, R.M.; Cordeiro, R.C.; Nakano, M.M. Capacidade Funcional: Estudo prospectivo em idosos residentes em uma instituição de longa permanência. Rev. Bras. Geriatr. E Gerontol. 2010, 13, 203–214. [Google Scholar] [CrossRef]
- Josino, J.B.; Costa, R.B.; Vasconcelos, T.B.; Domiciano, B.R.; Brasileiro, I.C. Análise do estado de funcionalidade de idosos residentes em unidades de longa permanência. Rev. Bras. Em Promoção Da Saúde 2015, 28, 351–360. [Google Scholar] [CrossRef][Green Version]
- Reis, L.A.; Mascarenhas, C.H.M.; Torres, G.V. Evaluation of functional capacity on institutionalized elderly in the City of Jequié/BA. Fiep Bull. 2008, 78, 89–92. [Google Scholar]
- Reis, L.A.; Torres, G.V. Influência da dor crônica na Influência da dor crônica na capacidade funcional de idosos institucionalizados. Rev. Bras. Enferm. 2011, 64, 274–280. [Google Scholar] [CrossRef]
- Miranda, V.S.; Decarvalho, V.B.; Machado, L.A.; Dias, J.M. Prevalence of chronic musculoskeletal disorders in elderly Brazilians: A systematic review of the literature. BMC Musculoskelet. Disord. 2012, 13, 82. [Google Scholar] [CrossRef]
- Bernfort, L.; Gerdle, B.; Rahmqvist, M.; Husberg, M.; Levin, L.A. Severity of chronic pain in an elderly population in Sweden—Impact on costs and quality of life. Pain 2015, 156, 521–527. [Google Scholar] [CrossRef]
- Santos, F.C.; Moraes, N.S.; Pastore, A.; Cendoroglo, M.S. Dor crônica em idosos longevos: Prevalência, características, mensurações e correlação com nível sérico de vitamina D. Rev. Dor. 2015, 16, 171–175. [Google Scholar] [CrossRef]
- Pereira, L.S.; Sherrington, C.; Ferreira, M.L.; Tiedemann, A.; Ferreira, P.H.; Blyth, F.M.; Close, J.C.; Taylor, M.; Lord, S.R. Self-reported chronic pain is associated with physical performance in older people leaving aged care rehabilitatio. Clin. Interv. Aging 2015, 9, 259–265. [Google Scholar] [CrossRef]
- Lach, H.W.; Parsons, J.L. Impact of fear of falling in long term care: An integrative review. J. Am. Med. Dir. Assoc. 2013, 14, 573–577. [Google Scholar] [CrossRef]
- Patel, K.V.; Dansie, E.J.; Turk, D.C. Impact of chronic musculoskeletal pain on objectively measured daily physical activity: A review of current findings. Pain Manag. 2013, 3, 467–474. [Google Scholar] [CrossRef]
- Hubscher, M.; Vogt, L.; Schmidt, K.; Fink, M.; Banzer, W. Perceived pain, fear of falling and physical function in women with osteoporosis. Gait Posture 2010, 32, 383–385. [Google Scholar] [CrossRef]
- Onder, G.; Cesari, M.; Russo, A.; Zamboni, V.; Bernabei, R.; Landi, F. Association between daily pain and physical function among old–old adults living in the community: Results from the ilSIRENTE study. Pain 2006, 121, 53–59. [Google Scholar] [CrossRef]

| Variables | Mean or n | Standard Deviation (SD) or % |
|---|---|---|
| Age (years) | 78.8 | ±7.62 |
| Institutionalization Time (years) | 3.80 | ±3.49 |
| Cognitive Function (MMSE) | 21.5 | ±3.5 |
| GDS-15 Score | 5.74 | ±3.24 |
| BMI (kg/m2) | 24.88 | ±5.13 |
| Gender | ||
| Male Female | 46 87 | 34.6% 65.4% |
| Marital status * | ||
| Married Single Divorced Widower | 12 57 25 38 | 9.1% 43.2% 18.9% 28.8% |
| Education ** | ||
| Illiterate Low education level High schooling | 31 77 22 | 23.8% 59.2% 16.9% |
| Nutritional Status ** | ||
| Malnutrition (<22 kg/m2) Eutrophy (22–27 kg/m2) Obesity (27 kg/m2) | 34 59 37 | 26.2% 45.4% 28.5% |
| Psychotropic Drug Use * | ||
| Yes No | 48 84 | 36.4% 83.6% |
| Use of Hypnotic Drugs * | ||
| Yes No | 40 92 | 30.3% 69.7% |
| Depression (GDS-15) | ||
| Yes (>5) No (≤5) | 66 67 | 49.6% 50.4% |
| Perceived Health | ||
| Satisfactory Unsatisfactory | 97 36 | 72.9% 27.1% |
| Variables | n or Mean | % or SD |
|---|---|---|
| Pain in General £ | ||
| Yea No | 73 54 | 57.5% 42.5% |
| Acute Pain £ | ||
| Yea No | 17 110 | 13.4% 86.6% |
| Chronic Pain £ | ||
| Yea No | 61 66 | 48.0% 52.0% |
| Balance Score | 2.73 (±1.44) | - |
| Sit and Stand Test-SPPB (s) | 20.27 (±6.41) | - |
| Gait Speed Test-SPPB (m/s) | 0.73 (±0.35) | |
| SPPB Total Score | 6.43 (±2.96) | - |
| Physical Performance-SPPB (%) ** | ||
| Disability or very poor performance (0–3) Poor performance (4–6) Moderate performance (7–9) Good performance (10–12) | - - - - | 25 (19.2%) 37 (28.5%) 47 (36.2%) 21 (16.2%) |
| N = 108 | ||
| GPM * | 28.81 | ±30.67 |
| Total Fear of Falls FES-I score * | 34.46 (±1.18) | |
| Older people with low concern * | 16.92 (±2.24) | 13 (12.0%) |
| Older people with moderate concern * | 22.65 (±1.98) | 20 (18.6%) |
| Older people with high concern * | 40.65 (±7.93) | 75 (69.4%) |
| Balance Score (0–4) a | Walking Speed (m/s) a | Test Stand Up from Chair(s) a | Total SPPB Score (0–12) a | FES-I € | |
|---|---|---|---|---|---|
| Pain | |||||
| Yes | 2.62 (±1.50) | 0.63 (±0.29) | 21.75 (±5.86) | 5.89 (±2.74) | 38.29 (±10.94) |
| No | 2.85 (±1.36) | 0.84 (±0.38) | 18.58 (±6.51) | 7.09 (±3.15) | 29.50 (±10.59) |
| p-value | 0.36 | 0.002 * | 0.02 * | 0.02 * | <0.001 ** |
| Acute Pain | |||||
| Yes | 2.29 (±1.57) | 0.53 (±0.19) | 23.92 (±3.96) | 4.53 (±2.37) | 37.31 (±11.83) |
| No | 2.78 (±1.42) | 0.75 (±0.35) | 19.78 (±6.46) | 6.69 (±2.95) | 34.01 (±11.71) |
| p-value | 0.19 | 0.04 * | 0.01 * | 0.005 * | 0.26 |
| Chronic Pain | |||||
| Yes | 2.65 (±1.53) | 0.65 (±0.31) | 21.48 (±6.28) | 6.06 (±2.80) | 38.61 (±11.36) |
| No | 2.77 (±1.38) | 0.79 (±0.37) | 19.31 (±6.29) | 6.71 (3.11) | 31.36 (±10.83) |
| p-value | 0.66 | 0.02 * | 0.11 | 0.22 | 0.001 ** |
| GPM | −0.110 | −0.324 | 0.308 | −0.241 | 0.31 b |
| p-value | 0.22 | 0.001 * | 0.004 * | 0.007 * | 0.001 ***b |
| Variables | ß | 95% CI | p Value |
|---|---|---|---|
| Balance a | |||
| Age | −0.045 | −1.192: −0.78 | 0.01 |
| Use of Hypnotics | −0.64 | −1.19: −0.08 | 0.03 |
| Gait Speed b | |||
| Age | −0.01 | −0.02: −0.002 | 0.01 |
| Acute pain | −0.23 | −0.44: −0.02 | 0.03 |
| Chair Lift Test c | |||
| Acute pain | 3.7 | −0.34: 7.75 | 0.04 |
| SPPB Total | |||
| Age | −0.1 | −0.16: −0.03 | 0.01 |
| Acute pain | −1.9 | −3.28: −0.43 | 0.01 |
| Variables | ß | 95% CI | p-Value |
|---|---|---|---|
| Dichotomous Pain | |||
| Age | −0.19 | −0.08: 0.46 | 0.17 |
| Male | −4.60 | −8.60: −0.60 | 0.02 |
| No use of psychotropics | −4.70 | −8.56: −0.85 | 0.01 |
| Perceived good health | −0.89 | −5.36: 3.57 | 0.69 |
| GDS score | 1.06 | 0.49: 1.63 | <0.01 |
| Dichotomous pain (yes) | 5.47 | 1.51: 9.43 | <0.01 |
| Categorical GPM | |||
| Age | 0.19 | −0.02: −0.002 | 0.18 |
| Male | −5.06 | −9.13: −1.00 | 0.01 |
| No use of psychotropics | −4.40 | −8.35: −0.44 | 0.03 |
| Good health perceived | 0.01 | −4.92: 4.94 | 0.90 |
| GDS score | 1.05 | 0.46: 1.63 | <0.01 |
| Pain Intensity (GPM) | |||
| Light | 0 | 0 | 0 |
| Moderate | 4.04 | −0.26: 8.36 | 0.06 |
| Intense | 7.15 | 0.27: 14.03 | 0.04 |
| Chronic Pain | |||
| Age | 0.22 | −0.05: −0.50 | 0.11 |
| Male | −5.43 | −9.43: −1.42 | <0.01 |
| No use of psychotropics | −4.79 | −8.73: −0.85 | 0.01 |
| Perceived health | −0.95 | −5.61: 3.70 | 0.68 |
| GDS score | 1.04 | 0.46: 1.62 | <0.01 |
| Chronic pain (yes) | 3.82 | −0.22: 7.86 | 0.06 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandes, S.G.; Sales, W.B.; Tavares, D.V.; Pereira, D.d.S.; Nóbrega, P.V.d.N.; Holanda, C.M.d.A.; Maciel, A.C.C. Relationship between Pain, Fear of Falling and Physical Performance in Older People Residents in Long-Stay Institutions: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 12014. https://doi.org/10.3390/ijerph191912014
Fernandes SG, Sales WB, Tavares DV, Pereira DdS, Nóbrega PVdN, Holanda CMdA, Maciel ACC. Relationship between Pain, Fear of Falling and Physical Performance in Older People Residents in Long-Stay Institutions: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(19):12014. https://doi.org/10.3390/ijerph191912014
Chicago/Turabian StyleFernandes, Sabrina Gomes, Weslley Barbosa Sales, Diego Villar Tavares, Dayanna da Silva Pereira, Patrícia Vidal de Negreiros Nóbrega, Cristina Marques de Almeida Holanda, and Alvaro Campos Cavalcanti Maciel. 2022. "Relationship between Pain, Fear of Falling and Physical Performance in Older People Residents in Long-Stay Institutions: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 19: 12014. https://doi.org/10.3390/ijerph191912014
APA StyleFernandes, S. G., Sales, W. B., Tavares, D. V., Pereira, D. d. S., Nóbrega, P. V. d. N., Holanda, C. M. d. A., & Maciel, A. C. C. (2022). Relationship between Pain, Fear of Falling and Physical Performance in Older People Residents in Long-Stay Institutions: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(19), 12014. https://doi.org/10.3390/ijerph191912014








