Clinical-Functional Vulnerability, Functional Capacity, and Falls in Octogenarians with Different Physical Activity Levels—A Cross-Sectional Study
Abstract
1. Introduction
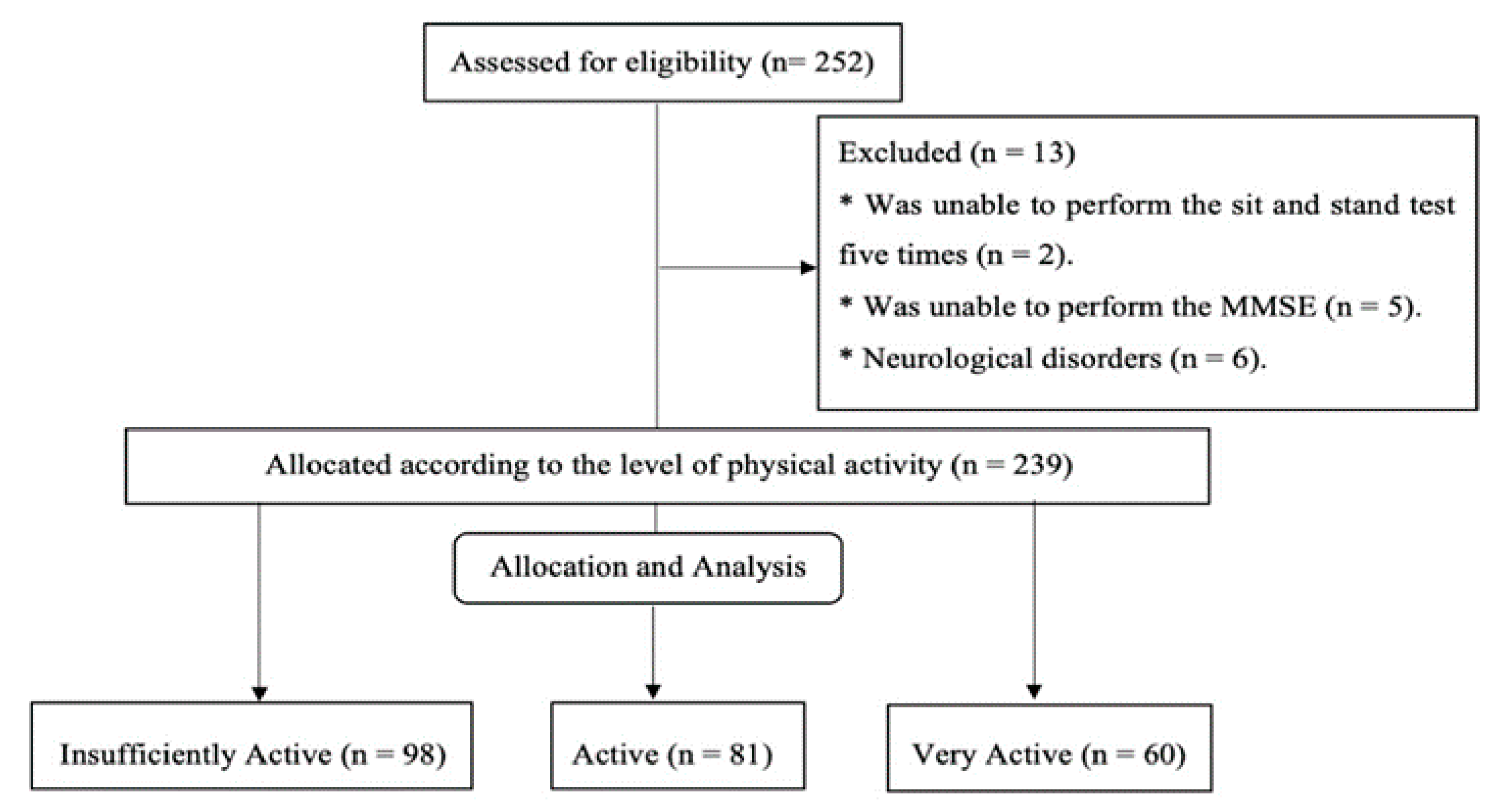
2. Methods
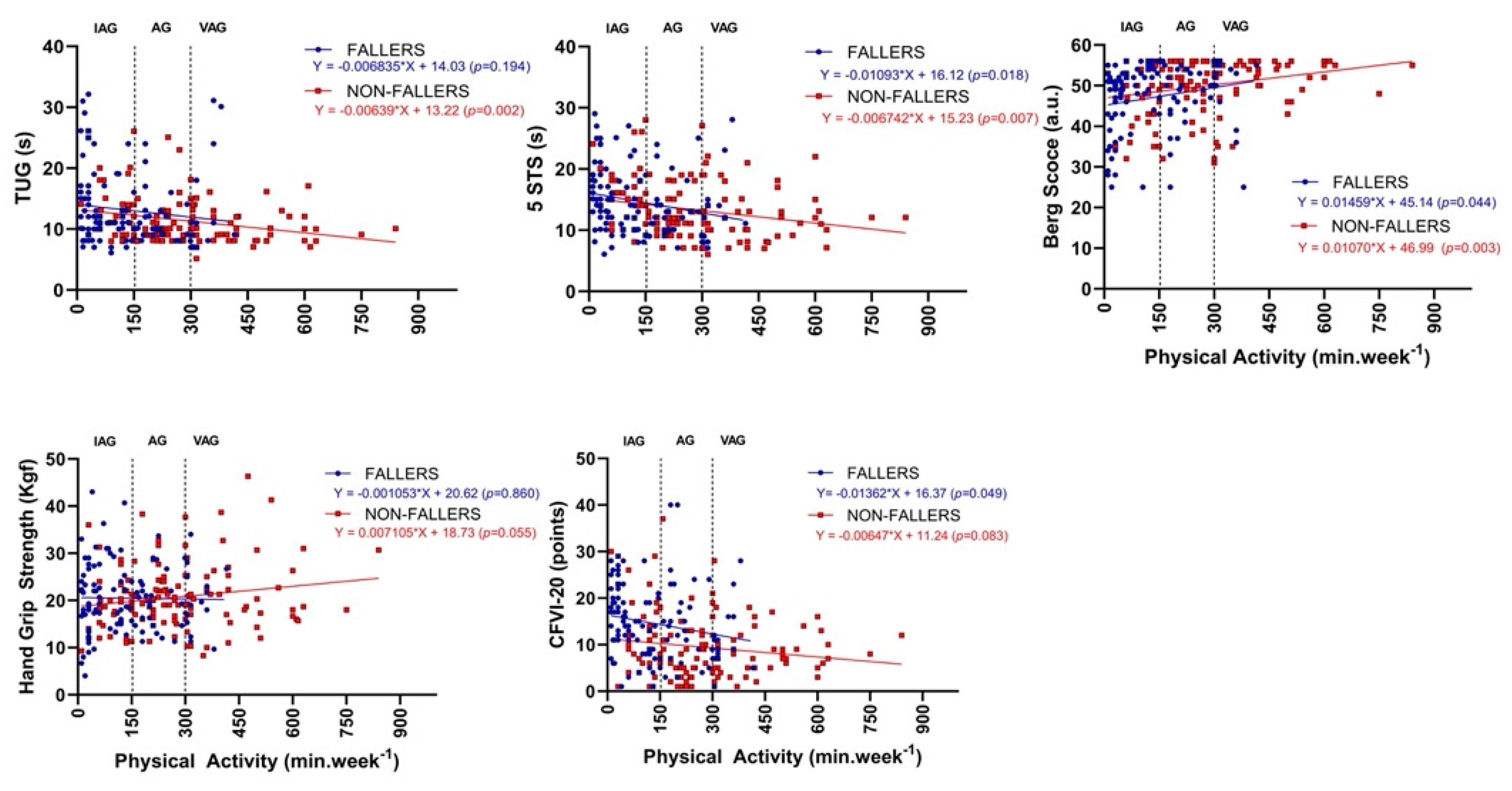
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, P.D.; Lv, Y.B.; Li, Z.H.; Yin, Z.X.; Li, F.R.; Wang, J.N.; Zhang, X.R.; Zhou, J.H.; Wu, X.B.; Duan, J.; et al. Age, period, and cohort effects on activities of daily living, physical performance, and cognitive functioning impairment among the oldest-old in China. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2020, 75, 1214–1221. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Vellas, B.; Van Kan, G.A.; Ankler, S.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.C.; Doehner, W.; Evans, J.; et al. Frailty Consensus: A Call to Action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef] [PubMed]
- Moreira, N.B.; Bento, P.C.B.; Vieira, E.R.; da Silva, J.L.P.; Rodacki, A.L.F. Comparison between the Clinical-Functional Vulnerability and the Frailty Phenotype to Identify Falls in Elderly: A Cross-Sectional Study. Ann. Phys. Rehabil. Med. 2022; in press. [Google Scholar]
- Landi, F.; Abbatecola, A.M.; Provinciali, M.; Corsonello, A.; Bustacchini, S.; Manigrasso, L.; Cherubini, A.; Bernabei, R.; Lattanzio, F. Moving against frailty: Does physical activity matter? Biogerontology 2010, 11, 537–545. [Google Scholar] [CrossRef]
- Berkemeyer, K.; Wijndaele, K.; White, T.; Cooper, A.J.M.; Luben, R.; Westgate, K.; Griffin, S.J.; Khaw, K.T.; Wareham, N.J.; Brage, S. The descriptive epidemiology of accelerometer-measured physical activity in older adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 2. [Google Scholar] [CrossRef]
- Moreira, N.B.; Rodacki, A.L.F.; Pereira, G.; Bento, P.C.B. Does functional capacity, fall risk awareness and physical activity level predict falls in older adults in different age groups? Arch. Gerontol. Geriatr. 2018, 77, 57–63. [Google Scholar] [CrossRef]
- Franceschi, C.; Garagnani, P.; Morsiani, C.; Conte, M.; Santoro, A.; Grignolio, A.; Monti, D.; Capri, M.; Salvioli, S. The continuum of aging and age-related diseases: Common mechanisms but different rates. Front. Med. 2018, 5, 61. [Google Scholar] [CrossRef]
- Ramsey, K.A.; Rojer, A.G.M.; D’Andrea, L.; Otten, R.H.J.; Heymans, M.W.; Trappenburg, M.C.; Verlaan, S.; Whittaker, A.C.; Meskers, C.G.M.; Maier, A.B. The association of objectively measured physical activity and sedentary behavior with skeletal muscle strength and muscle power in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2021, 67, 101266. [Google Scholar] [CrossRef]
- Lustosa, L.P.; Pereira, D.S.; Dias, R.C.; Britto, R.R.; Parentoni, A.N.; Souza, L.; Pereira, M. Tradução e adaptação transcultural do Minnesota Leisure Time Activities Questionnaire em idosos. Geriatr. Gerontol. 2011, 5, 57–65. [Google Scholar]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- de Moraes, E.N.; do Carmo, J.A.; de Moraes, F.L.; Azevedo, R.S.; Machado, C.J.; Montilla, D.E.R. Clinical-Functional Vulnerability Index-20 (IVCF-20): Rapid recognition of frail older adults. Rev. Saude Publica 2016, 50, 81. [Google Scholar] [CrossRef] [PubMed]
- Moreira, B.; Bento, P.C.B.; Vieira, E.R.; Silva, L.P.; Rodacki, A.L.F. Association between Domains of the Clinical-Functional Vulnerability Index and Falls History in Older Adults: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 7949. [Google Scholar] [CrossRef] [PubMed]
- Sato, S.; Takeda, N.; Yamada, T.; Nakamura, M.; Nemoto, Y.; Maruo, K.; Fukuda, Y.; Sawada, S.S.; Kitabatake, Y.; Arao, T. Physical activity and/or sedentary behaviour and the development of functional disability in community-dwelling older adults in Tsuru, Japan: A prospective cohort study (the Tsuru Longitudinal Study). BMJ Open 2022, 12, e056642. [Google Scholar] [CrossRef] [PubMed]
- Hortobágyi, T.; Mizelle, C.; Beam, S.; DeVita, P. Old adults perform activities of daily living near their maximal capabilities. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2003, 58, 453–460. [Google Scholar] [CrossRef]
- Zhou, J.; Liu, B.; Qin, M.Z.; Liu, J.P. A prospective cohort study of the risk factors for new falls and fragility fractures in self-caring elderly patients aged 80 years and over. BMC Geriatr. 2021, 21, 116. [Google Scholar] [CrossRef]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: A systematic review and meta- analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef]
- Bouatois, S. Five Times Sit to Stand Test Is a Predictor of recurrent Falls in Healthy Community Living Subjects aged 65 and Older. J. Am. Geriatr. Soc. 2008, 56, 1575–1577. [Google Scholar] [CrossRef]
- Thorbahn, L.D.; Newton, R.A. Use of the Berg balance test to predict falls in elderly persons. Phys. Ther. 1996, 76, 576–585. [Google Scholar] [CrossRef]
- Dionyssiotis, Y. Analyzing the problem of falls among older people. Int. J. Gen. Med. 2012, 5, 805–813. [Google Scholar] [CrossRef]
- Fujiwara, K.; Toyama, H.; Asai, H.; Maeda, K.; Yaguchi, C. Regular heel-raise training focused on the soleus for the elderly: Evaluation of muscle thickness by ultrasound. J. Physiol. Anthropol. 2010, 29, 23–28. [Google Scholar] [CrossRef]
- MacLean, M.K.; Ferris, D.P. Human muscle activity and lower limb biomechanics of overground walking at varying levels of simulated reduced gravity and gait speeds. PLoS ONE 2021, 16, e0253467. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, K. The features of muscle activity during chair standing and sitting motion in submerged condition. PLoS ONE 2019, 14, e0220602. [Google Scholar] [CrossRef] [PubMed]
- Rodacki, A.L.F.; Moreira, N.B.; Pitta, A.; Wolf, R.; Filho, J.M.; Rodacki, C.d.L.N.; Pereira, G. Is handgrip strength a useful measure to evaluate lower limb strength and functional performance in older women? Clin. Interv. Aging 2020, 15, 1045–1056. [Google Scholar] [CrossRef]
- Lin, Y.H.; Chen, Y.C.; Tseng, Y.C.; Tsai, S.T.; Tseng, Y.H. Physical activity and successful aging among middle-aged and older adults: A systematic review and meta-analysis of cohort studies. Aging 2020, 12, 7704–7716. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, F.; Macagnan, D.; Canei, F.C.; da Silva, M.R.; dos Santos, M.P.M. Physical activity level among older adults over 70 years old and very old adults. Fisioter. Mov. 2020, 33, 1–2. [Google Scholar] [CrossRef]
- Patti, A.; Zangla, D.; Sahin, F.N.; Cataldi, S.; Lavanco, G.; Palma, A.; Fischietti, F. Physical exercise and prevention of falls. Effects of a Pilates training method compared with a general physical activity program A randomized controlled trial. Medicine 2021, 100, e25289. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020; ISBN 9781134470006. [Google Scholar]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef] [PubMed]
- Visser, D.; Wattel, E.M.; Gerrits, K.H.L.; van der Wouden, J.C.; Meiland, F.J.M.; de Groot, A.J.; Jansma, E.P.; Hertogh, C.M.P.M.; Smit, E.B. Effectiveness and characteristics of physical fitness training on aerobic fitness in vulnerable older adults: An umbrella review of systematic reviews. BMJ Open 2022, 12, e058056. [Google Scholar] [CrossRef]
| Characteristics | ALL (n = 239) Mean ± SD | IAG (n = 98) Mean ± SD | AG (n = 81) Mean ± SD | VAG (n = 60) Mean ± SD | p Value |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Education level | 0.498 | ||||
| Illiterate | 29 (12.1) | 12 (12.2) | 12 (14.8) | 5 (8.3) | |
| 1–8 years | 158 (66.1) | 66 (67.3) | 51 (63.0) | 41 (68.3) | |
| >8 years | 24 (10.0) | 11 (11.2) | 5 (6.2) | 8 (13.4) | |
| Higher education | 28 (11.8) | 9 (9.3) | 13 (16.0) | 6 (10.0) | |
| Marital status | 0.724 | ||||
| Married | 58 (24.3) | 26 (26.5) | 17 (21.0) | 15 (25.0) | |
| Divorced | 8 (3.3) | 2 (2.0) | 3 (3.7) | 3 (5.0) | |
| Single | 17 (7.1) | 9 (9.2) | 6 (7.4) | 2 (3.3) | |
| Widowed | 156 (65.3) | 61 (62.2) | 55 (67.9) | 40 (66.7) |
| Characteristics | ALL (n = 239) Mean ± SD | IAG (n = 98) Mean ± SD | AG (n = 81) Mean ± SD | VAG (n = 60) Mean ± SD | p Value |
|---|---|---|---|---|---|
| Age (years) | 84 ± 3 | 84 ± 4 | 84 ± 3 | 84 ± 3 | 0.658 |
| BMI (kg m−2) | 26 ± 4 | 26 ± 4 | 27 ± 4 | 26 ± 3 | 0.343 |
| PA (min week−1) | 209 ± 157 | 69 ± 44 b,c | 221 ± 46 a,c | 421 ± 124 a,b | <0.001 |
| 5STS (s) | 13.97 ± 5.03 | 15.63 ± 5.16 b,c | 13.01 ± 4.55 | 12.56 ± 4.72 | <0.001 |
| TUG (s) | 12.23 ± 5.09 | 13.55 ± 5.72 b,c | 11.47 ± 4.00 | 11.11 ± 4.91 | 0.002 |
| BBS (points) | 48.61 ± 7.68 | 46.72 ± 8.25 c | 49.12 ± 7.11 | 51.00 ± 6.71 | 0.001 |
| HGS (kgf) | 20.58 ± 6.98 | 20.26 ± 7.31 | 20.65 ± 5.87 | 21.00 ± 7.86 | 0.843 |
| Gender | n (%) | n (%) | n (%) | n (%) | |
| Female | 176 (73.6) | 70 (39.8) | 59 (33.5) | 47 (26.7) | 0.620 |
| Male | 63 (26.4) | 28 (44.4) | 22 (34.9) | 13 (20.6) | |
| Falls | |||||
| Yes | 110 (46.0) | 67 (68.4) b,c | 29 (35.8) | 14 (23.3) | <0.001 |
| No | 129 (54.0) | 31 (31.6) b,c | 52 (64.2) | 46 (76.7) | |
| Frailty Vulnerability (CFVI-20) | |||||
| Low vulnerability | 67 (28.0) | 17 (17.3) b,c | 30 (37.0) | 20 (33.3) | 0.001 |
| Moderate vulnerability | 98 (41.0) | 37 (37.8) | 31 (38.3) | 30 (50.0) | |
| High vulnerability | 74 (31.0) | 44 (44.9) b,c | 20 (24.7) | 10 (16.7) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, L.P.; Moreira, N.B.; Grando, R.Z.; Bento, P.C.B.; Rodacki, A.L.F. Clinical-Functional Vulnerability, Functional Capacity, and Falls in Octogenarians with Different Physical Activity Levels—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 11909. https://doi.org/10.3390/ijerph191911909
da Silva LP, Moreira NB, Grando RZ, Bento PCB, Rodacki ALF. Clinical-Functional Vulnerability, Functional Capacity, and Falls in Octogenarians with Different Physical Activity Levels—A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(19):11909. https://doi.org/10.3390/ijerph191911909
Chicago/Turabian Styleda Silva, Letícia Pophal, Natália Boneti Moreira, Renata Zacharias Grando, Paulo César Baraúce Bento, and André Luiz Felix Rodacki. 2022. "Clinical-Functional Vulnerability, Functional Capacity, and Falls in Octogenarians with Different Physical Activity Levels—A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 19: 11909. https://doi.org/10.3390/ijerph191911909
APA Styleda Silva, L. P., Moreira, N. B., Grando, R. Z., Bento, P. C. B., & Rodacki, A. L. F. (2022). Clinical-Functional Vulnerability, Functional Capacity, and Falls in Octogenarians with Different Physical Activity Levels—A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(19), 11909. https://doi.org/10.3390/ijerph191911909







