Association between COVID-19 and Sick Leave for Healthcare Workers in a Large Academic Hospital in Southern Italy: An Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Variables
2.3. Statistical Analyses
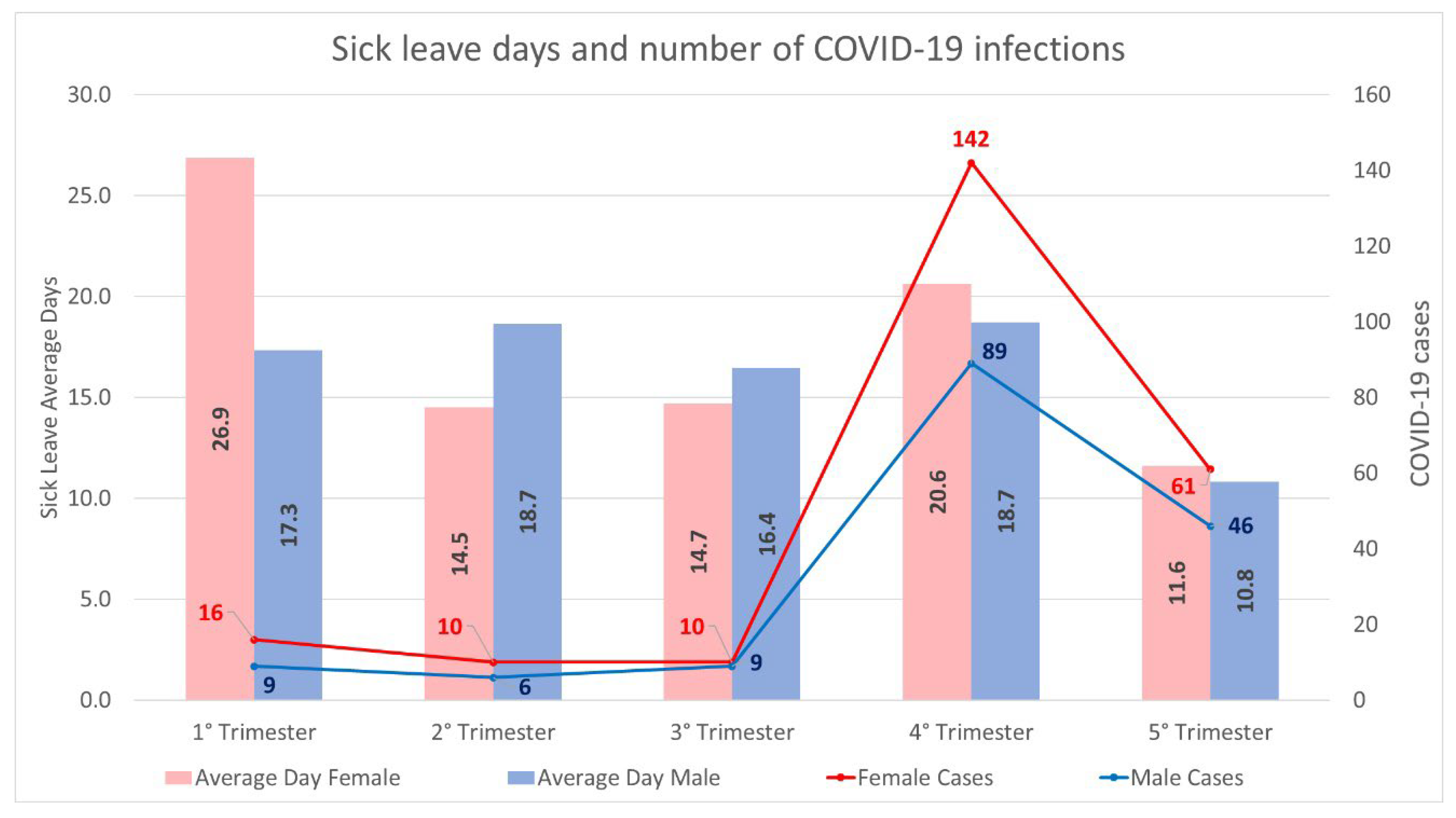
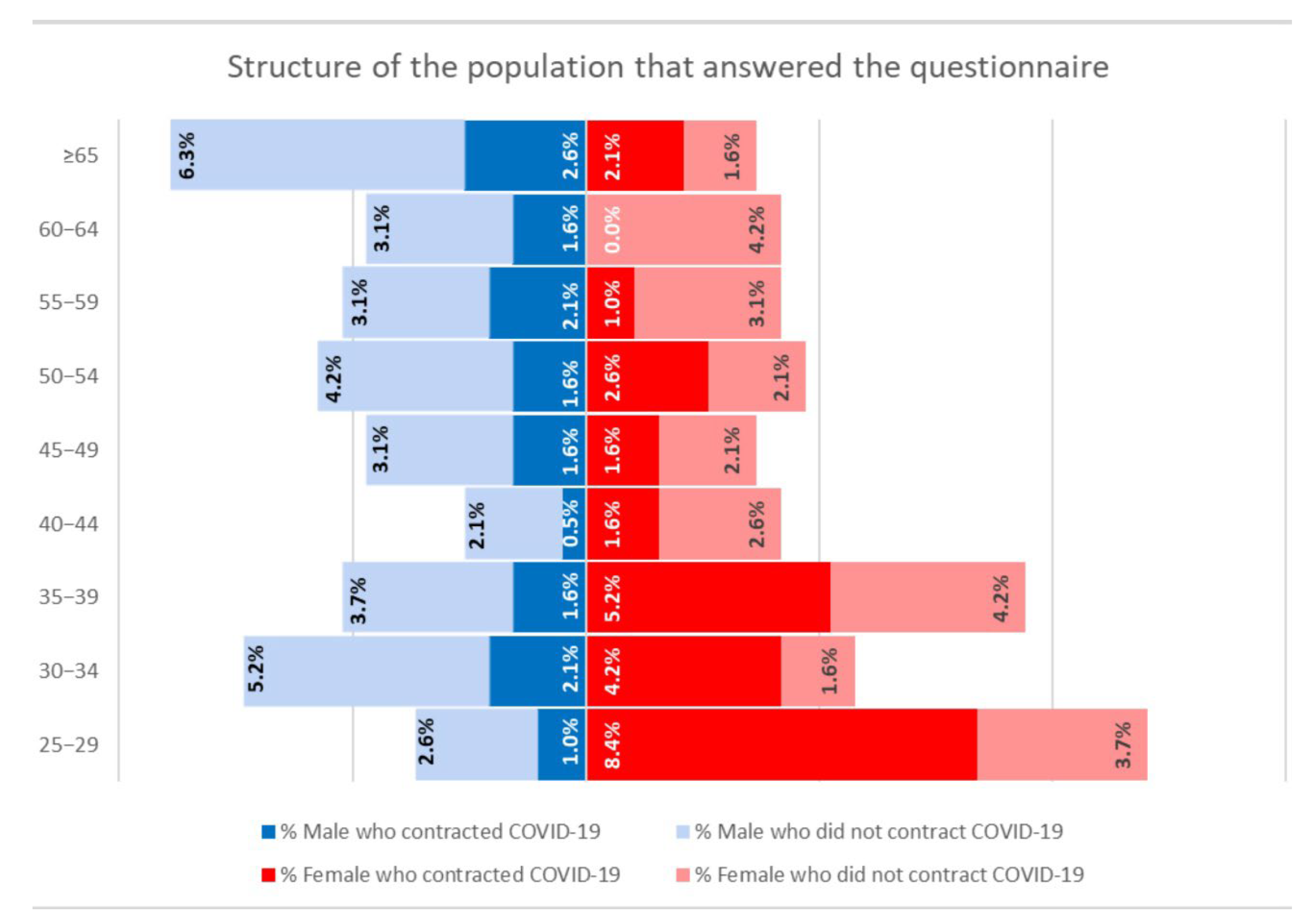
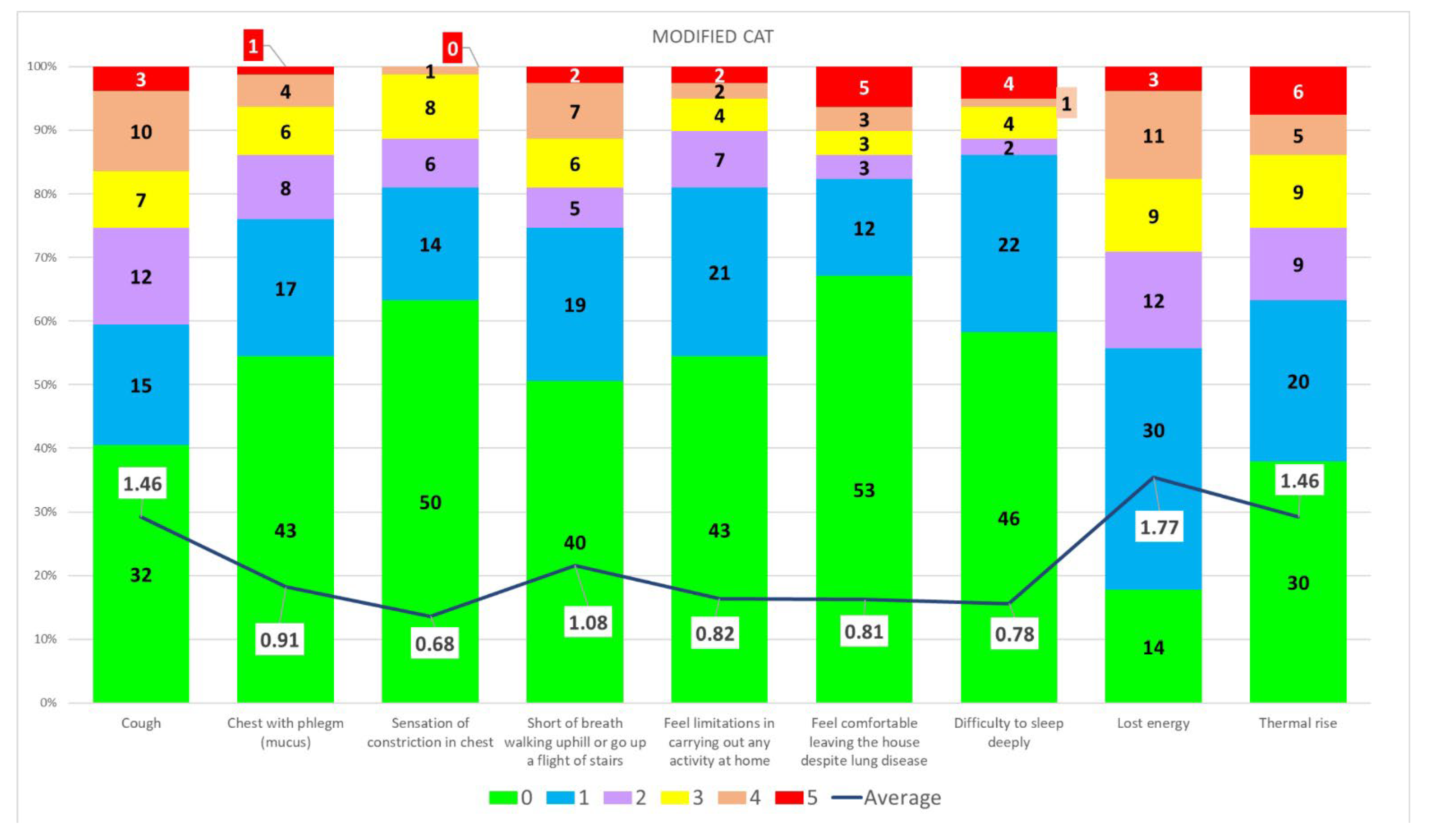
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johns Hopkins University of Medicine. Johns Hopkins Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 22 May 2022).
- Torjesen, I. Covid-19: Omicron may be more transmissible than other variants and partly resistant to existing vaccines, scientists fear. BMJ 2021, 375, n2943. [Google Scholar] [CrossRef] [PubMed]
- WHO. Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed on 22 May 2022).
- Public Health England. Investigation of novel SARS-COV-2 Variant Variant of Concern 202012/01; Public Health England: London, UK, 2020.
- Stefanelli, P.; Presti, A.L.; Ambrosio, L.; Martino, A.D.; Morabito, S.; Vaccari, G.; Bartolo, I.D.; Knijn, A.; Riccardo, F.; Petrone, D.; et al. Prevalenza E Distribuzione Delle Varianti Di SARS-CoV-2 Di Interesse Per La Sanità Pubblica in Italia Rapporto n. 5 del 23 luglio 2021; Istituto Superiore di Sanità: Rome, Italy, 2021.
- Singh, J.; Rahman, S.A.; Ehtesham, N.Z.; Hira, S.; Hasnain, S.E. SARS-CoV-2 variants of concern are emerging in India. Nat. Med. 2021, 27, 1131–1133. [Google Scholar] [CrossRef] [PubMed]
- Stefanelli, P.; Martino, A.D.; Presti, A.L.; Ambrosio, L.; Morabito, S.; Vaccari, G.; Bartolo, I.D.; Knijn, A.; Riccardo, F.; Petrone, D.; et al. Prevalenza E Distribuzione Delle Varianti Di SARS-CoV-2 Di Interesse Per La Sanità Pubblica in Italia Rapporto N. 16 Del 19 Gennaio 2022; Istituto Superiore di Sanità: Rome, Italy, 2022.
- Zhang, X.; Wu, S.; Wu, B.; Yang, Q.; Chen, A.; Li, Y.; Zhang, Y.; Pan, T.; Zhang, H.; He, X.; et al. SARS-CoV-2 Omicron strain exhibits potent capabilities for immune evasion and viral entrance. Signal Transduct. Target. Ther. 2021, 6, 430. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Wang, J.; Jian, F.; Xiao, T.; Song, W.; Yisimayi, A.; Huang, W.; Li, Q.; Wang, P.; An, R. Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature 2022, 602, 657–663. [Google Scholar] [CrossRef]
- Cele, S.; Jackson, L.; Khoury, D.S.; Khan, K.; Moyo-Gwete, T.; Tegally, H.; Emmanuel San, J.; Cromer, D.; Scheepers, C.; Amoako, D.G. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature 2022, 602, 654–656. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Lu, L.; Peng, Z.; Chen, L.-L.; Meng, X.; Zhang, C.; IP, D.; Chan, W.-M.; Chu, A.K.-H.; Jin, D.-Y.; et al. SARS-CoV-2 Omicron variant shows less efficient replication and fusion activity when compared with Delta variant in TMPRSS2-expressed cells. Emerg. Microbes Infect. 2022, 11, 277–283. [Google Scholar] [CrossRef]
- Meng, B.; Abdullahi, A.; Ferreira, I.A.T.M.; Goonawardane, N.; Saito, A.; Kimura, I.; Yamasoba, D.; Pereyra Gerber, P.; Fatihi, S.; Rathore, S.; et al. Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity. Nature 2022, 603, 706–714. [Google Scholar] [CrossRef]
- Nishiura, H.; Ito, K.; Anzai, A.; Kobayashi, T.; Piantham, C.; Rodríguez-Morales, A.J. Relative Reproduction Number of SARS-CoV-2 Omicron (B.1.1.529) Compared with Delta Variant in South Africa. J. Clin. Med. 2021, 11, 30. [Google Scholar] [CrossRef]
- Wolter, N.; Jassat, W.; Walaza, S.; Welch, R.; Moultrie, H.; Groome, M.; Amoako, D.G.; Everatt, J.; Bhiman, J.N.; Scheepers, C.; et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: A data linkage study. Lancet 2022, 399, 437–446. [Google Scholar] [CrossRef]
- Calvo-Bonacho, E.; Catalina-Romero, C.; Fernández-Labandera, C.; Fernández-Meseguer, A.; González-Quintela, A.; Martínez-Muñoz, P.; Quevedo, L.; Valdivielso, P.; Sánchez-Chaparro, M. COVID-19 and Sick Leave: An Analysis of the Ibermutua Cohort of Over 1,651,305 Spanish Workers in the First Trimester of 2020. Front. Public Health 2020, 8, 580546. [Google Scholar] [CrossRef]
- Alquézar-Arbé, A.; Piñera, P.; Jacob, J.; Martín, A.; Jiménez, S.; Llorens, P.; Martín-Sánchez, F.J.; Burillo-Putze, G.; García-Lamberechts, E.J.; del Castilloizzi, J.G.; et al. Impact of the COVID-19 pandemic on hospital emergency departments: Results of a survey of departments in 2020—the Spanish ENCOVUR study. Emergencias 2020, 32, 320–331. [Google Scholar]
- Bellotti, L.; Zaniboni, S.; Balducci, C.; Grote, G. Rapid Review on COVID-19, Work-Related Aspects, and Age Differences. Int. J. Environ. Res. Public Health 2021, 18, 5166. [Google Scholar] [CrossRef] [PubMed]
- Prato’, S.; Paladino, M.E.; Riva, M.A.; Belingheri, M. COVID-19 Vaccination and Asymptomatic Infection. J. Occup. Environ. Med. 2021, 63, e868–e870. [Google Scholar] [CrossRef] [PubMed]
- Strum, E.; Casagrande, Y.; Newton, K.; Unger, J.B. Healthcare workers benefit from second dose of COVID-19 mRNA vaccine: Effects of partial and full vaccination on sick leave duration and symptoms. Public Health Pract. 2022, 3, 100247. [Google Scholar] [CrossRef] [PubMed]
- Vahidy, F.S.; Pan, A.P.; Hagan, K.; Bako, A.T.; Sostman, H.D.; Schwartz, R.L.; Phillips, R.; Boom, M.L. Impact of mRNA vaccines in curtailing SARS-CoV-2 infection and disability leave utilisation among healthcare workers during the COVID-19 pandemic: Cross-sectional analysis from a tertiary healthcare system in the Greater Houston metropolitan area. BMJ Open 2021, 11, e054332. [Google Scholar] [CrossRef]
- Jones, P.W.; Brusselle, G.; Negro, R.W.D.; Ferrer, M.; Kardos, P.; Levy, M.L.; Perez, T.; Cataluna, J.J.S.; van der Molen, T.; Adamek, L.; et al. Properties of the COPD assessment test in a cross-sectional European study. Eur. Respir. J. 2011, 38, 29–35. [Google Scholar] [CrossRef] [Green Version]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef] [Green Version]
- Daynes, E.; Gerlis, C.; Briggs-Price, S.; Jones, P.; Singh, S.J. COPD assessment test for the evaluation of COVID-19 symptoms. Thorax 2021, 76, 185–187. [Google Scholar] [CrossRef]
- Lerum, T.V.; Maltzahn, N.N.; Aukrust, P.; Trøseid, M.; Henriksen, K.N.; Kåsine, T.; Dyrhol-Riise, A.-M.; Stiksrud, B.; Haugli, M.; Blomberg, B.; et al. Persistent pulmonary pathology after COVID-19 is associated with high viral load, weak antibody response, and high levels of matrix metalloproteinase-9. Sci. Rep. 2021, 11, 23205. [Google Scholar] [CrossRef]
- Ghobadi, H.; Ahari, S.S.; Kameli, A.; Lari, S.M. The Relationship between COPD Assessment Test (CAT) Scores and Severity of Airflow Obstruction in Stable COPD Patients. Tanaffos 2012, 11, 22–26. [Google Scholar]
- Westerlind, E.; Palstam, A.; Sunnerhagen, K.S.; Persson, H.C. Patterns and predictors of sick leave after Covid-19 and long Covid in a national Swedish cohort. BMC Public Health 2021, 21, 1023. [Google Scholar] [CrossRef] [PubMed]
- Colaneri, M.; Novelli, V.; Cutti, S.; Muzzi, A.; Resani, G.; Monti, M.S.; Rona, C.; Grugnetti, A.M.; Rettani, M.; Rovida, F.; et al. The experience of the health care workers of a severely hit SARS-CoV-2 referral Hospital in Italy: Incidence, clinical course and modifiable risk factors for COVID-19 infection. J. Public Health 2021, 43, 26–34. [Google Scholar] [CrossRef] [PubMed]
- McFarlin, K. Thomas, S.S.; Kane, T.; Buell, J.; Thomas, N.; Shivkumar, A. Characteristic Features of COVID-19 Illness Among Healthcare Workers: A Retrospective Analysis. Cureus 2021, 13, e18816. [Google Scholar] [CrossRef] [PubMed]

| Variable | Coefficient | [95% Confidence Interval] | |
|---|---|---|---|
| Trimester | −1.23 | −2.39 | −0.06 |
| Sex—Male | −2.18 | −4.39 | 0.04 |
| Age | 0.05 | −0.04 | 0.14 |
| Vaccinated | −3.11 | −4.44 | −1.78 |
| Variable | Coefficient | [95% Confidence Interval] | |
|---|---|---|---|
| Trimester | 1.04 | −0.93 | 3.01 |
| Sex—Male | −3.65 | −7.93 | 0.64 |
| Age | 0.05 | −0.11 | 0.20 |
| Received booster dose | 1.22 | −4.93 | 7.38 |
| COVID-19 infection after vaccine | −4.96 | −16.11 | 6.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palladino, R.; Mercogliano, M.; Fiorilla, C.; Frangiosa, A.; Iodice, S.; Sanduzzi Zamparelli, S.; Montella, E.; Triassi, M.; Sanduzzi Zamparelli, A. Association between COVID-19 and Sick Leave for Healthcare Workers in a Large Academic Hospital in Southern Italy: An Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 9670. https://doi.org/10.3390/ijerph19159670
Palladino R, Mercogliano M, Fiorilla C, Frangiosa A, Iodice S, Sanduzzi Zamparelli S, Montella E, Triassi M, Sanduzzi Zamparelli A. Association between COVID-19 and Sick Leave for Healthcare Workers in a Large Academic Hospital in Southern Italy: An Observational Study. International Journal of Environmental Research and Public Health. 2022; 19(15):9670. https://doi.org/10.3390/ijerph19159670
Chicago/Turabian StylePalladino, Raffaele, Michelangelo Mercogliano, Claudio Fiorilla, Alessandro Frangiosa, Sabrina Iodice, Stefano Sanduzzi Zamparelli, Emma Montella, Maria Triassi, and Alessandro Sanduzzi Zamparelli. 2022. "Association between COVID-19 and Sick Leave for Healthcare Workers in a Large Academic Hospital in Southern Italy: An Observational Study" International Journal of Environmental Research and Public Health 19, no. 15: 9670. https://doi.org/10.3390/ijerph19159670
APA StylePalladino, R., Mercogliano, M., Fiorilla, C., Frangiosa, A., Iodice, S., Sanduzzi Zamparelli, S., Montella, E., Triassi, M., & Sanduzzi Zamparelli, A. (2022). Association between COVID-19 and Sick Leave for Healthcare Workers in a Large Academic Hospital in Southern Italy: An Observational Study. International Journal of Environmental Research and Public Health, 19(15), 9670. https://doi.org/10.3390/ijerph19159670







