Prevalence, Predictors, and Experience of Moral Suffering in Nursing and Care Home Staff during the COVID-19 Pandemic: A Mixed-Methods Systematic Review
Abstract
:1. Introduction
- What is the estimated prevalence of MI and MD?
- What factors increase the likelihood of developing MI and MD?
- What is the psychological impact and general experience of MI and MD?
2. Materials and Methods
2.1. Main Method
2.2. Information Sources and Search Strategy
2.3. Eligibility Criteria
2.4. Study Selection, Quality Assessment, and Extraction Process
2.5. Data Analysis
3. Results
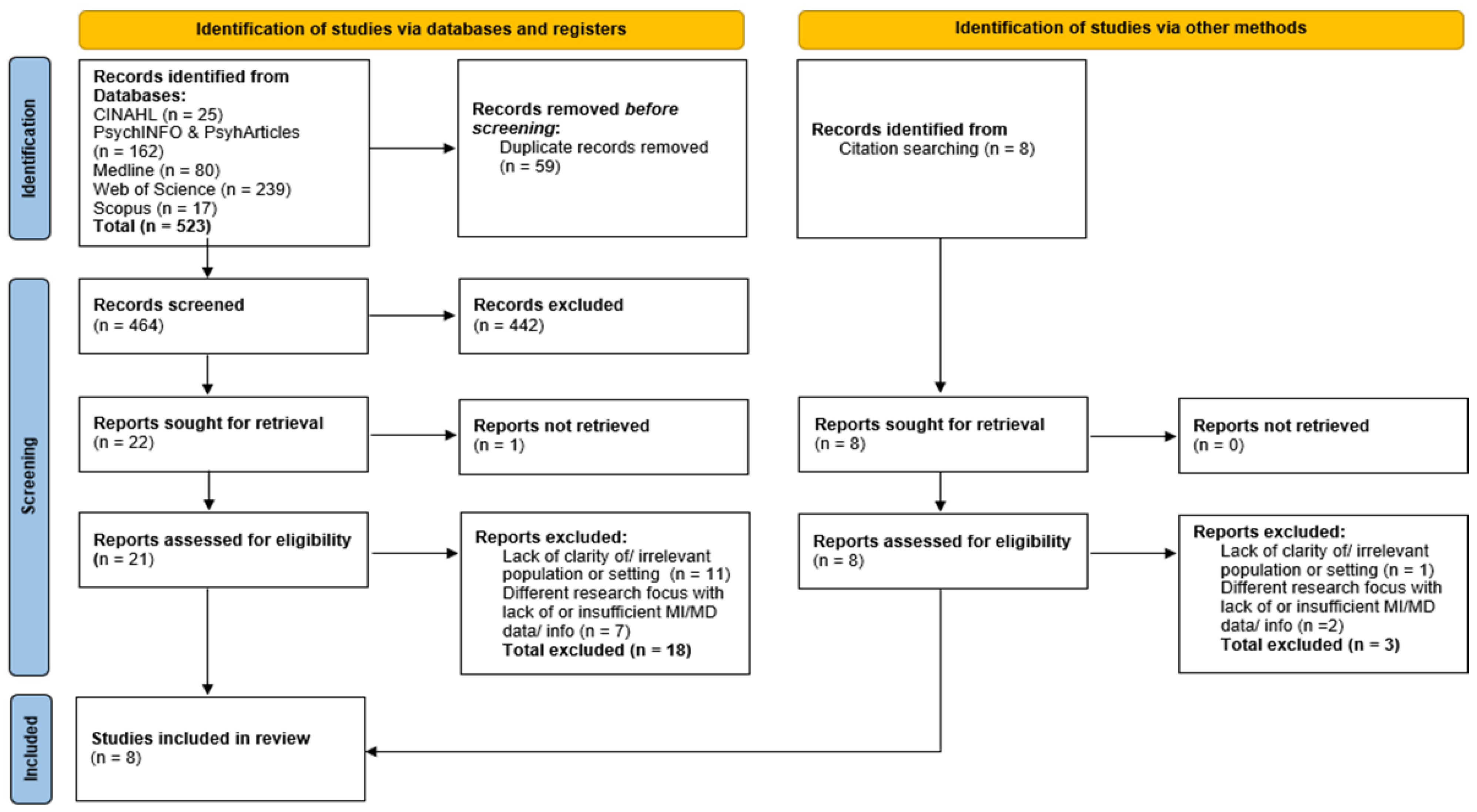
3.1. Number of Studies Screened and Included
3.2. Characteristics of Studies and Quality Appraisal
3.3. Quantitative Synthesis
3.3.1. Levels of MI and MD
3.3.2. MI and MD Psychosocial Impacts
3.4. Qualitative Synthesis
3.4.1. Resource Deficits
“Although I feel satisfied with my profession, I also feel helpless for not being able to carry out my duties effectively due to lack of resources. The measures are applied too late, and people die”[51] (p. 10, col. 4, lines 33–35).
“The whole thing has been exhausting and extremely stressful. We had an exposure in the nursing home and that was the worst two weeks of my career. No-one contracted COVID-19 but I was working over 12 h a day for the two weeks to ensure everyone was ok”[52] (p. 53, col. 4, lines 22–27).
“We had a lot of staff who were sick. We worked understaffed. We worked for two months under-staffed without adequate replacements. It was really painful and very tiring. We were very tired”[47] (p. 11, col. 1, lines 26–28).
“At the beginning of the COVID-19 pandemic, I felt panic. First, I didn’t know much about the COVID-19 virus. Then, I lacked some knowledge about epidemic prevention and control”[50] (p. 890, col. 2, lines 33–35).
3.4.2. Role Challenges
“We worked alternating shifts and were on duty here for 24, 48, or even 72 h. The workload increased a lot. We needed to disinfect the ward area, measure the body temperature of the residents three times per day, and observe whether residents had respiratory symptoms. But the number of nurses didn’t increase”[50] (pp. 890–891, col. 2, lines 42–43 [next page]).
“We were really torn between their happiness, their protection, and at the same time having to be a bit stricter and forcing them to stay in their rooms. It’s a bit abusive to tell someone we’re going to have to lock you up if you leave your room, for your safety, it doesn’t work for us, and in some cases we’ve been forced to lock them up if they’re positive, well we had to lock them up to prevent them from leaving, but it goes against the way we treat our residents”[47] (p. 11, col. 1, lines 17–21).
“I cry…alone, but I cry, when another resident has died or when I watch the news, here in Catalonia there have been horrible moments, when we are told that the elderly should not go to the ICU or to the hospital…that, making those decisions, the ethical dilemma…the feeling of helplessness…that leaves anyone upset, I think we’ll all go into depression when this passes…we’ve lived through some pretty scary, scary things…I’ll never be able to forget it (cries)” [49] (pp. 874–875, col. 2, lines 38–4 [next page]).
3.4.3. Communication and Leadership
“In this work we are totally abandoned, without protective equipment or anyone who controls what is going on”[51] (p. 10, col. 4, lines 7–8).
“Lack of clear instructions from government/Health department”[52] (p. 54, col. 4, lines 3–4).
“COVID-19 has been the trigger that has exposed the deficiencies of the system”[51] (p. 10, col. 4, lines 26–27).
3.4.4. Emotional and Psychosocial Consequences
“We cry together… I have cried with the residents, when the family called… I have cried of rage, of impotence and above all of sorrow, of infinite sorrow…”[49] (p. 875, col. 1, lines 6–8)
“I was scared of getting infected because of inadequate self-protection. We were short of protective equipment and wore the same mask for a few days at a time. I didn’t know if the disinfection that we usually do would be effective”[50] (p. 891, col. 2, lines 36–39).
“It is heartbreaking, and I feel guilty for not being able to remain calm and do more to save the life of my patient and the peace of mind of her children and grandchildren”[51] (p. 10, col. 4, lines 36–38).
3.5. Meta-Aggregation
4. Discussion
Limitations of Review
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO COVID-19 Dashboard. World Health Organization: Geneva, Switzerland, 2020; Available online: https://covid19.who.int/ (accessed on 13 January 2022).
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Mo, S.; Shi, J. The psychological consequences of the COVID-19 on residents and staff in nursing homes. Work. Aging Retire 2020, 6, 254–259. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Aging. Residential Facilities, Assisted Living, and Nursing Homes. National Institute on Aging. Available online: https://www.nia.nih.gov/health/residential-facilities-assisted-living-and-nursing-homes (accessed on 12 January 2022).
- Kang, S.; Jung, S.I. Age-related morbidity and mortality among patients with COVID-19. Infect. Chemother 2020, 52, 154–164. [Google Scholar] [CrossRef] [PubMed]
- Ouslander, J.G.; Grabowski, D.C. COVID-19 in Nursing Homes: Calming the Perfect Storm. J. Am. Geriatr. Soc. 2020, 68, 2153–2162. [Google Scholar] [CrossRef] [PubMed]
- Deaths Involving COVID-19 in the Care Sector, England and Wales—Office for National Statistics. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/deathsinvolvingcovid19inthecaresectorenglandandwales/deathsregisteredbetweenweekending20march2020andweekending21january2022 (accessed on 30 June 2022).
- Litam, S.D.A.; Balkin, R.S. Moral injury in health-care workers during COVID-19 pandemic. Traumatology 2021, 27, 14–19. [Google Scholar] [CrossRef]
- Williamson, V.; Murphy, D.; Greenberg, N. COVID-19 and experiences of moral injury in front-line key workers. Occup. Med. 2020, 70, 317–319. [Google Scholar] [CrossRef] [Green Version]
- Litz, B.T.; Stein, N.; Delaney, E.; Lebowitz, L.; Nash, W.P.; Silva, C.; Maguen, S. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clin. Psychol. Rev. 2009, 29, 695–706. [Google Scholar] [CrossRef]
- Shay, J. The trials of homecoming: Odysseus returns from iraq/afghanistan. Smith Coll. Stud. Soc. Work 2009, 79, 286–298. [Google Scholar] [CrossRef]
- Čartolovni, A.; Stolt, M.; Scott, P.A.; Suhonen, R. Moral injury in healthcare professionals: A scoping review and discussion. Nurs. Ethics 2021, 28, 590–602. [Google Scholar] [CrossRef]
- Shale, S. Moral injury and the COVID-19 pandemic: Reframing what it is, who it affects and how care leaders can manage it. BMJ 2020, 4, 224–227. [Google Scholar] [CrossRef]
- Kälvemark, S.; Höglund, A.T.; Hansson, M.G.; Westerholm, P.; Arnetz, B. Living with conflicts-ethical dilemmas and moral distress in the health care system. Soc. Sci. Med. 2004, 58, 1075–1084. [Google Scholar] [CrossRef]
- Corley, M.C. Nurse moral distress: A proposed theory and research agenda. Nurs. Ethics 2002, 9, 636–650. [Google Scholar] [CrossRef] [PubMed]
- Lamiani, G.; Borghi, L.; Argentero, P. When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. J. Health Psychol. 2016, 22, 51–67. [Google Scholar] [CrossRef] [PubMed]
- Nathaniel, A.K. Moral reckoning in nursing. West J. Nurs. Res. 2006, 28, 419–438. [Google Scholar] [CrossRef] [PubMed]
- Akram, F. Moral injury and the COVID-19 pandemic: A philosophical viewpoint. Ethics Med. Public Health 2021, 18, 100661. [Google Scholar] [CrossRef] [PubMed]
- Anderson-Shaw, L.K.; Zar, F.A. COVID-19, moral conflict, distress, and dying alone. J. Bioeth. Inq. 2020, 17, 777–782. [Google Scholar] [CrossRef]
- Nelson, K.E.; Hanson, G.C.; Boyce, D.; Ley, C.D.; Swavely, D.; Reina, M.; Rushton, C.H. Organizational Impact on Healthcare Workers’ Moral Injury During COVID-19. J. Nurs. Adm. 2022, 52, 57–66. [Google Scholar] [CrossRef]
- Maftei, A.; Holman, A. The prevalence of exposure to potentially morally injurious events among physicians during the COVID-19 pandemic. Eur. J. Psychotraumatol. 2021, 12, 1898791. [Google Scholar] [CrossRef]
- Nikbakht Nasrabadi, A.; Wibisono, A.H.; Allen, K.-A.; Yaghoobzadeh, A.; Bit-Lian, Y. Exploring the experiences of nurses’ moral distress in long-term care of older adults: A phenomenological study. BMC Nurs. 2021, 20, 1–156. [Google Scholar] [CrossRef]
- Spenceley, S.; Witcher, C.S.; Hagen, B.; Hall, B.; Kardolus-Wilson, A. Sources of moral distress for nursing staff providing care to residents with dementia. Dementia 2015, 16, 815–834. [Google Scholar] [CrossRef]
- Pijl-Zieber, E.M.; Awosoga, O.; Spenceley, S.; Hagen, B.; Hall, B.; Lapins, J. Caring in the wake of the rising tide: Moral distress in residential nursing care of people living with dementia. Dementia 2016, 17, 315–336. [Google Scholar] [CrossRef] [PubMed]
- de Veer, A.J.E.; Francke, A.L.; Struijs, A.; Willems, D.L. Determinants of moral distress in daily nursing practice: A cross sectional correlational questionnaire survey. Int. J. Nurs. Stud. 2013, 50, 100–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Preshaw, D.H.; Brazil, K.; McLaughlin, D.; Frolic, A. Ethical issues experienced by healthcare workers in nursing homes. Nurs. Ethics 2016, 23, 490–506. [Google Scholar] [CrossRef] [PubMed]
- Young, A.; Froggatt, K.; Brearley, S.G. ‘Powerlessness’ or ‘doing the right thing’—Moral distress among nursing home staff caring for residents at the end of life: An interpretive descriptive study. Palliat Med. 2017, 31, 853–860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brady, C.; Fenton, C.; Loughran, O.; Hayes, B.; Hennessy, M.; Higgins, A.; Leroi, I.; Shanagher, D.; McLoughlin, D.M. Nursing home staff mental health during the COVID-19 pandemic in the Republic of Ireland. Int. J. Geriatr. Psychiatry 2021, 16, 815–834. [Google Scholar] [CrossRef] [PubMed]
- Riello, M.; Purgato, M.; Bove, C.; MacTaggart, D.; Rusconi, E. Prevalence of post-traumatic symptomatology and anxiety among residential nursing and care home workers following the first COVID-19 outbreak in northern Italy. R. Soc. Open Sci. 2020, 7, 200880. [Google Scholar] [CrossRef]
- Greason, M. Ethical reasoning and moral distress in social care among long-term care staff. J. Bioeth. Inq. 2020, 17, 283–295. [Google Scholar] [CrossRef]
- Bettany-Saltikov, J.; Mcsherry, R. How to Do a Systematic Literature Review in Nursing: A Step-by-Step Guide, 2nd ed.; Open University Press: London, UK, 2016. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons Ltd.: Newark, DE, USA, 2019; Available online: https://library.biblioboard.com/viewer/21e7ce06-c562-40bb-b5d9-d6ef1dbe99e1 (accessed on 20 July 2022).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, 78–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Booth, A. Clear and present questions: Formulating questions for evidence based practice. Library Hi Tech 2006, 24, 355–368. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 3, 89. [Google Scholar] [CrossRef]
- Lockwood, C.; Munn, Z.; Porritt, K. Qualitative research synthesis: Methodological guidance for systematic reviewers utilizing meta-aggregation. Int. J. Evid. Based Healthc. 2015, 13, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Hannes, K.; Lockwood, C.; Pearson, A. A comparative analysis of three online appraisal instruments’ ability to assess validity in qualitative research. Qual. Health Res. 2010, 20, 1736–1743. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting systematic reviews of association (etiology). Int. J. Evid. Based Healthc. 2015, 13, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Moola, S.; Lisy, K.; Riitano, D.; Tufanaru, C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int. J. Evid. Based Healthc. 2015, 13, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Wang, Y.; Yang, Z.; Huang, D.; Weng, H.; Zeng, X. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef] [Green Version]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Improving the content validity of the mixed methods appraisal tool: A modified e-delphi study. J. Clin. Epidemiol. 2019, 111, 49–59. [Google Scholar] [CrossRef] [Green Version]
- Pace, R.; Pluye, P.; Bartlett, G.; Macaulay, A.C.; Salsberg, J.; Jagosh, J.; Seller, R. Testing the reliability and efficiency of the pilot mixed methods appraisal tool (MMAT) for systematic mixed studies review. Int. J. Nurs. Stud. 2012, 49, 47–53. [Google Scholar] [CrossRef]
- Lizarondo, L.; Stern, C.; Carrier, J.; Godfrey, C.; Rieger, K.; Salmond, S.; Apostolo, J.; Kirkpatrick, P.; Loveday, H. Chapter 8: Mixed methods systematic reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; University of Adelaide: Adelaide, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 10 January 2022).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Burnard, P. A method of analysing interview transcripts in qualitative research. Nurse Educ. Today 1991, 11, 461–466. [Google Scholar] [CrossRef]
- Blanco-Donoso, L.M.; Moreno-Jimenez, J.; Amutio, A.; Gallego-Alberto, L.; Moreno-Jimenez, B.; Garrosa, E. Stressors, job resources, fear of contagion, and secondary traumatic stress among nursing home workers in face of the COVID-19: The case of spain. J. Appl. Gerontol. 2021, 40, 244–256. [Google Scholar] [CrossRef]
- Kaelen, S.; van den Boogaard, W.; Pellecchia, U.; Spiers, S.; De Cramer, C.; Demaegd, G.; Fouqueray, E.; Van den Bergh, R.; Goublomme, S.; Decroo, T.; et al. How to bring residents’ psychosocial well-being to the heart of the fight against COVID-19 in Belgian nursing homes—A qualitative study. PLoS ONE 2021, 16, e0249098. [Google Scholar] [CrossRef] [PubMed]
- Nyashanu, M.; Pfende, F.; Ekpenyong, M.S. Triggers of mental health problems among frontline healthcare workers during the COVID-19 pandemic in private care homes and domiciliary care agencies: Lived experiences of care workers in the Midlands region, UK. Health Soc. Care Community 2020, 30, e370–e376. [Google Scholar] [CrossRef] [PubMed]
- Sarabia-Cobo, C.; Perez, V.; de Lorena, P.; Hermosilla-Grijalbo, C.; Saenz-Jalon, M.; Fernandez-Rodriguez, A.; Alconero-Camarero, A.R. Experiences of geriatric nurses in nursing home settings across four countries in the face of the COVID-19 pandemic. J. Adv. Nurs. 2021, 77, 869–878. [Google Scholar] [CrossRef]
- Zhao, S.; Yin, P.; Xiao, L.D.; Wu, S.; Li, M.; Yang, X.; Zhang, D.; Liao, L.; Feng, H. Nursing home staff perceptions of challenges and coping strategies during COVID-19 pandemic in china. Geriatr. Nurs. 2021, 42, 887–893. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Donoso, L.M.; Moreno-Jimenez, J.; Gallego-Alberto, L.; Amutio, A.; Moreno-Jimenez, B.; Garrosa, E. Satisfied as professionals, but also exhausted and worried!!: The role of job demands, resources and emotional experiences of spanish nursing home workers during the COVID-19 pandemic. Health Soc. Care Community 2021, 30, E148–E160. [Google Scholar] [CrossRef] [PubMed]
- Krzyzaniak, N.; Mae Scott, A.; Bakhit, M.; Bryant, A.; Taylor, M.; Del Mar, C. Impact of the COVID-19 pandemic on the Australian residential aged care facility (RACF) workforce. Aust. J. Adv. Nurs. 2021, 38, 370–376. [Google Scholar] [CrossRef]
- Thompson, D.-C.; Barbu, M.-G.; Beiu, C.; Popa, L.G.; Mihai, M.M.; Berteanu, M.; Popescu, M.N. The Impact of COVID-19 Pandemic on Long-Term Care Facilities Worldwide: An Overview on International Issues. BioMed Res. Int. 2020, 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T. How to Read a Paper, 6th ed.; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2019. [Google Scholar]
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing Mental Health Challenges Faced by Healthcare Workers during COVID-19 Pandemic. BMJ 2020, 369, m1211. [Google Scholar] [CrossRef] [Green Version]
- Porter, B.; Zile, A.; Peryer, G.; Farquhar, M.; Sanderson, K. The impact of providing end-of-life care during a pandemic on the mental health and wellbeing of health and social care staff: Systematic review and meta-synthesis. Soc. Sci. Med. 2021, 287, 114397. [Google Scholar] [CrossRef]
- Giebel, C.; Hanna, K.; Cannon, J.; Shenton, J.; Mason, S.; Tetlow, H.; Marlow, P.; Rajagopal, M.; Gabbay, M. Taking the ‘care’ out of care homes: The moral dilemma of institutional long-term care provision during COVID-19. Health Soc. Care Community 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
| SPICE Framework | SPICE Formulation for Review |
|---|---|
| Setting | Geriatric residential care settings (e.g., nursing and care homes) |
| Population | Residential care home staff (e.g., healthcare professionals and ancillary workers) |
| Interest | Moral injury (MI) and moral distress (MD) during COVID-19 |
| Comparison | Not relevant to review question |
| Evaluation | General experience of (including prevalence, predictors, and psychological impact) |
| Column Terms Combined with | Setting | Perspective/Population | Interest | Evaluation |
|---|---|---|---|---|
| AND | AND | AND | AND | |
| OR | Care home* | Staff* | Moral injur* | COVID* |
| OR | Nursing home* | Worker* | Morally injur* | Covid-19* |
| OR | Residential home* | Employee* | Moral distress* | Covid outbreak |
| OR | Residential care* | Member* | Morally distress* | Covid pandemic |
| OR | Retirement home* | Healthcare professional* | Moral* pain* | Cov-19* |
| OR | Convalescent home* | Healthcare support* | Moral dilemma* | 2019-ncov |
| OR | Senior citizen* home* | Healthcare work* | Moral transgres* | Sars-cov-2* |
| OR | Senior* home* | Healthcare assis* | Moral* challeng* | Coronavirus* |
| OR | Rest home* | Healthcare support* | Moral* concern* | 2020 Pandemic* |
| OR | Supported living* | Support work* | Moral* conflict* | |
| OR | Assisted living* | Nurse* | Moral agenc* | |
| OR | Hospice* | Care work* | Moral identit* | |
| OR | Palliative care* | Carer* | Moral* difficult* | |
| OR | Aged care* | Care assis* | Moral obligation* | |
| OR | Elderly*care* | Doctor* | Moral suffer* | |
| OR | Geriatric* | Medic* | Moral resilien* | |
| OR | End of life* care* | Allied health professional* | Ethical* concern* | |
| OR | End-of-life* care* | HCA* | Ethical dilemma* | |
| OR | Retirement facilit* | HCSW* | Ethical* difficult* | |
| OR | Residential setting* | Therapis* | Ethical transgress* | |
| OR | Older adult* | Manager* | Post-Traumatic Embitterment Disorder* | |
| OR | Admin* | PTED | ||
| OR | Clerica* | Potentially morally injurious event* | ||
| OR | Personal assis* | PMIE* | ||
| OR | PA* | Moral Consequence* | ||
| OR | Cleaner* | Moral repair* | ||
| OR | Cleaning staff* | |||
| OR | Non-clinical* | |||
| OR | Ancillary* | |||
| OR | Housekeep* |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Residential care settings for older adults (e.g., N&CH or assisted-living facilities) | Non-residential care settings or residential care settings for demographics not including older people (e.g., hospital settings or care home for young people) |
| N&CH staff (studies which involve N&CH, as well as other populations, are included) | Other populations with no indicated participation from nursing home staff (e.g., patients, families, etc.) |
| MI or MD (will include studies where MI is not explicitly stated but is implicitly implied, e.g., “ethical dilemma”) | Mental health difficulties, with no indication of MI or MD (i.e., MI/MD is not implicitly implied or explicitly stated) |
| COVID-19 pandemic | MI and MD outside of COVID-19 or during other disease outbreaks (e.g., Ebola) |
| Peer-reviewed journal articles | Not peer-reviewed |
| Qualitative, quantitative, and mixed-methods original studies | Editorials, commentaries, symposiums, reviews, gray literature, book chapters |
| Published in English language | Published in languages other than English |
| Publication date: 30 January 2020 to 3 January 2022 | Publication date before 30 January 2020 |
| Authors and Date | Study Design and Type | Population Characteristics | Setting | Aim(s) and Methods | Main Findings | |
|---|---|---|---|---|---|---|
| Blanco-Donoso et al. (2021a) [51] | Mixed-methods, cross-sectional survey design | Sample Size: n = 335. Population: N&CH staff. Mean Age: 36.12 years (SD = 10.26). Gender: 269 females, and 66 males. | N&CH Roles: 183 health and social care staff, 135 support staff, 5 center managers, and 12 unspecified roles. | Spanish N&CHs across 43 provinces | Main Aim(s):
Snowball sampling. Data Collection:
| Quantitative Findings:
|
| Blanco-Donoso et al. (2021b) [46] | Quantitative, cross-sectional survey design | Sample Size: N = 228. Population: N&CH workers. Mean Age: 26.29 (SD = 10.04). Gender: 183 females and45 males. | N&CH Roles: 15 doctors, 38 nurses, 44 nurse aides, 10 geriatric assistants, 19 social workers, 9 psychologists, 8 OT 5 physiotherapists, 2 management of center, and 79 unspecified roles. | N&CHs across 42 Spanish provinces | Main Aim(s):
Snowball sampling. Data Collection:
| Quantitative Findings Relevant to Review:
|
| Brady et al. (2021) [28] | Quantitative, cross-sectional survey design | Sample Size: N = 390. Population: N&CH staff. Age: ≤30 years, 85 (21.8%); 31–50 years, 187 (47.9%); and ≥51 years, 118 (30.3%). Gender: 337 females, 50 males, and 3 other/prefer not to say. | N&CH Roles: 120 nurses, 172 HCAs, and 98 non- clinical staff. | NHI affiliated N&CHs in Republic of Ireland | Main Aim(s):
Purposive and convenience sampling. Data Collection:
| Quantitative Findings Relevant to Review:
mean = 5.9 (SD = 3.0);
mean = 7.9 (SD = 4.8);
subscale (p = 0.030, adjusted p = 0.048);
|
| Kaelen et al. (2021) [47] | Qualitative, general qualitative inquiry | Sample Size: N = 44. Population: 8 N&CH staff groups. Mean Age: Not published. Gender: 38 females and 6 males. | N&CH Roles: 10 nurses, 17 nurse aids, 9 OTs or physical therapists, and 8 non-clinical support staff. | 8 Belgium N&CHs | Main Aim(s): To explore how staff perceived and experienced preparedness for addressing psychosocial and metal health needs of residents. Sampling Method: Purposive and convenience sampling. Data Collection: Focus group with N&CH staff.Analyses: Thematic content analysis. | Major Themes:
|
| Krzyzaniak et al. (2021) [52] | Mixed-methods survey design | Sample Size: Varies between each completed survey; N = 335–371. Population: Residential aged care facility (RACF) staff. Age Range: 20–73 years (mean age not published). Gender: Female, 320 (87%); male, 48 (13%); and other, 1 (0.3%). | N&CH Roles: 160 nurses, 16 nursing assistants, 10 other care assistants, 12 allied health professionals, 131 administrative personnel, 35 quality-and-compliance staff, 1 cleaning staff, and 1 kitchen staff. | Australian RACF | Main Aim(s): To understand the impact of the COVID-19 pandemic on the RACF workforce, including clinical, administrative, and auxiliary staff. Recruitment Method: Convenience sampling Data Collection: Adapted online survey with open-ended and closed questions about preparedness for the pandemic, information flow, PPE, management of COVID cases, visitor restriction, and other impacts on RACF staff. Quantitative Analyses Chi-square. Qualitative Analysis: Content analysis. | Quantitative:
|
| Nyashanu et al. (2020) [48] | Qualitative, exploratory qualitative approach (EQA) | Sample Size: N = 40 (N&CH staff = 20). Population: N&CH staff and domiciliary care workers. Age Range: 25–55+ years. Gender: 20 female and 10 male. | N&CH Roles: Not published/unspecified. | Private N&CHs and domiciliary care in West Midlands, UK | Main Aim(s):To explore triggers of mental health problems among frontline healthcare professionals. Recruitment Method: Convenience sampling. Data Collection: Semi-structured interviews. Analyses: Thematic analysis and interpretive phenomenological analysis (IPA). | Major Themes:
|
| Sarabia-Cobo et al. (2020) [49] | Qualitative, phenomenological design | Sample Size: N = 24. Population: Registered nurses in N&CHs. Mean Age: 31.2 years (SD = 4.28). Gender: 24 female. | N&CH Roles: 24 registered nurses. | 14 N&CHs across Spain, Italy, Peru, and Mexico | Main Aim(s):
Purposive and snowball sampling. Data Collection: In-depth semi-structured interviews. Analyses: Inductive content analysis. | Major Themes:
|
| Zhao et al. (2021) [50] | Qualitative, descriptive design | Sample Size: N = 21. Population: N&CH nursing staff. Mean Age: 42.7 years. Gender: 21 females. | N&CH Roles: 7 nurse managers, 7 registered nurses, and 7 nursing assistants | 7 N&CHs across China’s Hunan Province | Main Aim(s): To identify challenges faced by N&CH staff during the COVID-19 pandemic. Recruitment Method: Purposive sampling. Data Collection: In-depth semi-structured interviews. Analyses: Thematic analysis. | Major themes:
|
| JBI Critical Appraisal Checklist for Analytical Cross-Sectional and Prevalence Studies (2020) [38,39] | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Author(s) and Date | Inclusion Criteria in Sample Clearly Defined? | Study Participants Sampled in Appropriate Way? | Sample Size and Frame Adequate? | Study Subjects and Setting Described in Detail? | Exposure Measured in Valid and Reliable Way? | Objective, Standard Criteria Used for Measurement of Condition? | Confounding Factors Identified? Strategies to Deal with Them Stated? | Outcomes Measured in a Valid and Reliable Way? | Appropriate Statistical Analysis Used? | Response rate Adequate/Managed Appropriately? |
| Blanco-Donoso et al. (2021b) [46] | Y | Y | U | Y | Y | Y | N | Y | Y | U |
| Brady et al. (2021) [28] | Y | Y | N | Y | Y | Y | N | Y | Y | U |
| JBI Critical Appraisal Checklist for Qualitative Research (2020)[36] | ||||||||||
| Author(s) and Date | Congruity between stated Philosophical perspective and research methodology? | Congruity between research methodology and research question? | Congruity between research methodology and data collection methods? | Congruity between research methodology and representation and analysis of data? | Congruity between research methodology and interpretation of results? | Statement locating researcher culturally or theoretically? | Influence of researcher on research and vice versa addressed? | Participants and their voices adequately represented? | Research ethical? Evidence of ethical approval? | Do conclusions drawn report flow from analysis/interpretation data? |
| Kaelen et al. (2021) [47] | U | Y | Y | Y | Y | N | N | Y | Y | Y |
| Nyashanu et al. (2020) [48] | U | Y | Y | Y | Y | N | N | Y | Y | Y |
| Sarabia-Cobo et al. (2020) [49] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Zhao et al. (2021) [50] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y |
| Mixed-Methods Appraisal Tool (MMAT) Version 2018[41] | ||||||||||
| Author(s) and Date | Clear research questions? | Do collected data allow us to address research questions? | Adequate rationale for using mixed-methods design to address research question? | Different components of study effectively integrated to answer research question? | Outputs of the integration of qual and quant components adequately interpreted? | Divergences and inconsistencies between quant and qual results adequately addressed? | Different components of study adhere to quality criteria of each method tradition? | |||
| Blanco-Donoso et al. (2021a) [51] | Y | Y | U | Y | Y | Y | Y | |||
| Krzyzaniak et al. (2021) [52] | Y | Y | U | N | U | U | N | |||
| Superordinate Themes | Subtheme (s) | Author (s) and Date | |||||
|---|---|---|---|---|---|---|---|
| Blanco-Donoso et al. (2021a) [51] | Kaelen et al. (2021) [47] | Krzyzaniak et al. (2021) [52] | Nyashanu et al. (2020) [48] | Sarabia-Cobo et al. (2020) [49] | Zhao et al. (2021) [50] | ||
| Resource Deficits | Material Resource Deficits | √ | √ | √ | √ | √ | √ |
| Time Related Issues | √ | × | √ | × | √ | × | |
| Inadequate Staffing Levels | √ | √ | √ | √ | √ | √ | |
| Experience and Knowledge Deficit | √ | × | × | √ | √ | √ | |
| Role Challenges | Change in Role and Demands | √ | √ | √ | × | × | √ |
| Conflicting Principles and Decision-Making | × | √ | √ | √ | √ | √ | |
| Communication and Leadership | Feeling Undervalued, Abandoned, or Betrayed | √ | × | √ | √ | √ | × |
| Inadequate Guidance and Incoherent Information | √ | √ | √ | √ | √ | × | |
| Concerns before COVID-19 | √ | × | √ | × | √ | × | |
| Emotional and Psychosocial Consequences | Emotional Responses | √ | √ | √ | √ | √ | √ |
| Fear of Contagion | √ | × | √ | √ | √ | ||
| Grief and Loss | √ | × | √ | √ | √ | × | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laher, Z.; Robertson, N.; Harrad-Hyde, F.; Jones, C.R. Prevalence, Predictors, and Experience of Moral Suffering in Nursing and Care Home Staff during the COVID-19 Pandemic: A Mixed-Methods Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9593. https://doi.org/10.3390/ijerph19159593
Laher Z, Robertson N, Harrad-Hyde F, Jones CR. Prevalence, Predictors, and Experience of Moral Suffering in Nursing and Care Home Staff during the COVID-19 Pandemic: A Mixed-Methods Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(15):9593. https://doi.org/10.3390/ijerph19159593
Chicago/Turabian StyleLaher, Zainab, Noelle Robertson, Fawn Harrad-Hyde, and Ceri R. Jones. 2022. "Prevalence, Predictors, and Experience of Moral Suffering in Nursing and Care Home Staff during the COVID-19 Pandemic: A Mixed-Methods Systematic Review" International Journal of Environmental Research and Public Health 19, no. 15: 9593. https://doi.org/10.3390/ijerph19159593
APA StyleLaher, Z., Robertson, N., Harrad-Hyde, F., & Jones, C. R. (2022). Prevalence, Predictors, and Experience of Moral Suffering in Nursing and Care Home Staff during the COVID-19 Pandemic: A Mixed-Methods Systematic Review. International Journal of Environmental Research and Public Health, 19(15), 9593. https://doi.org/10.3390/ijerph19159593






