The North Italian Longitudinal Study Assessing the Mental Health Effects of SARS-CoV-2 Pandemic Health Care Workers—Part II: Structural Validity of Scales Assessing Mental Health
Abstract
:1. Introduction
2. Materials and Methods
2.1. Measurement Instruments
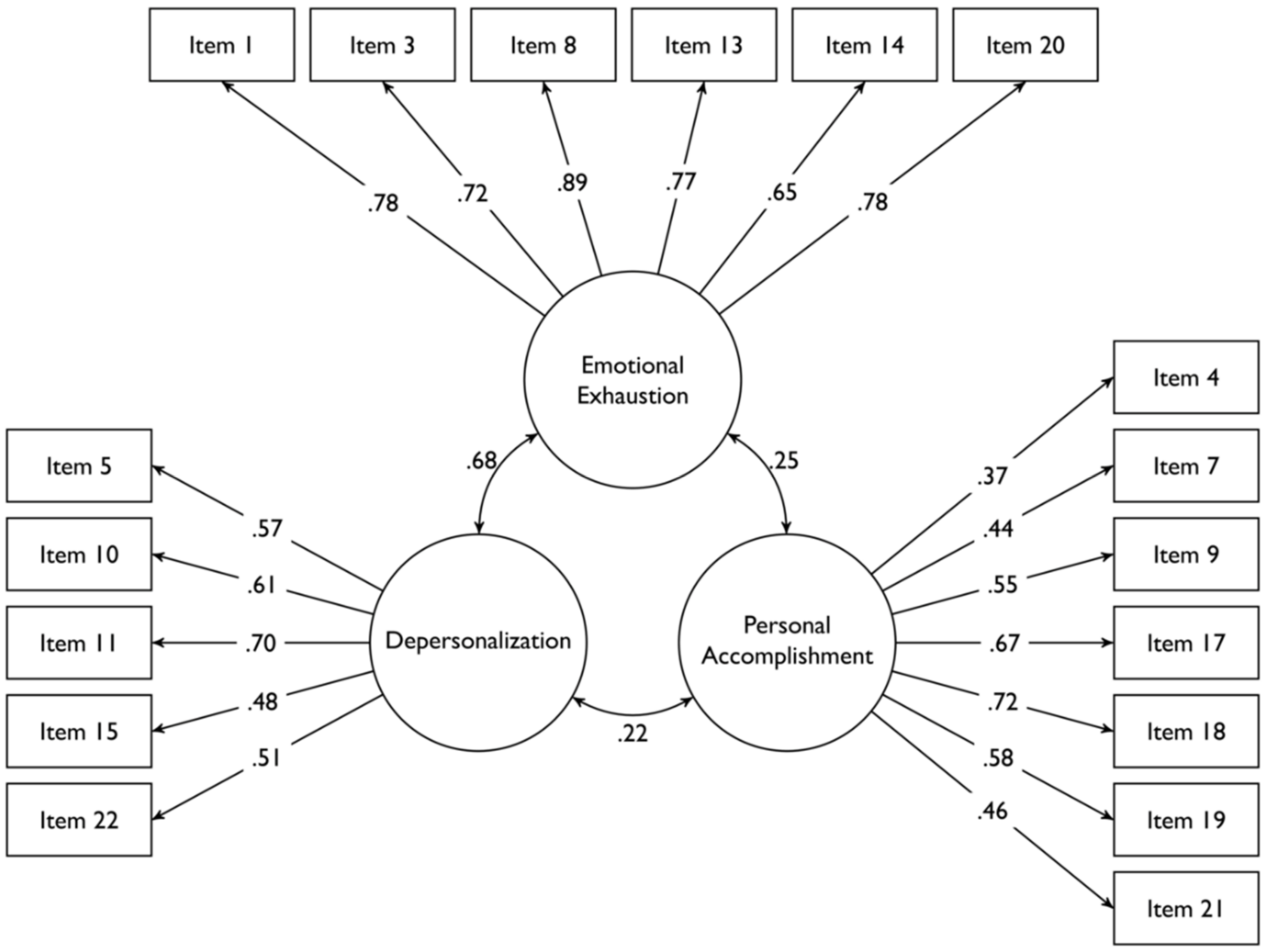
- Maslach Burnout Inventory (MBI) [24]. The MBI is a self-report questionnaire which assesses the three theoretical components of burnout, i.e., emotional exhaustion, depersonalization and personal accomplishment. It is composed of 22 Likert-type items assessing the frequency of feelings or attitudes reflecting the three components of burnout on a scale ranging from 0 (“never”) to 6 (“every day”). Higher scores in the emotional exhaustion and depersonalization scales reflect higher levels of burnout, whereas higher scores in the personal accomplishment subscale reflect lower levels of burnout. Reviews on the psychometric properties of the MBI showed that this measurement instruments has adequate construct validity and internal consistency [25]. The Italian translation of the MBI was found to reflect the same three-factor structure as the original version and showed adequate internal consistency [26].
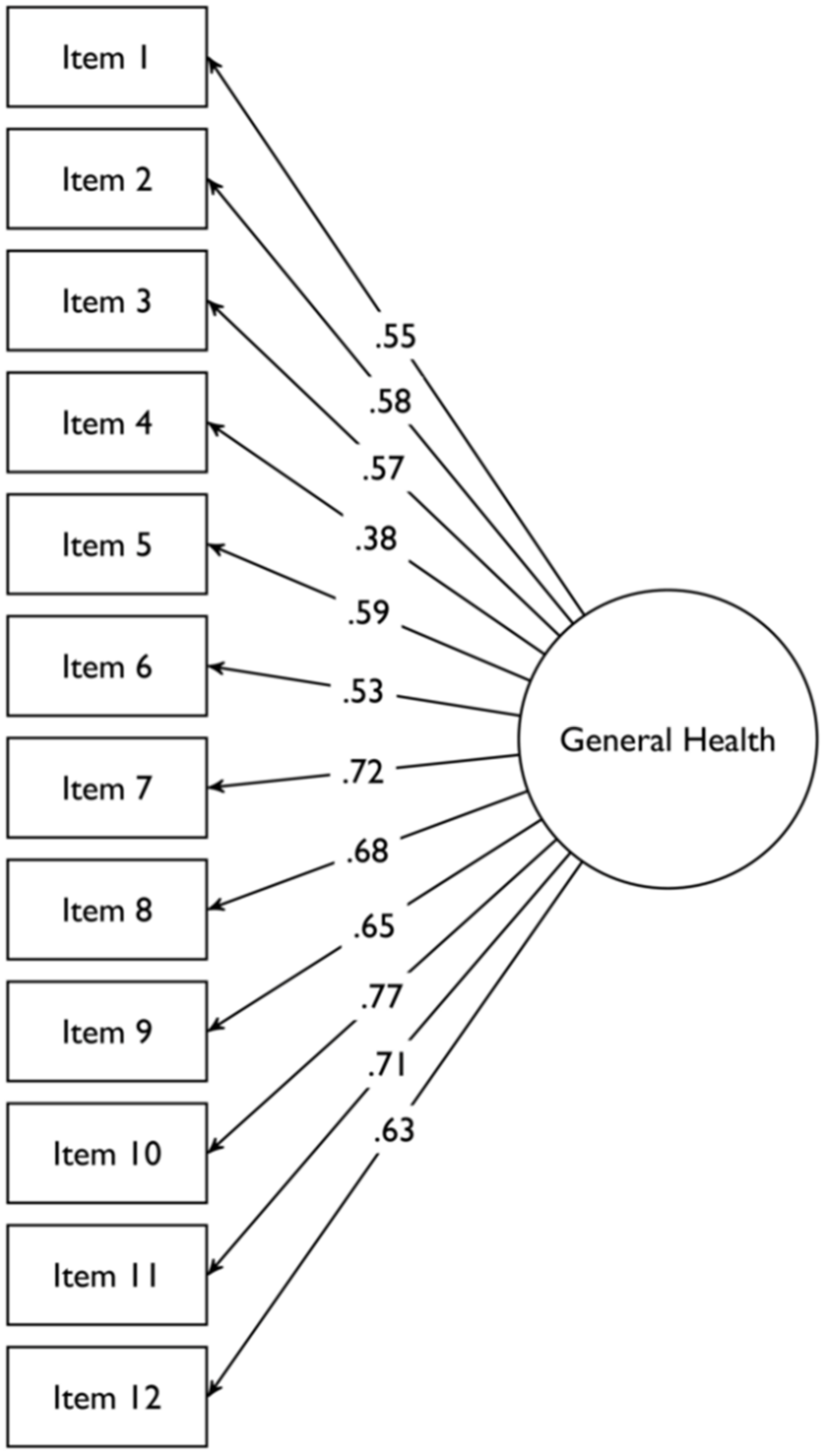
- General Health Questionnaire-12 (GHQ-12) [27]. The GHQ-12 is a self-report questionnaire originally developed for use in consulting settings to detect individuals with psychiatric disorders, whose 12-items version is an extensively used general measure of mental well-being. The GHQ-12 items assess the severity of a mental problem over the past two weeks using a 4-point Likert scale ranging from 0 (“less than usual”) to 3 (“much more than usual”). Higher scores indicate worse mental well-being. The factor structure of the GHQ-12 is debated, since unidimensional and multidimensional structures have been proposed [28,29,30]. However, it has been recognized that the retrieval of multiple dimensions is related to a wording effect rather than the presence of true distinct latent factors, since half of the GHQ-12 items have a positive wording and half a negative wording [31]. The Italian version of the GHQ-12 showed acceptable test–retest reliability [32].
- The PTSD Checklist for DSM-5-Short Form (PCL-5-SF) [33]. The PCL-5-SF is a 5-item version of the original 20-item PCL-5 questionnaire, which is a self-report measure assessing the frequency of the DSM-5 symptoms of PTSD in the past month using a Likert scale ranging from 1 (“Not at all”) to 5 (“extremely”). Higher scores indicate higher frequency of PTSD symptoms. The Italian version of this questionnaire has shown adequate construct validity, criterion validity and internal consistency [34].
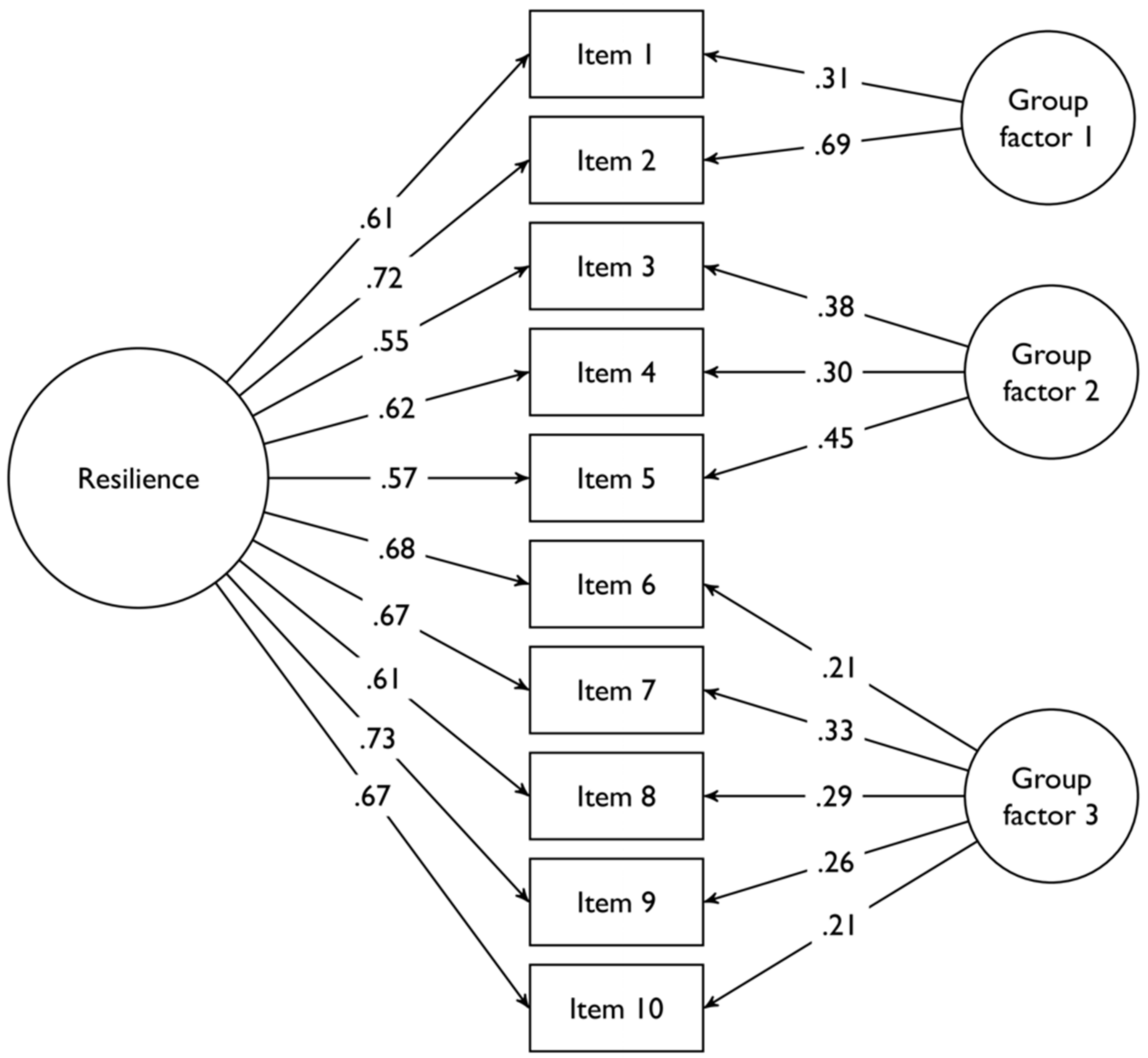
- The Connor-Davidson Resilience Scale-10 item version (CD-RISC-10) [35]. The CD-RISC-10 is a self-report questionnaire assessing resilience based on the Connor and Davidson definition, i.e., the ability to thrive in the face of adversity [35]. In this study, we employed the 10-item version. The items are scored using Likert scale ranging from 0 (“not true at all”) to 4 (“true nearly all the time”). Higher scores indicate higher levels of resilience. The Italian version of the CD-RISC-10 has shown adequate internal consistency and concurrent validity [36].
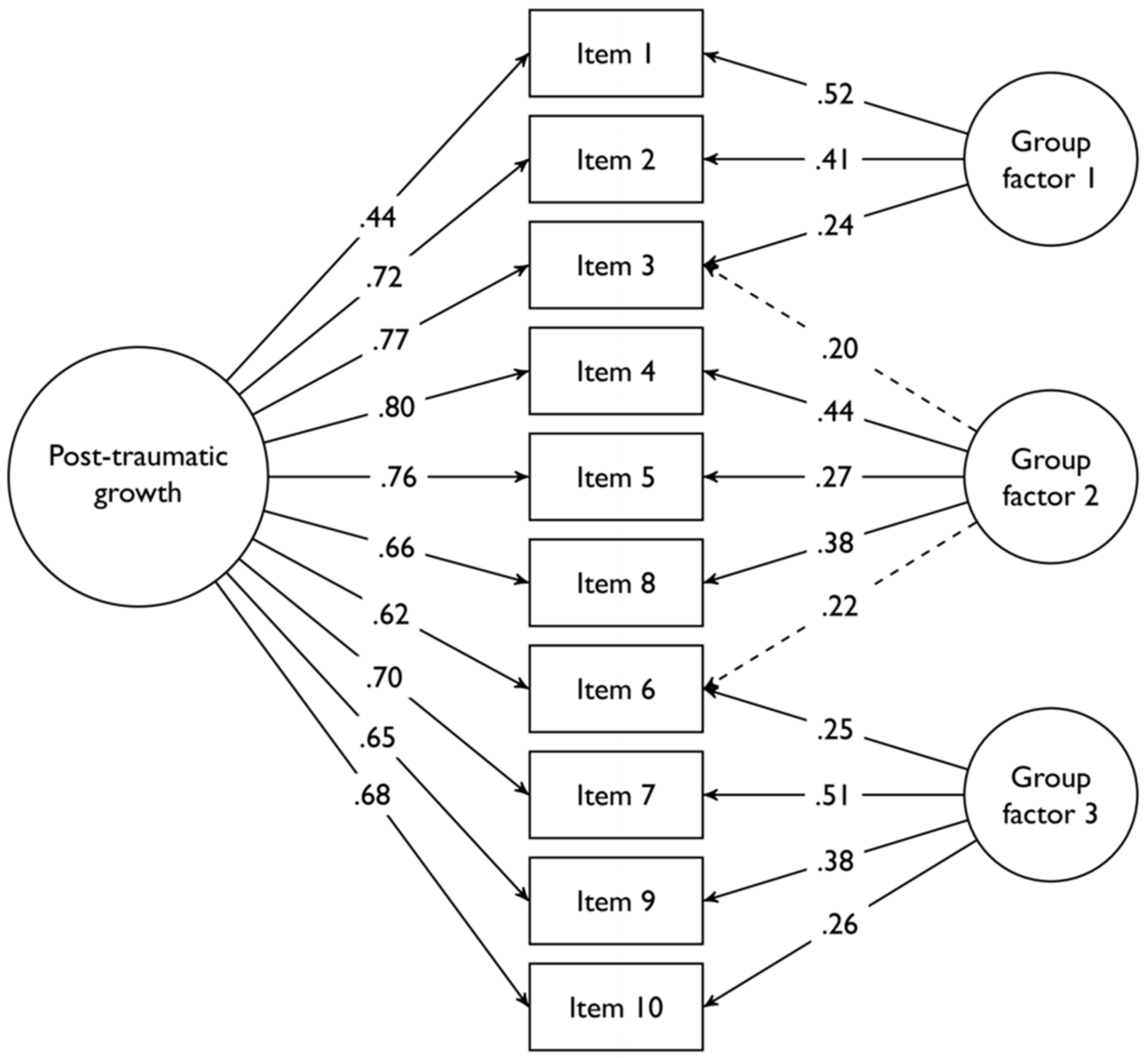
- The Post-Traumatic Growth Inventory-Short Form (PTGI-SF) [37]. The PTGI-SF is a self-rated questionnaire assessing positive outcomes reported by people who have experienced traumatic events. In this study we employed the 10-item version of this scale. The items are scored on a 6-point Likert scale ranging from 0 (“I did not experience this change as a result of my crisis”) to 5 (“I experienced this change to a very great degree as a result of my crisis”). Higher scores indicate higher levels of post-traumatic growth. The Italian version of the PTGI-SF has shown adequate internal consistency [38].
2.2. Statistical Analyses
2.2.1. Preliminary Analyses
2.2.2. Confirmatory Factor Analyses
2.2.3. Confirmatory Factor Analyses and Measurement Invariance of the Maslach Burnout Inventory
2.2.4. Factor Analyses of the GHQ-12, of the PCL-5-SF, of the PTGI-SF and of the CD-RISC-10 Scale
3. Results
3.1. Missing Data Analysis
3.2. Confirmatory Factor Analysis and Internal Consistency of the Maslach Burnout Inventory
3.3. Longitudinal Measurement Invariance of the Refined Version of the Maslach Burnout Inventory
3.4. Factor Analysis and Internal Consistency of the General Health Questionnaire-12, of the PCL-5-SF, of the Post-Traumatic Growth Inventory and of the Connor-Davidson Resilience Scale
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
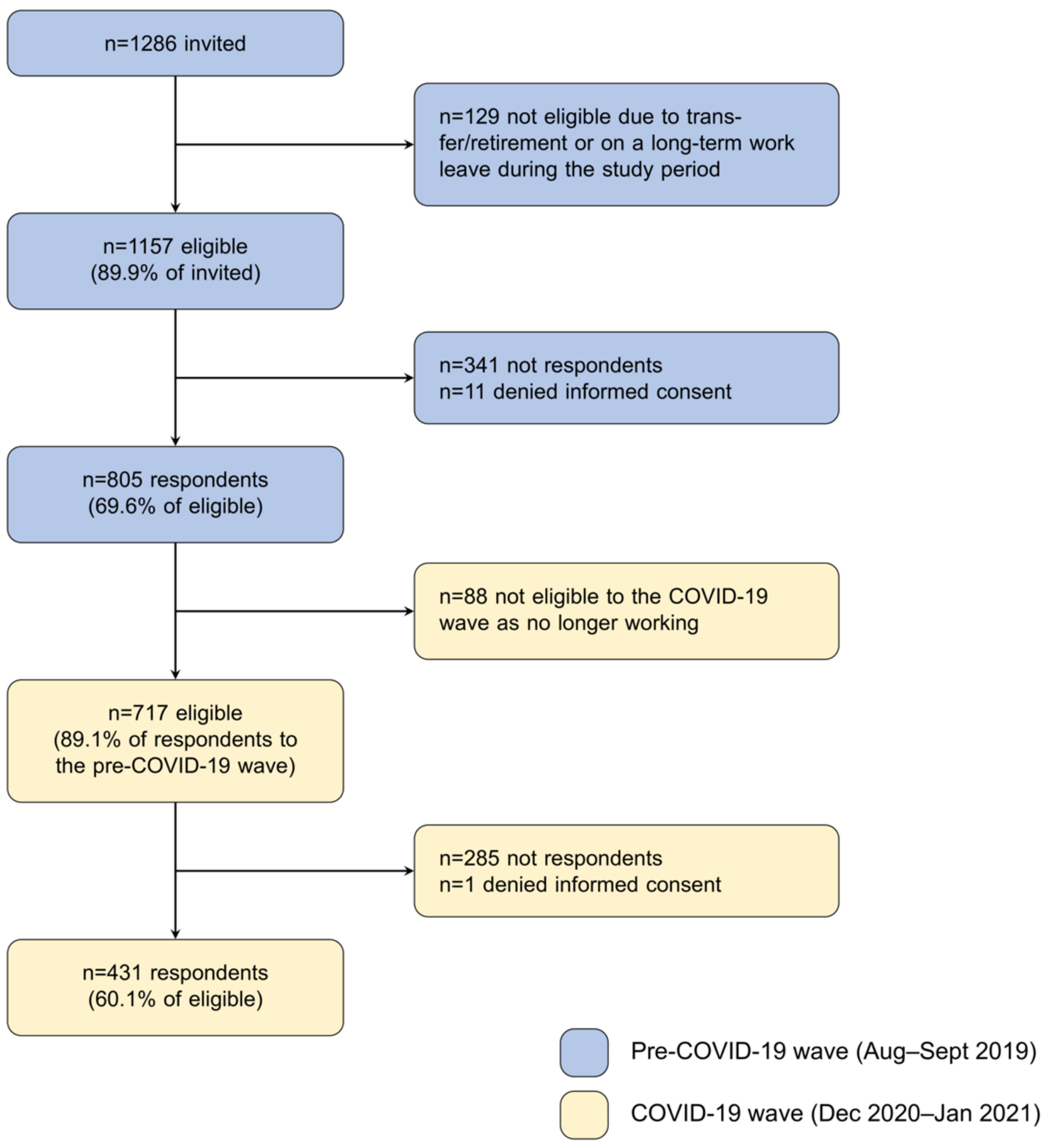
- Flowchart of the study participants
- 2.
- Representations of the factor structures of the questionnaires assessed in the study
References
- Johnson, J.; Hall, L.H.; Berzins, K.; Baker, J.; Melling, K.; Thompson, C. Mental Healthcare Staff Well-Being and Burnout: A Narrative Review of Trends, Causes, Implications, and Recommendations for Future Interventions. Int. J. Mental. Health Nurs. 2018, 27, 20–32. [Google Scholar] [CrossRef]
- Santini, Z.I.; Becher, H.; Jørgensen, M.B.; Davidsen, M.; Nielsen, L.; Hinrichsen, C.; Madsen, K.R.; Meilstrup, C.; Koyanagi, A.; Stewart-Brown, S.; et al. Economics of Mental Well-Being: A Prospective Study Estimating Associated Health Care Costs and Sickness Benefit Transfers in Denmark. Eur. J. Health Econ. 2021, 22, 1053–1065. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Chesworth, B.; Franchino-Olsen, H.; Macy, R.J. A Scoping Review of Vicarious Trauma Interventions for Service Providers Working With People Who Have Experienced Traumatic Events. Trauma Violence Abus. 2021. [Google Scholar] [CrossRef]
- Weaver, M.D.; Vetter, C.; Rajaratnam, S.M.W.; O’Brien, C.S.; Qadri, S.; Benca, R.M.; Rogers, A.E.; Leary, E.B.; Walsh, J.K.; Czeisler, C.A.; et al. Sleep Disorders, Depression and Anxiety Are Associated with Adverse Safety Outcomes in Healthcare Workers: A Prospective Cohort Study. J. Sleep Res. 2018, 27, e12722. [Google Scholar] [CrossRef] [Green Version]
- Melnyk, B.M.; Orsolini, L.; Tan, A.; Arslanian-Engoren, C.; Melkus, G.D.; Dunbar-Jacob, J.; Rice, V.H.; Millan, A.; Dunbar, S.B.; Braun, L.T. A National Study Links Nurses’ Physical and Mental Health to Medical Errors and Perceived Worksite Wellness. J. Occup. Environ. Med. 2018, 60, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Woo, T.; Ho, R.; Tang, A.; Tam, W. Global Prevalence of Burnout Symptoms among Nurses: A Systematic Review and Meta-Analysis. J. Psychiatr. Res. 2020, 123, 9–20. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, K.; Neff, D.M.; Pitman, S. Burnout in Mental Health Professionals: A Systematic Review and Meta-Analysis of Prevalence and Determinants. Eur. Psych. 2018, 53, 74–99. [Google Scholar] [CrossRef] [PubMed]
- Denning, M.; Goh, E.T.; Tan, B.; Kanneganti, A.; Almonte, M.; Scott, A.; Martin, G.; Clarke, J.; Sounderajah, V.; Markar, S.; et al. Determinants of Burnout and Other Aspects of Psychological Well-Being in Healthcare Workers during the Covid-19 Pandemic: A Multinational Cross-Sectional Study. PLoS ONE 2021, 16, e0238666. [Google Scholar] [CrossRef]
- Bolcato, M.; Aurilio, M.T.; Aprile, A.; Di Mizio, G.; Della Pietra, B.; Feola, A. Take-Home Messages from the COVID-19 Pandemic: Strengths and Pitfalls of the Italian National Health Service from a Medico-Legal Point of View. Healthcare 2021, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Giusti, E.M.; Pedroli, E.; D’Aniello, G.E.; Stramba Badiale, C.; Pietrabissa, G.; Manna, C.; Stramba Badiale, M.; Riva, G.; Castelnuovo, G.; Molinari, E. The Psychological Impact of the COVID-19 Outbreak on Health Professionals: A Cross-Sectional Study. Front. Psychol. 2020, 11, 1684. [Google Scholar] [CrossRef] [PubMed]
- Kok, N.; van Gurp, J.; Teerenstra, S.; van der Hoeven, H.; Fuchs, M.; Hoedemaekers, C.; Zegers, M. Coronavirus Disease 2019 Immediately Increases Burnout Symptoms in ICU Professionals: A Longitudinal Cohort Study. Crit. Care Med. 2021, 49, 419–427. [Google Scholar] [CrossRef]
- Gomez, S.; Anderson, B.J.; Yu, H.; Gutsche, J.; Jablonski, J.; Martin, N.; Kerlin, M.P.; Mikkelsen, M.E. Benchmarking Critical Care Well-Being: Before and After the Coronavirus Disease 2019 Pandemic. Crit. Care Explor. 2020, 2, e0233. [Google Scholar] [CrossRef]
- Lluch, C.; Galiana, L.; Doménech, P.; Sansó, N. The Impact of the COVID-19 Pandemic on Burnout, Compassion Fatigue, and Compassion Satisfaction in Healthcare Personnel: A Systematic Review of the Literature Published during the First Year of the Pandemic. Healthcare 2022, 10, 364. [Google Scholar] [CrossRef]
- Ghahramani, S.; Lankarani, K.B.; Yousefi, M.; Heydari, K.; Shahabi, S.; Azmand, S. A Systematic Review and Meta-Analysis of Burnout Among Healthcare Workers During COVID-19. Front. Psychiatry 2021, 12, 758849. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Xu, Q.; Kuang, X.; Zhang, X.; Fang, F.; Gui, L.; Li, M.; Tefsen, B.; Zha, L.; Liu, H. Prevalence and Factors Associated with Post-Traumatic Stress Disorder in Healthcare Workers Exposed to COVID-19 in Wuhan, China: A Cross-Sectional Survey. BMC Psychiatry 2021, 21, 572. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, R.; Sikhosana, N.; Green, H.; Halcomb, E.J.; Middleton, R.; Alananzeh, I.; Trakis, S.; Moxham, L. Anxiety and Depression among Healthcare Workers during the COVID-19 Pandemic: A Systematic Umbrella Review of the Global Evidence. BMJ Open 2021, 11, e054528. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.E.; Harris, C.; Danielle, L.C.; Boland, P.; Doherty, A.J.; Benedetto, V.; Gita, B.E.; Clegg, A.J. The Prevalence of Mental Health Conditions in Healthcare Workers during and after a Pandemic: Systematic Review and Meta-Analysis. J. Adv. Nurs. 2022, 78, 1551–1573. [Google Scholar] [CrossRef]
- Feingold, J.H.; Hurtado, A.; Feder, A.; Peccoralo, L.; Southwick, S.M.; Ripp, J.; Pietrzak, R.H. Posttraumatic Growth among Health Care Workers on the Frontlines of the COVID-19 Pandemic. J. Affect. Disord. 2022, 296, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Li, W.-Q.; Yuan, P.; Sun, J.; Xu, M.-L.; Wang, Q.-X.; Ge, D.-D.; Jiang, M.-M.; Xing, L.-Q.; Du, W.-J.; Li, Q. Resilience, Coping Style, and COVID-19 Stress: Effects on the Quality of Life in Frontline Health Care Workers. Psychol. Health Med. 2022, 27, 312–324. [Google Scholar] [CrossRef]
- Putnick, D.L.; Bornstein, M.H. Measurement Invariance Conventions and Reporting: The State of the Art and Future Directions for Psychological Research. Dev. Rev. 2016, 41, 71–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Widaman, K.F.; Ferrer, E.; Conger, R.D. Factorial Invariance within Longitudinal Structural Equation Models: Measuring the Same Construct across Time. Child Dev. Perspect. 2010, 4, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Osofsky, J.D.; Osofsky, H.J.; Mamon, L.Y. Psychological and Social Impact of COVID-19. Psychol. Trauma 2020, 12, 468–469. [Google Scholar] [CrossRef] [PubMed]
- Veronesi, G.; Giusti, E.M.; D’Amato, A.; Gianfagna, F.; Borchini, R.; Castelnuovo, G.; Iacoviello, L.; Ferrario, M.M. The North Italian Longitudinal Study Assessing the Mental Health Effects of SARS-CoV-2 Pandemic on Health Care Workers—Part I: Study Design and Psychometric Structural Validity of the HSE Indicator Tool and Work Satisfaction Scale. Int. J. Environ. Res. Public Health 2022, 19, 9514. [Google Scholar]
- Maslach, C.; Jackson, S.E. The Measurement of Experienced Burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Shoman, Y.; Marca, S.C.; Bianchi, R.; Godderis, L.; van der Molen, H.F.; Guseva Canu, I. Psychometric Properties of Burnout Measures: A Systematic Review. Epidemiol. Psychiatr. Sci. 2021, 30, e8. [Google Scholar] [CrossRef]
- Sirigatti, S.; Stefanile, C. The Maslach Burnout Inventory: Adattamento e Taratura per l’Italia; Organizzazioni Speciali: Firenze, Italy, 1993. [Google Scholar]
- Goldberg, D.P.; Hillier, V.F. A Scaled Version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef]
- Graetz, B. Multidimensional Properties of the General Health Questionnaire. Soc. Psychiatry Psychiatr. Epidemiol. 1991, 26, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Werneke, U.; Goldberg, D.P.; Yalcin, I.; Ustün, B.T. The Stability of the Factor Structure of the General Health Questionnaire. Psychol. Med. 2000, 30, 823–829. [Google Scholar] [CrossRef]
- Goldberg, D.P. User’s Guide to the General Health Questionnaire; NFER-NELSON: Windsor, UK, 1988. [Google Scholar]
- Hankins, M. The Factor Structure of the Twelve Item General Health Questionnaire (GHQ-12): The Result of Negative Phrasing? Clin. Pract. Epidemiol. Mental Health 2008, 4, 10. [Google Scholar] [CrossRef] [Green Version]
- Piccinelli, M.; Bisoffi, G.; Bon, M.G.; Cunico, L.; Tansella, M. Validity and Test-Retest Reliability of the Italian Version of the 12-Item General Health Questionnaire in General Practice: A Comparison between Three Scoring Methods. Compr. Psychiatry 1993, 34, 198–205. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma Stress 2015, 28, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Di Tella, M.; Romeo, A.; Zara, G.; Castelli, L.; Settanni, M. The Post-Traumatic Stress Disorder Checklist for DSM-5: Psychometric Properties of the Italian Version. Int. J. Environ. Res. Public Health 2022, 19, 5282. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.M.; Davidson, J.R.T. Development of a New Resilience Scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Di Fabio, A.; Palazzeschi, L. Connor-Davidson Resilience Scale: Proprietà Psicometriche Della Versione Italiana [Connor-Davidson Resilience Scale: Psychometric Properties of the Italian Version]. Counsel. Giornale Ital. Ric. Appl. 2012, 5, 101–110. [Google Scholar]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the Positive Legacy of Trauma. J. Trauma Stress 1996, 9, 455–471. [Google Scholar] [CrossRef] [PubMed]
- Prati, G.; Pietrantoni, L. Italian Adaptation and Confirmatory Factor Analysis of the Full and the Short Form of the Posttraumatic Growth Inventory. J. Loss Trauma 2014, 19, 12–22. [Google Scholar] [CrossRef]
- Little, R.J.A. A Test of Missing Completely at Random for Multivariate Data with Missing Values. J. Am. Stat. Assoc. 1988, 83, 1198–1202. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; Guilford Publications: New York, NY, USA, 2015; ISBN 1-4625-1779-X. [Google Scholar]
- Chen, F.F. Sensitivity of Goodness of Fit Indexes to Lack of Measurement Invariance. Struct. Equ. Model. Multidiscip. J. 2007, 14, 464–504. [Google Scholar] [CrossRef]
- Reise, S.P.; Moore, T.M.; Haviland, M.G. Bifactor Models and Rotations: Exploring the Extent to Which Multidimensional Data Yield Univocal Scale Scores. J. Pers. Assess. 2010, 92, 544–559. [Google Scholar] [CrossRef]
- Reise, S.P.; Scheines, R.; Widaman, K.F.; Haviland, M.G. Multidimensionality and Structural Coefficient Bias in Structural Equation Modeling: A Bifactor Perspective. Educ. Psychol. Meas. 2013, 73, 5–26. [Google Scholar] [CrossRef] [Green Version]
- Schmid, J.; Leiman, J.M. The Development of Hierarchical Factor Solutions. Psychometrika 1957, 22, 53–61. [Google Scholar] [CrossRef]
- Revelle, W. Psych: Procedures for Psychological, Psychometric, and Personality Research; Evanston, IL, USA, 2020. [Google Scholar]
- Kim, H.; Ji, J. Factor Structure and Longitudinal Invariance of the Maslach Burnout Inventory. Res. Soc. Work Pract. 2009, 19, 325–339. [Google Scholar] [CrossRef]
- Kanste, O.; Miettunen, J.; Kyngäs, H. Factor Structure of the Maslach Burnout Inventory among Finnish Nursing Staff. Nurs. Health Sci. 2006, 8, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Taku, K.; Cann, A.; Calhoun, L.G.; Tedeschi, R.G. The Factor Structure of the Posttraumatic Growth Inventory: A Comparison of Five Models Using Confirmatory Factor Analysis. J. Trauma Stress 2008, 21, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Loera, B.; Converso, D.; Viotti, S. Evaluating the Psychometric Properties of the Maslach Burnout Inventory-Human Services Survey (MBI-HSS) among Italian Nurses: How Many Factors Must a Researcher Consider? PLoS ONE 2014, 9, e114987. [Google Scholar] [CrossRef] [Green Version]
- Worley, J.A.; Vassar, M.; Wheeler, D.L.; Barnes, L.L.B. Factor Structure of Scores From the Maslach Burnout Inventory: A Review and Meta-Analysis of 45 Exploratory and Confirmatory Factor-Analytic Studies. Educ. Psychol. Meas. 2008, 68, 797–823. [Google Scholar] [CrossRef]
- Poghosyan, L.; Aiken, L.H.; Sloane, D.M. Factor Structure of the Maslach Burnout Inventory: An Analysis of Data from Large Scale Cross-Sectional Surveys of Nurses from Eight Countries. Int. J. Nurs. Stud. 2009, 46, 894–902. [Google Scholar] [CrossRef] [Green Version]
- De Beer, L.T.; Bianchi, R. Confirmatory Factor Analysis of the Maslach Burnout Inventory: A Bayesian Structural Equation Modeling Approach. Eur. J. Psychol. Assess. 2019, 35, 217–224. [Google Scholar] [CrossRef]
- Stalker, C.A.; Harvey, C.; Frensch, K.; Mandell, D.; Adams, G.R. Confirmatory Factor Analysis of the Maslach Burnout Inventory. Null 2008, 1, 77–94. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory, 3rd ed.; Scarecrow Education: Lanham, MD, USA, 1996. [Google Scholar]
- Meade, A.W.; Lautenschlager, G.J.; Hecht, J.E. Establishing Measurement Equivalence and Invariance in Longitudinal Data With Item Response Theory. Int. J. Test. 2005, 5, 279–300. [Google Scholar] [CrossRef]
- Murray, A.L.; Obsuth, I.; Eisner, M.; Ribeaud, D. Evaluating Longitudinal Invariance in Dimensions of Mental Health Across Adolescence: An Analysis of the Social Behavior Questionnaire. Assessment 2019, 26, 1234–1245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brincks, A.; Montag, S.; Howe, G.W.; Huang, S.; Siddique, J.; Ahn, S.; Sandler, I.N.; Pantin, H.; Brown, C.H. Addressing Methodologic Challenges and Minimizing Threats to Validity in Synthesizing Findings from Individual-Level Data Across Longitudinal Randomized Trials. Prev. Sci. 2018, 19, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Gross, R.A. Examining the Robustness of the Latent Growth Curve Model to Violations of Longitudinal Measurement Equivalence: A Methodological Study with Practical Applications in Child Development. Ph.D. Thesis, Indiana University, Bloomington, IN, USA, 2020. [Google Scholar]
- Marsh, H.; Guo, J.; Parker, P.; Nagengast, B.; Asparouhov, T.; Muthén, B.; Dicke, T. What to Do When Scalar Invariance Fails: The Extended Alignment Method for Multi-Group Factor Analysis Comparison of Latent Means Across Many Groups. Psychol. Methods 2017, 23, 524. [Google Scholar] [CrossRef]
- Kenny, D.A.; McCoach, D.B. Effect of the Number of Variables on Measures of Fit in Structural Equation Modeling. Struct. Equ. Model. 2003, 10, 333–351. [Google Scholar] [CrossRef]
- Zuromski, K.L.; Ustun, B.; Hwang, I.; Keane, T.M.; Marx, B.P.; Stein, M.B.; Ursano, R.J.; Kessler, R.C. Developing an Optimal Short-Form of the PTSD Checklist for DSM-5 (PCL-5). Depress. Anxiety 2019, 36, 790–800. [Google Scholar] [CrossRef] [PubMed]
- Kaur, N.; Porter, B.; LeardMann, C.A.; Tobin, L.E.; Lemus, H.; Luxton, D.D.; Armenta, R.; Bauer, L.; Bookwalter, D.; Bukowinski, A.; et al. Evaluation of a Modified Version of the Posttraumatic Growth Inventory-Short Form. BMC Med. Res. Methodol. 2017, 17, 69. [Google Scholar] [CrossRef] [PubMed]
- Cann, A.; Calhoun, L.G.; Tedeschi, R.G.; Taku, K.; Vishnevsky, T.; Triplett, K.N.; Danhauer, S.C. A Short Form of the Posttraumatic Growth Inventory. Anxiety Stress Coping 2010, 23, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Nartova-Bochaver, S.; Korneev, A.; Bochaver, K. Validation of the 10-Item Connor–Davidson Resilience Scale: The Case of Russian Youth. Front. Psychiatry 2021, 12, 611026. [Google Scholar] [CrossRef] [PubMed]
- Notario, B.; Solera-Martínez, M.; Serrano-Parra, M.; Bartolomé, R.; Garcia-Campayo, J.; Martinez Vizcaino, V. Reliability and Validity of the Spanish Version of the 10-Item Connor-Davidson Resilience Scale (10-Item CD-RISC) in Young Adults. Health Qual. Life Outcomes 2011, 9, 63. [Google Scholar] [CrossRef] [Green Version]
| Variable | Level | n (%) | Missing Data n (%) |
|---|---|---|---|
| Sex | Female | 622 (77.6) | 3 (0.3) |
| Male | 180 (22.4) | ||
| Age | 25–34 years | 126 (15.7) | 1 (0.1) |
| 35–44 years | 178 (22.1) | ||
| 45–54 years | 306 (38.1) | ||
| 55 years or more | 194 (24.1) | ||
| Job profile | Clerk | 102 (12.7) | |
| Doctor | 104 (12.9) | ||
| Nurse | 429 (53.3) | ||
| Nurse assistant | 170 (21.1) | ||
| Education attainment | Primary school | 115 (14.3) | 1 (0.1) |
| Secondary school | 295 (36.7) | ||
| Attended university | 20 (2.5) | ||
| Bachelor’s degree | 192 (23.9) | ||
| Master’s degree | 61 (7.6) | ||
| Postgraduate programs or specialization | 121 (15.0) | ||
| Job seniority | Less than 1 year | 57 (7.1) | 3 (0.3) |
| From 1 to 5 years | 167 (20.8) | ||
| From 6 to 15 years | 190 (23.7) | ||
| From 16 to 30 years | 255 (31.8) | ||
| More than 30 years | 133 (16.6) | ||
| Work seniority in current role | Less than 1 year | 62 (7.7) | 2 (0.2) |
| From 1 to 5 years | 232 (28.9) | ||
| From 6 to 15 years | 223 (27.8) | ||
| From 16 to 30 years | 230 (28.6) | ||
| More than 30 years | 56 (7.0) | ||
| Type of contract | Fixed-term | 14 (1.7) | 2 (0.2) |
| Permanent | 789 (98.3) | ||
| Type of employment | Full-time | 693 (86.3) | 2 (0.2) |
| Part-time | 110 (13.7) | ||
| Work scheduling | Non-shift work | 151 (18.8) | 2 (0.2) |
| Shift work (with night shifts) | 502 (62.5) | ||
| Shift work (without night shifts) | 150 (18.7) |
| Structure | Modifications with Respect to the Original Structure | CFI | RMSEA | Issues Affecting the Fit of the Structure * |
|---|---|---|---|---|
| Original three-correlated factors structure [24,26] | 0.8084 | 0.0829 | Presence of cross-loadings of items 6 (EE and DEP), 12 (EE, PA) and 16 (EE, DEP). Presence of correlated errors between items 6 and 16, 1 and 2, 2 and 3. | |
| Three-correlated factors structure, with deletion of items 12 and 16 | Removed items 12 and 16 | 0.8639 | 0.0730 | Presence of cross-loadings of items 6 (EE and DEP) and 2 (EE, DEP). Presence of local dependencies between items 1 and 2, 2 and 3. |
| Previous structure with further deletion of item 2, similarly to Kim and Ji, 2009 [47] | Removed items 2, 12, 16 | 0.8902 | 0.0639 | Presence of cross-loadings of items 6 (EE and DEP) and 2 (EE, DEP). Presence of local dependencies between items 6 and 5. |
| Previous structure with further deletion of item 6, similarly to Kanste et al., 2006 [48] | Removed items 2, 6, 12, 16 | 0.9260 | 0.0532 |
| Type of Invariance | CFI | RMSEA | ΔCFI | ΔRMSEA | Comment |
|---|---|---|---|---|---|
| Configural invariance | 0.9140 | 0.0457 | Configural invariance was met | ||
| Metric invariance | 0.9075 | 0.0467 | 0.0065 | 0.001 | Metric invariance was met |
| Scalar invariance | 0.8440 | 0.0597 | 0.0635 | 0.013 | Complete scalar invariance was not met |
| Scalar invariance (freed the constraints to the intercepts of items 4, 8, 13, 14 and 20) | 0.8836 | 0.0518 | 0.0239 * | 0.005 * | After freeing the loadings of five items, partial invariance was not met |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giusti, E.M.; Veronesi, G.; Callegari, C.; Castelnuovo, G.; Iacoviello, L.; Ferrario, M.M. The North Italian Longitudinal Study Assessing the Mental Health Effects of SARS-CoV-2 Pandemic Health Care Workers—Part II: Structural Validity of Scales Assessing Mental Health. Int. J. Environ. Res. Public Health 2022, 19, 9541. https://doi.org/10.3390/ijerph19159541
Giusti EM, Veronesi G, Callegari C, Castelnuovo G, Iacoviello L, Ferrario MM. The North Italian Longitudinal Study Assessing the Mental Health Effects of SARS-CoV-2 Pandemic Health Care Workers—Part II: Structural Validity of Scales Assessing Mental Health. International Journal of Environmental Research and Public Health. 2022; 19(15):9541. https://doi.org/10.3390/ijerph19159541
Chicago/Turabian StyleGiusti, Emanuele Maria, Giovanni Veronesi, Camilla Callegari, Gianluca Castelnuovo, Licia Iacoviello, and Marco Mario Ferrario. 2022. "The North Italian Longitudinal Study Assessing the Mental Health Effects of SARS-CoV-2 Pandemic Health Care Workers—Part II: Structural Validity of Scales Assessing Mental Health" International Journal of Environmental Research and Public Health 19, no. 15: 9541. https://doi.org/10.3390/ijerph19159541
APA StyleGiusti, E. M., Veronesi, G., Callegari, C., Castelnuovo, G., Iacoviello, L., & Ferrario, M. M. (2022). The North Italian Longitudinal Study Assessing the Mental Health Effects of SARS-CoV-2 Pandemic Health Care Workers—Part II: Structural Validity of Scales Assessing Mental Health. International Journal of Environmental Research and Public Health, 19(15), 9541. https://doi.org/10.3390/ijerph19159541







