Australian University Nursing and Allied Health Students’ and Staff Physical Activity Promotion Preparedness and Knowledge: A Pre-Post Study Using an Educational Intervention
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Intervention
2.2.1. Movement for Movement Physical Activity Resources
2.2.2. Physical Activity Champions
2.3. Survey
2.4. Curriculum Audit
2.5. Sample Size
2.6. Data Analysis
3. Results
3.1. Knowledge, Role Perception, Confidence, Barriers, and Feasibility in Regard to Physical Activity Promotion
3.2. Other Barriers to Promoting a Physically Active Lifestyle to Patients/Individuals
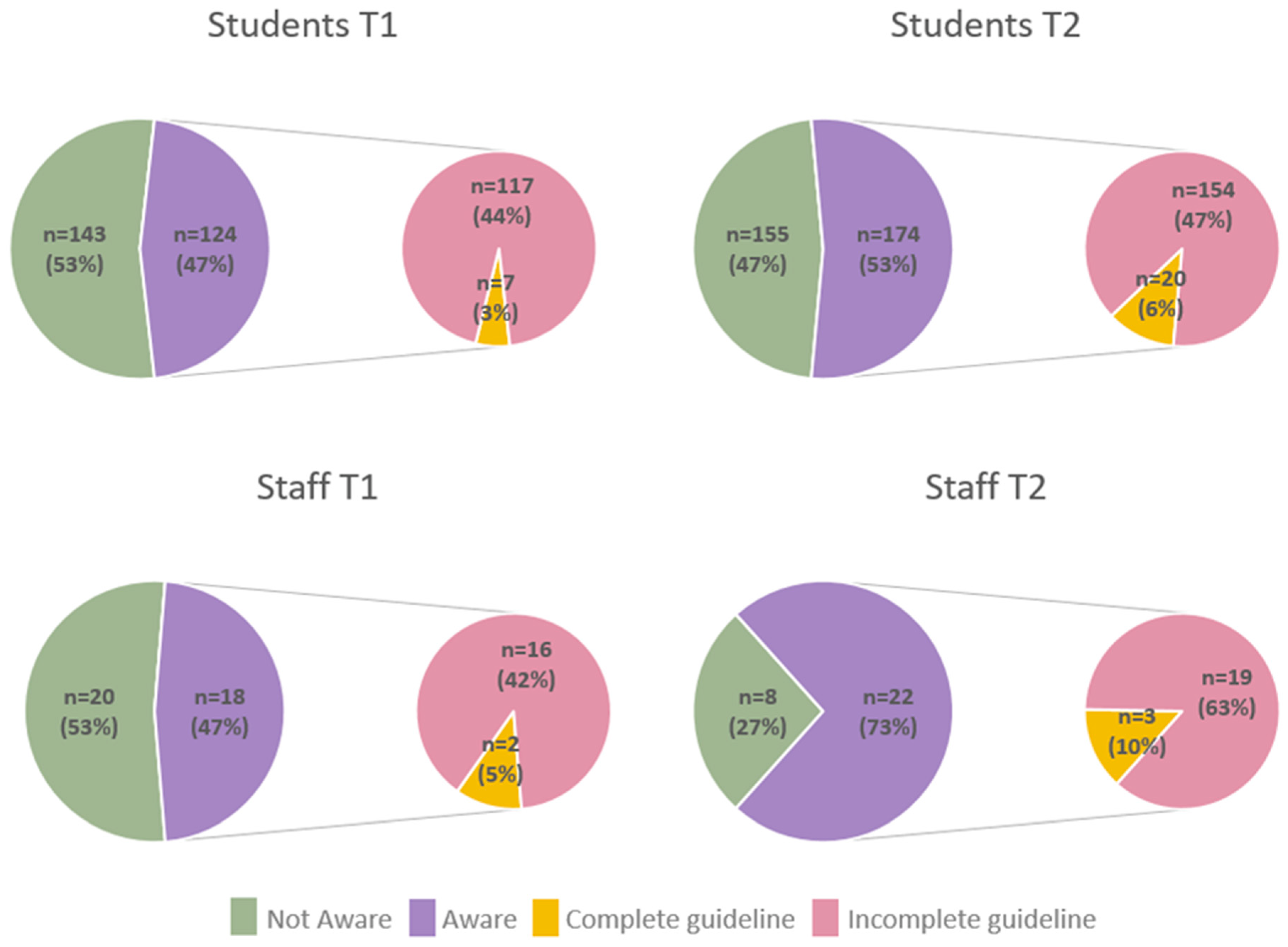
3.3. Awareness and Knowledge of the Australian Physical Activity and Sedentary Behaviour Guidelines
3.4. Curriculum Audit
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Rahmati, M.; Shamsi, M.M.; Khoramipour, K.; Malakoutinia, F.; Woo, W.; Park, S.; Yon, D.K.; Lee, S.W.; Shin, J.I.; Smith, L. Baseline Physical Activity Is Associated with Reduced Mortality and Disease Outcomes in COVID-19: A Systematic Review and Meta-Analysis. Rev. Med. Virol. 2022, e2349. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. National Health Survey 2020–21: Physical Activity. Available online: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/physical-activity/latest-release (accessed on 13 May 2022).
- National Heart Foundation of Australia. Blueprint for an active Australia, 3rd ed.; National Heart Foundation of Australia: Canberra, Australia, 2019. [Google Scholar]
- World Health Organisation. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organisation: Geneva, Switzerland, 2018. [Google Scholar]
- Orrow, G.; Kinmonth, A.-L.; Sanderson, S.; Sutton, S. Effectiveness of physical activity promotion based in primary care: Systematic review and meta-analysis of randomised controlled trials. BMJ 2012, 344, e1389. [Google Scholar] [CrossRef] [Green Version]
- Freene, N.; Davey, R.; McPhail, S.M. Frequency of a very brief intervention by physiotherapists to increase physical activity levels in adults: A pilot randomised controlled trial. BMC Sports Sci. Med. Rehabil. 2019, 11, 6. [Google Scholar] [CrossRef] [Green Version]
- Freene, N.; Cools, S.; Hills, D.; Bissett, B.; Pumpa, K.; Cooper, G. A wake-up call for physical activity promotion in Australia: Results from a survey of Australian nursing and allied health professionals. Aust. Health Rev. A Publ. Aust. Hosp. Assoc. 2017, 43, 165–170. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Health Service Usage and Health Related Actions, Australia, 2014–2015; Australian Bureau of Statistics: Canberra, Australia, 2017.
- Gates, A.B.; Swainson, M.G.; Moffatt, F.; Kerry, R.; Metsios, G.S.; Ritchie, I. Undergraduate examination and assessment of knowledge and skills is crucial in capacity planning for the future healthcare workforce in physical activity interventions. Br. J. Sports Med. 2020, 54, 1015–1016. [Google Scholar] [CrossRef]
- Fletcher, R.B.; Meyer, L.H.; Anderson, H.; Johnston, P.; Rees, M. Faculty and Students Conceptions of Assessment in Higher Education. High. Educ. 2012, 64, 119–133. [Google Scholar] [CrossRef]
- Sambell, K.; McDowell, L. The Construction of the Hidden Curriculum: Messages and meanings in the assessment of student learning. Assess. Eval. High. Educ. 1998, 23, 391–402. [Google Scholar] [CrossRef]
- Huijg, J.; Gebhardt, W.; Verheijden, M.; Zouwe, N.; Vries, J.; Middelkoop, B.; Crone, M. Factors Influencing Primary Health Care Professionals’ Physical Activity Promotion Behaviors: A Systematic Review. Int. J. Behav. Med. 2015, 22, 32–50. [Google Scholar] [CrossRef]
- Hsiao, Y.-C.; Chen, M.-Y.; Gau, Y.-M.; Hung, L.-L.; Chang, S.-H.; Tsai, H.-M. Short-Term Effects of a Health Promotion Course for Taiwanese Nursing Students. Public Health Nurs. 2005, 22, 74–81. [Google Scholar] [CrossRef]
- Yeh, L.; Chen, C.H.; Wang, C.J.; Wen, M.J.; Fetzer, S.J. A preliminary study of a healthy-lifestyle-promoting program for nursing students in Taiwan. J. Nurs. Educ. 2005, 44, 563–565. [Google Scholar] [CrossRef]
- Lenz, T.L. An Elective Course on Lifestyle Modifications in Pharmacotherapy. Am. J. Pharm. Educ. 2007, 71, 1–7. [Google Scholar] [CrossRef]
- Kotecki, J.E.; Clayton, B.D. Educating Pharmacy Students about Nutrition and Physical Activity Counseling. Am. J. Health Educ. 2003, 34, 34–40. [Google Scholar] [CrossRef]
- Persky, A.M. An Exercise Prescription Course to Improve Pharmacy Students’ Confidence in Patient Counseling. Am. J. Pharm. Educ. 2009, 73, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Korn, L.; Ben-Ami, N.; Azmon, M.; Einstein, O.; Lotan, M. Evaluating the Effectiveness of a Health Promotion Intervention Program Among Physiotherapy Undergraduate Students. Med. Sci. Monit. 2017, 23, 3518–3527. [Google Scholar] [CrossRef] [Green Version]
- Matthews, J.; Hall, A.M.; Keogh, A. Evaluating the effects of behavior change training on the knowledge, confidence and skills of sport and exercise science students. BMC Sports Sci. Med. Rehabil. 2020, 12, 62. [Google Scholar] [CrossRef]
- Ryan, J.M.; Cameron, E.M.; McGowan, E.L. Changing Physical Activity Counseling Outcomes Among Future Health Professionals. Clin. Kinesiol. (Online Ed.) 2017, 71, 25–33. [Google Scholar]
- Stoutenberg, M.; Powell, B.J.; Busignani, P.J.; Bowersock, A.H.; Pojednic, R. Identifying Key Physical Activity Categories and Topics to Include in Health Professional Training Programs. Teach. Learn. Med. 2020, 32, 362–370. [Google Scholar] [CrossRef]
- Gates, A.B. Making every contact count for physical activity—For tomorrow’s patients: The launch of the interdisciplinary, undergraduate, resources on exercise medicine and health in the U.K. Br. J. Sports Med. 2016, 50, 322–323. [Google Scholar] [CrossRef]
- Gates, A.B.; Kerry, R.; Moffatt, F.; Ritchie, I.K.; Meakins, A.; Thornton, J.S.; Rosenbaum, S.; Taylor, A. Movement for movement: Exercise as everybody's business? Br. J. Sports Med. 2017, 51, 767–768. [Google Scholar] [CrossRef]
- World Health Organization. United Kingdom Physical Activity FactSheet 2018. Available online: http://www.euro.who.int/__data/assets/pdf_file/0004/382585/united-kingdom-eng.pdf?ua=1 (accessed on 29 January 2022).
- Freene, N. Canberra physiotherapy students’ commit to making every contact count for physical activity! BJSM Br. J. Sports Med. Blog 2017. Available online: https://blogs.bmj.com/bjsm/2017/09/10/canberra-physiotherapy-students-commit-making-every-contact-count-physical-activity/ (accessed on 13 May 2022).
- Shirley, D.; Van der Ploeg, H.P.; Bauman, A.E. Physical Activity Promotion in the Physical Therapy Setting: Perspectives from Practitioners and Students. Phys. Ther. 2010, 90, 1311–1322. [Google Scholar] [CrossRef] [Green Version]
- Taylor, N.F.; Dodd, K.J.; Shields, N.; Bruder, A. Therapeutic exercise in physiotherapy practice is beneficial: A summary of systematic reviews 2002–2005. Aust. J. Physiother. 2007, 53, 7–16. [Google Scholar] [CrossRef] [Green Version]
- The American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th Edition. Available online: https://www.aapor.org/Standards-Ethics/Standard-Definitions-(1).aspx (accessed on 13 May 2022).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Pojednic, R.; Stoutenberg, M. Key Steps to Implementing Physical Activity into Health Professional Training Programs. Curr. Sports Med. Rep. 2020, 19, 396–398. [Google Scholar] [CrossRef]
- Milton, K.; Larner, J.; Hanson, S.; Jones, A. Embedding Physical Activity into the Healthcare Curriculum—A Case Study. Educ. Prim. Care 2020, 31, 176–179. [Google Scholar] [CrossRef]
- Dacey, M.L.; Kennedy, M.A.; Polak, R.; Phillips, E.M. Physical activity counseling in medical school education: A systematic review. Med. Educ. Online 2014, 19, 24325. [Google Scholar] [CrossRef] [Green Version]
- Phillips, E.; Pojednic, R.; Polak, R.; Bush, J.; Trilk, J. Including lifestyle medicine in undergraduate medical curricula. Med. Educ. Online 2015, 20, 26150. [Google Scholar] [CrossRef] [PubMed]
- Fie, S.; Norman, I.J.; While, A.E. The relationship between physicians’ and nurses’ personal physical activity habits and their health-promotion practice: A systematic review. Health Educ. J. 2013, 72, 102–119. [Google Scholar] [CrossRef]
| Student | Staff | |||
|---|---|---|---|---|
| Characteristic | T1 | T2 | T1 | T2 |
| (n = 267) | (n = 330) | (n = 38) | (n = 30) | |
| Gender, Female n (%) | 230 (86.1) | 271 (82.1) | 28 (73.7) | 23 (76.7) |
| Student age (yrs), median (Q1, Q3) | 24 (21, 33) | 23 (20, 31) | - | - |
| Staff age (yrs), ≥45 yrs n (%) | - | - | 19 (50) | 16 (53.4) |
| Discipline, n (%) | ||||
| Occupational Therapy | 21 (7.9) | 11 (3.3) * | 3 (7.9) | 1 (3.3) |
| Physiotherapy | 41 (15.4) | 56 (17.0) | 5 (13.2) | 8 (26.7) |
| Pharmacy | 24 (9) | 12 (3.6) | 1 (2.6) | 1 (3.3) |
| Nutrition and Dietetics | 12 (4.5) | 15 (4.5) | - | - |
| Nursing | 79 (29.7) | 122 (37.0) | 9 (23.7) | 11 (36.7) |
| Midwifery | 13 (4.9) | 12 (3.6) | 6 (15.8) | 4 (13.3) |
| Psychology | 41 (15.4) | 40 (12.1) | 4 (10.5) | 1 (3.3) |
| Vision Science and Optometry | 3 (1.1) | 9 (2.7) | 2 (5.3) | 1 (3.3) |
| Speech Pathology | 4 (1.5) | 7 (2.1) | - | - |
| Counselling | 2 (0.8) | 3 (0.9) | 3 (7.9) | 1 (3.3) |
| Sport and Exercise Science | 11 (4.1) | 30 (9.1) | 2 (5.3) | 2 (6.7) |
| Medical Radiation Science | 6 (2.3) | 8 (2.4) | - | - |
| Public Health | 9 (3.4) | 5 (1.5) | 1 (2.6) | 0 (0) |
| Undergraduate, n (%) | 214 (80.1) | 281 (85.2) | - | - |
| Year of degree n (%) | ||||
| First | 113 (42.3) | 123 (37.3) | - | - |
| Second | 79 (29.6) | 120 (36.4) | - | - |
| Third | 58 (21.7) | 63 (19.1) | - | - |
| Fourth | 17 (6.4) | 24 (7.3) | - | - |
| Years since completing first health degree | - | - | 22 (10) | 20 (15, 24) |
| Trained health professional, yes n (%) | - | - | 32 (84.2) | 28 (93.3) |
| Health professional currently practicing, yes n (%) | - | - | 16 (50) | 15 (53.6) |
| Encouraging patients to have a more physically active lifestyle in the last month, often (>6 patients) n (%) | - | - | 9 (56.3) | 8 (53.4) |
| Practice type, private practice n (%) | - | - | 9 (56.3) | 8 (53.3) |
| Patients/wk, median (Q1, Q3) | - | - | 9 (4, 22) | 6 (3, 15) |
| Years in practice, mean (SD) | - | - | 18.6 (10.5) | 22.5 (8.5) |
| Hours worked/wk, median (Q1, Q3) | - | - | 13 (5, 40) | 6 (4, 28) |
| How physically active do you think you are currently compared with other Australians of your sex and age? More active n (%) | 140 (53.4) | 159 (48.9) | 18 (47.4) | 20 (69) |
| Students | Staff | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Agree n (%) | Median (Q1, Q3) | Agree n (%) | Median (Q1, Q3) | ||||
| T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | |
| Knowledge of physical activity messages a | ||||||||
| Taking the stairs at work and generally being more active each day is enough physical activity to improve health | 146 (49) | 194 (54) | 3 (2, 4) | 2 (2, 4) | 16 (37) | 13 (41) | 4 (2, 4) | 4 (2, 4) |
| Half an hour of walking on most days is all the physical activity that is needed for good health | 145 (49) | 153 (42) | 3 (2, 4) | 3 (2, 4) | 19 (44) | 11 (34) | 3 (2, 4) | 4 (2, 4) |
| Physical activity that is good for health must make you puff and pant | 87 (29) | 90 (25) | 4 (2, 4) | 4 (3, 4) | 15 (35) | 13 (41) | 4 (2, 4) | 4 (2, 4) |
| Several short walks on most days is better than one round of golf per week for good health | 231 (77) | 285 (79) | 2 (2, 2) | 2 (2, 2) * | 30 (70) | 31 (97) | 2 (2, 3) | 2 (1, 2) * |
| Health Professionals role b | ||||||||
| Discussing the benefits of a physically active lifestyle with patients/individuals is part of the health professional’s role | 284 (95) | 346 (95) | 1 (1, 2) | 1 (1, 2) | 40 (93) | 31 (97) | 1 (1, 2) | 1 (1, 2) |
| Suggesting to patients/individuals ways to increase daily physical activity is part of the health professional’s role | 274 (92) | 329 (91) | 2 (1, 2) | 2 (1, 2) | 37 (86) | 29 (91) | 2 (1, 2) | 1 (1, 2) |
| Health professionals should be physically active to act as a role model for their patients/individuals | 268 (90) | 324 (89) | 2 (1, 2) | 2 (1, 2) | 38 (88) | 26 (81) | 2 (1, 2) | 2 (1, 2) |
| Confidence in providing physical activity messages c | ||||||||
| I would feel confident in giving general advice to patients/individuals on a physically active lifestyle | 226 (76) | 264 (73) | 2 (1, 2) | 2 (1, 3) | 26 (70) | 24 (83) | 2 (1, 3) | 2 (1, 2) |
| I would feel confident in suggesting specific physical activity programs for my patients/individuals | 143 (48) | 185 (51) | 3 (2, 4) | 2 (2, 4) | 15 (42) | 18 (62) | 3 (1, 4) | 2 (1, 4) |
| Barriers to physical activity promotion d | ||||||||
| Lack of time | 142 (50) | 190 (55) | 3.5 (3, 4) | 4 (3, 4) | 22 (56) | 20 (67) | 4 (3, 4) | 4 (3, 4) |
| Lack of counselling skills | 102 (36) | 129 (37) | 3 (2, 4) | 3 (3, 4) | 19 (49) | 17 (57) | 3 (3, 4) | 4 (3, 4) |
| Lack of remuneration for promoting physical activity | 65 (23) | 63 (18) | 3 (2, 3) | 3 (2, 3) | 11 (28) | 3 (10) | 2 (2, 4) | 2 (1, 3) |
| Lack of interest in promoting physical activity | 78 (28) | 97 (28) | 3 (2, 4) | 3 (2, 4) | 10 (26) | 6 (20) | 3 (2, 4) | 3 (2, 3) |
| Feeling it would not change the patient’s/individual’s behaviour | 118 (42) | 129 (37) | 3 (2, 4) | 3 (2, 4) | 12 (31) | 13 (43) | 3 (3, 4) | 3 (3, 4) |
| Feeling it would not be beneficial for the patient/individual | 44 (16) | 38 (26) | 2 (2, 3) | 2 (2, 3) | 3 (8) | 4 (13) | 2 (2, 3) | 2 (2, 3) |
| Feasibility of physical activity promotion strategies e | ||||||||
| Brief counselling integrated into regular consultations | 224 (83) | 259 (79) | 2 (1, 2) | 2 (1, 2) | 19 (76) | 26 (87) | 2 (1, 2) | 2 (1, 2) |
| Separate one-on-one consultations | 162 (60) | 181 (55) | 2 (2, 3) | 2 (2,4) | 16 (42) | 13 (43) | 3 (2, 4) | 3 (2, 4) |
| Group sessions | 173 (64) | 212 (64) | 2 (1, 3) | 2 (2, 3) | 17 (45) | 23 (77) | 3 (2, 4) | 2 (2, 2) |
| Distribution of resources (e.g., brochures) | 229 (85) | 285 (86) | 1 (1, 2) | 1 (1, 2) | 33 (87) | 27 (90) | 1 (1,2) | 1 (1, 2) |
| Themes | Students | Staff |
|---|---|---|
| Lack of PA promotion skills | Lack of confidence to counsel on physical activity especially with overweight or obese patients/individuals (Public Health) Not wanting to cause offence to a patient (Physiotherapy) | Lacks courage to discuss tough issues (Nursing) Not having skills in assessing ambivalence and motivation (Nursing) |
| Feeling hypocritical | Embarrassed by own lack of personal physical fitness (Nursing) Clinician’s own inactive lifestyle may impact their willingness to encourage clients to understand the benefits of physical activity (Psychology) | Not wanting to give advice on something they don’t do personally (Physiotherapy) |
| Understanding the benefits of PA promotion by all HPs, for all patients, in all settings | Focus on immediate issue (Pharmacy) Feeling it is not part of our role (Speech Pathology) Not wanting to counter/contradict gp/specialist recommendations (Occupational Therapy) | Difficulty with talking about physical activity in the setting as may not directly relate to the service we provide (Vision Science & Optometry) |
| Organisational support is key | Not promoted by the organisation health professionals work in (Nursing) | Lack of organisational support and reinforcement of fundamental care activities (Nursing) |
| Subject Characteristics | T1 | T2 |
|---|---|---|
| (n = 41) | (n = 48) | |
| Discipline, n (%) | ||
| Occupational Therapy | 3 (7.3) | 4 (8.3) |
| Physiotherapy | 12 (29.3) | 12 (25) |
| Pharmacy | 2 (4.9) | 4 (8.3) |
| Nutrition and Dietetics | 2 (4.9) | 2 (4.2) |
| Nursing | 2 (4.9) | 3 (6.3) |
| Midwifery | 7 (17.1) | 7 (14.6) |
| Psychology | 0 (0) | 0 (0) |
| Vision Science and Optometry | 0 (0) | 1 (2.1) |
| Speech Pathology | 0 (0) | 0 (0) |
| Counselling | 0 (0) | 0 (0) |
| Sport and Exercise Science | 7 (17.1) | 6 (12.5) |
| Medical Radiation Science | 0 (0) | 0 (0) |
| Public Health | 0 (0) | 0 (0) |
| Inter-professional | 6 (14.6) | 9 (18.8) |
| Undergraduate, n (%) | 24 (58.5) | 30 (62.5) |
| Year of Degree, n (%) | ||
| First | 17 (41.5) | 18 (37.5) |
| Second | 8 (19.5) | 12 (25) |
| Third | 13 (31.7) | 14 (29.2) |
| Fourth | 1 (2.4) | 2 (4.2) |
| Multiple years | 2 (4.9) | 2 (4.2) |
| Teaching Period, n (%) | ||
| Semester 1 | 21 (51.2) | 27 (56.3) |
| Semester 2 | 20 (48.8) | 20 (41.7) |
| Winter Term | 0 (0) | 1 (2.1) |
| Number of Students/subject, median (Q1, Q3) | 33 (25, 60) | 41 (22, 65) |
| Specific physical activity content in lectures, yes n (%) | 33 (80.5) | 38 (79.2) |
| Number of lectures/subject, median (Q1, Q3) | 2 (1, 3.5) | 2 (1, 5) |
| Specific physical activity content in lectures (hrs), median (Q1, Q3) | 0.5 (0.15, 1) | 1 (0.15, 2) |
| Specific physical activity content in tutorials, yes n (%) | 29 (70.7) | 37 (77.1) |
| Number of tutorials/subject, median (Q1, Q3) | 1 (0, 2.5) | 1 (1, 5) |
| Specific physical activity content in tutorials (hrs), median (Q1, Q3) | 0.5 (0, 1.75) | 1 (0.35, 2.5) |
| Assessment of physical activity content, yes n (%) | 21 (51.2) | 28 (58.3) |
| Type of physical activity content included, yes n (%) | ||
| Physical activity guideline components | 22 (53.7) | 29 (60.4) |
| Health benefits of physical activity | 40 (97.6) | 47 (97.9) |
| Physical activity promotion skills | 26 (63.4) | 36 (75) |
| Movement for Movement resources | 2 (4.9) | 14 (29.2) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freene, N.; Porra, K.; Bousie, J.A.; Naunton, M.; Ball, N.; Flood, A.; Bail, K.; Smith, S.D.-V.; Blenkin, M.; Cheong, L.; et al. Australian University Nursing and Allied Health Students’ and Staff Physical Activity Promotion Preparedness and Knowledge: A Pre-Post Study Using an Educational Intervention. Int. J. Environ. Res. Public Health 2022, 19, 9255. https://doi.org/10.3390/ijerph19159255
Freene N, Porra K, Bousie JA, Naunton M, Ball N, Flood A, Bail K, Smith SD-V, Blenkin M, Cheong L, et al. Australian University Nursing and Allied Health Students’ and Staff Physical Activity Promotion Preparedness and Knowledge: A Pre-Post Study Using an Educational Intervention. International Journal of Environmental Research and Public Health. 2022; 19(15):9255. https://doi.org/10.3390/ijerph19159255
Chicago/Turabian StyleFreene, Nicole, Katie Porra, Jaquelin A. Bousie, Mark Naunton, Nick Ball, Andrew Flood, Kasia Bail, Sally De-Vitry Smith, Milli Blenkin, Lynn Cheong, and et al. 2022. "Australian University Nursing and Allied Health Students’ and Staff Physical Activity Promotion Preparedness and Knowledge: A Pre-Post Study Using an Educational Intervention" International Journal of Environmental Research and Public Health 19, no. 15: 9255. https://doi.org/10.3390/ijerph19159255
APA StyleFreene, N., Porra, K., Bousie, J. A., Naunton, M., Ball, N., Flood, A., Bail, K., Smith, S. D.-V., Blenkin, M., Cheong, L., Shanahan, M., Isbel, S., Leung, M., & Gates, A. B. (2022). Australian University Nursing and Allied Health Students’ and Staff Physical Activity Promotion Preparedness and Knowledge: A Pre-Post Study Using an Educational Intervention. International Journal of Environmental Research and Public Health, 19(15), 9255. https://doi.org/10.3390/ijerph19159255







