Opportunistic Pathogens of Recreational Waters with Emphasis on Antimicrobial Resistance—A Possible Subject of Human Health Concern
Abstract
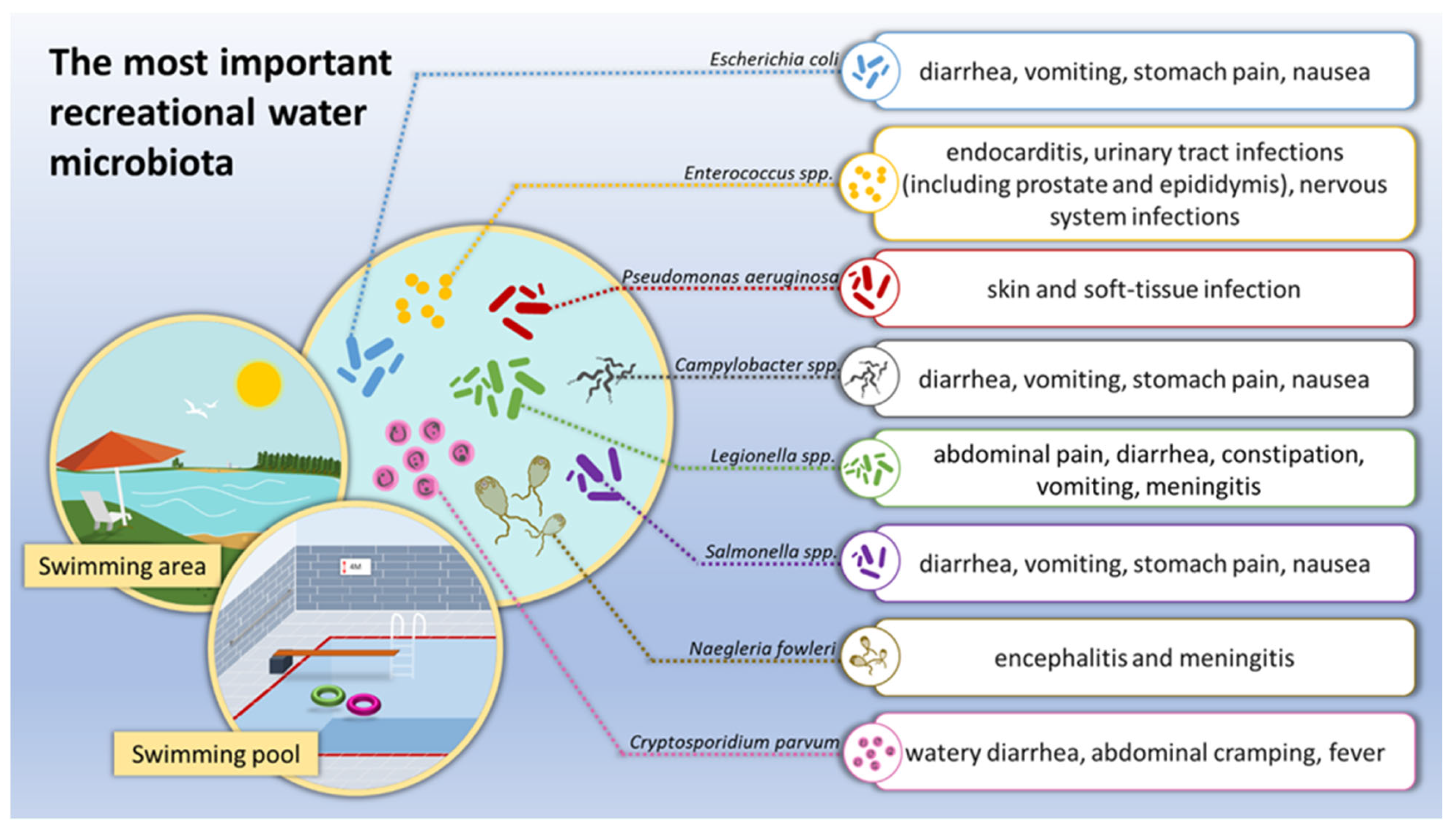
1. Introduction
2. Opportunistic Pathogens in Recreational Water
2.1. Sources of Water Contamination
2.2. Waterborne and Water-Based Opportunistic Pathogens in Recreational Water
2.3. Water as a Source of Disease-Causing Microorganisms
3. Antimicrobial Resistance of Microorganisms Isolated from Water
Health Problems after Contact with Microbial-Contaminated Water including Drug-Resistant Bacteria
4. Recreational Water Quality Law and Regulations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Naidoo, S.; Olaniran, A.O. Treated wastewater effluent as a source of microbial pollution of surface water resources. Int. J. Environ. Res. Public Health 2014, 11, 249–270. [Google Scholar] [CrossRef]
- Edokpayi, J.N.; Odiyo, J.O.; Durowoju, O.S. Impact of wastewater on surface water quality in developing countries: A case study of South Africa. Water Qual. 2017, 10, 401–416. [Google Scholar] [CrossRef]
- Fewtrell, L.; Kay, D. Recreational water and infection: A review of recent findings. Curr. Environ. Health Rep. 2015, 2, 85–94. [Google Scholar] [CrossRef]
- Pruden, A.; Ashbolt, N.; Miller, J. Part 3 Bacteria. Overview of Issues for Water Bacterial Pathogens. In Global Water Pathogen Project 2019; Rose, J.B., Jiménez-Cisneros, B., Eds.; Michigan State University: East Lansing, MI, USA, 2019; Available online: http://www.waterpathogens.org/book/overview-of-issues-for-water-bacterial-pathogens (accessed on 19 June 2020).
- DeFlorio-Barker, S.; Wade, T.S.; Turyk, M.; Dorevitch, S. Water recreation and illness severity. J. Water Health 2016, 14, 713–726. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines for Safe Recreational Water Environments, Volume 1: Coastal and Fresh Waters; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Information on HIV/AIDS Treatment, Prevention and Research. Available online: https://hivinfo.nih.gov/home-page (accessed on 25 July 2020).
- Cabral, J.P.S. Water Microbiology. Bacterial Pathogens and Water. Int. J. Environ. Res. Public Health 2010, 7, 3657–3703. [Google Scholar] [CrossRef]
- World Health Organization. Emerging Issues in Water and Infectious Disease; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Magana-Arachchi, D.N.; Wanigatunge, R.P. Ubiquitous waterborne pathogens. In Waterborne Pathogens; Butterworth-Heinemann: Oxford, UK, 2020; pp. 15–42. [Google Scholar] [CrossRef]
- Cozorici, D.; Măciucă, R.-A.; Stancu, C.; Tihăuan, B.-M.; Uță, R.B.; Codrea, C.I.; Matache, R.; Pop, C.-E.; Wolff, R.; Fendrihan, S. Microbial Contamination and Survival Rate on Different Types of Banknotes. Int. J. Environ. Res. Public Health 2022, 19, 4310. [Google Scholar] [CrossRef]
- USEPA. Recreational Water Quality Criteria; Office of Water, United States Environmental Protection Agency: Washington, DC, USA, 2012. [Google Scholar]
- WHO Recommendations on Scientific, Analytical and Epidemiological Developments Relevant to the Parameters for Bathing Water Quality in the Bathing Water Directive (2006/7/EC) 2018. Available online: https://circabc.europa.eu/d/d/workspace/SpacesStore/9e89152c-7cfe-4391-9bcf-c173519e8181/WHO%20Recommendations%20on%20EC%20BWD.pdf (accessed on 14 October 2020).
- Fang, Y.; Xie, G.L.; Lou, M.M.; Li, B.; Muhammad, I. Diversity analysis of Burkholderia cepacia complex in the water bodies of West Lake, Hangzhou, China. J. Microbiol. 2011, 49, 309–314. [Google Scholar] [CrossRef]
- Shanks, O.C.; Peed, L.A.; Kelty, C.A.; Sivaganesan, M.; Nietech, C.T. Pollution Source-Targeted Water Safety Management: Characterization of Diffuse Human Fecal Pollution Sources with Land Use Informatino, Strategic Water Sampling, and Quantitative Real-Time PCR. In Global Water Pathogen Project 2019; Rose, J.B., Jiménez-Cisneros, B., Eds.; Michigan State University: East Lansing, MI, USA, 2019; Available online: http://www.waterpathogens.org/book/characterization-of-diffuse-human-fecal-pollution-sources-with-land-use-information-strategic-water-sampling-quantitative-real-time-PCR (accessed on 14 October 2020).
- Dufour, A.; Wade, T.J.; Kay, D. Epidemiological studies on swimmer health effects associated with potential exposure to zoonotic pathogens in bathing beach water—A review. In Animal Waste, Water Quality and Human Health; Dufour, A., Bartram, J., Bos, R., Gannon, V., Eds.; World Health Organization: London, UK, 2012; Chapter 11; pp. 415–428. [Google Scholar]
- Converse, R.R.; Kinzelman, J.L.; Sams, E.A.; Hudgens, E.; Dufour, A.P.; Ryu, H.; Santo-Domingo, J.W.; Kelty, C.A.; Shanks, O.C.; Siefring, S.D.; et al. Dramatic improvements in beach water quality following gull removal. Environ. Sci. Technol. 2012, 46, 10206–10213. [Google Scholar] [CrossRef]
- Wang, J.D.; Solo-Gabriele, H.M.; Abdelzaher, A.M.; Fleming, L.E. Estimation of enterococci input from bathers and animals on a recreational beach using camera images. Mar. Pollut. Bull. 2010, 60, 1270–1278. [Google Scholar] [CrossRef]
- Strauch, D. Survival of pathogenic micro-organisms and parasites in excreta, manure and sewage sludge. Rev. Sci. Tech. Off. Int. Epiz. 1991, 10, 813–846. [Google Scholar] [CrossRef]
- Blasco, M.D.; Esteve, C.; Alcaide, E. Multiresistant waterborne pathogens isolated from water reservoirs and cooling systems. J. Appl. Microbiol. 2008, 105, 469–475. [Google Scholar] [CrossRef]
- Jin, Y.; Flury, M. Fate and transport of viruses in porous media. Adv. Agron. 2002, 77, 39–102. [Google Scholar]
- Chiarini, L.; Bevivino, A.; Dalmastri, C.; Tabacchioni, S.; Visca, P. Burkholderia cepacia complex species: Health hazards and biotechnological potential. Trends Microbiol. 2006, 14, 277–286. [Google Scholar] [CrossRef]
- Drevinek, P.; Holden, M.T.; Ge, Z.; Jones, A.M.; Ketchell, I.; Gill, R.T.; Mahenthiralingam, E. Gene expression changes linked to antimicrobial resistance, oxidative stress, iron depletion and retained motility are observed when Burkholderia cenocepacia grows in cystic fibrosis sputum. BMC Infect. Dis. 2008, 8, 121. [Google Scholar] [CrossRef]
- Peeters, C.; Depoorter, E.; Praet, J.; Vandamme, P. Extensive cultivation of soil and water samples yields various pathogens in patients with cystic fibrosis but not Burkholderia multivorans. J. Cyst. Fibros. 2016, 15, 769–775. [Google Scholar] [CrossRef][Green Version]
- Pandey, P.K.; Kass, P.H.; Soupir, M.L.; Biswas, S.; Singh, V.P. Contamination of water resources by pathogenic bacteria. AMB Expr. 2014, 4, 51. [Google Scholar] [CrossRef]
- WHO. Water Quality and Health. Drinking Water Chlorination—A Review of Disinfection Practices and Issues. 2014. Available online: http://www.waterandhealth.org/drinkingwater/wp.html (accessed on 8 June 2022).
- WHO. Water Sanitation and Health. 2015. Available online: http://www.who.int/water_sanitation_health/diseases (accessed on 8 June 2022).
- Bourque, D.; Vinetz, J. Illnesses associated with freshwater recreation during international travel. Curr. Infect. Dis. Rep. 2018, 20, 19. [Google Scholar] [CrossRef]
- Fayer, R.; Morgan, U.; Upton, S.J. Epidemiology of Cryptosporidium: Transmission, detection and identification. Int. J. Parasitol. 2000, 30, 1305–1322. [Google Scholar] [CrossRef]
- Romanowska-Duda, Z.; Mankiewicz-Boczek, J.; Tarczyńska, M.; Walter, Z.; Zalewski, M. The effect of toxic Cyanobacteria (Blue-Green Algae) on water plants and animal cells. Pol. J. Environ. Stud. 2002, 11, 561–566. [Google Scholar]
- Falconer, I.R. An overview of problems caused by toxic blue–green algae (cyanobacteria) in drinking and recreational water. Environ. Toxicol. 1999, 14, 5–12. [Google Scholar] [CrossRef]
- Figueras, S.; Ashbolt, N. Part 3 Bacteria. Aeromonas. In Global Water Pathogen Project 2019; Rose, J.B., Jiménez-Cisneros, B., Eds.; Michigan State University: East Lansing, MI, USA, 2019; Available online: http://www.waterpathogens.org/book/aeromonas (accessed on 19 June 2020).
- Garcia-Aljaro, C.; Momba, M.; Muniesa, M. Part 3 Bacteria Pathogenic members of Escherichia coli & Shigella spp. Shigellosis. In Global Water Pathogen Project 2019; Rose, J.B., Jiménez-Cisneros, B., Eds.; Michigan State University: East Lansing, MI, USA, 2019; Available online: http://www.waterpathogens.org/book/ecoli (accessed on 19 June 2020).
- Gibney, K.B.; O’Toole, J.; Sinclair, M.; Leder, K. Burden of Disease Attributed to Waterborne Transmission of Selected Enteric Pathogens, Australia, 2010. Am. J. Trop Med. Hyg. 2017, 96, 1400–1403. [Google Scholar] [CrossRef]
- Ahmed, W.; Sawant, S.; Huygens, F.; Goonetilleke, A.; Gardner, T. Prevalence and occurrence of zoonotic bacterial pathogens in surface waters determined by quantitative PCR. Water Res. 2009, 43, 4918–4928. [Google Scholar] [CrossRef]
- Wade, T.J.; Calderon, R.L.; Brenner, K.P.; Sams, E.; Beach, M.; Haugland, R.; Wymer, L.; Dufour, A.P. High Sensitivity of Children to Swimming-Associated Gastrointestinal Illness: Results Using a Rapid Assay of Recreational Water Quality. Epidemiology 2008, 19, 375–383. [Google Scholar] [CrossRef]
- Hunter, P.R. Drinking water and diarrhoeal disease due to Escherichia coli. J. Water Health 2003, 1, 65–72. [Google Scholar] [CrossRef]
- Dufour, A.P.; Behymer, T.D.; Cantú, R.; Magnuson, M.; Wymer, L.J. Ingestion of swimming pool water by recreational swimmers. J. Water Health 2017, 15, 429–437. [Google Scholar] [CrossRef]
- Medema, G.J.; Payment, P.; Dufour, A.; Robertson, W.; Waite, M.; Hunter, P.; Kirby, R.; Andersson, Y. Safe drinking water: An ongoing challenge. In Assessing Microbial Safety of Drinking Water Improving Approaches and Method; WHO & OECD, IWA Publishing: London, UK, 2003; pp. 11–45. [Google Scholar]
- Minor, L. The genus Salmonella. In The Prokaryotes: An Evolving Electronic Resource for the Microbiological Community, 3rd ed.; Dworkin, M., Falkow, S., Rosenberg, E., Eds.; Springer: New York, NY, USA, 2003; p. 314. [Google Scholar]
- Laube, S.; Farrel, A.M. Bacterial skin infections in the elderly: Diagnosis and treatment. Drugs Aging 2002, 19, 331–342. [Google Scholar] [CrossRef]
- Arvanitidou, M.; Kanellou, K.; Vagiona, D.G. Diversity of Salmonella spp. and fungi in Northern Greek rivers and their correlation to faecal pollution indicators. Environ. Res. 2005, 99, 278–284. [Google Scholar] [CrossRef]
- WHO (World Health Organization). Guidelines for Drinking-Water Quality, Incorporating 1st and 2nd Addenda, Volume 1, Recommendations, 3rd ed.; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Kumar, S.; Mukhopadhyay, P.; Chatterjee, M.; Bandyopadhyay, M.K.; Bandyopadhyay, M.; Ghosh, T.; Samaddar, D. Necrotizing fasciitis caused by Aeromonas caviae. Avicenna J. Med. 2012, 2, 94–96. [Google Scholar] [CrossRef]
- Tsai, Y.H.; Hsu, R.W.; Huang, T.J.; Hsu, W.H.; Huang, K.C.; Li, Y.Y.; Peng, K.T. Necrotizing soft-tissue infections and sepsis caused by Vibrio vulnificus compared with those caused by Aeromonas species. J. Bone Joint Surg. Am. 2007, 89, 631–636. [Google Scholar] [CrossRef]
- Hiransuthikul, N.; Tantisiriwat, W.; Lertutsahakul, K.; Vibhagool, A.; Boonma, P. Skin and soft tissue infections among tsunami survivors in southern Thailand. Clin. Infect. Dis. 2005, 41, 93–96. [Google Scholar] [CrossRef]
- Cebrián, F.; Montero, J.; Fernández, P. New approach to environmental investigation of an explosive legionnaires disease outbreak in Spain: Early identification of potential risk sources by rapid Legionella spp. immunosensing technique. BMC Infect. Dis. 2018, 18, 696. [Google Scholar] [CrossRef] [PubMed]
- Perkins, A.; Trimmier, M. Recreational waterborne illnesses: Recognition, treatment and prevention. Am. Fam. Physician 2017, 95, 554–560. [Google Scholar] [PubMed]
- Price, C.T.; Muszynski, M.J.; Zielinski, J.A.; Stewart, C. Motorboat propeller injuries: Report of thirteen cases with review of mechanism of injury and bacterial considerations. J. Trauma Treat. 2015, 4, 267. [Google Scholar] [CrossRef]
- Sorvillo, F.; Fujioka, K.; Nahlen, B.; Tonnery, M.; Kebabjian, R.; Mascola, L. Swimming-associated cryptosporidiosis. Am. J. Public Health 1992, 82, 742–744. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J. The Review on Antimicrobial Resistance. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. 2016. Available online: https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf (accessed on 14 October 2020).
- WHO. Global Action Plan on Antimicrobial Resistance 2015. Available online: https://www.who.int/antimicrobial-resistance/global-action-plan/en/ (accessed on 14 October 2020).
- CDC. Antibiotic Resistance Threats in the United States. U.S. Department of Health and Human Services, CDC: Atlanta, GA, USA, 2019. Available online: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf (accessed on 14 October 2020).
- European Environment Agency. European Bathing Water Quality in 2019. Available online: https://www.eea.europa.eu//publications/european-bathing-water-quality-in-2019 (accessed on 14 October 2020).
- Wolny-Koładka, K.; Lenart-Boroń, A. Phenotypic and molecular assessment of drug resistance profile and genetic diversity of waterborne Escherichia coli. Water Air Soil Pollut. 2016, 227, 146. [Google Scholar] [CrossRef][Green Version]
- Harnisz, M.; Korzeniewska, E. The prevalence of multidrug-resistant Aeromonas spp. in the municipal wastewater system and their dissemination in the environment. Sci. Total Environ. 2018, 626, 377–383. [Google Scholar] [CrossRef]
- Chojniak, J.; Jałowiecki, Ł.; Dorgeloh, E.; Hegedusova, B.; Ejhed, H.; Magnér, J.; Płaza, G. Application of the BIOLOG system for characterization of Serratia marcescens ss marcescens isolated from onsite wastewater technology (OSWT). Acta Biochim. Pol. 2015, 62, 799–805. [Google Scholar] [CrossRef]
- Lenart-Boroń, A.; Prajsnar, J.; Boroń, P. Survival and antibiotic resistance of bacteria in artificial snow produced from contaminated water. Water Environ. Res. 2017, 89, 2059–2069. [Google Scholar] [CrossRef]
- Giebułtowicz, J.; Tyski, S.; Wolinowska, R.; Grzybowska, W.; Zaręba, T.; Drobniewska, A.; Wroczyński, P.; Nałęcz-Jawecki, G. Occurrence of antimicrobial agents, drug-resistant bacteria, and genes in the sewage-impacted Vistula River (Poland). Environ. Sci. Pollut. Res. 2018, 25, 5788–5807. [Google Scholar] [CrossRef]
- Cantón, R.; Novais, A.; Valverde, A.; Machado, E.; Peixe, L.; Baquero, F.; Coque, T.M. Prevalence and spread of extended pectrum β-lactamase-producing Enterobacteriaceae in Europe. Clin. Microbiol. Infect. 2008, 14, 144–153. [Google Scholar] [CrossRef]
- EUCAST Guidelines for Detection of Resistance Mechanisms and Specific Resistances of Clinical and/or Epidemiological Importance 2017. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Resistance_mechanisms/EUCAST_detection_of_resistance_mechanisms_170711.pdf (accessed on 14 October 2020).
- Zhang, X.X.; Zhang, T.; Fang, H.H.P. Antibiotic resistance genes in water environment. Appl. Microbiol. Biotechnol. 2009, 82, 397–414. [Google Scholar] [CrossRef] [PubMed]
- Kummu, M.; de Moel, H.; Ward, P.J.; Varis, O. How Close Do We Live to Water? A Global Analysis of Population Distance to Freshwater Bodies. PLoS ONE 2011, 6, e20578. [Google Scholar] [CrossRef] [PubMed]
- Halliday, E.; Gast, R.J. Bacteria in beach sands: An emerging challenge in protecting coastal water quality and bather health. Environ. Sci. Technol. 2011, 45, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Directive 2006/7/EC of the European Parliament and the European Council of 15 February 2006 concerning the management of bathing water quality and repealing Directive 76/160/EEC. Off. J. Eur. Union 2013, L64/37.
- Regulation of the Polish Minister of Health of 17th January 2019 on the supervision of the quality of bathing water and the place used for bathing. J. Laws 86 2019, item 478, 5312–5317.
- Regulation of the Polish Minister of Health of 9th November 2015 on the requirements to be met by water in swimming pools. J. Laws 2015.
- Straub, T.M.; Chandler, D.P. Towards a unified system for detecting waterborne pathogens. J. Microbiol. Methods 2003, 53, 185–197. [Google Scholar] [CrossRef]
- Ramírez-Castillo, F.Y.; Loera-Muro, A.; Jacques, M.; Garneau, P.; Avelar-González, F.J.; Harel, J.; Guerrero-Barrera, A.L. Waterborne pathogens: Detection methods and challenges. Pathogens 2015, 4, 307–334. [Google Scholar] [CrossRef]
- McLellan, S.L.; Eren, A.M. Discovering new indicators of fecal pollution. Trends Microbiol. 2014, 22, 697–706. [Google Scholar] [CrossRef]
- Naughton, C.; Mihelcic, J.R. Introduction to the Importance of Sanitation. In Global Water Pathogen Project 2017; Rose, J.B., Jiménez-Cisneros, B., Eds.; Michigan State University: East Lansing, MI, USA, 2017; Available online: http://www.waterpathogens.org/book/introduction (accessed on 5 December 2020).
- Gromiec, M. A new paradigum "Nutriens-Energy-Water (N-E-W)" for water- sewerage works. In Water Supply and Water Quality T.1; Dymaczewski, Z., Jeż-Walkowiak, J., Eds.; PZITS Wielkopolska Branch: Poznań, Poland, 2012; Available online: https://www.biblos.pk.edu.pl/ST/2016/12/100000296498/100000296498_Dymaczewski_ZaopatrzenieWWode.pdf (accessed on 2 June 2022).
- Sano, D.; Haas, C.N.; Rose, J.B. A QMRA Framework for Sanitation Treatment Decisions. In Global Water Pathogen Project; Rose, J.B., Jiménez-Cisneros, B., Eds.; Michigan State University: East Lansing, MI, USA, 2019; Available online: http://www.waterpathogens.org/book/a-QMRA-framework-for-sanitation-treatment-decisions (accessed on 5 December 2020).
- Kaushik, M.; Kumar, S.; Kapoor, R.K.; Gulati, P. Integrons and antibiotic resistance genes in water-borne pathogens: Threat detection and risk assessment. J. Med. Microbiol. 2019, 68, 679–692. [Google Scholar] [CrossRef]
| Species | Category | Literature Source |
|---|---|---|
| Legionella spp. | water-based | [28] |
| Salmonella spp. | waterborne | |
| Vibrio vulnificus | waterborne/water-based | |
| Mycobacterium marinum | water-based | |
| Edwardsiella tarda | waterborne | |
| Burkholderia pseudomallei | water-based | |
| Aeromonas spp. | waterborne/water-based | |
| Campylobacter spp. | waterborne | |
| other Gram-negative bacilli/rods * | waterborne/water-based | |
| Leptospira spp. | water-based | |
| Schistosoma spp. | water-based | |
| Giardia duodentalis | waterborne | |
| Naegleria fowleri | water-based | |
| Cryptosporidium | waterborne | [29] |
| Cyanobacteria | waterborne/water-based | [30,31] |
| Legionella pneumophila | water-based | [4] |
| Mycobacterium avium complex | ||
| Pseudomonas aeruginosa | ||
| Aeromonas spp. | waterborne | [32] |
| Enteroinvasive Escherichia coli (EIEC) | water-based | [33] |
| Escherichia coli O157:H7 | ||
| Shigella spp. | ||
| Salmonella spp. | waterborne | [34] |
| Pathogen | Infectious Dose | Literature |
|---|---|---|
| Cryptosporidium parvum | 87 oocysts | [29] |
| Salmonella typhi | 105 cells | [35] |
| Salmonella typhimurium | 109 cells | |
| Campylobacter jejuni | 500 cells | |
| Enterohaemorrhagic E. coli (EHEC) O157:H7 | 10–100 cells | |
| Enterohaemorrhagic E. coli (EHEC) | 102–106 cells | [37] |
| Enteroinvasive E. coli (EIEC) | 106–1010 cells | |
| Enterotoxigenic E. coli (ETEC) | 108–1010 cells | |
| Enteropathogenic E. coli (EPEC) | 108–1010 cells |
| Disease/Ailment | Etiological Factor | Source of Microorganisms | Number of Cases | Treatment/Results | Literature |
|---|---|---|---|---|---|
| wound infection | Aeromonas caviae | trauma due to foreign body to the foot | 1 | treatment: amoxicillin with clavulanic acid (deterioration) hospitalization: ceftriaxone, amikacin full recovery | [44] |
| necrotizing soft-tissue infection | Aeromonas spp. | contaminated water | 15 A. hydrophila-10 A. sobria-4 A. caviae-1 | treatment: ceftriaxone or ceftazidime combined with doxycycline or gentamicin results: 5 limb amputations, sepsis, skin lesions, hypotension; mortality rate: 27% | [45] |
| skin and soft-tissue infection | Aeromonas spp. | contamination of water after tsunami wave | 145 A. hydrophila-104 A. veronii biovar sobria-41 | most cases resistant to amoxicillin-clavulanate and first-generation cephalosporins | [46] |
| Escherichia coli | 116 | susceptible to antibiotics | |||
| Klebsiella pneumoniae | 93 | susceptible to antibiotics | |||
| Proteus spp. | 47 P. vulgaris-27 P. mirabilis-20 | most cases resistant to amoxicillin-clavulanate and first-generation cephalosporins | |||
| Pseudomonas aeruginosa | 77 | most cases resistant to amoxicillin-clavulanate and first-generation cephalosporins | |||
| Staphylococcus spp. | 17 S. aureus-11 (including 2 MRSA cases) CoNS-6 | empirical therapy was undertaken-amoxicillin-clavulanate and first-generation cephalosporins | |||
| pneumonia | Legionella pneumophila serogroup 1 Pontiac Philadelphia ST899 | contaminated water supply network | 277 | not mentioned | [47] |
| pneumonia | Legionella spp. | fresh water | - | quinolone | [48] |
| multiple complex deep lacerations right leg | Pseudomonas fluorescens; Klebsiella pneumoniae | fresh water- fall and struck by a propeller of a motorboat | 1 | hospitalization: piperacillin-tazobactam, vancomycin | [49] |
| Candida tropicalis | hospitalization: cefazolin, gentamicin | ||||
| leg lacerations, foot open fractures | Staphylococcus aureus (MSSA) | fresh water-wakebording | 1 | hospitalization: cefazolin, gentamicin, ciprofloxacin | |
| forearm lacerations | Staphylococcus aureus (MSSA) | fresh water-fall from a jet ski | 1 | hospitalization: clindamycin, gentamicin | |
| legs and back multiple lacerations | Acinetobacter baumannii, MRSA, MSSA | fresh water | 1 | hospitalization: piperacillin-tazobactam | |
| watery diarrhea, abdominal cramping, fever | Cryptosporidium | water in a swimming pool | 5 | 2 patients required hospitalization | [50] |
| Microorganism | Source of Microorganism | Presented Antibiotic Resistance | Literature |
|---|---|---|---|
| Aeromonas spp. | municipal wastewater system | over 72% classified as multidrug resistant most isolates were resistant to beta-lactams, tetracyclines and aminoglycosides | [56] |
| Serratia marcescens | aerated filter system of onsite wastewater treatment facility | loss of sensitivity for 5 antibiotics: lomefloxacin, enoxacin (fluoroquinolones), nalidixic acid (quinolone), paromomycin (aminoglycoside), novobiocin | [57] |
| Escherichia coli | recreational water | 53% strains resistant to ampicillin 56% strains resistant to ticarcillin | [55] |
| Escherichia coli | water and contaminated artificial snow | 74.19% E. coli isolated from snow were resistant to ampicillin and 51.61% isolates to amoxicillin-clavulanate 45% of isolates classified as multidrug resistant (MDR) | [58] |
| Enterococcus faecalis, Enterococcus faecium, Gram- negative rods | river | 13% of E. faecalis isolates resistant to fluoroquinolones, tetracyclines, aminoglycosides, 31% of E. faecium resistant to beta-lactams, fluoroquinolones, tetracyclines and aminoglycosides, nearly 50% of Gram-negative isolates resistant to beta-lactams | [59] |
| Parameter | Excellent Quality | Good Quality | Sufficient Quality |
|---|---|---|---|
| Intestinal enterococci (cfu/100 mL) | 200 * | 400 * | 330 ** |
| Escherichia coli (cfu/100 mL) | 500 * | 1000 * | 900 ** |
| The Highest Permitted Number of Microorganisms (cfu—Colony Forming Units or MPN—the most Probable Number) | |||||
|---|---|---|---|---|---|
| Parameter | Water Introduced into the Pool Basin from the Circulation System a | Water in the Pool Basin * | Water in Swimming Pool Basins Equipped with Devices Generating Water-air Aerosol b | Water in Pool Basins Made Available for Swimming Lessons for Infants and Toddlers up to 3 Years of Age | Water in Showers |
| Escherichia coli per 100 mL of water | 0 | 0 | 0 | 0 | – |
| Pseudomonas aeruginosa per 100 mL of water | 0 | 0 | 0 | 0 | – |
| Total number of microorganisms at 36 ± 2 °C after 48 h per 1 mL of water c | 20 | 100 | 100 | 100 | – |
| Coagulase positive staphylococci per 100 mL of water | – | – | – | 0 | – |
| Legionella spp. per 100 mL of water | 0 | 0 d | 0 | 0 | <100 e |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stec, J.; Kosikowska, U.; Mendrycka, M.; Stępień-Pyśniak, D.; Niedźwiedzka-Rystwej, P.; Bębnowska, D.; Hrynkiewicz, R.; Ziętara-Wysocka, J.; Grywalska, E. Opportunistic Pathogens of Recreational Waters with Emphasis on Antimicrobial Resistance—A Possible Subject of Human Health Concern. Int. J. Environ. Res. Public Health 2022, 19, 7308. https://doi.org/10.3390/ijerph19127308
Stec J, Kosikowska U, Mendrycka M, Stępień-Pyśniak D, Niedźwiedzka-Rystwej P, Bębnowska D, Hrynkiewicz R, Ziętara-Wysocka J, Grywalska E. Opportunistic Pathogens of Recreational Waters with Emphasis on Antimicrobial Resistance—A Possible Subject of Human Health Concern. International Journal of Environmental Research and Public Health. 2022; 19(12):7308. https://doi.org/10.3390/ijerph19127308
Chicago/Turabian StyleStec, Joanna, Urszula Kosikowska, Mariola Mendrycka, Dagmara Stępień-Pyśniak, Paulina Niedźwiedzka-Rystwej, Dominika Bębnowska, Rafał Hrynkiewicz, Joanna Ziętara-Wysocka, and Ewelina Grywalska. 2022. "Opportunistic Pathogens of Recreational Waters with Emphasis on Antimicrobial Resistance—A Possible Subject of Human Health Concern" International Journal of Environmental Research and Public Health 19, no. 12: 7308. https://doi.org/10.3390/ijerph19127308
APA StyleStec, J., Kosikowska, U., Mendrycka, M., Stępień-Pyśniak, D., Niedźwiedzka-Rystwej, P., Bębnowska, D., Hrynkiewicz, R., Ziętara-Wysocka, J., & Grywalska, E. (2022). Opportunistic Pathogens of Recreational Waters with Emphasis on Antimicrobial Resistance—A Possible Subject of Human Health Concern. International Journal of Environmental Research and Public Health, 19(12), 7308. https://doi.org/10.3390/ijerph19127308








