Rapid Detection of Clostridium botulinum in Food Using Loop-Mediated Isothermal Amplification (LAMP)
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents and Instruments
2.2. Selection of Target DNA Fragment
2.3. Design and Determination of the Optimal LAMP Primers
2.4. LAMP Reactions
2.5. Detection of the Amplification Products of LAMP Reactions
2.6. Determination of the Optimal Temperature for LAMP Reaction
2.7. Specificity of LAMP Reactions
2.8. Sensitivity of LAMP Assay and PCR Method
2.9. Validation of the Optimized LAMP Assay and Potential Kit Assembly
3. Results
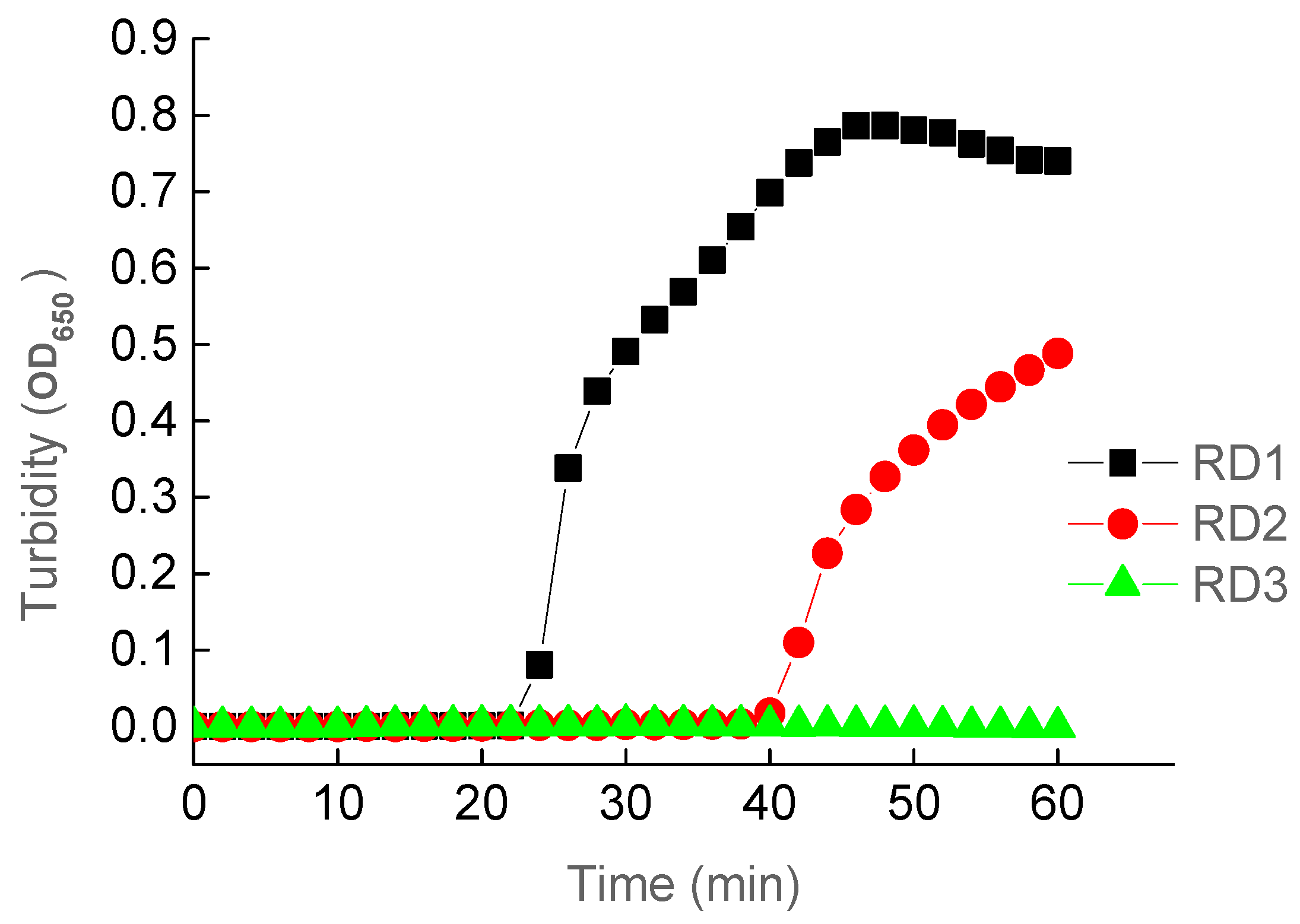
3.1. The Optimal Primers for LAMP Reactions
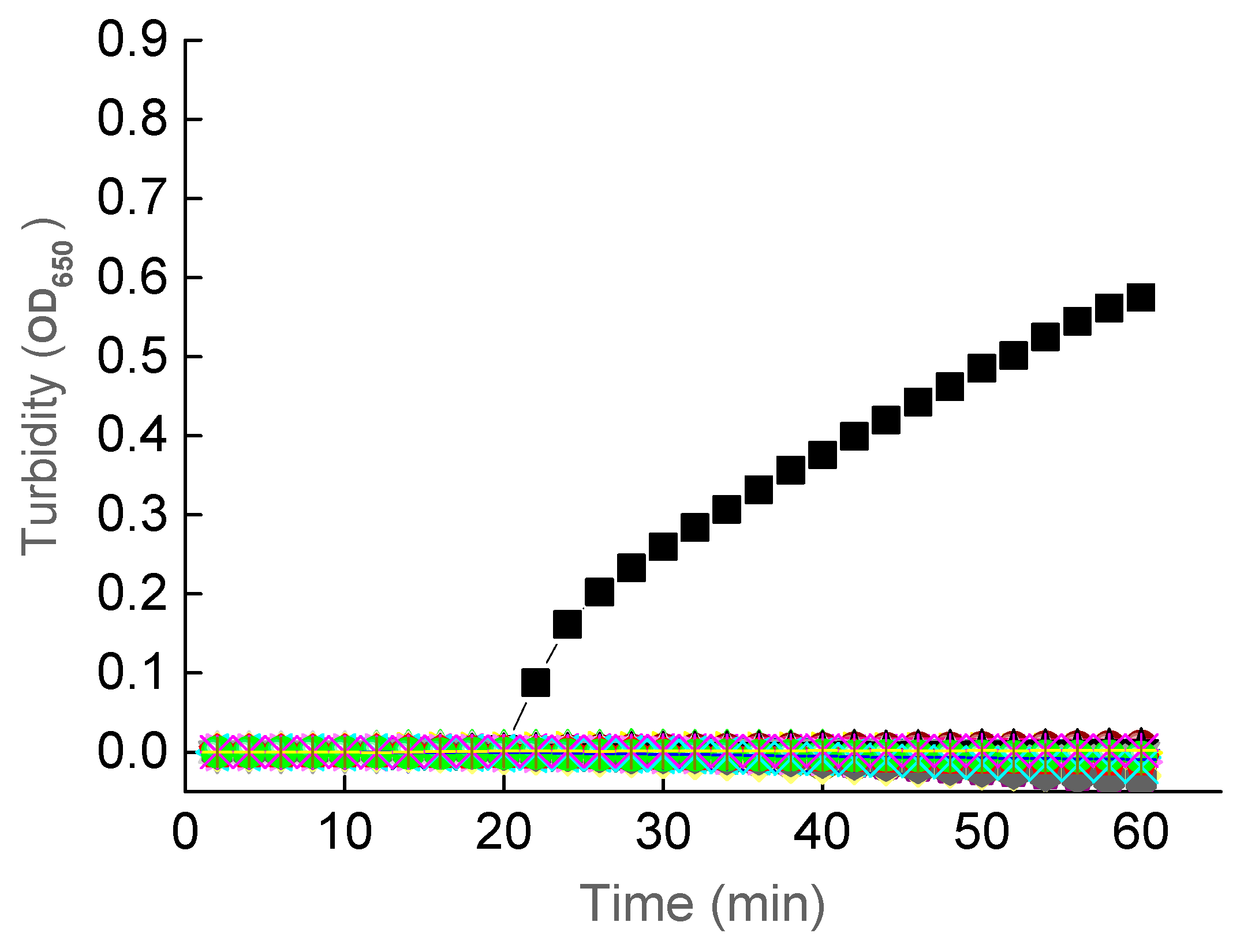
3.2. The Optimal Temperature for LAMP Reactions
3.3. Specificity of the LAMP Assay
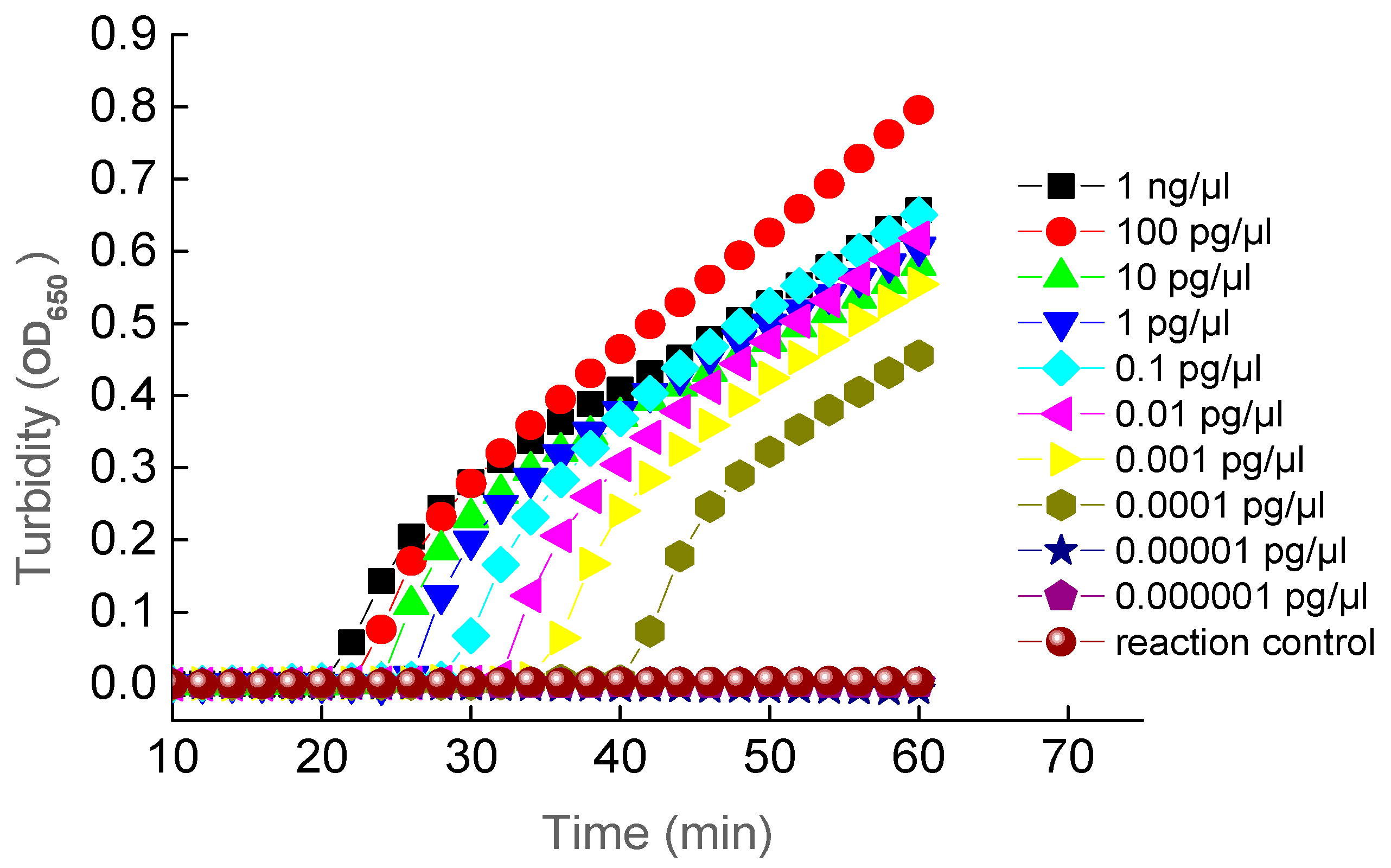
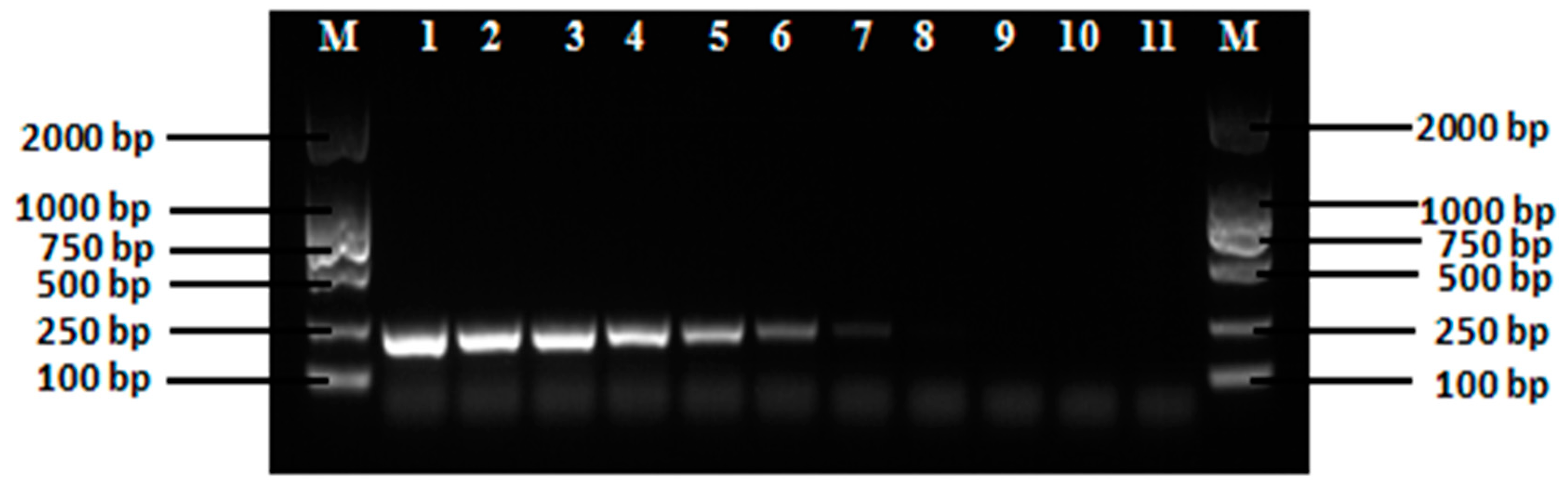
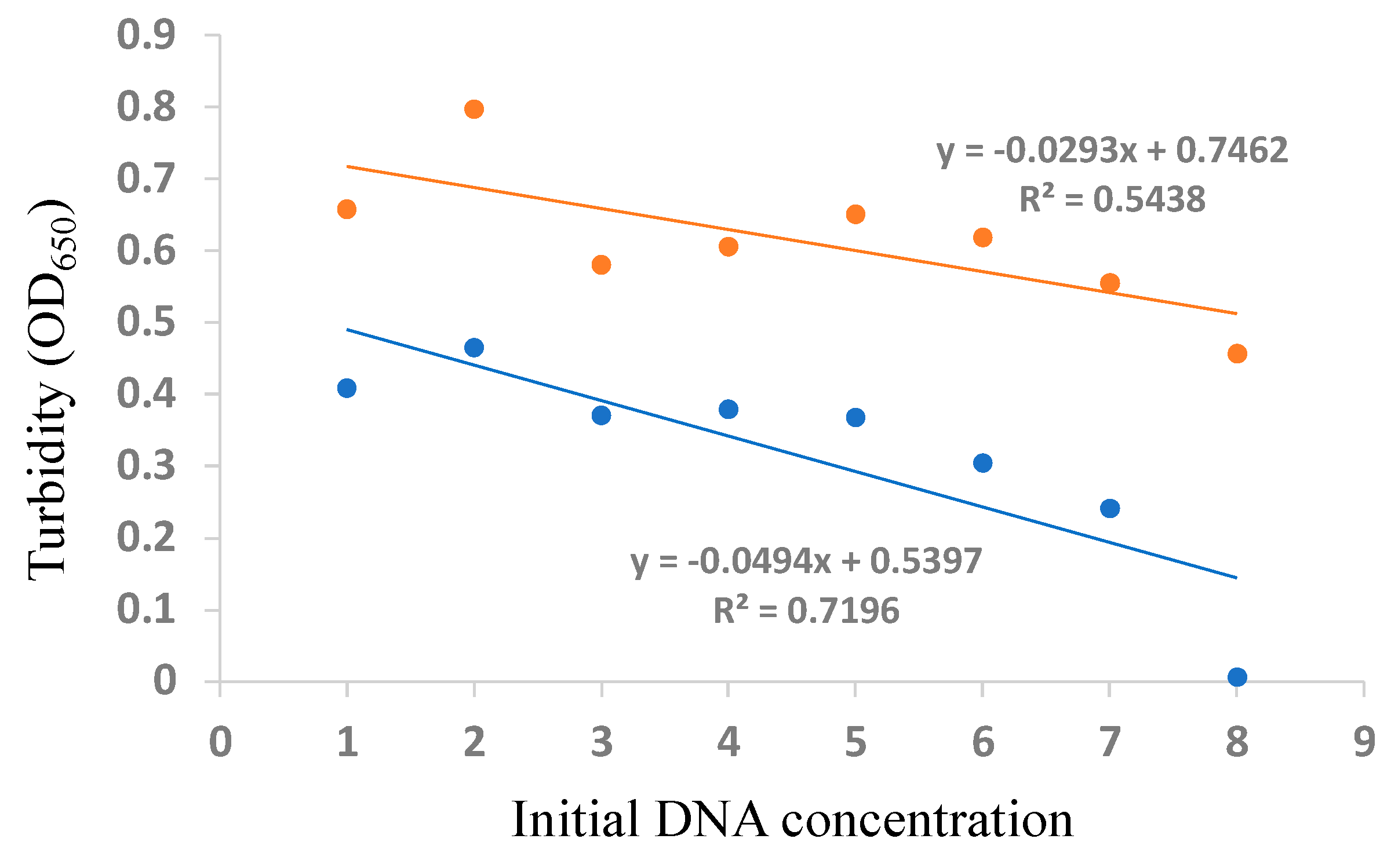
3.4. Sensitivity of the LAMP Assay and PCR
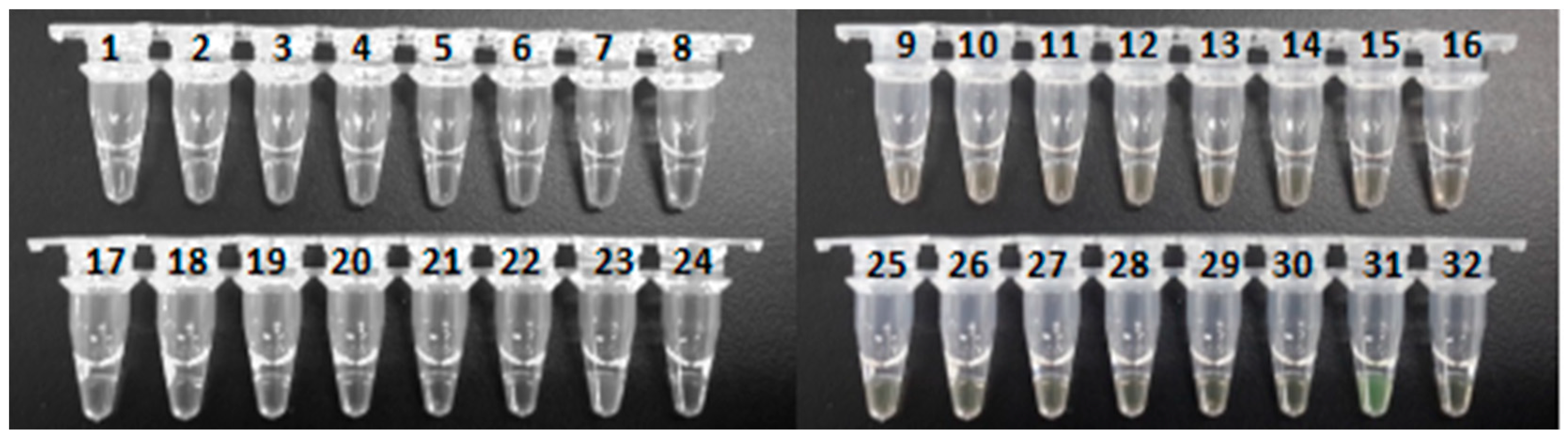
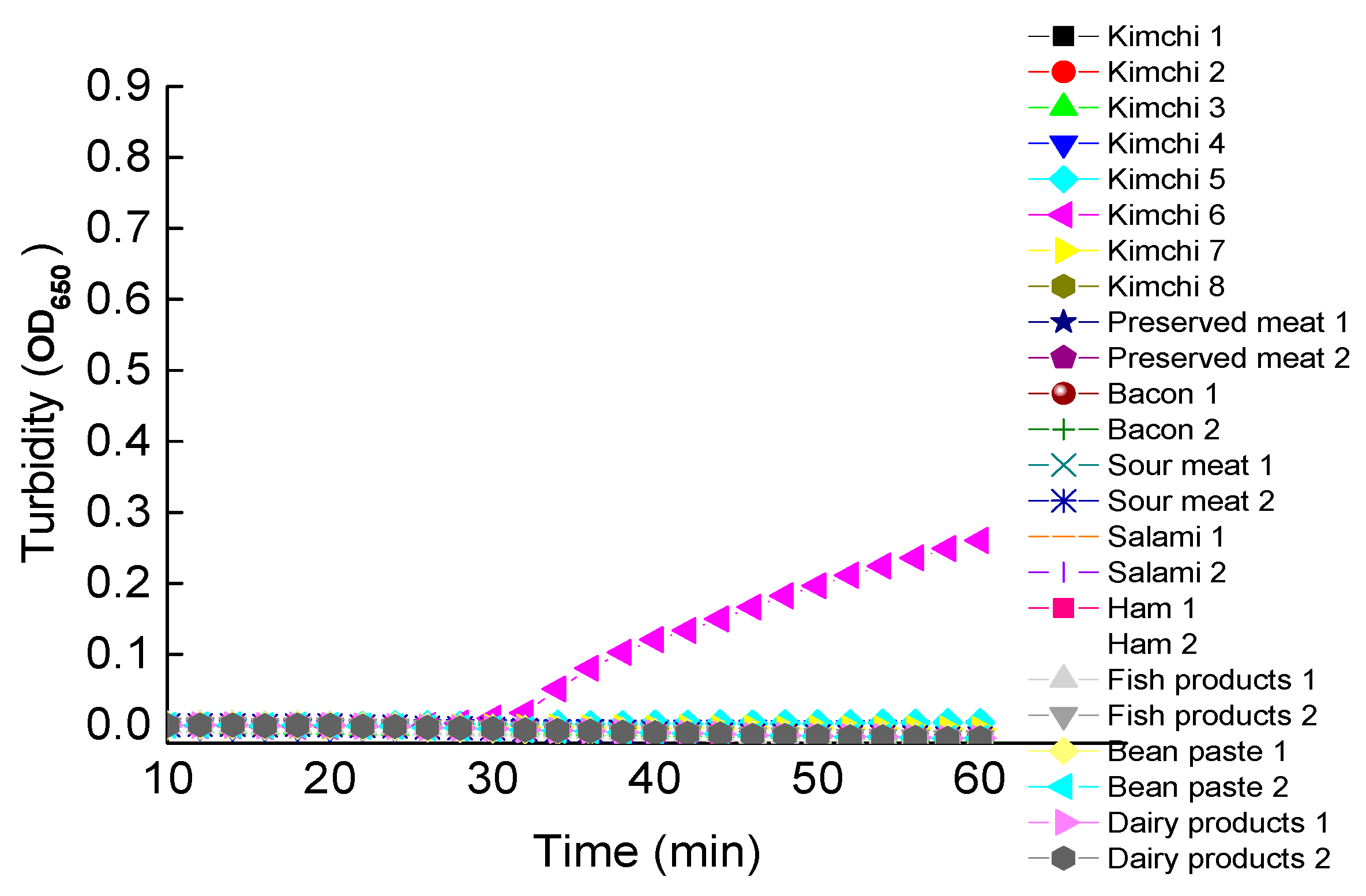
3.5. Verification of the Established LAMP Assay
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shukla, H.D.; Sharma, S.K. Clostridium botulinum: A bug with beauty and Weapon. Crit. Rev. Microbiol. 2005, 31, 11–18. [Google Scholar] [CrossRef]
- Dutta, S.R.; Passi, D.; Singh, M.; Singh, P.; Sharma, S.; Sharma, A. Botulinum toxin the poison that heals: A brief review. Natl. J. Maxillofac Surg. 2016, 7, 10–16. [Google Scholar]
- Poulain, B.; Popoff, M.R. Why are botulinum neurotoxin-producing bacteria so diverse and botulinum neurotoxins so toxic? Toxins 2019, 11, 34. [Google Scholar] [CrossRef] [PubMed]
- Sobel, J. Botulism. Clin. Infect. Dis. 2005, 41, 1167–1173. [Google Scholar] [CrossRef] [PubMed]
- Gu, S.; Rumpel, S.; Zhou, J.; Strotmeier, J.; Bigalke, H.; Perry, K.; Shoemaker, C.B.; Rummel, A.; Jin, R. Botulinum neurotoxin is shielded by NTNHA in an interlocked complex. Science 2012, 335, 977–981. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Masuyer, G.; Zhang, J.; Shen, Y.; Lundin, D.; Henriksson, L.; Miyashita, S.; Martrnez-Carranza, M.; Dong, M.; Stenmark, P. Identification and characterization of a novel botulinum neurotoxin. Nat. Commun. 2017, 8, 14130. [Google Scholar] [CrossRef]
- Hatheway, C.L. Closridium botulinum: Ecology and Control in Foods; Hauschild, A.H.W., Dodds, K.L., Eds.; Marcel Dekker, Inc.: New York, NY, USA, 1993; pp. 3–20. [Google Scholar]
- Peck, M.W.; Smith, T.J.; Anniballi, F.; Austin, J.W.; Bano, L.; Bradshaw, M.; Cuervo, P.; Cheng, L.W.; Derman, Y.; Dorner, B.G.; et al. Historical perspectives and guidelines for botulinum neurotoxin subtype nomenclature. Toxins 2017, 9, 38. [Google Scholar] [CrossRef]
- Kukreja, R.V.; Singh, B.R. Comparative role of neurotoxin-associated proteins in the structural stability and endopeptidase activity of botulinum neurotoxin complex types A and E. Biochemistry 2007, 46, 14316–14324. [Google Scholar] [CrossRef]
- Popoff, M.R. Ecology of neurotoxigenic strains of clostridia. Curr. Top. Microbiol. Immunol. 1995, 195, 1–29. [Google Scholar]
- Hatheway, C.L. Toxigenic clostridia. Clin. Microbiol. Rev. 1990, 3, 66–98. [Google Scholar] [CrossRef]
- Chellapandi, P.; Prisilla, A. Clostridium botulinum type A-virulome-gut interactions: A systems biology insight. Hum. Microbiome J. 2018, 7–8, 15–22. [Google Scholar] [CrossRef]
- Cagan, E.; Peker, E.; Dogan, M.; Caksen, H. Infant botulism. Eur. J. Med. 2010, 42, 92–94. [Google Scholar] [CrossRef]
- Xin, W.; Huang, Y.; Ji, B.; Li, P.; Wu, Y.; Liu, J.; Wang, X.; Yang, H.; Kang, L.; Gao, S.; et al. Identification and characterization of Clorstridium botulinum strains associated with an infant botulism case in China. Anaerobe 2019, 55, 1–7. [Google Scholar] [CrossRef]
- Grenda, T.; Kwiatek, K. Application of molecular-biology methods to the diagnosis of botulism in mallard ducks. Bull. Vet. Inst. Pulawy 2009, 53, 365–368. [Google Scholar]
- Grenda, T.; Kukier, E.; Goldsztejn, M.; Kozieł, N.; Kwiatek, K. Botulism: Current problem in veterinary medicine. Med. Weter. 2016, 72, 152–156. [Google Scholar]
- Son, K.; Kim, Y.K.; Woo, C.; Wang, S.J.; Kim, Y.; Oem, J.K.; Jheong, W.; Jeong, J. Minimizing an outbreak of avian botulism (Clostridium botulinum type C) in Incheon, South Korea. J. Vet. Med. Sci. 2018, 80, 553–556. [Google Scholar] [CrossRef] [PubMed]
- Matović, K.; Mišić, D.; Karabasil, N.; Nedić, N.; Dmitrić, M.; Jevtić, G. Clostridium botulinum spores in European honey bees from Serbia. J. Apic. Res. 2019, 58, 420–426. [Google Scholar] [CrossRef]
- Grenda, T.; Grabczak, M.; Sieradzki, Z.; Kwiatek, K.; Pohorecka, K.; Skubida, M.; Bober, A. Clostridium botulinum spores in Polish honey samples. J. Vet. Sci. 2018, 19, 635–642. [Google Scholar] [CrossRef]
- Mustafina, R.; Maikanov, B.; Wiśniewski, J.; Tracz, M.; Anusz, K.; Grenda, T.; Kukier, E.; Goldsztejn, M.; Kwiatek, K. Contamination of honey produced in the Republic of Kazakhstan with Clostridium botulinum. Bull. Vet. Inst. Pulawy 2015, 59, 241–246. [Google Scholar] [CrossRef]
- Maier, M.B.; Schweiger, T.; Lenz, C.A.; Vogel, R.F. Inactivation of non-proteolytic Clostridium botulinum type E in low-acid foods and phosphate buffer by heat and pressure. PLoS ONE 2018, 13, e0200102. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, T.; Haque, S.; Somvanshi, P. In silico identification of molecular mimics involved in the pathogenesis of Clostridium botulinum ATCC 3502 strain. Microb. Pathog. 2018, 121, 238–244. [Google Scholar] [CrossRef]
- Bhardwaj, T.; Somvanshi, P. A computational approach using mathematical modeling to assess the peptidoglycan biosynthesis of Clostridium botulinum ATCC 3502 for potential drug targets. Gene Rep. 2018, 12, 179–186. [Google Scholar] [CrossRef]
- Davies, J.R.; Rees, J.; Liu, S.M.; Acharya, K.R. High resolution crystal structures of Clostridium botulinum neurotoxin A3 and A4 binding domains. J. Struct. Biol. 2018, 202, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Eivazzadeh-Keihan, R.; Pashazadeh-Panahi, P.; Baradaran, B.; de la Guardia, M.; Hejazi, M.; Sohrabi, H.; Mokhtarzadeh, A.; Maleki, A. Recent progress in optical and electrochemical biosensors for sensing of Clostridium botulinum neurotoxin. Trends Anal. Chem. 2018, 103, 184–197. [Google Scholar] [CrossRef]
- Walper, S.A.; Aragoneś, G.L.; Sapsford, K.E.; Brown, C.W., III; Rowland, C.E.; Breger, J.C.; Medintz, I.L. Detecting biothreat agents: From current diagnostics to developing sensor technologies. ACS Sens. 2018, 3, 1894–2024. [Google Scholar] [CrossRef]
- Wangroongsarb, P.; Kohda, T.; Jittaprasartsin, C.; Suthivarakom, K.; Kamthalang, T.; Umeda, K.; Sawanpanyalert, P.; Kozaki, S.; Ikuta, K. Molecular characterization of Clostridium botulinum isolates from foodborne outbreaks in Thailand, 2010. PLoS ONE 2014, 9, e77792. [Google Scholar] [CrossRef] [PubMed]
- Carter, A.T.; Peck, M.W. Genomes, neurotoxins and biology of Clostridium botulinum Group I and Group II. Res. Microbiol. 2015, 166, 303–317. [Google Scholar] [CrossRef]
- Scalfaro, C.; Auricchio, B.; De Medici, D.; Anniballi, F. Foodborne botulism: An evolving public health challenge. Infect. Dis. 2019, 51, 97–101. [Google Scholar] [CrossRef]
- Lindstrom, M.; Korkeala, H. Laboratory diagnostics of botulism. Clin. Microbiol. Rev. 2006, 19, 298–314. [Google Scholar] [CrossRef] [PubMed]
- Grenda, T.; Kukier, E.; Kwiatek, K. Methods and difficulties in detection of Clostridium botulinum and its toxins. Pol. J. Vet. Sci. 2014, 17, 195–205. [Google Scholar] [CrossRef]
- Maslanka, S.E.; Lúquez, C.; Dykes, J.K.; Tepp, W.H.; Pier, C.L.; Pellett, S.; Raphael, B.H.; Kalb, S.R.; Barr, J.R.; Rao, A.; et al. A novel botulinum neurotoxin, previously reported as serotype H, has a hybrid-like structure with regions of similarity to the structures of serotypes A and F and is neutralized with serotype A antitoxin. J. Infect. Dis. 2016, 213, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Thirunavukkarasu, N.; Johnson, E.; Pillai, S.; Hodge, D.; Stanker, L.; Wentz, T.; Singh, B.; Venkateswaran, K.; McNutt, P.; Adler, M.; et al. Botulinum neurotoxin detection methods for public health response and surveillance. Front. Bioeng. Biotechnol. 2018, 6, 80. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.K.; Lin, N.H.; Griese, S.E.; Chatham-Stephens, K.; Badell, M.L.; Sobel, J. Clinical Criteria to Trigger Suspicion for Botulism: An evidence-based tool to facilitate timely recognition of suspected cases during sporadic events and outbreaks. Clin. Infect. Dis. 2018, 2018 (Suppl. 1), 66. [Google Scholar] [CrossRef]
- Hobbs, R.J.; Thomas, C.A.; Haliwell, J.; Gwenin, C.D. Rapid detection of botulinum neurotoxins—A review. Toxins 2019, 11, 418. [Google Scholar] [CrossRef]
- Nepal, M.R.; Jeong, T.C. Alternative methods for testing botulinum toxin: Current status and future perspectives. Biomol. Ther. 2020, 28, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.K.; Ferreira, J.L.; Eblen, B.S.; Whiting, R.C. Detection of type A, B, E, and F Clostridium botulinum neurotoxins in foods by using an amplified enzyme-linked immunosorbent assay with digoxigenin-labeled antibodies. Appl. Environ. Microbiol. 2006, 72, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Maslanka, S.E.; Lúquez, C.; Raphael, B.H.; Dykes, J.K.; Joseph, L.A. Utility of botulinum toxin ELISA A, B, E, F kits for clinical laboratory investigations of human botulism. Botulinum J. 2011, 2, 72–92. [Google Scholar] [CrossRef]
- De Medici, D.; Anniballi, F.; Wyatt, G.M.; Lindstrom, M.; Messelhaußer, U.; Aldus, C.F.; Delibato, E.; Korkeala, H.; Peck, M.W.; Fenicia, L. Multiplex PCR for detection of botulinum neurotoxin-producing Clostridia in clinical, food, and environmental samples. Appl. Environ. Microbiol. 2009, 75, 6457–6461. [Google Scholar] [CrossRef]
- Singh, A.K.; Stanker, L.H.; Sharma, S.K. Botulinum neurotoxin: Where are we with detection technologies? Crit. Rev. Microbiol. 2013, 39, 43–56. [Google Scholar] [CrossRef]
- Koh, C.Y.; Schaff, U.Y.; Piccini, M.E.; Stanker, L.H.; Cheng, L.W.; Ravichandran, E.; Singh, B.R.; Sommer, G.; Singh, A.K. Centrifugal microfluidic platform for ultrasensitive detection of botulinum toxin. Anal. Chem. 2015, 87, 922–928. [Google Scholar] [CrossRef]
- Babrak, L.; Lin, A.; Stanker, L.H.; McGarvey, J.; Hnasko, R. Rapid microfluidic assay for the detection of botulinum neurotoxin in animal sera. Toxins 2016, 8, 13. [Google Scholar] [CrossRef]
- Cheng, W.L.; Land, M.K.; Tam, C.; Brandon, D.L.; Stanker, H.L. Technologies for Detecting Botulinum Neurotoxins in Biological and Environmental Matrices; InTech: London, UK, 2016; pp. 125–144. [Google Scholar]
- Huang, Y.; Shi, Y.; Ye, C.; Xu, X. Establishment of real-time PCR assays for rapid detection of Clostridium botulinum type A and B. Dis. Surveill. 2019, 34, 844–848. [Google Scholar]
- Wu, L.; Li, Y.; Yan, A.; Jiang, Z. Detection of Clostridium botulinum type A and B strains in food poisoning sample by real-time fluorescent quantitative PCR. Chin. J. Health Lab. Technol. 2018, 28, 163–165. [Google Scholar]
- Lindstrom, M.; Keto, R.; Markkula, A.; Nevas, M.; Hielm, S.; Korkeala, H. Multiplex PCR assay for detection and identification of Clostridium botulinum types A, B, E, and F in food and fecal material. Appl. Environ. Microbiol. 2001, 67, 5694–5699. [Google Scholar] [CrossRef] [PubMed]
- Fach, P.; Micheau, P.; Mazuet, C.; Perelle, S.; Popoff, M. Development of real-time PCR tests for detecting botulinum neurotoxins A, B, E, F producing Clostridium botulinum, Clostridium baratii and Clostridium butyricum. J. Appl. Microbiol. 2009, 107, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Raphael, B.H.; Anreadis, J.D. Real-time PCR detection of the nontoxic nonhemagglutinin gene as a rapid screening method for bacterial isolates harboring the botulinum neurotoxin (A-G) gene complex. J. Microbiol. Methods 2007, 71, 343–346. [Google Scholar] [CrossRef]
- Williamson, C.H.D.; Vazquez, A.J.; Hill, K.; Smith, T.J.; Nottingham, R.; Stone, N.E.; Sobek, C.J.; Cocking, J.H.; Fernández, R.A.; Caballero, P.A.; et al. Differentiating botulinum neurotoxin-producing Clostridia with a simple, multiplex PCR assay. Appl. Environ. Microbiol. 2017, 83, e00806-17. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.J.; Skerry, J.C.; Smith, T.J.; Arnon, S.S.; Douek, D.C. Universal and specific quantitative detection of botulinum neurotoxin genes. BMC Microbiol. 2010, 10, 267. [Google Scholar] [CrossRef] [PubMed]
- Maikanov, B.; Mustafina, R.; Auteleyeva, L.; Wisniewski, J.; Anusz, K.; Grenda, T.; Kwiatek, K.; Goldsztejn, M.; Grabczak, M. Clostridium botulinum and Clostridium perfringens occurrence in Kazakh honey samples. Toxins 2019, 11, 472. [Google Scholar] [CrossRef] [PubMed]
- Peck, M.W.; Plowman, J.; Aldus, C.F.; Wyatt, G.M.; Izurieta, W.P.; Stringer, S.C.; Barker, G.C. Development and application of a new method for specific and sensitive enumeration of spores of nonproteolytic Clostridium botulinum types B, E, and F in foods and food materials. Appl. Environ. Microbiol. 2010, 76, 6607–6614. [Google Scholar] [CrossRef] [PubMed]
- Le Maréchal, C.; Fourour, S.; Ballan, V.; Rouxel, S.; Souillard, R.; Chemaly, M. Detection of Clostridium botulinum group III in environmental samples from farms by real-time PCR using four commercial DNA extraction kits. BMC Res. Notes 2018, 11, 441. [Google Scholar] [CrossRef] [PubMed]
- Notomi, T.; Okayama, H.; Masubuchi, H.; Yonekawa, T.; Watanabe, K.; Hase, T. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 2000, 28, 63. [Google Scholar] [CrossRef]
- Liu, W.; Huang, S.; Liu, N.; Dong, D.; Yang, Z.; Tang, Y.; Ma, W.; He, X.; Ao, D.; Xu, Y.; et al. Establishment of an accurate and fast detection method using molecular beacons in loop-mediated isothermal amplification assay. Sci. Rep. 2017, 7, 40125. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, T.; Kurosaki, Y.; Fujinami, Y.; Takizawa, T.; Yasuda, J. Rapid and simple detection of Clostridium botulinum types A and B by loop-mediated isothermal amplification. J. Appl. Microbiol. 2009, 106, 1252–1259. [Google Scholar] [CrossRef]
- Liu, W.; Zou, D.; Li, Y.; Wang, X.; He, X.; Wei, X.; Shao, C.; Li, X.; Shang, W.; Yu, K.; et al. Sensitive and rapid detection of the New Delhi metallo-beta-lactamase gene by loop-mediated isothermal amplification. J. Clin. Microbiol. 2012, 50, 1580–1585. [Google Scholar] [CrossRef]
- Li, X.; Liu, W.; Wang, J.; Zou, D.; Wang, X.; Yang, Z.; Yin, Z.; Gui, Q.; Shang, W.; Li, H.; et al. Rapid detection of Trichinella spiralis larvae in muscles by loop-mediated isothermal amplification. Int. J. Parasitol. 2012, 42, 1119–1126. [Google Scholar] [CrossRef]
- Huang, S.; Xie, T.; Yan, J. Principle and application of loop-mediated isothermal amplification. Chin. J. Biol. 2011, 24, 1511–1513. [Google Scholar]
- Wang, X.R.; Wu, l.F.; Wang, Y.; Ma, Y.Y.; Chen, F.H.; Qu, H.L. Rapid detection of Staphlococcus aureus by loop-mediated isothermal amplification. Appl. Biochem. Biotechnol. 2015, 175, 882–891. [Google Scholar] [CrossRef]
- Tirloni, E.; Bernardi, C.; Drago, S.; Stampone, G.; Pomillio, F.; Cattaneo, P.; Stella, S. Evaluation of a loop-mediated isothermal amplification method for the detection of Listeria monocytogenes in dairy food. Ital. J. Food Saf. 2017, 6, 6890. [Google Scholar] [CrossRef]
- Yaqing, H.; Wenping, Z.; Zhiyi, Y.; Xionghu, W.; Shouyi, Y.; Hong, Y.; Yingchun, D.; Guifang, H. Detection of human Enterovirus 71 reverse transcription loop-mediated isothermal amplification (RT-LAMP). Lett. Appl. Microbiol. 2012, 54, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Becherer, L.; Borst, N.; Bakheit, M.; Frischmann, S.; Zengerle, R.; von Stetten, F. Loop-mediated isothermal amplification (LAMP)—Review and classification of methods for sequence-specific detection. Anal. Methods 2020, 12, 717–746. [Google Scholar] [CrossRef]
- Yamazaki, W.; Kumeda, Y.; Misawa, N.; Nakaguchi, Y.; Nishibuchi, M. Development of a loop-mediated isothermal amplification assay for sensitive and rapid detection of the tdh and trh genes of Vibrio parahaemolyticus and related Vibrio species. Appl. Environ. Microbiol. 2010, 76, 820–828. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, S.; Sasaki, Y.; Seno, M. Rapid and sensitive detection of norovirus genomes in oysters by a two-step isothermal amplification assay system combining nucleic acid sequence-based amplification and reverse transcription-loop-mediated isothermal amplification assays. Appl. Environ. Microbiol. 2008, 74, 3912–3914. [Google Scholar] [CrossRef][Green Version]
- Yang, Q.; Domesie, K.J.; Ge, B. Loop-mediated isothermal amplification for Salmonella detection in food and feed: Current applications and future directions. Foodborne Pathog. Dis. 2018, 15, 309–331. [Google Scholar] [CrossRef] [PubMed]
- Kubota, R.; Jenkins, D.M. Real-time duplex applications of loop-mediated amplification (LAMP) by assimilating probes. Int. J. Mol. Sci. 2015, 16, 4786–4799. [Google Scholar] [CrossRef] [PubMed]
- Almasi, M.A.; Almasi, G. Loop-mediated isothermal amplification (LAMP) for embryo sex determination in pregnant women at eight weeks of pregnancy. J. Reprod. Infertil. 2017, 18, 197–204. [Google Scholar] [PubMed]
- Jia, Y.; Fu, B.; Wang, Y.; Ma, X.; Zhang, X.; Yuan, N.; Zhang, W. Detection of Bacillus cereus in milk by real-time fluorescence loop-mediated isothermal amplification method. Food Sci. 2016, 37, 184–189. [Google Scholar]
- Hutson, R.A.; Zhou, Y.; Collins, M.D.; Johnson, E.A.; Hatheway, C.L.; Sugiyama, H. Genetic characterization of Clostridium botulinum type A containing silent type B neurotoxin gene sequences. J. Biol. Chem. 1996, 271, 10786–10792. [Google Scholar] [CrossRef]
- Woudstra, C.; Maréchal, C.L.; Souillard, R.; Bayon-Auboyer, M.H.; Anniballi, F.; Auricchio, B.; De Medici, D.; Bano, L.; Koene, M.; Sansonetti, M.H.; et al. Molecular gene profiling of Clostridium botulinum Group III and its detection in naturally contaminated samples originatig from various European countries. Appl. Environ. Microbiol. 2015, 81, 1495–2505. [Google Scholar] [CrossRef] [PubMed]
- Grenda, T.; Kukier, E.; Goldsztejn, M.; Kwiatek, K.; Kozieł, N. Optimisation of protocol for Clostridium botulinum detection in mink feed. Bull. Vet. Inst. Pulawy 2015, 59, 377–382. [Google Scholar] [CrossRef]
- East, A.K.; Collins, M.D. Conserved structure of genes encoding components of botulinum neurotoxin complex M and the sequence of the gene coding for the nontoxic component in nonproteolytic Clostridium botulinum type F. Curr. Microbiol. 1994, 29, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Hill, K.K.; Smith, T.J.; Helma, C.H.; Ticknor, L.O.; Foley, B.T.; Svensson, R.T.; Brown, J.L.; Johnson, E.A.; Smith, L.A.; Okinaka, R.T.; et al. Genetic diversity among botulinum neurotoxin-producing clostridial strains. J. Bacteriol. 2007, 189, 818–832. [Google Scholar] [CrossRef]
- Cui, Q.; Liu, W.; Yang, Z.; Lu, S.; Yuan, J.; Li, Y. Quick detection of L2 type cephalosporinase beta lactamase gene in Stenotrophomonas maltophilia by loop-mediated isothermal amplification. Mil. Med. Sci. 2013, 37, 943–946. [Google Scholar]
- Tian, X.; Feng, J.; Wang, Y. Direct loop-mediated isothermal amplification assay for on-site dtection of Staphylococcus aureus. FEMS Microbiol. Lett. 2018, 365, fny092. [Google Scholar] [CrossRef] [PubMed]
- Nagamine, K.; Hase, T.; Notomi, T. Accelerated reaction by loop-mediated isothermal amplification using loop primers. Mol. Cell. Probes 2002, 16, 223. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Lv, B.; Jiang, W.; Bai, L.; Wu, G.; Wang, J.; Wang, R.; Pan, A.; Tang, X. Rapid detection technique of duck-derived components in beef and sheep products by LAMP. J. Food Sci. Biotechnol. 2019, 38, 126–133. [Google Scholar]
- Fan, R.H.; Huang, M.; Zhong, H.; Ye, X.; Luo, Y. Establishment of RT-LAMP assay for detection of Freesia mosaic virus. Exp. Method Technol. 2019, 45, 153–156. [Google Scholar]
- Kaneko, H.; Kawana, T.; Fukushima, E.; Suzutani, T. Tolerance of loop-mediated isothermal amplification to a culture medium and biological substances. J. Biochem. Bioph. Meth. 2007, 70, 499–501. [Google Scholar] [CrossRef]
- Mori, Y.; Nagamine, K.; Tomita, N.; Notomi, T. Detection of loop-mediated isothermal amplification reaction by turbidity derived from magnesium pyrophosphate formation. Biochem. Biophys. Res. Commun. 2001, 289, 150–154. [Google Scholar] [CrossRef]
- Sharma, S.K.; Eblen, B.S.; Bull, R.L.; Burr, D.H.; Whiting, R.C. Evaluation of lateral-flow Clostridium botulinum neurotoxin detection kits for food analysis. Appl. Environ. Microbiol. 2005, 71, 3935–3941. [Google Scholar] [CrossRef]


| Primer Sets | Primer Names and Types | DNA Sequences (5′ to 3′) |
|---|---|---|
| RD1 | F3 (outer forward primer) | AAGTATAAATTCCCCGGTAGA |
| B3 (outer backward primer) | GCTTGTAAGAACTTATCTTTTTCAC | |
| FIP (forward inner primer) | TGGGAGCAACCTTAAAAGCCTTAAAAAATGTTGTAGTAGTTAGAGCT | |
| BIP (backward inner primer) | GGTGGCGCCAGAGAGATATTAGAATCATATATTCCCCCATCAA | |
| LF (loop forward primer) | AAACCGTATCAGTTTTTCT | |
| LB (loop backward primer) | ATGGCGAATCTTTGAGTATA | |
| RD2 | F3 (outer forward primer) | GTTCTTACAAGCCATTATTACTTTG |
| B3 (outer backward primer) | AAGGAAATGGAATAGTACTTGAA | |
| FIP (forward inner primer) | ATCCATAAGGAAATGGAATAGCTGTAAAGAATTAATAGTACTAACGCTGG | |
| BIP (backward inner primer) | TATAGGTGGAGGGTATTATGCACCTTTATTAGATTTTGGTGCTGATCC | |
| RD3 | F3 (outer forward primer) | ATGATTCTAATTTTCTTTCACAAGA |
| B3 (outer backward primer) | GATTTTGGTGCTGATCCAA | |
| FIP (forward inner primer) | TCCCCAGCGTTAGTACTATTAATTCTGTGAAAAAGATAAGTTCTTACAAGC | |
| BIP (backward inner primer) | TGATTTCTACAGCTATTCCATTTCCTTCATATTAGGTGCATAATACCCTC |
| Number of Bacteria | Species of Bacteria |
|---|---|
| 1 | Shigella flexneri ATCC12022 * |
| 2 | Escherichia coli ATCC25922 * |
| 3 | Yersinia enterocolitica ATCC23715 * |
| 4 | Enterococcus faecalis ATCC29212 * |
| 5 | Pseudomonas aeruginosa 10211 * |
| 6 | Staphylococcus aureus 1897/2722 * |
| 7 | Streptococcus dysgalactiae ATCC12388 * |
| 8 | Bacillus cereus ATCC11778 * |
| 9 | Streptococcus pneumoniae 31002 * |
| 10 | Enterococcus faecium ATCC29212 * |
| 11 | Vibrio Parahemolyticus ATCC17802 * |
| 12 | Staphylococcus epidermidis 1.2429 * |
| 13 | Salmonella enterica ATCC14028 * |
| 14 | Streptococcus uberis ATCC700407 * |
| 15 | Clostridium tetani ATCC19406 |
| 16 | Clostridium perfringens NCTC8798 |
| 17 | Clostridium difficile ATCC9689 |
| 18 | Clostridium beijerinckii NCIMB8052 |
| 19 | Clostridium acetobutylicum ATCC824 |
| 20 | Clostridium sporogenes ATCC19404 |
| 21 | Clostridium sordellii ATCC9714 |
| 22 | Clostridium butyricum ATCC25755 |
| 23 | Clostridium tertium CICC10820 |
| 24 | Bntorobater sakazakii ATCC29544 |
| 25 | Clostridium bifermentans CICC22952 |
| 26 | Clostridium thermosaccharolyticum ATCC7956 |
| 27 | Bacillus stearothermophilus ATCC7953 |
| 28 | Bacillus thuringiensis LSZ9408 |
| 29 | Bacillus subtilis ATCC6633 |
| 30 | Bacillus megaterium DSM90 |
| Sample | Genomic DNA Concentration (ng/μL) |
|---|---|
| Korean kimchi 1–16 | 1.8–45.2 |
| Preserved meat (pork) 1–8 | 143.5–154.6 |
| Bacon 1–8 | 89.5–124.2 |
| Sour meat (pork) 1–8 | 123.5–180.1 |
| Salami (pork) 1–8 | 125.2–165.6 |
| Ham (pork) 1–8 | 68.5–95.6 |
| Fish product (canned sardine) 1–8 | 105.5–127.3 |
| Soybean paste 1–8 | 176.2–275.2 |
| Dairy product (powdered cow milk) 1–8 | 125.8–151.1 |
| Pork rib 1–8 | 106.2–143.5 |
| Fish product (canned anchovy) 1–8 | 51.8–70.1 |
| Fish product (canned tuna) 1–8 | 19.6–26.9 |
| Fish product (canned salmon) 1–8 | 82.5–95.4 |
| Fish product (canned yellow croaker) 1–8 | 29.8–40.1 |
| Stinky tofu 1–8 | 215.1–235.7 |
| Dried tofu 1–8 | 135.9–158.7 |
| Vegetarian meat 1–8 | 60.8–73.5 |
| Vegetarian cow stomach 1–8 | 40.2–51.1 |
| Vegetarian ham 1–8 | 74.6–92.7 |
| Quail egg (canned) 1–8 | 28.9–41.7 |
| Chicken foot (canned) 1–8 | 50.2–67.1 |
| Honey 1–8 | 95.2–105.2 |
| Condition | LAMP | PCR |
|---|---|---|
| Temperature of reaction | Isothermal | Cycling |
| Time of completion | Short (~90 min) | Long (~24 h) |
| Detection method | Direct examination of turbidity in a positive reaction with visual fluorescence | Requirement of high precision of detection on the agarose gel electrophoresis |
| Specificity and sensitivity | Increased by specifically designed primers to recognize four or six independent regions in the target DNA sequence | PCR primers recognize only two independent regions of the target sequence |
| Purification of DNA sample | Not required due to its less susceptibility | Required |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.; Li, H.; Yang, L.; Wang, L.; Sun, R.; Shearer, J.E.S.; Sun, F. Rapid Detection of Clostridium botulinum in Food Using Loop-Mediated Isothermal Amplification (LAMP). Int. J. Environ. Res. Public Health 2021, 18, 4401. https://doi.org/10.3390/ijerph18094401
Chen Y, Li H, Yang L, Wang L, Sun R, Shearer JES, Sun F. Rapid Detection of Clostridium botulinum in Food Using Loop-Mediated Isothermal Amplification (LAMP). International Journal of Environmental Research and Public Health. 2021; 18(9):4401. https://doi.org/10.3390/ijerph18094401
Chicago/Turabian StyleChen, Yufei, Hao Li, Liu Yang, Lei Wang, Ruyi Sun, Julia E. S. Shearer, and Fengjie Sun. 2021. "Rapid Detection of Clostridium botulinum in Food Using Loop-Mediated Isothermal Amplification (LAMP)" International Journal of Environmental Research and Public Health 18, no. 9: 4401. https://doi.org/10.3390/ijerph18094401
APA StyleChen, Y., Li, H., Yang, L., Wang, L., Sun, R., Shearer, J. E. S., & Sun, F. (2021). Rapid Detection of Clostridium botulinum in Food Using Loop-Mediated Isothermal Amplification (LAMP). International Journal of Environmental Research and Public Health, 18(9), 4401. https://doi.org/10.3390/ijerph18094401






