Development, Pilot Study, and Psychometric Analysis of the AHRQ Surveys on Patient Safety Culture™ (SOPS®) Workplace Safety Supplemental Items for Hospitals
Abstract
:1. Introduction
2. Materials and Methods
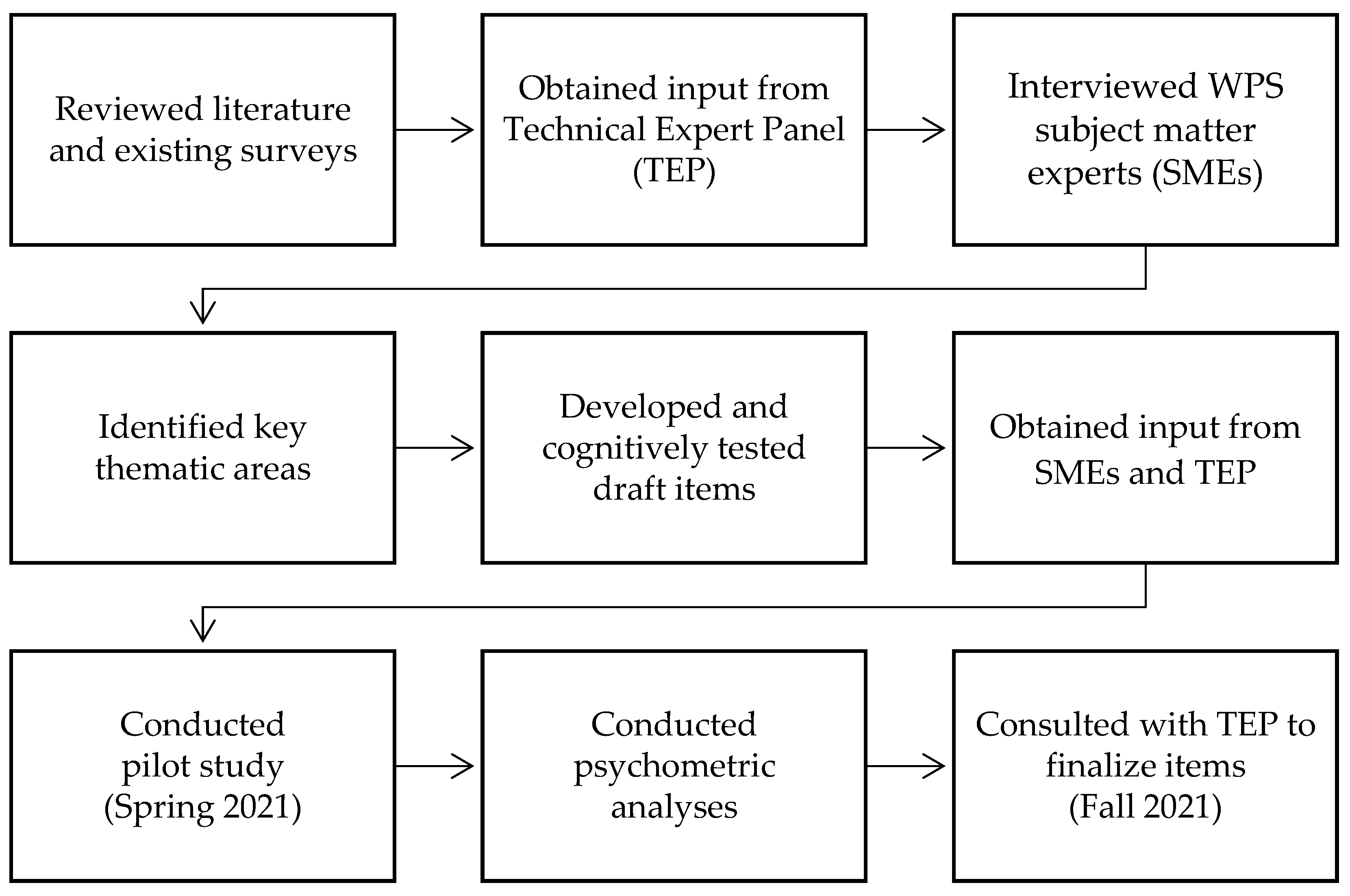
2.1. Supplemental Item Development
2.2. Measures
2.3. Pilot Study
2.4. Analyses
2.4.1. Item Analysis
2.4.2. Internal Consistency Reliability
2.4.3. Confirmatory Factor Analysis (CFA)
2.4.4. Site-Level Reliability Analysis
2.4.5. Hospital-Level Percent Positive Scores and Correlations
3. Results
3.1. Pilot Hospital Characteristics
3.2. Characteristics of the Respondents
3.3. Item Analysis
3.3.1. Internal Consistency Reliability Analysis
3.3.2. TEP Review and Input
3.3.3. Confirmatory Factor Analysis (CFA)
3.3.4. Site-Level Reliability
3.3.5. Hospital Level Percent Positive Scores and Correlations
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Steering Committee for Patient Safety. National Action Plan to Advance Patient Safety; Institute for Healthcare Improvement: Boston, MA, USA, 2020; Available online: www.ihi.org/SafetyActionPlan (accessed on 21 February 2022).
- Gerwig, K.; Hodgson, M.; Kingston, M.B. A Healthcare Acquired Condition: Workforce Harm (8–11 December 2019); IHI Forum: Orlando, FL, USA, 2021. [Google Scholar]
- U.S. Bureau of Labor Statistics. Injuries, Illnesses, and Fatalities, Table R8 Page. Survey of Occupational and Illness Data. Detailed Industry by Selected Events or Exposures (Rate). Available online: https://www.bls.gov/iif/oshwc/osh/case/cd_r8_2020.htm (accessed on 21 February 2022).
- Centers for Disease Control and Prevention. The National Institute for Occupational Safety and Health (NIOSH). Safe Patient Handling and Mobility (SPHM) Page. Available online: https://www.cdc.gov/niosh/topics/safepatient/default.html (accessed on 3 March 2022).
- Kayser, S.A.; Wiggermann, N.E.; Kumpar, D. Factors associated with safe patient handling practice in acute care and its relationship with patient mobilization: A cross-sectional study. Int. J. Nurs. Stud. 2020, 104, 103508. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Workbook for Designing, Implementing, and Evaluating a Sharps Injury Prevention Program. Available online: https://www.cdc.gov/sharpssafety/pdf/sharpsworkbook_2008.pdf (accessed on 21 February 2022).
- Bahat, H.; Hasidov-Gafni, A.; Youngster, I.; Goldman, M.; Levtzion-Korach, O. The prevalence and underreporting of needlestick injuries among hospital workers: A cross-sectional study. Int. J. Qual. Health Care 2021, 33, mzab009. [Google Scholar] [CrossRef] [PubMed]
- Boden, L.I.; Petrofsky, Y.V.; Hopcia, K.; Wagner, G.R.; Hashimoto, D. Understanding the hospital sharps injury reporting pathway. Am. J. Ind. Med. 2015, 58, 282–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeoh, H.T.; Lockhart, T.E.; Wu, X. Nonfatal Occupational Falls Among US Health Care Workers, 2008–2010. Workplace Health Saf. 2013, 61, 3–8. [Google Scholar] [CrossRef]
- Phillips, J.P. Workplace violence against health care workers in the United States. N. Engl. J. Med. 2016, 374, 1661–1669. [Google Scholar] [CrossRef]
- The Joint Commission. Physical and verbal violence against health care workers. Sentin. Event Alert 2018, 59, 1–7. Available online: https://www.jointcommission.org/-/media/tjc/documents/resources/patient-safety-topics/sentinel-event/sea-59-workplace-violence-final2.pdf (accessed on 1 June 2022).
- Lanctôt, N.; Guay, S. The aftermath of workplace violence among healthcare workers: A systematic literature review of the consequences. Aggress. Violent Behav. 2014, 19, 492–501. [Google Scholar] [CrossRef]
- Arnetz, J.E.; Hamblin, L.; Ager, J.; Luborsky, M.; Upfal, M.J.; Russell, J.; Essenmacher, L. Underreporting of workplace violence: Comparison of self-report and actual documentation of hospital incidents. Workplace Health Saf. 2015, 63, 200–210. [Google Scholar] [CrossRef] [Green Version]
- Galizzi, M.; Miesmaa, P.; Punnett, L.; Slatin, C. Phase in Healthcare Research Team. Injured workers’ underreporting in the health care industry: An analysis using quantitative, qualitative, and observational data. Ind. Relat. A J. Econ. Soc. 2010, 49, 22–43. [Google Scholar]
- Stephens, W. Violence against Healthcare Workers: A Rising Epidemic. Am. J. Manag. Care 2019. Available online: https://www.ajmc.com/view/violence-against-healthcare-workers-a-rising-epidemic (accessed on 1 June 2022).
- de Castro, A.B. Barriers to Reporting a Workplace Injury: Recognizing the difficulties and encouraging a determined approach. AJN Am. J. Nurs. 2003, 103, 112. [Google Scholar] [CrossRef] [PubMed]
- Rangachari, P.L.; Woods, J. Preserving organizational resilience, patient safety, and staff retention during COVID-19 requires a holistic consideration of the psychological safety of healthcare workers. Int. J. Environ. Res. Public Health 2020, 17, 4267. [Google Scholar] [CrossRef] [PubMed]
- De Kock, J.H.; Latham, H.A.; Leslie, S.J.; Grindle, M.; Munoz, S.A.; Ellis, L.; Polson, R.; O’Malley, C.M. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 2021, 21, 104. [Google Scholar] [CrossRef] [PubMed]
- Salazar de Pablo, G.; Vaquerizo-Serrano, J.; Catalan, A.; Arango, C.; Moreno, C.; Ferre, F.; Shin, J.; Sullivan, S.; Brondino, N.; Solmi, M.; et al. Impact of coronavirus syndromes on physician and mental health of healthcare workers: Systematic review and meta-analysis. J. Affect. Disord. 2020, 275, 48–57. [Google Scholar] [CrossRef]
- Stericycle. Key Insights to Safeguard the Environment and the Environment of Care. Healthcare Workplace Safety Trend Report. Available online: https://www.stericycle.com/en-us/resource-center/original-research/healthcare-workplace-safety-report (accessed on 21 February 2022).
- Capone, V.; Borrelli, R.; Marino, L.; Schettino, G. Mental well-being and job satisfaction of hospital physicians during COVID-19: Relationships with efficacy beliefs, organizational support, and organizational non-technical skills. Int. J. Environ. Res. Public Health 2022, 19, 3734. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. Hospital Survey on Patient Safety Culture Page. Surveys on Patient Safety Culture™ (SOPS®). Available online: https://www.ahrq.gov/sops/surveys/hospital/index.html (accessed on 21 February 2022).
- Sorra, J.; Yount, N.; Famolaro, T. AHRQ Hospital Survey on Patient Safety Culture Version 2.0: User’s Guide. (Prepared by Westat, under Contract No. HHSP233201500026I/ HHSP23337004T). Rockville, MD Agency for Healthcare Research and Quality (AHRQ Publication No. 19-0076). 2019. Available online: https://www.ahrq.gov/sites/default/files/wysiwyg/sops/surveys/hospital/hospitalsurvey2-users-guide.pdf (accessed on 1 June 2022).
- Wagner, A.; Hammer, A.; Manser, T.; Martus, P.; Sturm, H.; Rieger, M.A. Do occupational and patient safety culture in hospitals share predictors in the field of psychosocial working conditions? Findings from a cross-sectional study in German university hospitals. Int. J. Environ. Res. Public Health 2018, 15, 2131. [Google Scholar] [CrossRef] [Green Version]
- Pousette, A.; Larsman, P.; Eklöf, M.; Törner, M. The relationship between patient safety climate and occupational safety climate in healthcare–A multi-level investigation. J. Saf. Res. 2017, 61, 187–198. [Google Scholar] [CrossRef]
- Linzer, M.; Poplau, S.; Babbott, S.; Collins, T.; Guzman-Corrales, L.; Menk, J.; Murphy, M.L.; Ovington, K. Worklife and wellness in academic general internal medicine: Results from a national survey. J. Gen. Intern. Med. 2016, 31, 1004–1010. [Google Scholar] [CrossRef] [Green Version]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- De Vellis, R.F. Scale Development: Theory and Applications; Sage: Thousand Oaks, CA, USA, 2003; Volume 26. [Google Scholar]
- Dong, Y.; Peng, C.Y.J. Principled missing data methods for researchers. SpringerPlus 2013, 2, 222. [Google Scholar] [CrossRef] [Green Version]
- Graham, J.W. Missing data analysis: Making it work in the real world. Annu. Rev. Psychol. 2009, 60, 549–576. [Google Scholar] [CrossRef] [Green Version]
- Stevens, J.P. Applied Multivariate Statistics for the Social Sciences, 4th ed.; Lawrence Erlbaum: Mahwah, NJ, USA, 2002. [Google Scholar]
- Schumacker, R.; Lomax, R. A Beginner’s Guide to Structural Equation Modeling, 2nd ed.; Lawrence Erlbaum: Mahwah, NJ, USA, 2004. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 2nd ed.; The Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Kenny, D.A. Measuring Model Fit. Available online: http://davidakenny.net/cm/fit.htm (accessed on 21 February 2022).
- Raudenbush, S.W.; Bryk, A.S. Hierarchical Linear Models, 2nd ed.; Sage: Thousand Oaks, CA, USA, 2002. [Google Scholar]
- Shah, M.K.; Gandrakota, N.; Cimiotti, J.P.; Ghose, N.; Moore, M.; Ali, M.K. Prevalence of and factors associated with nurse burnout in the US. JAMA Netw. Open 2021, 4, e2036469. [Google Scholar] [CrossRef] [PubMed]
- Agency for Healthcare Research and Quality. Workplace Safety Supplemental Items for Hospital SOPS Page. Surveys on Patient Safety Culture™ (SOPS®). Available online: https://www.ahrq.gov/sops/surveys/hospital/supplemental-items/workplace-safety.html (accessed on 21 February 2022).
| Composite Measures | Description of Survey Item Content | Number of Survey Items |
|---|---|---|
| Protection from Workplace Hazards * | Procedures are in place to protect providers and staff from workplace hazards; providers and staff are provided with personal protective equipment (PPE), they are trained to use it and use it appropriately. | 4 |
| Moving, Transferring, or Lifting Patients | Equipment or assistive devices are available, staff use them when needed, and staff are available when needed to move, transfer, or lift patients. | 3 |
| Addressing Workplace Aggression from Patients or Visitors * | Physical and verbal aggression from patients or visitors is problematic; and effective policies, procedures, and training are in place to manage workplace aggression. | 5 |
| Addressing Workplace Aggression from Providers or Staff * | Physical and verbal aggression among providers and staff is problematic; and effective policies and procedures are in place to manage workplace aggression. | 3 |
| Supervisor, Manager, or Clinical Leader Support for Workplace Safety | Supervisors, managers, or clinical leaders monitor the workplace, seriously consider suggestions for improving safety, encourage providers and staff to report their concerns, and can be trusted to keep providers and staff safe. | 4 |
| Hospital Management Support for Workplace Safety | Hospital management shows that workplace safety is a top priority, provides adequate resources for workplace safety, and takes action to address concerns. | 3 |
| Workplace Safety and Reporting | Whether or not providers and staff notice or experience workplace safety hazards, injuries, or verbal or physical aggression and whether they report them; providers and staff can report concerns about workplace safety without fear of negative consequences. | 9 |
| CFA Model Fit Criteria | |||
|---|---|---|---|
| CFI | RMSEA | SRMR | |
| <5.00 | ≥0.95 | <0.06 | <0.08 |
| Pilot Study Hospitals | ||
|---|---|---|
| Number | Percent | |
| Bed Size | ||
| 6–24 beds | 4 | 14% |
| 25–49 beds | 5 | 18% |
| 50–99 beds | 9 | 32% |
| 100–199 beds | 6 | 21% |
| 200 beds or more | 4 | 14% |
| Teaching Status | ||
| Teaching | 18 | 64% |
| Nonteaching | 10 | 36% |
| Hospital Ownership | ||
| Government (federal and non-federal) | 11 | 39% |
| Non-government not for profit | 11 | 39% |
| Investor owned (for profit) | 6 | 21% |
| U.S. Census Region | ||
| Northeast | 7 | 25% |
| South | 4 | 14% |
| Midwest | 10 | 36% |
| West | 7 | 25% |
| Respondents | ||
|---|---|---|
| Number | Percent | |
| Hospital Staff Position | ||
| Nursing Staff (RN, LVN, LPN, Nurse Practitioner) | 2361 | 35% |
| Support Staff (Receptionist, Clerical Staff, Housekeeping Staff) | 1301 | 20% |
| Other Clinical Staff (Pharmacist, Therapist, Technologist) | 1196 | 18% |
| Other Position | 847 | 13% |
| Supervisor, Manager, Clinical/Senior Leader | 778 | 12% |
| Physician, Physician Assistant, Resident | 162 | 2% |
| Total | 6645 | 100% |
| Missing | 39 | - |
| Overall total | 6684 | - |
| Unit/Work Area | ||
| Patient Care | 1875 | 28% |
| Administration/Management | 967 | 15% |
| Other Unit/Work Area | 854 | 13% |
| Clinical Services | 836 | 13% |
| Multiple Units/No Specific Unit | 645 | 10% |
| Medical/Surgical | 636 | 10% |
| Support Services | 523 | 8% |
| Surgical Services | 298 | 4% |
| Total | 6634 | 100% |
| Missing | 50 | - |
| Overall total | 6684 | - |
| Composite Measures and Items | % Positive | % MI | % DNA/DK |
|---|---|---|---|
| Protection from Workplace Hazards (four items) | |||
| This unit has effective procedures to protect providers and staff from exposure to hazardous materials, contagious diseases, blood, or other bodily fluids | 92% | <1% | 12% |
| In this unit, providers and staff are provided with the appropriate personal protective equipment (PPE) | 91% | <1% | 10% |
| In this unit, providers and staff are trained to properly put on, use, and remove PPE | 92% | 1% | 11% |
| In this unit, providers and staff use PPE appropriately | 89% | 1% | 11% |
| Moving, Transferring, or Lifting Patients (three items) | |||
| Equipment or assistive devices are available when needed to help move, transfer, or lift patients in this unit | 75% | 1% | 42% |
| In this unit, staff use equipment or assistive devices when needed to help move, transfer, or lift patients, even if it takes more time | 74% | 1% | 43% |
| In this unit, enough staff are available when needed to help move, transfer, or lift patients | 64% | 1% | 39% |
| Addressing Workplace Aggression from Patients or Visitors (five items) | |||
| In this unit, there is a problem with patients or visitors being physically aggressive toward providers or staff (negatively worded) * | 59% | 3% | 25% |
| In this unit, there is a problem with patients or visitors being verbally aggressive toward providers or staff (negatively worded) * | 45% | 3% | 24% |
| In this unit, there are effective policies and procedures to keep providers and staff safe from aggressive patients or visitors | 71% | 3% | 22% |
| In this unit, providers and staff are trained to recognize early signs of aggressive behavior from patients or visitors | 72% | 3% | 20% |
| In this unit, providers and staff are trained on how to deescalate or calm down aggressive behavior from patients or visitors | 67% | 3% | 20% |
| Addressing Workplace Aggression from Providers or Staff (three items) | |||
| In this unit, there is a problem with providers or staff being physically aggressive toward other providers or staff (negatively worded) * | 91% | 3% | 14% |
| In this unit, there is a problem with providers or staff being verbally aggressive toward other providers or staff (negatively worded) * | 74% | 4% | 13% |
| In this unit, there are effective policies and procedures to address providers and staff who behave aggressively toward other providers or staff | 65% | 4% | 19% |
| Supervisor, Manager, or Clinical Leader Support for Workplace Safety (four items) | |||
| My supervisor, manager, or clinical leader regularly monitors the workplace to identify unsafe working conditions for providers and staff | 77% | 2% | 8% |
| My supervisor, manager, or clinical leader seriously considers provider or staff suggestions for improving workplace safety | 78% | 2% | 6% |
| My supervisor, manager, or clinical leader encourages providers and staff to report their concerns about workplace safety | 83% | 2% | 5% |
| My supervisor, manager, or clinical leader can be trusted to do the right thing to keep providers and staff safe | 82% | 2% | 5% |
| Hospital Management Support for Workplace Safety (three items) | |||
| The actions of hospital management show that the safety of providers and staff is a top priority | 70% | 2% | 5% |
| Hospital management provides adequate resources to ensure the safety of providers and staff | 70% | 3% | 5% |
| Hospital management takes action to address provider and staff concerns about workplace safety | 69% | 3% | 6% |
| Workplace Safety and Reporting (one item) | |||
| I can report my concerns about workplace safety without fear of negative consequences for me | 76% | 2% | 2% |
| Overall Rating on Workplace Safety for Providers and Staff (one item) | |||
| How would you rate your unit/work area on workplace safety for providers and staff? | 50% | 3% | N/A |
| Work Stress/Burnout (one item) | % | % No Burnout and Burnout |
|---|---|---|
| Using your own definition of “burnout”, please select one of the answers below: | ||
| I have no symptoms of burnout. | 32% | 69% (No symptoms of burnout) |
| I am under stress, and don’t always have as much energy as I did, but I don’t feel burned out. | 37% | |
| I am definitely burning out and have one or more symptoms of burnout, e.g., emotional exhaustion. | 21% | 32% (Symptoms of burnout) |
| The symptoms of burnout that I am experiencing won’t go away. I think about work frustrations a lot. | 8% | |
| I feel completely burned out. I am at the point where I may need to seek help. | 3% |
| Measures and Items | CFA Standardized Factor Loading | Cronbach’s Alpha (Alpha If Item Deleted) | Site- Level Reliability |
|---|---|---|---|
| Composite Measures and Items | |||
| Protection from Workplace Hazards (three items) | - | 0.87 | 0.80 |
| This unit has effective procedures to protect providers and staff from exposure to hazardous materials, contagious diseases, blood, or other bodily fluids | 0.83 | (0.81) | 0.77 |
| In this unit, providers and staff are provided with the appropriate personal protective equipment (PPE) | 0.86 | (0.78) | 0.80 |
| In this unit, providers and staff use PPE appropriately | 0.78 | (0.84) | 0.74 |
| Moving, Transferring, or Lifting Patients (three items) | - | 0.83 | 0.76 |
| Equipment or assistive devices are available when needed to help move, transfer, or lift patients in this unit | 0.90 | (0.70) | 0.78 |
| In this unit, staff use equipment or assistive devices when needed to help move, transfer, or lift patients, even if it takes more time | 0.86 | (0.71) | 0.76 |
| In this unit, enough staff are available when needed to help move, transfer, or lift patients | 0.64 | (0.88) | 0.73 |
| Addressing Workplace Aggression from Patients or Visitors (two items) | - | 0.89 | 0.86 |
| In this unit, there is a problem with patients or visitors being physically aggressive toward providers or staff (negatively worded) | 0.85 | (N/A) | 0.87 |
| In this unit, there is a problem with patients or visitors being verbally aggressive toward providers or staff (negatively worded) | 0.94 | (N/A) | 0.83 |
| Workplace Aggression Policies, Procedures, and Training (two items) | - | 0.67 | 0.80 |
| In this unit, there are effective policies and procedures to keep providers and staff safe from aggressive patients or visitors | 0.84 | (N/A) | 0.69 |
| In this unit, providers and staff are trained on how to deescalate or calm down aggressive behavior from patients or visitors | 0.59 | (N/A) | 0.86 |
| Supervisor, Manager, or Clinical Leader Support for Workplace Safety (three items) | - | 0.92 | 0.77 |
| My supervisor, manager, or clinical leader regularly monitors the workplace to identify unsafe working conditions for providers and staff | 0.85 | (0.91) | 0.72 |
| My supervisor, manager, or clinical leader encourages providers and staff to report their concerns about workplace safety | 0.89 | (0.88) | 0.75 |
| My supervisor, manager, or clinical leader can be trusted to do the right thing to keep providers and staff safe | 0.92 | (0.87) | 0.78 |
| Hospital Management Support for Workplace Safety (three items) | - | 0.96 | 0.85 |
| The actions of hospital management show that the safety of providers and staff is a top priority | 0.94 | (0.95) | 0.84 |
| Hospital management provides adequate resources to ensure the safety of providers and staff | 0.95 | (0.95) | 0.85 |
| Hospital management takes action to address provider and staff concerns about workplace safety | 0.95 | (0.95) | 0.84 |
| Single-Item Measures | |||
| Addressing Verbal Aggression from Providers or Staff | |||
| In this unit, there is a problem with providers or staff being verbally aggressive toward other providers or staff | - | - | 0.80 |
| Workplace Safety and Reporting | |||
| I can report my concerns about workplace safety without fear of negative consequences for me | - | - | 0.76 |
| Work Stress/Burnout | |||
| Using your own definition of “burnout”, please select one of the answers below | - | - | 0.62 |
| Overall Rating | |||
| How would you rate your unit/work area on workplace safety for providers and staff? | - | - | 0.86 |
| CFA Model Fit Indices | |||||
|---|---|---|---|---|---|
| CFI | RMSEA (CI) | SRMR | |||
| 1202.24 * | 89 | 13.5 | 0.98 | 0.04 (0.04–0.05) | 0.05 |
| Workplace Safety Measures | Mean Score | SD | Correlations | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | |||
| Composite Measures | % Positive | ||||||||||
| (1) Protection from Workplace Hazards | 90% | 4% | - | ||||||||
| (2) Moving, Transferring, or Lifting Patients | 73% | 10% | 0.57 | - | |||||||
| (3) Addressing Workplace Aggression from Patients or Visitors | 58% | 13% | 0.39 | 0.58 | - | ||||||
| (4) Workplace Aggression Policies, Procedures, and Training | 69% | 11% | −0.14 | 0.20 | 0.02 | - | |||||
| (5) Supervisor, Manager, or Clinical Leader Support for Workplace Safety | 82% | 7% | 0.55 | 0.60 | 0.53 | 0.15 | - | ||||
| (6) Hospital Management Support for Workplace Safety | 70% | 10% | 0.79 | 0.76 | 0.49 | 0.20 | 0.73 | - | |||
| Single-Item Measures | % Positive | ||||||||||
| (7) Addressing Verbal Aggression from Providers or Staff | 78% | 9% | 0.27 | 0.57 | 0.60 | 0.41 | 0.72 | 0.48 | - | ||
| (8) Workplace Safety and Reporting | 78% | 8% | 0.44 | 0.47 | 0.55 | 0.30 | 0.80 | 0.72 | 0.72 | - | |
| % Burned out | |||||||||||
| (9) Work Stress/Burnout | 30% | 8% | −0.61 | −0.32 | −0.15 | 0.20 | −0.64 | −0.60 | −0.32 | −0.44 | - |
| Overall Rating | % Positive | ||||||||||
| (10) Overall Rating on Workplace Safety for Providers and Staff | 53% | 11% | 0.75 | 0.79 | 0.52 | 0.13 | 0.77 | 0.90 | 0.53 | 0.68 | −0.64 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zebrak, K.; Yount, N.; Sorra, J.; Famolaro, T.; Gray, L.; Carpenter, D.; Caporaso, A. Development, Pilot Study, and Psychometric Analysis of the AHRQ Surveys on Patient Safety Culture™ (SOPS®) Workplace Safety Supplemental Items for Hospitals. Int. J. Environ. Res. Public Health 2022, 19, 6815. https://doi.org/10.3390/ijerph19116815
Zebrak K, Yount N, Sorra J, Famolaro T, Gray L, Carpenter D, Caporaso A. Development, Pilot Study, and Psychometric Analysis of the AHRQ Surveys on Patient Safety Culture™ (SOPS®) Workplace Safety Supplemental Items for Hospitals. International Journal of Environmental Research and Public Health. 2022; 19(11):6815. https://doi.org/10.3390/ijerph19116815
Chicago/Turabian StyleZebrak, Katarzyna, Naomi Yount, Joann Sorra, Theresa Famolaro, Laura Gray, Deborah Carpenter, and Andrew Caporaso. 2022. "Development, Pilot Study, and Psychometric Analysis of the AHRQ Surveys on Patient Safety Culture™ (SOPS®) Workplace Safety Supplemental Items for Hospitals" International Journal of Environmental Research and Public Health 19, no. 11: 6815. https://doi.org/10.3390/ijerph19116815
APA StyleZebrak, K., Yount, N., Sorra, J., Famolaro, T., Gray, L., Carpenter, D., & Caporaso, A. (2022). Development, Pilot Study, and Psychometric Analysis of the AHRQ Surveys on Patient Safety Culture™ (SOPS®) Workplace Safety Supplemental Items for Hospitals. International Journal of Environmental Research and Public Health, 19(11), 6815. https://doi.org/10.3390/ijerph19116815







