Cross-Cultural Adaptation and Psychometric Properties of the Malay Version of the Communication Skills Attitude Scale (CSAS) among Medical Students in Malaysia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Study Tool
2.3. Conduct of the Study
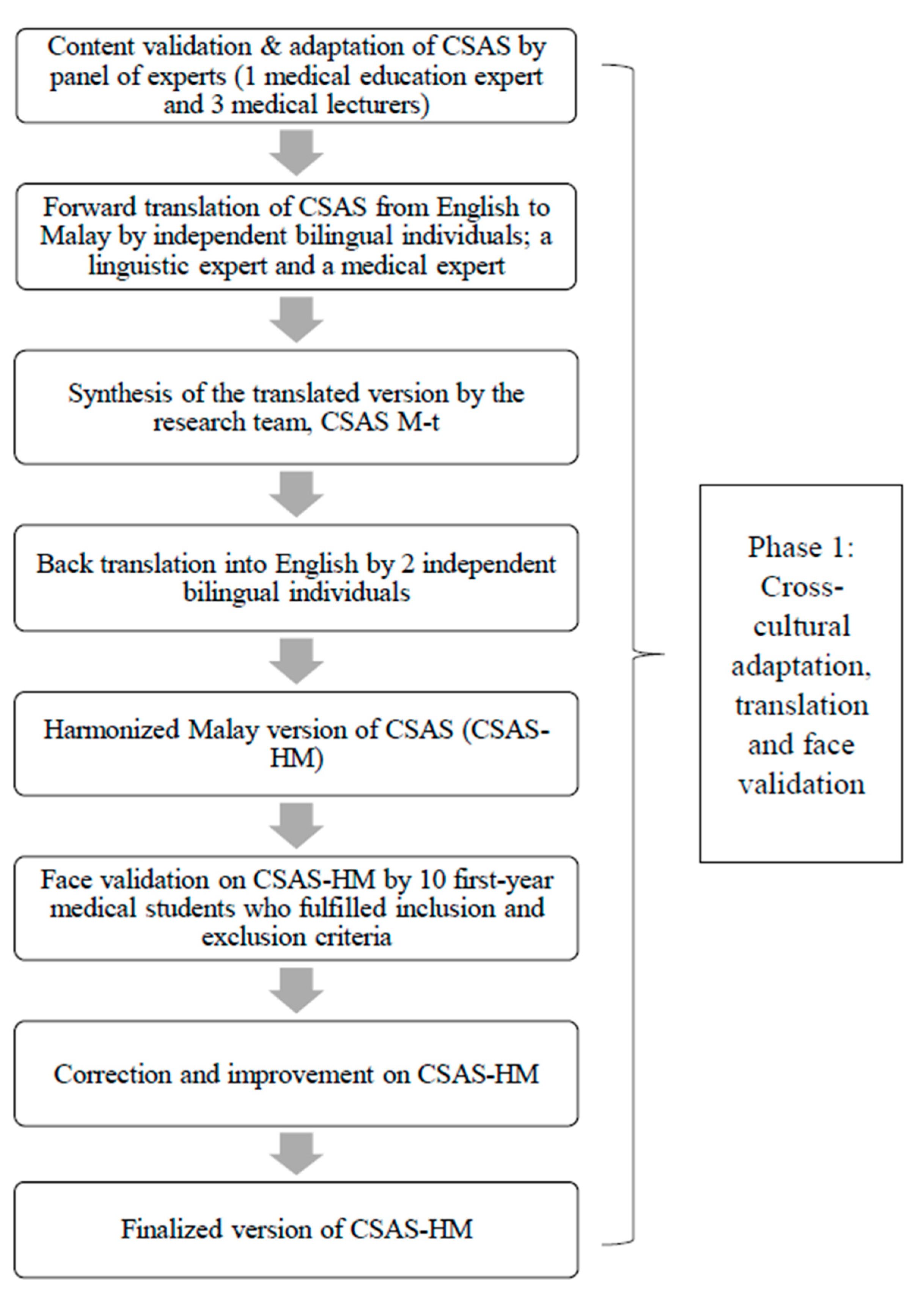
2.3.1. Phase 1: Cross-Cultural Adaptation, Translation, and Face Validation
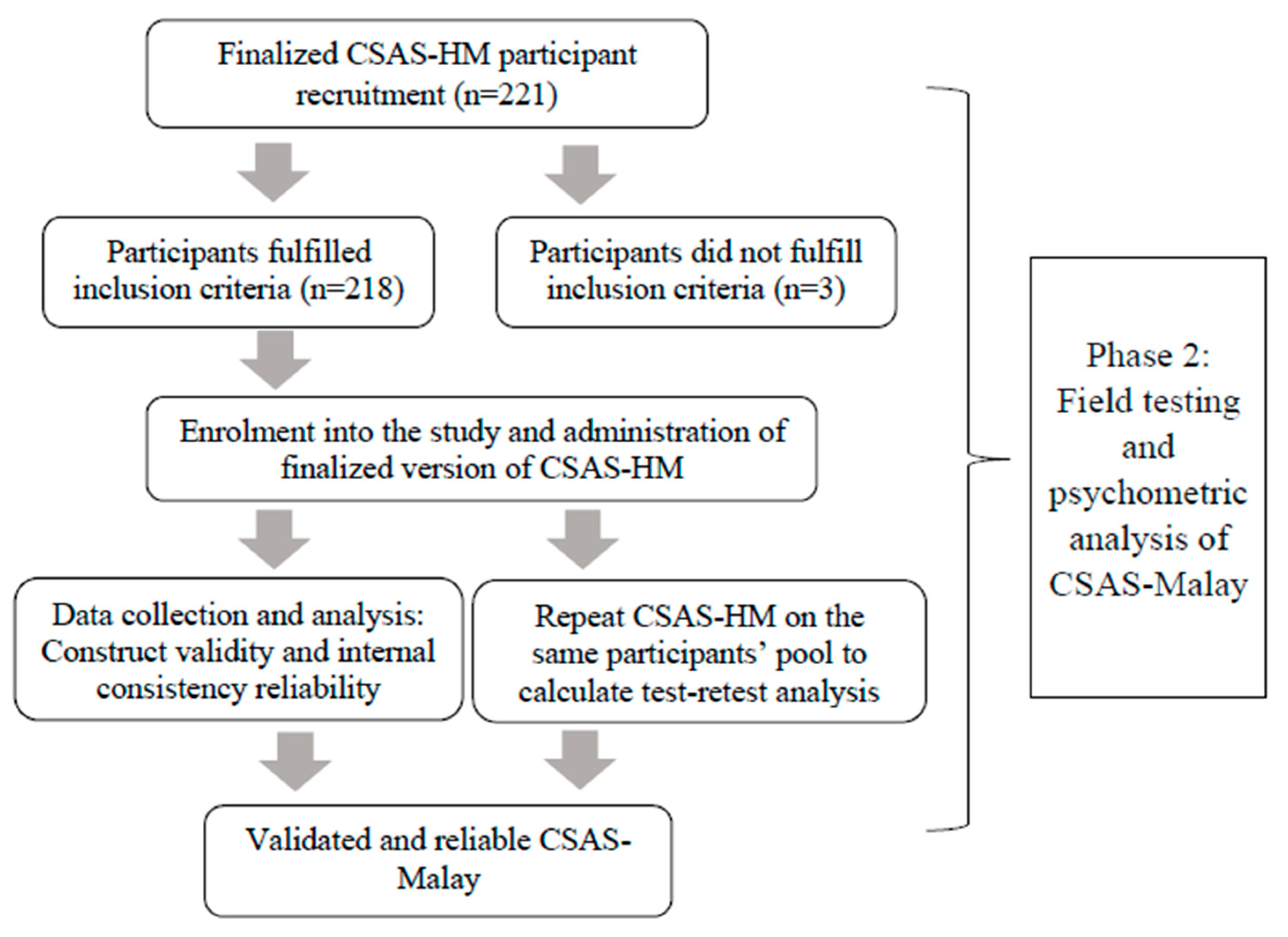
2.3.2. Phase 2: Field Testing and Psychometric Analysis
2.4. Statistical Analysis
3. Results
3.1. Demographic Details of Participants
3.2. Cross-Cultural Adaptation, Translation, and Face Validation
3.3. Psychometric Analysis
3.4. Reliability
4. Discussion
4.1. Strengths and Limitations
4.2. Implications on Curriculum Improvement & Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. CSAS Original
- In order to be a good doctor I must have good communication skills
- I can’t see the point in learning communication skills
- Nobody is going to fail their medical degree for having poor communication skills
- Developing my communication skills is just as important as developing my knowledge of medicine
- Learning communication skills has helped or will help me respect patients
- I haven’t got time to learn communication skills
- Learning communication skills is interesting
- I can’t be bothered to turn up to sessions on communication skills
- Learning communication skills has helped or will help facilitate my team-working skills
- Learning communication skills has improved my ability to communicate with patients
- Communication skills teaching states the obvious and then complicates it
- Learning communication skills is fun
- Learning communication skills is too easy
- Learning communication skills has helped or will help me respect my colleagues
- I find it difficult to trust information about communication skills given to me by non-clinical lecturers
- Learning communication skills has helped or will help me recognize patients’ rights regarding confidentiality and informed consent
- Communication skills teaching would have a better image if it sounded more like a science subject
- When applying for medicine, I thought it was a really good idea to learn communication skills
- I don’t need good communication skills to be a doctor
- I find it hard to admit to having some problems with my communication skills
- I think it’s really useful learning communication skills on the medical degree
- My ability to pass exams will get me through medical school rather than my ability to communicate
- Learning communication skills is applicable to learning medicine
- I find it difficult to take communication skills learning seriously
- Learning communication skills is important because my ability to communicate is a lifelong skill
- Communication skills learning should be left to psychology students, not medical students
Appendix B. CSAS-Malay
- Saya tidak nampak kepentingan mempelajari kemahiran komunikasi
- Pelajar perubatan tidak akan gagal dalam memperoleh ijazah perubatan kerana mempunyai kemahiran komunikasi yang lemah
- Menguasai kemahiran komunikasi adalah sama pentingnya dengan menguasai ilmu perubatan
- Mempelajari kemahiran berkomunikasi telah membantu atau akan membantu saya untuk menghormati pesakit
- Saya tiada masa untuk mempelajari kemahiran komunikasi
- Mempelajari kemahiran komunikasi adalah menarik
- Saya tidak peduli untuk menghadiri kelas kemahiran komunikasi
- Mempelajari kemahiran komunikasi telah membantu atau akan menambahkan kemahiran saya bekerja secara berpasukan
- Mempelajari kemahiran komunikasi telah menambah baik kebolehan saya berkomunikasi dengan pesakit
- Mempelajari kemahiran komunikasi adalah menyeronokkan
- Mempelajari kemahiran komunikasi terlalu mudah
- Mempelajari kemahiran komunikasi telah atau akan membantu saya menghormati rakan sekerja
- Saya berasa sukar untuk menerima ilmu kemahiran komunikasi yang diajar oleh pensyarah bukan dari bidang perubatan
- Pengajaran kemahiran komunikasi akan lebih menarik jika ia disampaikan seperti subjek sains
- Semasa memohon kursus perubatan, saya fikir mempelajari kemahiran komunikasi adalah idea yang sangat baik
- Kemahiran komunikasi yang baik tidak diperlukan untuk menjadi seorang doctor
- Saya berasa sukar untuk mengakui terdapat sedikit masalah dengan kemahiran komunikasi saya
- Saya berpandangan mempelajari kemahiran komunikasi sangat berguna semasa kursus perubatan
- Keupayaan saya untuk lulus peperiksaan akan memastikan saya lulus jurusan perubatan dan bukannya kemampuan saya berkomunikasi
- Mempelajari kemahiran komunikasi boleh diaplikasikan dalam mempelajari ilmu perubatan
- Saya berasa sukar untuk menganggap pembelajaran kemahiran komunikasi sebagai sesuatu yang serius
- Mempelajari kemahiran komunikasi sangat penting kerana kebolehan saya berkomunikasi merupakan kemahiran sepanjang hayat
- Kemahiran komunikasi sepatutnya hanya dipelajari oleh pelajar psikologi, bukannya pelajar perubatan
References
- Dictionary, B. Available online: http://www.businessdictionary.com/definition/communication-skills.html (accessed on 11 June 2020).
- Bukstein, D.A. Patient adherence and effective communication. Ann. Allergy Asthma Immunol. 2016, 117, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.; Silverman, J.; Draper, J. Teaching and Learning Communciation Skills in Medicine, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2005. [Google Scholar]
- Hausberg, M.C.; Hergert, A.; Kroger, C.; Bullinger, M.; Rose, M.; Andreas, S. Enhancing medical students’ communication skills: Development and evaluation of an undergraduate training program. BMC Med. Educ. 2012, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Australian Health Practitioner Regulation Agency. Good Medical Practice: A Code of Conduct for Doctors in Australia. Available online: https://www.medicalboard.gov.au/codes-guidelines-policies/code-of-conduct.aspx (accessed on 1 September 2020).
- General Medical Council. Outcomes for Graduates. Available online: https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates (accessed on 6 November 2020).
- Malaysian Medical Council. Guidelines for Accreditation of the Malaysian Undergraduate Medical Education Programme. Available online: http://www.mmc.gov.my/images/contents/downloadable/Accreditation%20Guidelines%202016.pdf (accessed on 1 September 2020).
- Busch, A.-K.; Rockenbauch, K.; Schmutzer, G.; Brähler, E. Do medical students like communication? Validation of the German CSAS (Communication Skills Attitude Scale). GMS Z. Med. Ausbild. 2015, 32, Doc11. [Google Scholar] [CrossRef] [PubMed]
- Harlak, H.; Gemalmaz, A.; Gurel, F.S.; Dereboy, C.; Ertekin, K. Communication skills training: Effects on attitudes toward communication skills and empathic tendency. Educ. Health 2008, 21, 62. [Google Scholar]
- Rees, C.; Sheard, C. Evaluating first-year medical students’ attitudes to learning communication skills before and after a communication skills course. Med. Teach. 2003, 25, 302–307. [Google Scholar] [CrossRef]
- Anvik, T.; Gude, T.; Grimstad, H.; Baerheim, A.; Fasmer, O.B.; Hjortdahl, P.; Holen, A.; Risberg, T.; Vaglum, P. Assessing medical students’ attitudes towards learning communication skills--which components of attitudes do we measure? BMC Med. Educ. 2007, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Khashab, S.S. Attitudes of alexandria medical students towards communication skills learning. J. Egypt Public Health Assoc. 2006, 81, 355–372. [Google Scholar] [PubMed]
- Rees, C.; Sheard, C.; Davies, S. The development of a scale to measure medical students’ attitudes towards communication skills learning: The Communication Skills Attitude Scale (CSAS). Med. Educ. 2002, 36, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Cleland, J.; Foster, K.; Moffat, M. Undergraduate students’ attitudes to communication skills learning differ depending on year of study and gender. Med. Teach. 2005, 27, 246–251. [Google Scholar] [CrossRef]
- Fazel, I.; Aghamolaei, T. Attitudes toward learning communication skills among medical students of a university in Iran. Acta Med. Iran. 2011, 49, 625–629. [Google Scholar]
- Benbassat, J.; Baumal, R.; Borkan, J.M.; Ber, R. Overcoming barriers to teaching the behavioral and social sciences to medical students. Acad. Med. 2003, 78, 372–380. [Google Scholar] [CrossRef]
- Rees, C.E.; Sheard, C.E.; McPherson, A.C. A qualitative study to explore undergraduate medical students’ attitudes towards communication skills learning. Med. Teach. 2002, 24, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Rees, C.; Sheard, C. The relationship between medical students’ attitudes towards communication skills learning and their demographic and education-related characteristics. Med. Educ. 2002, 36, 1017–1027. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Yi, Y.H.; Ahn, D.S. Developing a Korean communication skills attitude scale: Comparing attitudes between Korea and the West. Med. Educ. 2009, 43, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Ihmeideh, F.M.; Al-Omari, A.A.; Al-Dababneh, K.A. Attitudes Toward Communication Skills among Students’-Teachers’ in Jordanian Public Universities; Edith Cowan University: Joondalup, WA, Australia, 2010; Volume 35, pp. 1–11. [Google Scholar]
- Koponen, J.; Pyörälä, E.; Isotalus, P. Comparing three experiential learning methods and their effect on medical students’ attitudes to learning communication skills. Med. Teach. 2012, 34, e198–e207. [Google Scholar] [CrossRef]
- Molinuevo, B.; Torrubia, R. Validation of the Catalan version of the communication skills attitude scale (CSAS) in a cohort of south European medical and nursing students. Educ. Health 2011, 24, 499. [Google Scholar]
- Zhang, Y.; Jiang, G.; Sun, Y.; Zhao, X.; Yu, X. Cross-cultural adaptation and psychometric properties of the Chinese version of the Communication Skills Attitude Scale among medical students in Liaoning province, China: A cross-sectional study. BMJ Open 2018, 8, e020931. [Google Scholar] [CrossRef]
- Baharudin, N.; Yassin, M.S.M.; Badlishah-Sham, S.F.; Yusof, Z.Y.M.; Ramli, A.S. Validation of the Communication Skills Attitude Scale (CSAS) Questionnaire in a Cohort of Malaysian Medical Students. J. Clin. Health Sci. 2017, 2, 46–53. [Google Scholar] [CrossRef]
- Gjersing, L.; Caplehorn, J.R.; Clausen, T. Cross-cultural adaptation of research instruments: Language, setting, time and statistical considerations. BMC Med. Res. Methodol. 2010, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Prinsen, C.A.; Bouter, L.M.; Vet, H.C.; Terwee, C.B. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) and how to select an outcome measurement instrument. Braz. J. Phys. Ther. 2016, 20, 105–113. [Google Scholar] [CrossRef]
- Armstrong, T.S.; Cohen, M.Z.; Eriksen, L.; Cleeland, C. Content validity of self-report measurement instruments: An illustration from the development of the Brain Tumor Module of the M.D. Anderson symptom inventory. Oncol. Nurs. Forum. 2005, 32, 669–676. [Google Scholar] [CrossRef]
- Rodrigues, I.B.; Adachi, J.D.; Beattie, K.A.; MacDermid, J.C. Development and validation of a new tool to measure the facilitators, barriers and preferences to exercise in people with osteoporosis. BMC Musculoskelet. Disord. 2017, 18, 540. [Google Scholar] [CrossRef]
- Zamanzadeh, V.; Ghahramanian, A.; Rassouli, M.; Abbaszadeh, A.; Alavi-Majd, H.; Nikanfar, A.R. Design and implementation content validity study: Development of an instrument for measuring patient-centered communication. J. Caring. Sci. 2015, 4, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Lynn, M.R. Determination and quantification of content validity. Nurs. Res. 1986, 35, 382–385. [Google Scholar] [CrossRef] [PubMed]
- Polit, D.F.; Beck, C.T. The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; Sage: London, UK, 2018. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics, 7th ed.; Pearson: Boston, MA, USA, 2019. [Google Scholar]
- Wood, N.D.; Akloubou Gnonhosou, D.C.; Bowling, J. Combining parallel and exploratory factor analysis in identifying relationship scales in secondary data. Marriage Fam. Rev. 2015, 51, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Litwin, M.S. How to Measure Survey Reliability and Validity; Sage: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Singh, A.S.; Vik, F.N.; Chinapaw, M.J.M.; Uijtdewilligen, L.; Verloigne, M.; Fernández-Alvira, J.M.; Stomfai, S.; Manios, Y.; Martens, M.; Brug, J. Test-retest reliability and construct validity of the ENERGY-child questionnaire on energy balance-related behaviours and their potential determinants: The ENERGY-project. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 136. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Rubio, D.M.; Berg-Weger, M.; Tebb, S.S.; Lee, E.S.; Rauch, S. Objectifying content validity: Conducting a content validity study in social work research. Soc. Work Res. 2003, 27, 94–104. [Google Scholar] [CrossRef]
| Characteristics of Participants | Total (n = 218) N (%) | Median (Interquartile Range) |
|---|---|---|
| Age (years) | 19(0.00) | |
| 19 | 205(94) | |
| 20 | 3(1.4) | |
| 21 | 8(3.7) | |
| 23 | 1(0.5) | |
| 25 | 1(0.5) | |
| Gender | ||
| Male | 61(28) | |
| Female | 157(72) | |
| Ethnicity | ||
| Malay | 214(98.2) | |
| Non-Malay | 4(1.8) | |
| Family monthly household income 1 | ||
| >MYR13148 | 50(22.9) | |
| MYR3001-13147 | 106(48.7) | |
| <MYR3001 | 54(24.8) | |
| Not known | 8(3.7) | |
| First language | ||
| Malay | 204(93.6) | |
| English | 13(6.0) | |
| Others | 1(0.4) | |
| Self-rating on communication skills | ||
| Very good | 11(5.0) | |
| Good | 119(54.6) | |
| Satisfactory | 69(31.7) | |
| Weak | 18(8.3) | |
| Very weak | 1(0.5) | |
| Do students think their communication skills need improving | ||
| Yes | 217(99.5) | |
| No | 1(0.5) |
| Items | Questions | Positive (P)/ Negative (N) Scale | Factor | |
|---|---|---|---|---|
| 1 | 2 | |||
| Q14 | Learning communication skills has helped or will help me respect my colleagues | P | 0.740 | −0.077 |
| Q10 | Learning communication skills has improved my ability to communicate with patients | P | 0.645 | −0.147 |
| Q9 | Learning communication skills has helped or will help facilitate my team-working skills | P | 0.673 | −0.366 |
| Q21 | I think it’s really useful learning communication skills on the medical degree | P | 0.662 | −0.324 |
| Q23 | Learning communication skills is applicable to learning medicine | P | 0.616 | −0.065 |
| Q16 | Learning communication skills has helped or will help me recognise patients’ rights regarding confidentiality and informed consent | P | 0.597 | −0.140 |
| Q25 | Learning communication skills is important because my ability to communicate is a lifelong skill | P | 0.554 | 0.143 |
| Q5 | Learning communication skills has helped or will help me respect patients | P | 0.531 | −0.308 |
| Q18 | When applying for medicine, I thought it was a really good idea to learn communication skills | P | 0.517 | −0.404 |
| Q4 | Developing my communication skills is just as important as developing my knowledge of medicine | P | 0.485 | −0.314 |
| Q12 | Learning communication skills is fun | P | 0.474 | −0.274 |
| Q26 | Communication skills learning should be left to psychology students, not medical students | N | −0.263 | 0.371 |
| Q24 | I find it difficult to take communication skills learning seriously | N | −0.207 | 0.553 |
| Q22 | My ability to pass exams will get me through medical school rather than my ability to communicate | P | −0.149 | 0.497 |
| Q8 | I can’t be bothered to turn up to sessions on communication skills | N | 0.116 | 0.518 |
| Q2 | I can’t see the point in learning communication skills | N | −0.284 | 0.488 |
| Q3 | Nobody is going to fail their medical degree for having poor communication skills | N | −0.083 | 0.436 |
| Q20 | I find it hard to admit to having some problems with my communication skills | N | 0.032 | 0.420 |
| Q19 | I don’t need good communication skills to be a doctor | N | −0.251 | 0.490 |
| Q6 | I haven’t got time to learn communication skills | N | −0.117 | 0.370 |
| Q13 | Learning communication skills is too easy | N | 0.382 | 0.335 |
| Q7 | Learning communication skills is interesting | P | 0.294 | −0.324 |
| Q17 | Communication skills teaching would have a better image if it sounded more like a science subject | N | 0.159 | 0.304 |
| Subscale | Cronbach’s Alpha | Items | Corrected Item-Total Correlation | Cronbach’s Alpha If Item Deleted | Intraclass Correlation Coefficient (ICC (95%CI)) |
|---|---|---|---|---|---|
| PAS | 0.815 | Q4 | 0.443 | 0.805 | 0.853 (0.699–0.929) |
| Q5 | 0.442 | 0.804 | 0.783 (0.555–0.895) | ||
| Q9 | 0.601 | 0.792 | 0.807 (0.599–0.907) | ||
| Q10 | 0.526 | 0.798 | 0.882 (0.747–0.944) | ||
| Q12 | 0.393 | 0.815 | 0.737 (0.449–0.874) | ||
| Q14 | 0.576 | 0.791 | 0.915 (0.822–0.959) | ||
| Q16 | 0.457 | 0.803 | 0.725 (0.425–0.868) | ||
| Q18 | 0.484 | 0.801 | 0.856 (0.703–0.931) | ||
| Q21 | 0.566 | 0.793 | 0.754 (0.490–0.881) | ||
| Q23 | 0.486 | 0.800 | 0.736 (0.452–0.873) | ||
| Q25 | 0.437 | 0.805 | 0.783 (0.556–0.889) | ||
| NAS | 0.614 | Q2 | 0.442 | 0.598 | 0.878 (0.749–0.941) |
| Q3 | 0.302 | 0.604 | 0.846 (0.680–0.926) | ||
| Q6 | 0.267 | 0.611 | 0.811 (0.607–0.909) | ||
| Q8 | 0.353 | 0.592 | 0.820 (0.630–0.913) | ||
| Q13 | 0.031 | 0.636 | 0.775 (0.551–0.891) | ||
| Q17 | 0.114 | 0.630 | 0.809 (0.605–0.907) | ||
| Q19 | 0.353 | 0.600 | 0.950 (0.898–0.976) | ||
| Q20 | 0.241 | 0.619 | 0.726 (0.431–0.868) | ||
| Q22 | 0.346 | 0.594 | 0.777 (0.492–0.897) | ||
| Q24 | 0.405 | 0.579 | 0.752 (0.494–0.880) | ||
| Q26 | 0.356 | 0.599 | 0.764 (0.510–0.887) | ||
| Q7(rev) | 0.225 | 0.618 | 0.852 (0.696–0.928) |
| Author [Reference] | Country | Language | Subscale | Cronbach’s Alpha | Items |
|---|---|---|---|---|---|
| Rees et al. [13] | United Kingdom | English | Positive attitude scale | 0.873 | 4,5,7,9,10,12,14,16,18,21,22,23,25 |
| Negative attitude scale | 0.805 | 1,2,3,6,8,11,13,15,17,19,20,24,26 | |||
| Mohamad Isa et al. | Malaysia | Malay | Positive attitude scale | 0.815 | 4,5,9,10,14,16,18,20,21,23,25 |
| (this study) | Negative attitude scale | 0.614 | 2,3,6,7,8,13,17,18,19,24,22,26 | ||
| Zhang et al. [23] | China | Chinese | Importance of communication skills | 0.771 | 1,4,5,9,10,14,16,21,25 |
| Negative beliefs | 0.601 | 2,6,8,11,13,15,19,24,26 | |||
| Motivation | 0.637 | 12,17,23 | |||
| Assessment | 0.704 | 3,20,22 | |||
| Busch et al. [8] | Germany | German | Positive attitude scale | 0.864 | 4,5,9,10,14,16,23 |
| Negative attitude scale | 0.838 | 2,6,7,11,12,15,17,19,21,24,25,26 | |||
| Koponen et al. [21] | Finland | Finnish | Positive attitude scale | 0.882–0.895 | 4,5,7,9,10,12,14,16,18,21,22,23,25 |
| Negative attitude scale | 0.794–0.828 | 1,2,3,6,8,11,13,15,17,19,20,24,26 | |||
| Molinuevo et al. [22] | Spain | Catalan | Positive attitude scale | 0.83 | 1,4,5,7,9,10,12,14,16,18,21,23,25 |
| Negative attitude scale | 0.64 | 2,3,6,8,11,15,17,20,22,24 | |||
| Ihmeideh et al. [20] | Jordan | Arab | Positive attitude scale | 0.87 | 4,5,7,9,10,12,14,16,18,21,22,23,25 |
| Negative attitude scale | 0.81 | 1,2,3,6,8,11,13,15,17,19,20,24,26 | |||
| Ahn et al. [19] | Korea | Korean | Facilitating interpersonal skill | 0.752 | 4,5,9,10,14,16 |
| Importance within medical context | 0.744 | 2,19,21,26 | |||
| Motivation | 0.68 | 8,11,23,24 | |||
| Assessment | 0.446 | 3,22 | |||
| Overconfidence | 0.496 | 13,20 | |||
| Harlak et al. [9] | Turkey | Turkish | Positive attitude scale | 0.92 | 1,4,5,7,8,9,10,12,13,14,16,18,21,23,25 |
| Negative attitude scale | 0.71 | 2,3,6,11,15,17,19,20,22,24,26 | |||
| Anvik et al. [11] | Norway | Norwegian | Learning | 0.861 | 2,6,7,8,10,11,12,13,18,21,24,25,26 |
| Importance | 0.532 | 1,3,4,19,22 | |||
| Respecting | 0.775 | 5,9,14,16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohamad-Isa, M.-Z.; Mohamed-Yassin, M.-S.; Badlishah-Sham, S.F.; Baharudin, N.; Ramli, A.S. Cross-Cultural Adaptation and Psychometric Properties of the Malay Version of the Communication Skills Attitude Scale (CSAS) among Medical Students in Malaysia. Int. J. Environ. Res. Public Health 2021, 18, 3778. https://doi.org/10.3390/ijerph18073778
Mohamad-Isa M-Z, Mohamed-Yassin M-S, Badlishah-Sham SF, Baharudin N, Ramli AS. Cross-Cultural Adaptation and Psychometric Properties of the Malay Version of the Communication Skills Attitude Scale (CSAS) among Medical Students in Malaysia. International Journal of Environmental Research and Public Health. 2021; 18(7):3778. https://doi.org/10.3390/ijerph18073778
Chicago/Turabian StyleMohamad-Isa, Mohamad-Zikri, Mohamed-Syarif Mohamed-Yassin, Siti Fatimah Badlishah-Sham, Noorhida Baharudin, and Anis Safura Ramli. 2021. "Cross-Cultural Adaptation and Psychometric Properties of the Malay Version of the Communication Skills Attitude Scale (CSAS) among Medical Students in Malaysia" International Journal of Environmental Research and Public Health 18, no. 7: 3778. https://doi.org/10.3390/ijerph18073778
APA StyleMohamad-Isa, M.-Z., Mohamed-Yassin, M.-S., Badlishah-Sham, S. F., Baharudin, N., & Ramli, A. S. (2021). Cross-Cultural Adaptation and Psychometric Properties of the Malay Version of the Communication Skills Attitude Scale (CSAS) among Medical Students in Malaysia. International Journal of Environmental Research and Public Health, 18(7), 3778. https://doi.org/10.3390/ijerph18073778






