The Economic Costs of Childhood Disability: A Literature Review
Abstract
1. Introduction
- To identify costs of childhood disability from selected references and categorize them according to setting, type of disability, perspective, and time horizon.
- To quantify the burden of disability on the health system and society by comparing the cost to current health expenditure (CHE) per capita and gross domestic product (GDP) per capita.
2. Materials and Methods
2.1. Searching Strategy and Databases
2.2. Identifying Relevant Literature
2.3. Data Extraction
2.4. Categorizing Costs
- Direct-medical: costs for diagnosis, treatment, managing complications of the condition causing the disability.
- Direct non-medical: includes special education, rehabilitation, and transportation costs.
- Indirect non-medical: productivity loss and time lost by parents due to caring for the disabled child.
- Future related: medical costs related to the condition causing disability that happen in the future years.
- Future unrelated: includes future productivity loss by the disabled children and their caregivers.
2.5. Critical Appraisal
2.6. Synthesis of Evidence
- ○
- Country (name, developed/developing)
- ○
- Perspective (household, health system, or societal perspective)
- ○
- Methods of costing
- ○
- Disability category (types of disability/medical condition)
- ○
- Time horizon
2.7. Summarizing Results and Currency Conversion
3. Results
3.1. Finding Relevant Studies
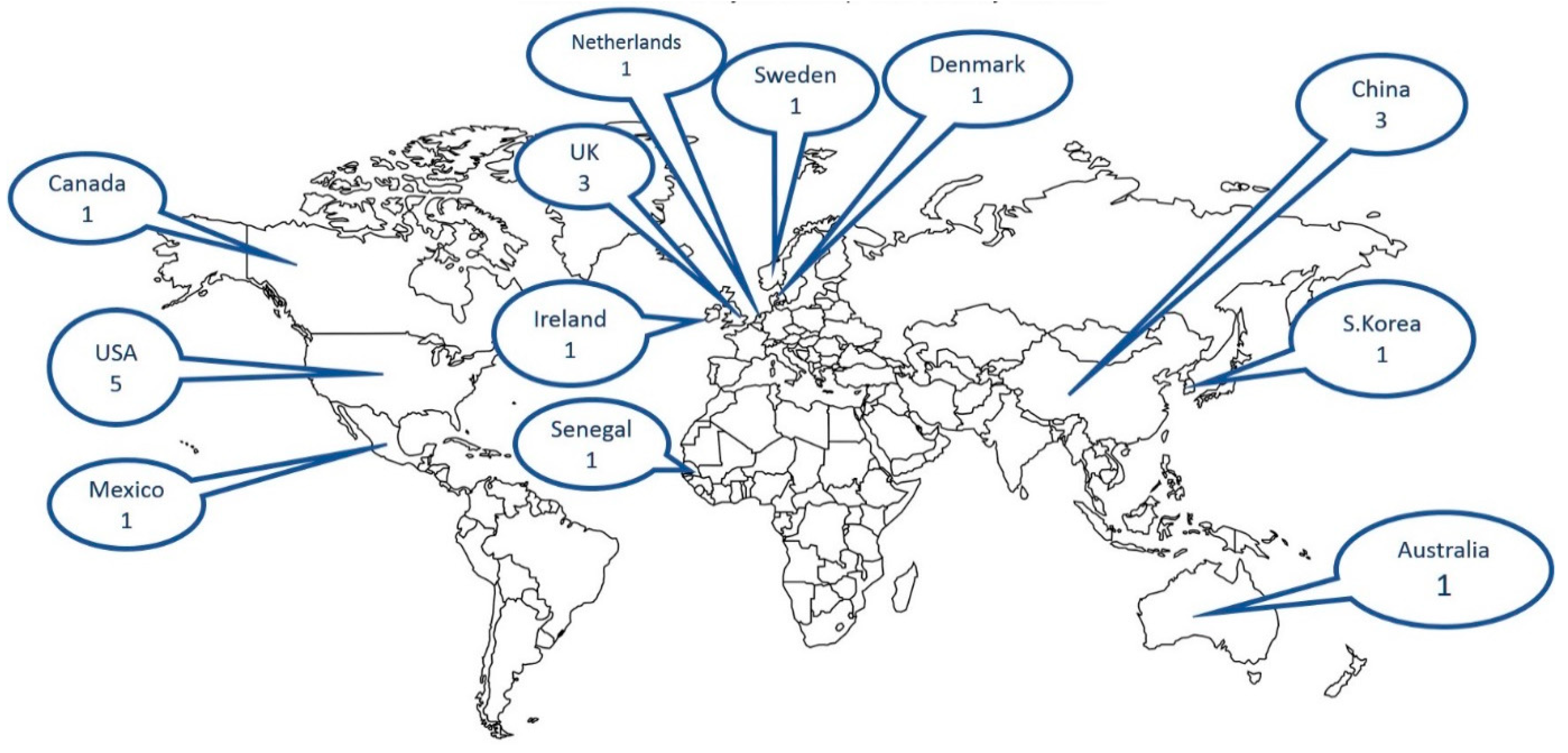
3.2. Summary of the Results
General Methodological Findings
3.3. Lifetime Cost Studies
3.4. Magnitude of the Burden
4. Discussion
4.1. Definition of Disability
4.2. Human Capital vs. Friction Cost
4.3. Societal vs. Household vs. Health System Perspective
4.4. Developed vs. Developing
4.5. Mean vs. Median
4.6. How Significant Is the Burden?
4.7. Strengths and Limitations
4.8. Recommendations for Policy Makers
4.9. Need for Further Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Search Strategy for OVID Medline Database
- (cost* adj5 (economic or illness or sickness or disease* or care or direct or indirect)).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] (127447)
- exp “cost of illness”/ or exp healthcare costs/ (82347)
- 1 or 2 (146362)
- (disable* or disabilit* handicap* or impairment* paralys* paralyz*).mp. [mp=title, abstract, original title, nameof substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] (77792)
- exp Disabled Persons/ (62208)
- cerebral palsy.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] (26008)
- exp cerebral palsy/ (19602)
- (down* syndrome or mongolism or trisomy?21).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] (29343)
- exp down syndrome/ (23636)
- autis*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] (46566)
- exp Autistic Disorder/ or exp Autism Spectrum Disorder/ (26617)
- 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 (187674)
- (child* or boy* or girl* or adolescent* or infant* or pediatric* or paediatric or (schoolage* or (school adj1 age*)) or (preschool* or (pre adj1 school*))).mp. [mp=title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms] (3934927)
- exp child/ or exp Disabled Children/ or exp Child Health Services/ (1841396)
- 13 or 14 (3935165)
- 3 and 12 and 15 (1121)
- limit 16 to (english language and yr=“1980 -Current”) (1046)
Appendix B. Search Strategy for OVID Embase Database
- (cost* adj5 (economic or illness or sickness or disease* or care or direct or indirect)).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (284046)
- exp “cost of illness”/ or exp health care costs/ (291451)
- 1 or 2 (370332)
- (disable* or disabilit* handicap* or impairment* paralys* paralyz*).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (63633)
- exp Disabled Persons/ (57465)
- cerebral palsy.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (41772)
- exp cerebral palsy/ (38329)
- (down* syndrome or mongolism or trisomy?21).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (40125)
- exp down syndrome/ (36240)
- autis*.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (69358)
- exp Autistic Disorder/ or exp Autism Spectrum Disorder/ (63878)
- 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 (230190)
- (child* or boy* or girl* or adolescent* or infant* or pediatric* or paediatric or (schoolage* or (school adj1 age*)) or (preschool* or (pre adj1 school*))).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] (4146231)
- exp child/ or exp Disabled Children/ or exp Child Health Services/ (2909761)
- 13 or 14 (4427076)
- 3 and 12 and 15 (1415)
- limit 16 to (english language and yr=“1980-Current”) (1326)
Appendix C. Search Strategy for OVID Econlit Database
- (disable* or disabilit* handicap* or impairment* paralys* paralyz*).mp. [mp=heading words, abstract, title, country as subject] (1187)
- cerebral palsy.mp. [mp=heading words, abstract, title, country as subject] (9)
- (down* syndrome or mongolism or trisomy?21).mp. [mp=heading words, abstract, title, country as subject] (10)
- autis*.mp. [mp=heading words, abstract, title, country as subject] (70)
- (child* or boy* or girl* or adolescent* or infant* or pediatric* or paediatric or (schoolage* or (school adj1 age*)) or (preschool* or (pre adj1 school*))).mp. [mp=heading words, abstract, title, country as subject] (39334)
- (cost* or burden*).mp. [mp=heading words, abstract, title, country as subject] (191228)
- 1 or 2 or 3 or 4 (1268)
- 5 and 6 and 7 (44)
- limit 8 to (yr=“1980-Current” and english) (42)
Appendix D. Search Strategy for OVID Global Health Database
- (cost* adj5 (economic or illness or sickness or disease* or care or direct or indirect)).mp. [mp=abstract, title, original title, broad terms, heading words, identifiers, cabicodes] (24319)
- exp “cost of illness”/ or exp health care costs/ (11630)
- estimated costs/ or health care costs/ or costs/ or social costs/ or unit costs/ or specific costs/ or total costs/ (26116)
- exp “cost analysis”/ or exp costs/ or exp “cost effectiveness analysis”/ (30831)
- 1 or 2 or 3 or 4 (38096)
- (disable* or disabilit* handicap* or impairment* paralys* paralyz*).mp. [mp=abstract, title, original title, broad terms, heading words, identifiers, cabicodes] (6019)
- exp Disabled Persons/ (4887)
- cerebral palsy.mp. [mp=abstract, title, original title, broad terms, heading words, identifiers, cabicodes] (1407)
- exp cerebral palsy/ (1061)
- (down* syndrome or mongolism or trisomy?21).mp. [mp=abstract, title, original title, broad terms, heading words, identifiers, cabicodes] (1981)
- autis*.mp. [mp=abstract, title, original title, broad terms, heading words, identifiers, cabicodes] (2467)
- disabilities.sh. (7353)
- exp disabilities/ or exp people with disabilities/ (11117)
- cerebral palsy.sh. (1061)
- exp autism/ (1831)
- Down’s syndrome.sh. (1623)
- 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 (18089)
- (child* or boy* or girl* or adolescent* or infant* or pediatric* or paediatric or (schoolage* or (school adj1 age*)) or (preschool* or (pre adj1 school*))).mp. [mp=abstract, title, original title, broad terms, heading words, identifiers, cabicodes] (530913)
- exp children/ (339666)
- 18 or 19 (530913)
- 5 and 17 and 20 (108)
- limit 21 to (english language and yr=“1980-Current”) (89)
Appendix E
| Yes | No | N/A | |
|---|---|---|---|
| Was a well-defined question posed in answerable form? | |||
| |||
| |||
| |||
| |||
| Were all the important and relevant costs identified? | |||
| |||
| |||
| |||
| Were costs measured accurately in appropriate physical units (e.g., hours of nursing time, number of physician visits, lost work-days)? | |||
| |||
| |||
| Were the costs valued credibly? | |||
| |||
| |||
| |||
| Were costs adjusted for differential timing? | |||
| |||
| |||
| Was uncertainty in the estimates of costs adequately characterized? | |||
| |||
| |||
| |||
| Did the presentation and discussion of study results include all issues of concern to users? | |||
| |||
| |||
| |||
Appendix F
| Author and Setting | Research Question | Perspective and Time Horizon | Medical Condition | Method of Disability Definition | Method(s) of Calculating Cost | Summary of the Main Findings/2019 Dollars | Comments |
|---|---|---|---|---|---|---|---|
| Francesca Solmi [33], 2018, UK, Developed | to quantify the cost of mental and physical disability in childhood and adolescence to families in the UK | household, weekly | multiple | Disability Discrimination Act definition | Compensating Variation | Annual additional costs to households with a mentally disabled child ≈$3600, for severely disabled child ≈$4200 and for physically disabled children ≈$2600 | New approach for estimating burden of disability |
| Martin Knapp [38], 2009, UK, Developed | to estimate the societal costs of Autism Spectrum Disorders (ASDs) in the UK by combining national data | societal, lifetime | ASD | Confirmed diagnosis of Autism or Pervasive Developmental Disorder (PDD) from a variety of tests and instruments in the original studies | modular approach from several sources to obtain nationally representative data cost per individual: service use data from recent studies lost productivity: estimated from national estimates of average weekly wage for full-time employees at April 2005 (£431) | Average annual total cost of supporting a child with ASDs ≈$42,500 Lifetime costs of a child with ASD and intellectual disability ≈$2 million | |
| Michael L. Ganz [39], 2007, USA, Developed | To estimate lifetime incremental societal costs of autism in the United States | societal, lifetime | ASD | multiple sources | (A prevalence-based cohort) cross-sectional cost data from different age groups were used to create prevalence-based cost estimates that approximate incidence-based estimates Direct medical and non-medical costs: obtained from the literature. Indirect costs: computed using human capital approach. Costs were projected across the life span, and discounted, then incremental age-specific costs were computed | The lifetime per capita incremental societal cost of autism is ≈$4.3 million | |
| Leslie S. Wilson [43], 2005, USA, Developed | compare types, amounts, and costs of care provided toHuman Immune deficiency Virus HIV-positive children and chronically ill children, using healthy children to control for basic care needs | societal, annual | multiple | Not clear | Human capital approachMarket replacement method to calculate the value of lost opportunity | Annual costs for homecare for chronically ill child ≈$36,000 and for HIV positive child ≈$13,000 Informal caregiving represents a substantial economic value to society | Provides good details on estimating opportunity costs |
| Marie Kruse [40], 2009, Denmark, Developed | to quantify the average societal costs of Cerebral Palsy (CP) per individual over a lifetime in Denmark | societal, lifetime | CP | CP cases registered in the National registry | Quantified health care, productivity, and social care costs by means of register-based data, in a cross-sectional perspective. Data for CP cases were linked to the information of national registers by the unique personal identifier, allowing identification of costs attributable to CP. Productivity loss estimated by human capital approach Social care costs: estimated from published information on average costs per user, and validated by a group of experts. | The lifetime costs of CP were fo males ≈$1.35 million and females ≈$1.25 millionhigh social care costs and productivity costs associated with CP Healthcare costs are only 7% of total lifetime societal costs | Good details on methods of calculating each type of cost. The unique personal identifier used in all Danish registers allows comprehensive register linkages and vast analysis opportunities. |
| Krister Jarbrink [44], 2007, Sweden, Developed | to describe and evaluate the societal costs of ASD for children living in a Swedish municipality | societal, annual | ASD | Confirmed diagnosis of ASD | Data collected from service use and combined with unit costsproductivity loss, by human capital approach (lost hour of work was valued using the average gross wage) The unit cost for valuation of losses in time for unpaid work and leisure time was set to 35 percent of the average gross wage | Additional annual societal cost due to ASD ≈$69,000 Main cost drivers are the community support services and schooling | very good methodology for estimating societal costs mall sample size |
| Elizabeth A. Geelhoed [45], 2011, Australia, Developed | To assess the direct annual health care costs for children and adolescents with Down syndrome (DS) in Western Australia | health system, annual | DS | children/young adults registered in Disability Services Commission with DS | Resource items: from survey reported by the family, computed to units per year, and costed according to the unit price Medical costs: from the Medical Benefit ScheduleHome and community care services: from the Disability Services Commission Hospital admission costs: mean bed day costMedications: Schedule of Pharmaceutical Benefits Complementary medicines, non-durable health-related products, and therapeutic devices: based on expenditure provided by the parents | The total mean annual health care costs across all age groups was ≈$3600, with a median of ≈$1500Overall, costs decrease with age with most costs in the first two years of life | Good details of how the cost of each item was calculated Costs presented in both meanto represent the total cost burden, and median to represent expected cost for an individual |
| Aine Roddy [46], 2019, Ireland, Developed | Estimate the societal cost of childhood ASDs and explain the variation in costs between state and family Out-Of-Pocket (OOP) expenditure | societal, annual | ASD | from autism organizations database and social media! | Data collected through an online survey to parentsA bottom-up prevalence based cost-of-illness methodology adopting a societal perspective Resources consumed: multiplied by unit costs then summed to produce individual aggregate costs Parental OOP expenditure: only attributable to ASD Informal care costs: only for parents who gave up employment because of their child’s condition using a human capital approachbased on the industrial wage per hour | Annual average family OOP costs for ASD case ≈$33,500 Annual average state expenditure per ASD child ≈$16,500 | good details on costing methods, systematic NO control group /low response rate /convenience sample, may not representative |
| Bin Wang [42], 2008, China, Developing | Measure the economic burden of CP in China and its societal impact | societal, lifetime | CP | Confirmed CP diagnostic documentation from a secondary or tertiary hospital | Estimates were obtained from interviewing caregivers of individuals with CP Human capital approach for indirect cost Incidence approach rather than prevalenceservice demand rather than need | Average lifetime economic burden of a new CP case born in China in 2003 ≈$91,000 Indirect (productivity) costs are responsible for 93% of total economic loss, and direct healthcare and developmental costs make up 3% each | sample bias is likely as they only recruited 319 patients (all admitted in hospitals) because there is no registry |
| Dallas Genereaux [47], 2015, Canada, Developed | estimate OOP costs to parents, and the non-health system costs to society, of raising a child with intellectual developmental disorder (IDD) | societal, annual | multiple | Confirmed diagnosis of IDD of unknown cause | Directly reported costs: taken at face value Opportunity costs: by human capital approach (market-replacement method based on job classification) Non-hospital therapies: cost per encounter method using labor-market wages for the position Non-parent volunteered care: labor market average rate Income loss by parents: hourly wage or yearly income based on their current or most recent job | Median annual parental costs of caring for an IDD child ≈$37,000 Median annual non-health system societal costs ≈$23,000 Main parental cost drivers = income loss and care giving time Main societal cost driver = special educationParental and societal costs increase with IDD severity Parental costs are not adequately compensated by government | Very nuanced description of how each cost was estimated Small sample size, no comparison group |
| Silvia Martınez-Valverde [48], 2019, Mexico, Developing | Investigate the burden of OOP household expenditures and time spent on care by families responsible for children with DS | household, annual | DS | Confirmed diagnosis of DS in the outpatient clinic of the genetics department | Cross-sectional analysis based on survey of families of DS childrenTotal OOP expenditures = medical care and transportation for one year Available household expenditures = total household expenditures—the cost of food and housing Catastrophic expenditures = if total OOP on medical care and transportation >30% of available household expenditures | 67% of the households with children with DS were within the lower four deciles (I–IV) of expenses, indicating a limited ability to pay for medical services. Yearly OOP expenditures for a child with DS represented 27% of the available household expenditure, which is equivalent to ≈$500 33% of families with DS children had catastrophic expenses 46% of the families had to borrow money to pay for medical expenses | Highlight differences in the health system between developed vs developing countries where the family pays a lot of OOP |
| Paul W. Newacheck [49], 2004, USA, Developed | To examine health care utilization and expenditure patterns for children with disabilities | health system, annual | multiple | Bio-psycho-social approach | not clear if self-reported or from insurance claims! | children with disabilities had much higher health care expenditures ≈$3800 than non-disabled ≈$676 and higher OOP expenditures Low-income families are especially vulnerable to burdensome OOP | |
| M A Hoving [50], 2007, Netherlands, Developed | Estimate and categorize the expenditures for children with intractable spastic CP | societal, annual | CP | Diagnosis with intractable spastic CP | Bottom-up, disease specific, prevalence-based cost-of-illness study | From a societal perspective, mean annual costs were ≈$57,000 more than 11 times the CHE per capita 95% of costs are outside the medical care sector The societal costs are 71% paid by the health insurers, 24% by the government, 5% by the families | |
| Andrew Kageleiry [35], 2016, USA, Developed | To estimate incremental medical costs for DS children, up to the age of 18 years in the USA | health system, 0-18 years | DS | International Classification of Diseases, Ninth revision, Clinical Modification (ICD-9-CM) diagnosis of DS | Claim database was used to conduct retrospective cohort study OOP expenses: from claims data (co-pay and co-insurance) The observation period for each individual was split into clinically relevant age categories | Average total incremental medical costs for a privately insured DS child from birth till 18 years of age ≈$275,000 of which ≈$20,000 are OOP expenses incurred by the family | Only direct OOP not including premium and not including education, transportation. very narrow scope |
| Moon Seok Park [41], 2011, South Korea, Developed | lifetime healthcare costs attributable to cerebral palsy in S. Korea | health system, lifetime | CP | CP diagnosis by Korean Standard Disease Classification Codes | Medical cost data attributable to CP was retrieved from claims data of the national health insurance according to the disease classification codes CP | The attributable lifetime medical cost of CP in South Korea was ≈$32,000, which is 1.8 times the basic lifetime medical cost of the general population | Lifetime cost calculated only from health system perspective but no direct non-medical cost / no OOP / no indirect costs or lost productivity Narrow scope for lifetime |
| Barbara Barrett [34], 2015, UK, Developed | Utilization and costs for: adolescents with autistic disorder, adolescents with other ASDs, adolescents with other special educational needs and typically developing adolescents | societal, 6 months | ASD | Clinically diagnosed ASD according to ICD-10 | Resource use data: self-reported via interview of parents Total costs: multiply each resource used by unit costs of public services in UK | Costs per individual were highest in the autistic disorder group (≈$35,100), followed by the special educational needs group (≈$29,500), the broader autism spectrum disorder group (≈$28,500) and the typically developing group (≈$9500) | STRENGTH: There is comparison group/highlights significant cost of educational services in ASD WEAKNESS: no indirect family cost, no OOP costs calculated |
| Chun-Zi Peng [51], 2009, USA, Developed | To estimate healthcare utilization rates and cost of care for children with pervasive developmental disorders (PDD) | health system, annual | multiple | Children with PPD diagnosis by ICD-9 | Costs were calculated by summing the claim charges. | Average annual medical cost for children with PDD ≈$10,500, eight times that of normal children | Claims analysis with only direct healthcare data not including OOP/education/other non-medical related expenditures/no societal cost |
| Ulla K. Griffiths [36], 2012, Senegal, Developing | estimate the costs of meningitis sequelae in children in Senegal from the perspective of households | household, lifetime | Bacterial meningitis | “sequela” was defined according to the 2006 Global Burden of Disease project | Self-reported by caregivers even for lostproductivity i.e., income foregone (more appropriate to low-income settings than the human capital or the friction cost approach) | Lifetime cost of meningitis sequelae (≈$41,000) is approximately 26 times higher than the mean cost of treating an acute meningitis episode | The first study that has assessed the costs of meningitis sequelae from the perspective of households in a low-income setting. |
| Nina Xiong [52], 2011, China, Developing | To estimate family costs of raising autistic, physically disabled, or mentally disabled children | household, annual | multiple | Not clear | Formula: the raising burden of children with disability = [(the income per person per year of family of normal children—that of family of disabled children) + (the cost per person per year of disabled children—that of normal children)—(the economic assistance per family per year of disabled children—assistance of normal children)] | Annual average raising burden of children with autism ≈$3600, physical disability ≈$3000, mental disability ≈$1200 | |
| Jian-Jun Ou [37], 2015, China, Developing | evaluate the employment and financial burdens of families with ASD-diagnosed pre-schoolers | household, annual | ASD | diagnosed with ASD in a local hospital | A questionnaire with open questions: (How much total income do you expect that all family members would have earned in the past year if your child did not have the disease?) (What were the total educational expenses of the ASD or OD child in your household over the past year, including general/special school education, extracurricular practice, related books/materials, and so on?) | The average loss of annual income associated with having a child with ASD was ≈$7500, compared with ≈$3500 for families of OD children | Opportunity cost is measured through parents’ reporting rather than the typical human capital method |
References
- World Health Organisation; World Bank. World report on disability. Lancet 2011, 377. Available online: http://www.larchetoronto.org/wordpress/wp-content/uploads/2012/01/launch-of-World-Report-on-Disability-Jan-27-121.pdf (accessed on 10 July 2019). [CrossRef]
- WHO. WHO Disability and Health Fact Sheet. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/disability-and-health (accessed on 29 October 2018).
- World Health Organization; UNICEF. Early Childhood Development & Disability: A Discussion Paper; WHO Press: Geneva, Switzerland, 2012; pp. 1–36. [Google Scholar]
- Cappa, C.; Petrowski, N.; Njelesani, J. Navigating the landscape of child disability measurement: A review of available data collection instruments. Alter 2015, 9, 317–330. [Google Scholar] [CrossRef]
- Maulik, P.K.; Darmstadt, G.L. Childhood Disability in Low- and Middle-Income Countries: Overview of Screening, Prevention, Services, Legislation, and Epidemiology. Pediatrics 2007, 120, S1–S55. [Google Scholar] [CrossRef]
- Mitra, S.; Posarac, A.; Vick, B. Disability and Poverty in Developing Countries: A Multidimensional Study. World Dev. 2013, 41, 1–18. [Google Scholar] [CrossRef]
- Porterfield, S.L.; Tracey, C. Disentangling the Dynamics of Family Poverty and Child Disability: Does Disability Come First? Center for Social Development: Saint Louis, MO, USA, 2003. [Google Scholar]
- Dávila Quintana, C.D.; Malo, M.A. Poverty dynamics and disability: An empirical exercise using the European community household panel. J. Soc. Econ. 2012, 41, 350–359. [Google Scholar] [CrossRef]
- Yeo, R.; Moore, K. Including Disabled People in Poverty Reduction Work: “Nothing About Us, Without Us ”. World Dev. 2003, 31, 571–590. [Google Scholar] [CrossRef]
- Mizunoya, S.; Mitra, S.; Yamasaki, I. Disability and school attendance in 15 low- and middle-income countries. World Dev. 2018, 104, 388–403. [Google Scholar] [CrossRef]
- Filmer, D. Disability, Poverty, And Schooling in Developing Countries: Results from 14 Household Surveys. World Bank Econ. Rev. 2008, 22, 141–163. [Google Scholar] [CrossRef]
- Ali, Z.; Zulfiqar, A. Economics of Disability in Bangladesh; Shiree Working Paper No. 29; EEP/Shiree: Dhaka, Bangladesh, 2015; p. 16. [Google Scholar]
- Mont, D. Childhood Disability and Poverty. SSRN Electron. J. 2019. [Google Scholar] [CrossRef]
- Mont, D.; Cappa, C.; Chetri, N.B.; Dorji, C.; Hingst, G.; Khan, N. Poverty, Maternal Education and Child Disability: Evidence from Bhutan. Disabil. Int. Dev. 2013, 3, 13–20. Available online: www.zbdw.de (accessed on 11 July 2019).
- Hakim, G.; Jaganjac, N. A Note on Disability Issues in the Middle East and North Africa; The World Bank: Washington, DC, USA, 2005. [Google Scholar]
- Banks, L.M.; Polack, S. The Economic Costs of Exclusion and Gains of Inclusion of People with Disabilities: Evidence from Low and Middle Income Countries; International Centre for Evidence in Disability: London, UK, 2014. [Google Scholar]
- Mitra, S.; Palmer, M.; Kim, H.; Mont, D.; Groce, N. Extra costs of living with a disability: A review and agenda for research. Disabil. Health J. 2017, 10, 475–484. [Google Scholar] [CrossRef]
- Ettaro, L.; Songer, T.J.; Zhang, P.; Engelgau, M.M. Cost-of-Illness Studies in Diabetes Mellitus. PharmacoEconomics 2004, 22, 149–164. [Google Scholar] [CrossRef]
- Rice, D.P. Estimating the cost of illness. Am. J. Public Health Nations Health 1967, 57, 424–440. [Google Scholar] [CrossRef]
- Fox-Rushby, J.; Cairns, J. Economic Evaluation; McGraw-Hill Education: Berkshire, UK, 2005. [Google Scholar]
- Vassall, A.; Sweeney, S.; Kahn, J.G.; Gomez, G.; Bollinger, L.; Marseille, E.; Herzel, B.; Plosky, W.D.; Cunnama, L.; Sinanovic, E.; et al. Reference Case for Estimating the Costs of Global Health Services and Interventions; Global Health Cost Consortium: Washington, DC, USA, 2017. [Google Scholar]
- Stabile, M.; Allin, S. The Economic Costs of Childhood Disability. Future Child. 2012, 22, 65–96. [Google Scholar] [CrossRef] [PubMed]
- Beecham, J. Annual Research Review: Child and adolescent mental health interventions: A review of progress in economic studies across different disorders. J. Child Psychol. Psychiatry 2014, 55, 714–732. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.; Dumont, S.; Jacobs, P.; Azzaria, L. The Personal Costs of Caring for a Child with a Disability: A Review of the Literature. Public Health Rep. 2007, 122, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Siddaway, A.P.; Wood, A.M.; Hedges, L.V. How to Do a Systematic Review: A Best Practice Guide for Conducting and Reporting Narrative Reviews, Meta-Analyses, and Meta-Syntheses. Annu. Rev. Psychol. 2019, 70, 747–770. [Google Scholar] [CrossRef] [PubMed]
- Moher, D. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264. [Google Scholar] [CrossRef]
- World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 4 August 2020).
- Aveyard, H. Doing a Literature Review in Health and Social Care: A Practical Guide, 3rd ed.; Open University Press: Maidenhead, UK, 2014. [Google Scholar]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes, 4th ed.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- World Health Organization. Global Health Expenditure Database. 2019. Available online: https://apps.who.int/nha/database/ViewData/Indicators/en (accessed on 20 September 2019).
- International Monetary Fund. World Economic Outlook Database. 2018. Available online: https://www.imf.org/external/pubs/ft/weo/2018/02/weodata/weoselgr.aspx (accessed on 9 February 2019).
- International Monetary Fund. Consumer Price Index—Сopy of By Country—IMF Data [Internet]. Available online: http://data.imf.org/?sk=4FFB52B2-3653-409A-B471-D47B46D904B5&sId=1485878802128 (accessed on 19 August 2019).
- Solmi, F.; Melnychuk, M.; Morris, S. The cost of mental and physical health disability in childhood and adolescence to families in the UK: Findings from a repeated cross-sectional survey using propensity score matching. BMJ Open 2018, 8, e018729. [Google Scholar] [CrossRef]
- Barrett, B.; Mosweu, I.; Jones, C.R.; Charman, T.; Baird, G.; Simonoff, E.; Pickles, A.; Happé, F.; Byford, S. Comparing service use and costs among adolescents with autism spectrum disorders, special needs and typical development. Autism 2015, 19, 562–569. [Google Scholar] [CrossRef]
- Kageleiry, A.; Samuelson, D.; Duh, M.S.; Lefebvre, P.; Campbell, J.; Skotko, B.G. Out-of-pocket medical costs and third-party healthcare costs for children with Down syndrome. Am. J. Med. Genet. Part A 2017, 173, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, U.K.; Dieye, Y.; Fleming, J.; Hajjeh, R.; Edmond, K. Costs of Meningitis Sequelae in Children in Dakar, Senegal. Pediatric Infect. Dis. J. 2012, 31, e189–e195. [Google Scholar] [CrossRef] [PubMed]
- Ou, J.-J.; Shi, L.-J.; Xun, G.-L.; Chen, C.; Wu, R.-R.; Luo, X.-R.; Zhang, F.-Y.; Zhao, J.-P. Employment and financial burden of families with preschool children diagnosed with autism spectrum disorders in urban China: Results from a descriptive study. BMC Psychiatry 2015, 15, 3. [Google Scholar] [CrossRef] [PubMed]
- Knapp, M.; Romeo, R.; Beecham, J. Economic cost of autism in the UK. Autism 2009, 13, 317–336. [Google Scholar] [CrossRef] [PubMed]
- Ganz, M.L. The Lifetime Distribution of the Incremental Societal Costs of Autism. Arch. Pediatric Adolesc. Med. 2007, 161, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Kruse, M.; Michelsen, S.I.; Flachs, E.M.; Brønnum-Hansen, H.; Madsen, M.; Uldall, P. Lifetime costs of cerebral palsy. Dev. Med. Child Neurol. 2009, 51, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Park, M.S.; Kim, S.J.; Chung, C.Y.; Kwon, D.G.; Choi, I.H.; Lee, K.M. Prevalence and lifetime healthcare cost of cerebral palsy in South Korea. Health Policy 2011, 100, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Chen, Y.; Zhang, J.; Li, J.; Guo, Y.; Hailey, D. A preliminary study into the economic burden of cerebral palsy in China. Health Policy 2008, 87, 223–234. [Google Scholar] [CrossRef]
- Wilson, L.S.; Moskowitz, J.T.; Acree, M.; Heyman, M.B.; Harmatz, P.; Ferrando, S.J.; Folkman, S. The Economic Burden of Home Care for Children with HIV and Other Chronic Illnesses. Am. J. Public Health 2005, 95, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Järbrink, K. The economic consequences of autistic spectrum disorder among children in a Swedish municipality. Autism 2007, 11, 453–463. [Google Scholar] [CrossRef]
- Geelhoed, E.A.; Bebbington, A.; Bower, C.; Deshpande, A.; Leonard, H. Direct Health Care Costs of Children and Adolescents with Down Syndrome. J. Pediatrics 2011, 159, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Roddy, A.; O’Neill, C. The economic costs and its predictors for childhood autism spectrum disorders in Ireland: How is the burden distributed? Autism 2019, 23, 1106–1118. [Google Scholar] [CrossRef]
- Genereaux, D.; Van Karnebeek, C.D.; Birch, P.H. Costs of caring for children with an intellectual developmental disorder. Disabil. Health J. 2015, 8, 646–651. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Valverde, S.; Salinas-Escudero, G.; García-Delgado, C.; Garduño-Espinosa, J.; Morán-Barroso, V.F.; Granados-García, V.; Tiro-Sánchez, M.T.; Toledano-Toledano, F.; Aldaz-Rodríguez, M.V. Out-of-pocket expenditures and care time for children with Down Syndrome: A single-hospital study in Mexico City. PLoS ONE 2019, 14, e0208076. [Google Scholar] [CrossRef] [PubMed]
- Newacheck, P.W.; Inkelas, M.; Kim, S.E. Health services use and health care expenditures for children with disabilities. Pediatrics 2004, 114, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Hoving, M.; Evers, S.M.; Ament, A.; Van Raak, E.; Vles, J. Intractable spastic cerebral palsy in children: A Dutch cost of illness study. Dev. Med. Child Neurol. 2007, 49, 397–398. [Google Scholar] [CrossRef]
- Peng, C.-Z.; Hatlestad, P.; Klug, M.G.; Kerbeshian, J.; Burd, L. Health Care Costs and Utilization Rates for Children with Pervasive Developmental Disorders in North Dakota from 1998 to 2004: Impact on Medicaid. J. Child Neurol. 2009, 24, 140–147. [Google Scholar] [CrossRef]
- Xiong, N.; Yang, L.; Yu, Y.; Hou, J.; Li, J.; Li, Y.; Liu, H.; Zhang, Y.; Jiao, Z. Investigation of raising burden of children with autism, physical disability and mental disability in China. Res. Dev. Disabil. 2011, 32, 306–311. [Google Scholar] [CrossRef]
- Melnychuk, M.; Solmi, F.; Morris, S. Using compensating variation to measure the costs of child disability in the UK. Eur. J. Health Econ. 2018, 19, 419–433. [Google Scholar] [CrossRef] [PubMed]
- Mihaylova, B.; Briggs, A.; O’Hagan, A.; Thompson, S.G. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2010, 20, 897–916. [Google Scholar] [CrossRef] [PubMed]

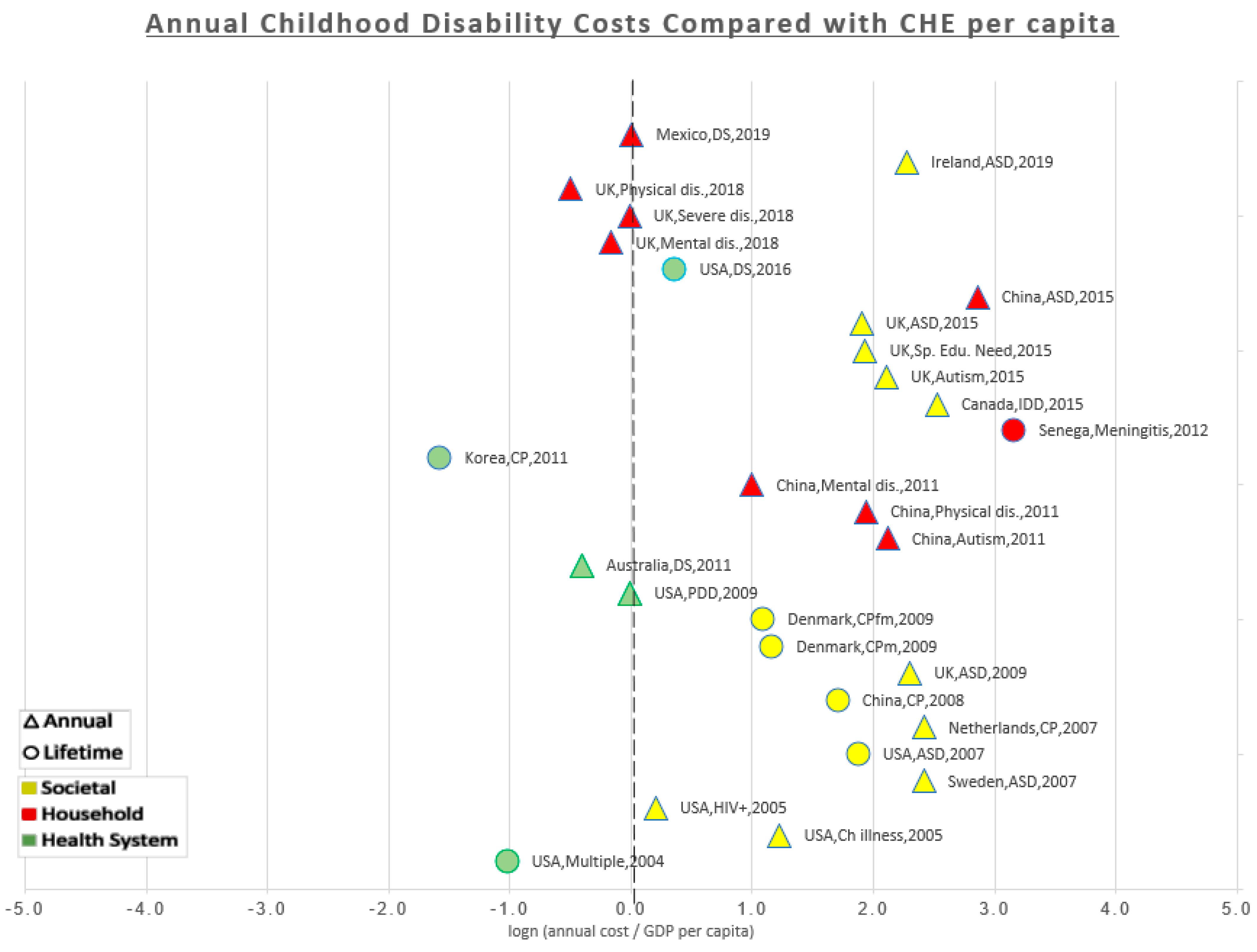
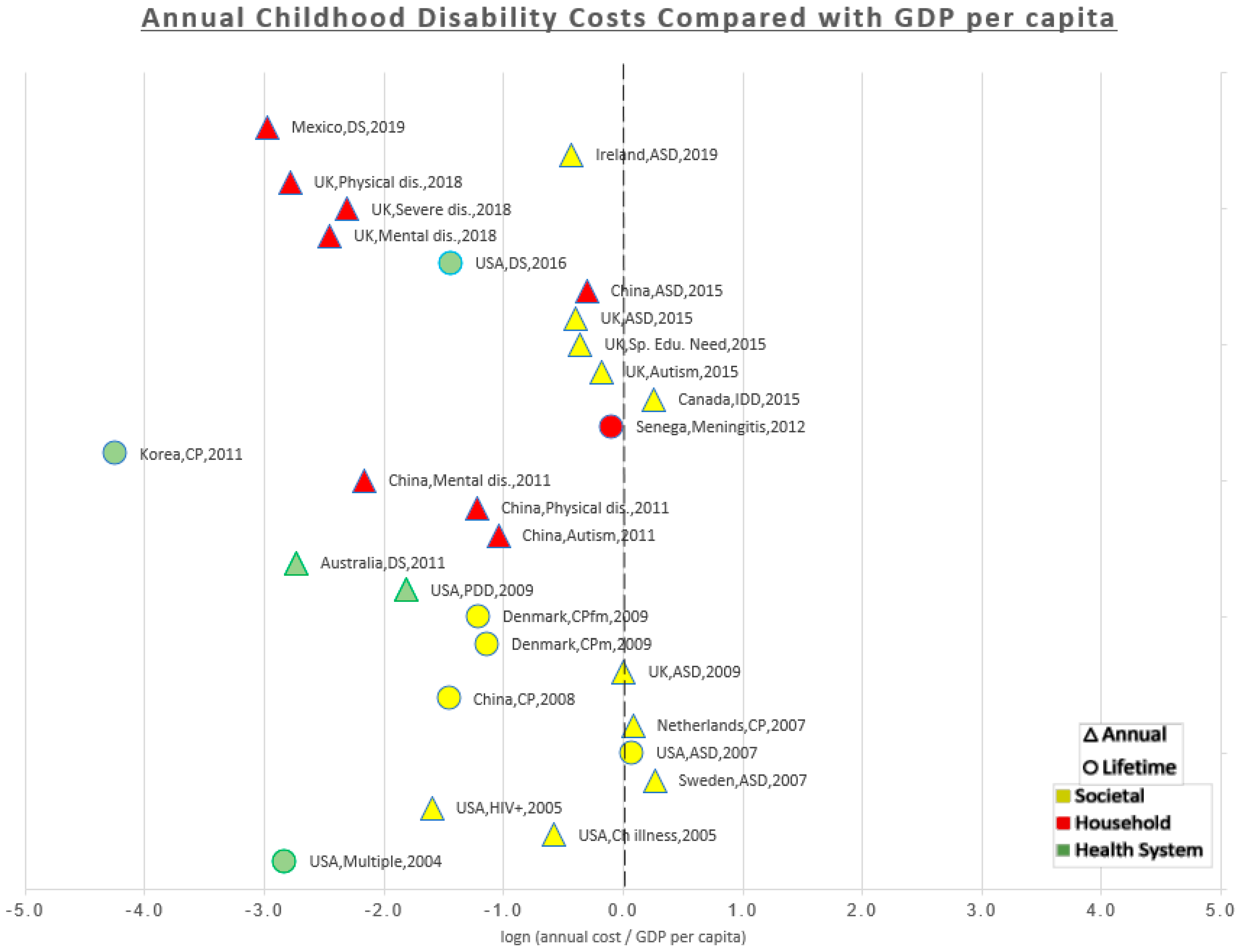
| First Author and Year of Publication | Setting | Perspective | Time Horizon | Medical Condition | Costs in 2019 US$ | CHE per Capita 2019 US$ (% of Estimated Costs) * | GDP per Capita 2019 US$ (% of Estimated Costs) ** |
|---|---|---|---|---|---|---|---|
| Solmi [33], 2018 | UK, Developed | Household | Weekly | Mentally Disabled | Annual 3625 | 4267 (85%) | 42,310 (9%) |
| Severely Disabled | Annual 4200 | 4267 (98%) | 42,310 (10%) | ||||
| Physically Disabled | Annual 2600 | 4267 (61%) | 42,310 (6%) | ||||
| Knapp [38], 2009 | UK, Developed | Societal | Lifetime | ASD | Lifetime 2,060,060 | ||
| Annual † 42,539 | 4267 (997%) | 42,310 (101%) | |||||
| Ganz [39], 2007 | USA, Developed | Societal | Lifetime | ASD | Lifetime 4,345,600 | ||
| Annual 69,530 | 10,640 (653%) | 64,767 (107%) | |||||
| Wilson [43], 2005 | USA, Developed | Societal | Annual | Chronically ill | Annual 36,310 | 10,640 (341%) | 64,767 (56%) |
| HIV positive | Annual 13,039 | 10,640 (123%) | 64,767 (20%) | ||||
| Kruse [40], 2009 | Denmark, Developed | Societal | Lifetime | CP | Lifetime 1,344,340 men 1,250,550 women | ||
| Annual 19,205 men 17,865 women | 6000 (320%) (298%) | 59,999 (32%) (30%) | |||||
| Jarbrink [44], 2007 | Sweden, Developed | Societal | Annual | ASD | Annual 68,863 | 6156 (1119%) | 53,004 (130%) |
| Geelhoed [45], 2011 | Australia, Developed | Health system | Annual | DS | Annual 3602 | 5393 (67%) | 55,421 (6%) |
| Roddy [46], 2019 | Ireland, Developed | Societal | Annual | ASD | Annual 49,867 | 5130 (972%) | 76,911 (65%) |
| Wang [42], 2008 | China, Developing | Societal | Lifetime | CP | Lifetime 91,046 | ||
| Annual 2365 | 429 (551%) | 10,153 (23%) | |||||
| Genereaux [47], 2015 | Canada, Developed | Societal | Annual | IDD | Annual 60,059 | 4806 (1250%) | 46,419 (129%) |
| Martınez-Valverde [48], 2019 | Mexico, Developing | Household | Annual | DS | Annual 501 | 498 (101%) | 9858 (5%) |
| Newacheck [49], 2004 | USA, Developed | Health system | Annual | Multiple | Annual 3833 | 10,640 (36%) | 64,767 (6%) |
| Hoving [50], 2007 | Netherlands, Developed | Societal | Annual | CP | Annual 57,383 | 5112 (1123%) | 53,016 (108%) |
| Kageleiry [35], 2016 | USA, Developed | Health system | Childhood (0–18 yrs) | DS | 0–18 yrs 275,603 | ||
| Annual 15,311 | 10,640 (144%) | 64,767 (24%) | |||||
| Park [41], 2011 | South Korea, Developed | Health system | Lifetime | CP | Lifetime 32,003 | ||
| Annual 457 | 2203 (21%) | 30,028 (1%) | |||||
| Barrett [34], 2015 | UK, Developed | societal | 6 months | Autistic Disorder | Annual 35,100 | 4267 (823%) | 42,310 (83%) |
| Special Educational Needs | Annual 29,503 | 4267 (691%) | 42,310 (70%) | ||||
| ASD | Annual 28,548 | 4267 (669%) | 42,310 (67%) | ||||
| Peng [51], 2009 | USA, Developed | Health system | Annual | PDD | Annual 10,538 | 10,640 (99%) | 64,767 (16%) |
| Griffiths [36], 2012 | Senegal, Developing | Household | Lifetime | Bacterial Meningitis | Lifetime 41,230 | ||
| Annual 1374 | 58 (2370%) | 1510 (91%) | |||||
| Xiong [52], 2011 | China, Developing | Household | Annual | Autism | Annual 3566 | 429 (831%) | 10,153 (35%) |
| Physical Disability | Annual 2989 | 429 (697%) | 10,153 (29%) | ||||
| Mental Disability | Annual 1164 | 429 (271%) | 10,153 (11%) | ||||
| Ou [37], 2015 | China, Developing | Household | Annual | ASD | Annual 7470 | 429 (1741%) | 10,153 (74%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahat, A.R.S.; Greco, G. The Economic Costs of Childhood Disability: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 3531. https://doi.org/10.3390/ijerph18073531
Shahat ARS, Greco G. The Economic Costs of Childhood Disability: A Literature Review. International Journal of Environmental Research and Public Health. 2021; 18(7):3531. https://doi.org/10.3390/ijerph18073531
Chicago/Turabian StyleShahat, Ahmed Ramadan Shokry, and Giulia Greco. 2021. "The Economic Costs of Childhood Disability: A Literature Review" International Journal of Environmental Research and Public Health 18, no. 7: 3531. https://doi.org/10.3390/ijerph18073531
APA StyleShahat, A. R. S., & Greco, G. (2021). The Economic Costs of Childhood Disability: A Literature Review. International Journal of Environmental Research and Public Health, 18(7), 3531. https://doi.org/10.3390/ijerph18073531






