Predictors of Psychological Distress in Women with Endometriosis: The Role of Multimorbidity, Body Image, and Self-Criticism
Abstract
1. Introduction
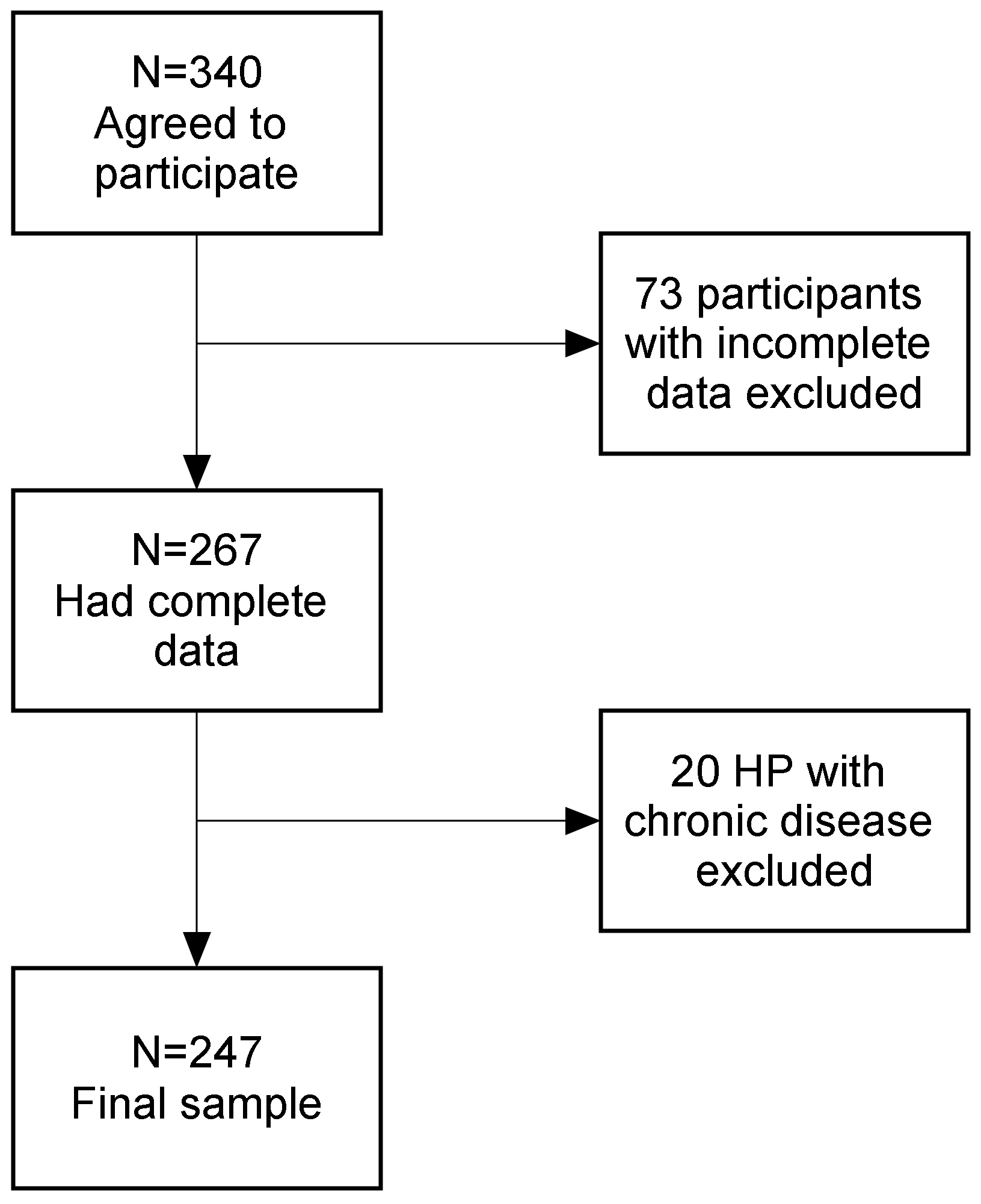
2. Materials and Methods
2.1. Measures
2.2. Statistical Analysis
3. Results
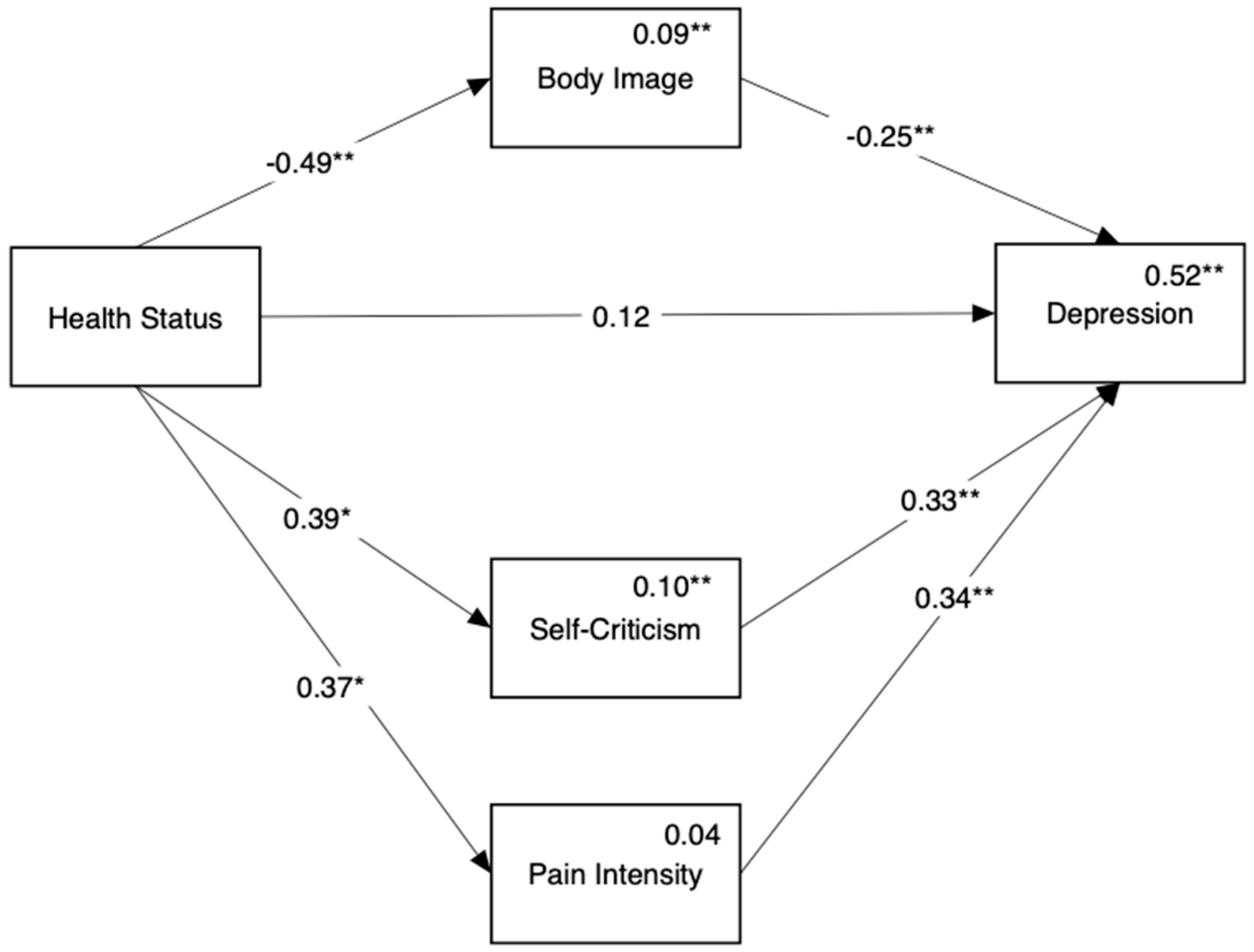
3.1. Role of Body Image and Self-Criticism in the Emergence of Depressive Symptoms in Endometriosis Participants
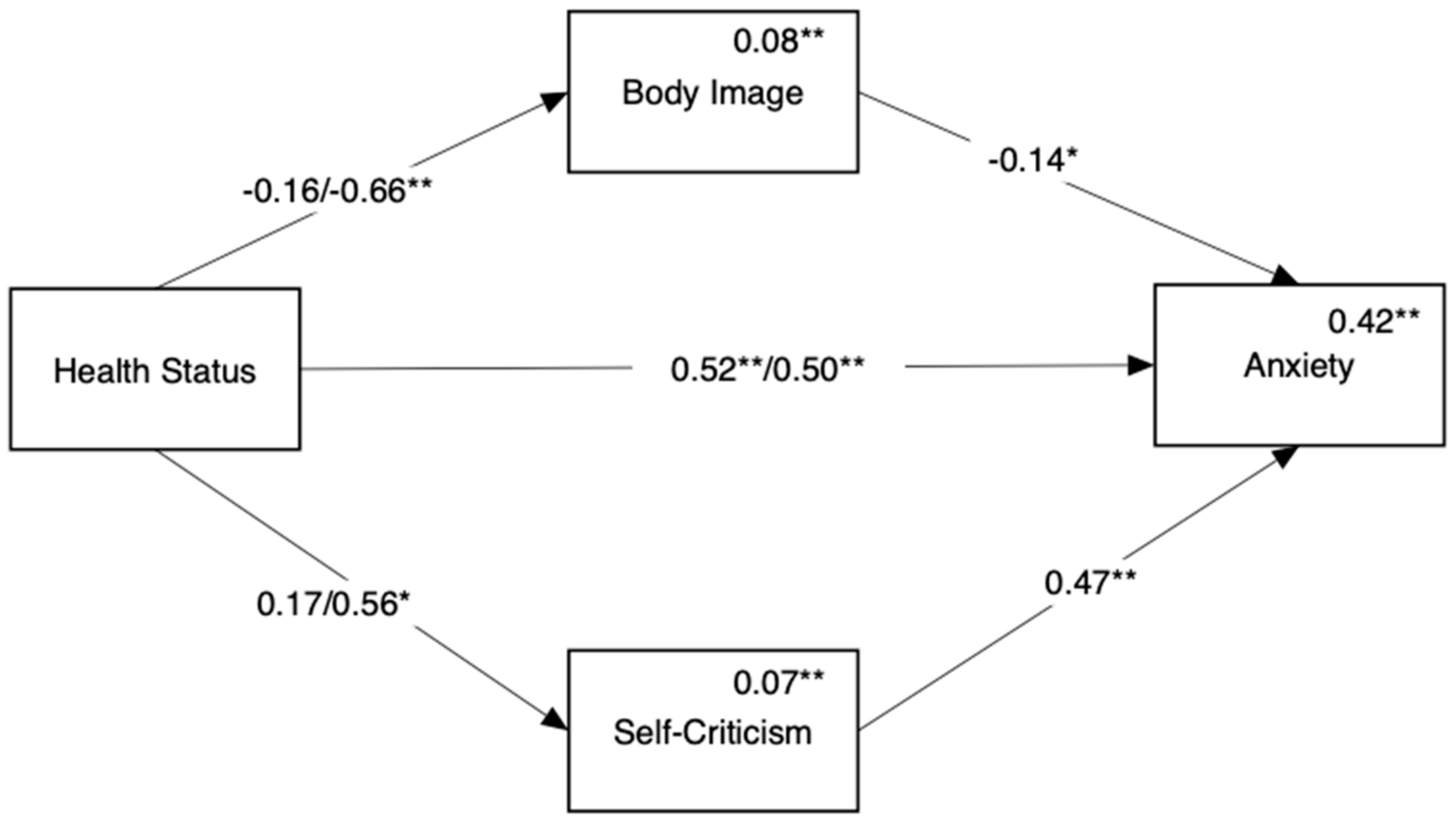
3.2. Role of Body Image and Self-Criticism in the Emergence of Depressive Symptoms in Endometriosis Participants with or without ACI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnson, N.P.; Hummelshoj, L.; Adamson, G.D.; Keckstein, J.; Taylor, H.S.; Abrao, M.S.; Bush, D.; Kiesel, L.; Tamimi, R.; Sharpe-Timms, K.L.; et al. World Endometriosis Society consensus on the classification of endometriosis. Hum. Reprod. 2017, 32, 315–324. [Google Scholar] [CrossRef]
- Painter, J.N.; Anderson, C.A.; Nyholt, D.R.; Macgregor, S.; Li, J.; Lee, S.H.; Lambert, A.; Zhao, Z.Z.; Roseman, F.; Guo, Q.; et al. Genome-wide association study identifies a locus at 7p15. 2 associated with endometriosis. Nat. Genet. 2011, 43, 51–54. [Google Scholar] [CrossRef]
- Bulletti, C.; Coccia, M.E.; Battistoni, S.; Borini, A. Endometriosis and infertility. J. Assist. Reprod. Genet. 2010, 27, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsov, L.; Dworzynski, K.; Davies, M.; Overton, C. Guideline committee diagnosis and management of endometriosis: Summary of NICE guidance. BMJ 2017, 358, j3935. [Google Scholar] [CrossRef]
- Lemaire, G. More than just menstrual cramps: Symptoms and uncertainty among women with endometriosis. J. Obstet. Gynecol. Neonatal Nurs. 2004, 1, 71–79. [Google Scholar] [CrossRef]
- De Nardi, P.; Ferrari, S. Deep Pelvic Endometriosis: A Multidisciplinary Approach; Springer: Milan, Italy, 2011. [Google Scholar]
- Meuleman, C.; Vandenabeele, B.; Fieuws, S.; Spiessens, C.; Timmerman, D.; D’Hooghe, T. High prevalence of endometriosis in infertile women with normal ovulation and normospermic partners. Fertil. Steril. 2009, 1, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.J.; Sharma, V.; Sharma, S.; Mazmanian, D. A systematic review of the association between psychiatric disturbances and endometriosis. J. Obstet. Gynaecol. Can. 2015, 37, 1006–1015. [Google Scholar] [CrossRef]
- Thomas, E.; Moss-Morris, R.; Faquhar, C. Coping with emotions and abuse history in women with chronic pelvic pain. J. Psychosom. Res. 2006, 60, 109–112. [Google Scholar] [CrossRef]
- Hudson, N.; Culley, L.; Law, C.; Mitchell, H.; Denny, E.; Raine-Fenning, N. “We needed to change the mission statement of the marriage”: Biographical disruptions, appraisals and revisions among couples living with endometriosis. Sociol. Health Illn. 2016, 38, 721–735. [Google Scholar] [CrossRef]
- Fritzer, N.; Haas, D.; Oppelt, P.; Renner, S.; Hornung, D.; Wölfler, M.; Ulrich, U.; Fischerlehner, G.; Sillem, M.; Hudelist, G. More than just bad sex: Sexual dysfunction and distress in patients with endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.E.; Kesmodel, U.S.; Baldursson, E.B.; Schultz, R.; Forman, A. The influence of endometriosis-related symptoms on work life and work ability: A study of Danish endometriosis patients in employment. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 331–339. [Google Scholar] [CrossRef]
- Donatti, L.; Ramos, D.G.; Andres, M.D.P.; Passman, L.J.; Podgaec, S. Patients with endometriosis using positive coping strategies have less depression, stress and pelvic pain. Einstein 2017, 15, 65–70. [Google Scholar] [CrossRef]
- Jia, S.Z.; Leng, J.H.; Shi, J.H.; Sun, P.R.; Lang, J.H. Health-related quality of life in women with endometriosis: A systematic review. J. Ovarian Res. 2012, 5, 29. [Google Scholar] [CrossRef]
- Friedl, F.; Riedl, D.; Fessler, S.; Wildt, L.; Walter, M.; Richter, R.; Schüßler, G.; Böttcher, B. Impact of endometriosis on quality of life, anxiety, and depression: An Austrian perspective. Arch. Gynecol. Obstet. 2015, 292, 1393–1399. [Google Scholar] [CrossRef] [PubMed]
- Vitale, S.G.; La Rosa, V.L.; Rapisarda, A.M.; Laganà, A.S. Impact of endometriosis on quality of life and psychological well-being. J. Psychosom. Obstet. Gynaecol. 2016, 38, 317–319. [Google Scholar] [CrossRef] [PubMed]
- Facchin, F.; Barbara, G.; Dridi, D.; Alberico, D.; Buggio, L.; Somigliana, E.; Saita, E.; Vercellini, P. Mental health in women with endometriosis: Searching for predictors of psychological distress. Hum. Reprod. 2017, 32, 1855–1861. [Google Scholar] [CrossRef] [PubMed]
- Facchin, F.; Barbara, G.; Saita, E.; Mosconi, P.; Roberto, A.; Fedele, L.; Vercellini, P. Impact of endometriosis on quality of life and mental health: Pelvic pain makes the difference. J. Psychosom. Obstet. Gynecol. 2015, 36, 135–141. [Google Scholar] [CrossRef]
- Facchin, F.; Saita, E.; Barbara, G.; Dridi, D.; Vercellini, P. “Free butterflies will come out of these deep wounds”: A grounded theory of how endometriosis affects women’s psychological health. J. Health Psychol. 2018, 23, 538–549. [Google Scholar] [CrossRef]
- Melis, I.; Litta, P.; Nappi, L.; Agus, M.; Melis, G.B.; Angioni, S. Sexual function in women with deep endometriosis: Correlation with quality of life, intensity of pain, depression, anxiety, and body image. Int. J. Sex. Health 2014, 27, 175–185. [Google Scholar] [CrossRef]
- Moradi, M.; Parker, M.; Sneddon, A.; Lopez, V.; Ellwood, D. Impact of endometriosis on women’s lives: A qualitative study. BMC Womens Health 2014, 14, 123. [Google Scholar] [CrossRef]
- Gilbert, P. Body shame: A biopsychosocial conceptualisation and overview, with treatment implications. In Body Shame Conceptualisation, Research and Treatment; Gilbert, P., Miles, J., Eds.; Brunner: London, UK, 2002; pp. 3–54. [Google Scholar]
- Tiggemann, M. Sociocultural perspectives on human appearance and body image. In Body Image: A Handbook of Science, Practice, and Prevention; Cash, T.F., Smolak, L., Eds.; Guilford: New York, NY, USA, 2011; pp. 12–19. [Google Scholar]
- Quick, V. Social theory applied to body image and chronic illness in youth. Am. J. Lifestyle Med. 2013, 8, 15–20. [Google Scholar] [CrossRef]
- Duarte, C.; Pinto-Gouveia, J.; Ferreira, C.; Batista, D. Body image as a source of shame: A new measure for the assessment of the multifaceted nature of body image shame. Clin. Psychol. Psychother. 2015, 22, 656–666. [Google Scholar] [CrossRef]
- Gilbert, P. Compassion Focused Therapy: The CBT Distinctive Features Series; Routledge: London, UK, 2010. [Google Scholar]
- Shahar, G. Erosion: The Psychopathology of Self-Criticism; Oxford University Press: New York, NY, USA, 2015. [Google Scholar]
- Gilbert, P.; McEwan, K.; Mitra, R.; Franks, L.; Richter, A.; Rockliff, H. Feeling safe and content: A specific affect regulation system? Relationship to depression, anxiety, stress, and self-criticism. J. Posit. Psychol. 2008, 3, 182–191. [Google Scholar] [CrossRef]
- Campos, R.C.; Besser, A.; Blatt, S.J. The mediating role of self-criticism and dependency in the association between perceptions of maternal caring and depressive symptoms. Depress. Anxiety 2010, 27, 1149–1157. [Google Scholar] [CrossRef]
- Joeng, J.R.; Turner, S.L. Mediators between self-criticism and depression: Fear of compassion, self-compassion, and importance to others. J. Couns. Psychol. 2015, 62, 453–463. [Google Scholar] [CrossRef]
- Morotti, M.; Vincent, K.; Becker, C.M. Mechanisms of pain in endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 209, 8–13. [Google Scholar] [CrossRef]
- Grogan, S.; Turley, E.; Cole, J. “So many women suffer in silence”: A thematic analysis of women’s written accounts of coping with endometriosis. Psychol. Health 2018, 33, 1364–1378. [Google Scholar] [CrossRef]
- Zarbo, C.; Brugnera, A.; Frigerio, L.; Malandrino, C.; Rabboni, M.; Bondi, E.; Compare, A. Behavioral, cognitive, and emotional coping strategies of women with endometriosis: A critical narrative review. Arch. Womens Ment. Health 2018, 21, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Cavaggioni, G.; Lia, C.; Resta, S.; Antonielli, T.; Benedetti Panici, P.; Megiorni, F.; Porpora, M.G. Are mood and anxiety disorders and alexithymia associated with endometriosis? A preliminary study. Biomed. Res. Int. 2014, 2014, 786830. [Google Scholar] [CrossRef] [PubMed]
- Márki, G.; Bokor, A.; Rigó, J.; Rigó, A. Physical pain and emotion regulation as the main predictive factors of health-related quality of life in women living with endometriosis. Hum. Reprod. 2017, 32, 1432–1438. [Google Scholar] [CrossRef] [PubMed]
- Teng, S.W.; Horng, H.C.; Ho, C.H.; Yen, M.S.; Chao, H.T.; Wang, P.H.; Taiwan Association of Gynecology Systematic Review Group. Women with endometriosis have higher comorbidities: Analysis of domestic data in Taiwan. J. Chin. Med. Assoc. 2016, 79, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.A.; Missmer, S.A.; Vitonis, A.F.; Sarda, V.; Laufer, M.R.; DiVasta, A.D. Prevalence of migraines in adolescents with endometriosis. Fertil. Steril. 2018, 109, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Schomacker, M.L.; Hansen, K.E.; Ramlau-Hansen, C.H.; Forman, A. Is endometriosis associated with irritable bowel syndrome? A cross-sectional study. Eur. J. Obst. Gynecol. Reprod. Biol. 2018, 231, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Shigesi, N.; Kvaskoff, M.; Kirtley, S.; Feng, Q.; Fang, H.; Knight, J.C.; Missmer, S.A.; Rahmioglu, N.; Zondervan, K.T.; Becker, C.M. The association between endometriosis and autoimmune diseases: A systematic review and meta-analysis. Hum. Reprod. Update 2019, 25, 486–503. [Google Scholar] [CrossRef] [PubMed]
- Van den Bussche, H.; Koller, D.; Kolonko, T.; Hansen, H.; Wegscheider, K.; Glaeske, G.; von Leitner, E.C.; Schäfer, I.; Schön, G. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC Public Health 2011, 11. [Google Scholar] [CrossRef]
- Read, J.R.; Sharpe, L.; Modini, M.; Dear, B.F. Multimorbidity and depression: A systematic review and meta-analysis. J. Affect. Disord. 2017, 221, 36–46. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Tylka, T.L.; Wood-Barcalow, N.L. The Body Appreciation Scale-2: Item refinement and psychometric evaluation. Body Image 2015, 12, 53–67. [Google Scholar] [CrossRef]
- Geller, S.; Handelzalts, J.E.; Levy, S.; Boxer, N.; Todd, J.; Swami, V. An examination of the factor structure and preliminary assessment of the psychometric properties of a Hebrew translation of the Body Appreciation Scale-2 (BAS-2). Body Image 2020, 34, 145–154. [Google Scholar] [CrossRef]
- Blatt, S.J.; D’Afflitti, J.P.; Quinlan, D.M. Experiences of depression in normal young adults. J. Abnorm. Psychol. 1976, 85, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Partial, conditional, and moderated moderated mediation: Quantification, inference, and interpretation. Commun. Monogr. 2018, 85, 4–40. [Google Scholar] [CrossRef]
- Laganà, A.S.; La Rosa, V.L.; Rapisarda, A.M.C.; Valenti, G.; Sapia, F.; Chiofalo, B.; Rossetti, D.; Ban Frangež, H.; Vrtačnik Bokal, E.; Vitale, S.G. Anxiety and depression in patients with endometriosis: Impact and management challenges. Int. J. Womens Health 2017, 9, 323–330. [Google Scholar] [CrossRef]
- Birk, J.L.; Kronish, M.; Moise, N.; Falzon, L.; Yoon, S.; Davidson, K.W. Depression and multimorbidity: Considering temporal characteristics of the associations between depression and multiple chronic diseases. Health Psychol. 2019, 38, 802–811. [Google Scholar] [CrossRef]
- Denny, E. “I never know from one day to another how I will feel”: Pain and uncertainty in women with endometriosis. Qual. Health Res. 2009, 19, 985–995. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak ofCOVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef]
- Leonardi, M.; Horne, A.W.; Vincent, K.; Sinclair, J.; Sherman, K.A.; Ciccia, D.; Condous, G.; Johnson, N.P.; Armour, M. Self-management strategies to consider to combat endometriosis symptoms during the COVID-19 pandemic. Hum. Reprod. Open 2020, 2020, hoaa028. [Google Scholar] [CrossRef]
- Novais, R.F.S.R.; da Câmara-França, B.E.; Lasmar, R.B.; Lasmar, B.P. Endometriosis and its relationship with depression. Int. J. Clin. Med. 2018, 9, 71–78. [Google Scholar] [CrossRef][Green Version]
- Urteaga, I.; McKillop, M.; Elhadad, N. Learning endometriosis phenotypes from patient-generated data. NPJ Digit. Med. 2020, 3. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Koyanagi, A.; Kohler-Forsberg, O.; Benros, M.E.; Munk Laursen, T.; Haro, J.M.; Nordentoft, M.; Hjorthoj, C. Mortality in unipolar depression preceding and following chronic somatic diseases. Acta Psychiatr. Scand. 2018, 138, 500–508. [Google Scholar] [CrossRef]
- Triolo, F.; Harber-Aschan, L.; Belvederi, M.M.; Calderón-Larranaga, A.; Vetrano, D.L.; Sjöberg, L.; Marengoni, A.; Dekhtyar, S. The complex interplay between depression and multimorbidity in late life: Risks and pathways: Depression and multimorbidity. Mech. Ageing Dev. 2020, 192, 111383. [Google Scholar] [CrossRef]
- Lorenzatto, C.; Vieira, M.J.N.; Marques, A.; Benetti-Pinto, C.L.; Petta, C.A. Evaluation of pain and depression in women with endometriosis after multiprofessional group intervention. Rev. Assoc. Med. Bras. 2007, 53, 433–438. [Google Scholar]
- Ferreira, C.; Dias, B.; Oliveira, S. Behind women’s body image-focused shame: Exploring the role of fears of compassion and self-criticism. Eat. Behav. 2019, 32, 12–17. [Google Scholar] [CrossRef]
- Sepulcri Rde, P.; do Amaral, V.F. Depressive symptoms, anxiety, and quality of life in women with pelvic endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2009, 142, 53–56. [Google Scholar] [CrossRef]
- Eisenberg, M.E.; Neumark-Sztainer, D.; Haines, J.; Wall, M.; Neumark-Sztainer, D.; Falkner, N.; Little, R.J.A. Weight-teasing and emotional well-being in adolescents: Longitudinal findings from Project EAT. J. Adolesc. Health 2006, 38, 675–683. [Google Scholar] [CrossRef]
- Grogan, S. Body Image: Understanding Body Dissatisfaction in Men, Women and Children; Routledge: London, UK, 2016. [Google Scholar]
- Rodin, J.; Silberstein, L.; Striegel-Moore, R. Women and weight: A normative discontent. In Psychology and Gender; Sondereregger, T.B., Ed.; University of Nebraska Press: Lincoln, OR, USA, 1985; pp. 267–307. [Google Scholar]
- Gilbert, P. The origins and nature of compassion focused therapy. Br. J. Clin. Psychol. 2014, 53, 6–41. [Google Scholar] [CrossRef]
- Lillis, J.; Hayes, S.C.; Bunting, K.; Masuda, A. Teaching acceptance and mindfulness to improve the lives of the obese: A preliminary test of a theoretical model. Ann. Behav. Med. 2009, 37, 58–69. [Google Scholar] [CrossRef]
- De Graaff, A.A.; Dirksen, C.D.; Simoens, S.; De Bie, B.; Hummelshoj, L.; D’Hooghe, T.M.; Dunselman, G.A.J. Quality of life outcomes in women with endometriosis are highly influenced by recruitment strategies. Hum. Reprod. 2015, 30, 1331–1341. [Google Scholar] [CrossRef]


| HP (n = 112) | Endometriosis (n = 73) | Endometriosis ACI (n = 62) | |||||
|---|---|---|---|---|---|---|---|
| M (SD) | Med, R | M (SD) | Med, R | M (SD) | Med, R | F(2, 244) | |
| Depression | 6.8 (5.0) a | 6.0, 0.0–24.0 | 10.9 (6.4) b | 10.0, 0.0–27.0 | 13.6 (5.9) c | 13.0, 0.0–25.0 | 30.6 ** |
| Anxiety | 5.9 (4.8) a | 4.0, 0.0–20.0 | 9.6 (6.4) b | 8.0, 0.0–21.0 | 10.9 (5.8) b | 10.0, 0.0–21.0 | 18.7 ** |
| Body image | 3.7 (0.8) a | 3.7, 1.7–5.0 | 3.6 (0.8) a | 3.7, 1.8–5.0 | 3.2 (0.9) b | 3.2, 1.4–5.0 | 7.1 ** |
| Self-criticism | 4.1 (0.8) a | 4.0, 2.5–6.0 | 4.2 (0.9) a | 4.1, 2.6–6.2 | 4.5 (0.9) b | 4.5, 2.2–6.7 | 4.1 * |
| Self-Criticism | Depression | Anxiety | M (SD) | |
|---|---|---|---|---|
| Body image | −0.54 | −0.51 | −0.39 | 3.5 (0.8) |
| Self-criticism | 0.58 | 0.55 | 4.2 (0.9) | |
| Depression | 0.77 | 9.7 (6.3) | ||
| Anxiety | 8.3 (6.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geller, S.; Levy, S.; Ashkeloni, S.; Roeh, B.; Sbiet, E.; Avitsur, R. Predictors of Psychological Distress in Women with Endometriosis: The Role of Multimorbidity, Body Image, and Self-Criticism. Int. J. Environ. Res. Public Health 2021, 18, 3453. https://doi.org/10.3390/ijerph18073453
Geller S, Levy S, Ashkeloni S, Roeh B, Sbiet E, Avitsur R. Predictors of Psychological Distress in Women with Endometriosis: The Role of Multimorbidity, Body Image, and Self-Criticism. International Journal of Environmental Research and Public Health. 2021; 18(7):3453. https://doi.org/10.3390/ijerph18073453
Chicago/Turabian StyleGeller, Shulamit, Sigal Levy, Sapir Ashkeloni, Bar Roeh, Ensherah Sbiet, and Ronit Avitsur. 2021. "Predictors of Psychological Distress in Women with Endometriosis: The Role of Multimorbidity, Body Image, and Self-Criticism" International Journal of Environmental Research and Public Health 18, no. 7: 3453. https://doi.org/10.3390/ijerph18073453
APA StyleGeller, S., Levy, S., Ashkeloni, S., Roeh, B., Sbiet, E., & Avitsur, R. (2021). Predictors of Psychological Distress in Women with Endometriosis: The Role of Multimorbidity, Body Image, and Self-Criticism. International Journal of Environmental Research and Public Health, 18(7), 3453. https://doi.org/10.3390/ijerph18073453








