Can Working Conditions and Employees’ Mental Health Be Improved via Job Stress Interventions Designed and Implemented by Line Managers and Human Resources on an Operational Level?
Abstract
1. Introduction
Aim
2. Materials and Methods
2.1. Setting and Intervention Design
2.2. Effect Evaluation
2.2.1. Survey Data on Working Conditions, Motivation, and Health
2.2.2. Register Data on Employee Turnover and Sickness Absence
2.3. Analytical Strategy
2.4. Ethics Approval and Consent to Participate
3. Results
3.1. Overall Intervention Effects on Working Conditions, Motivation, and Health
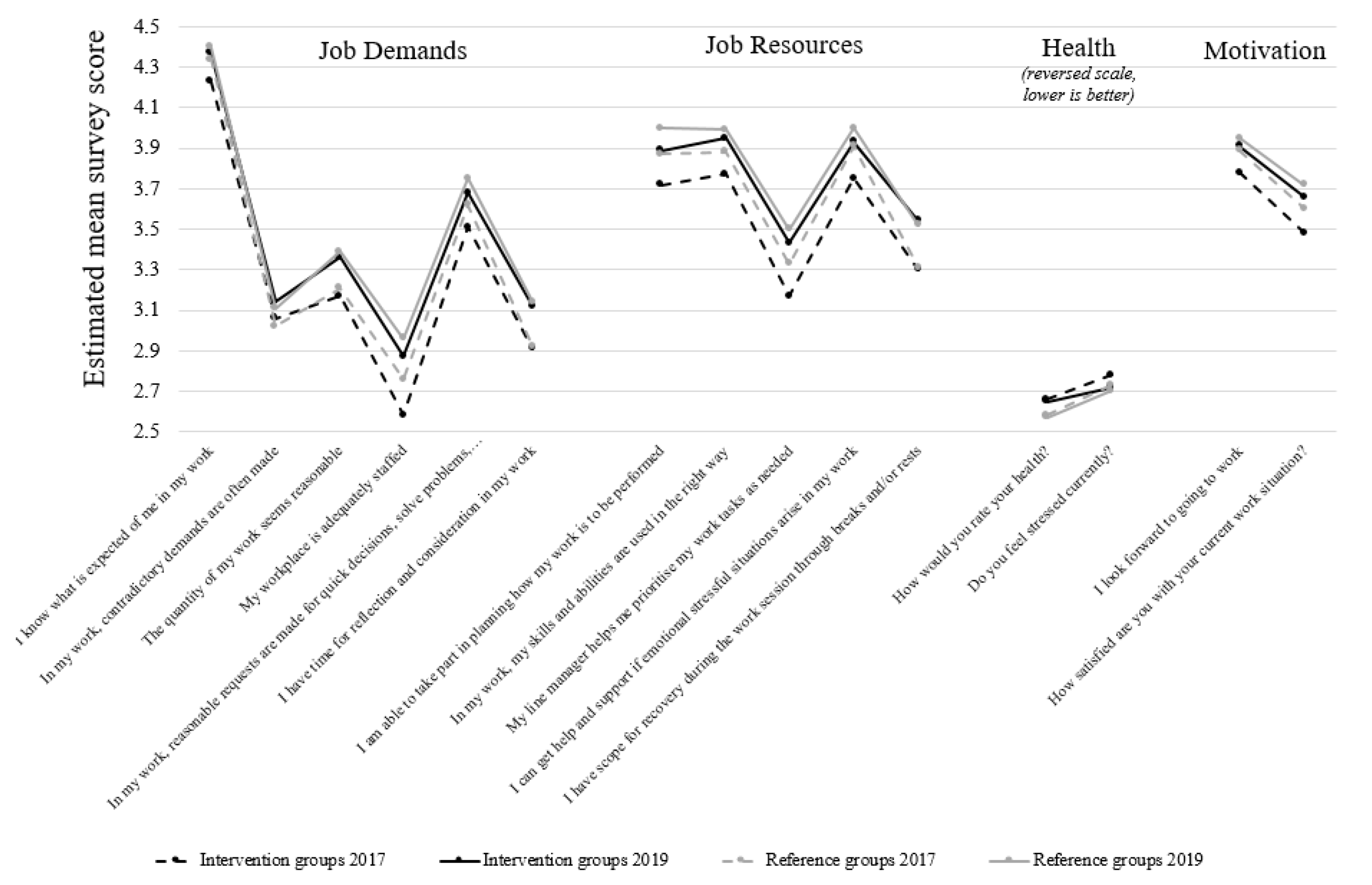
3.2. Differences in Working Conditions, Motivation, and Health Between Intervention Groups and Reference Groups, and Their Development over Time
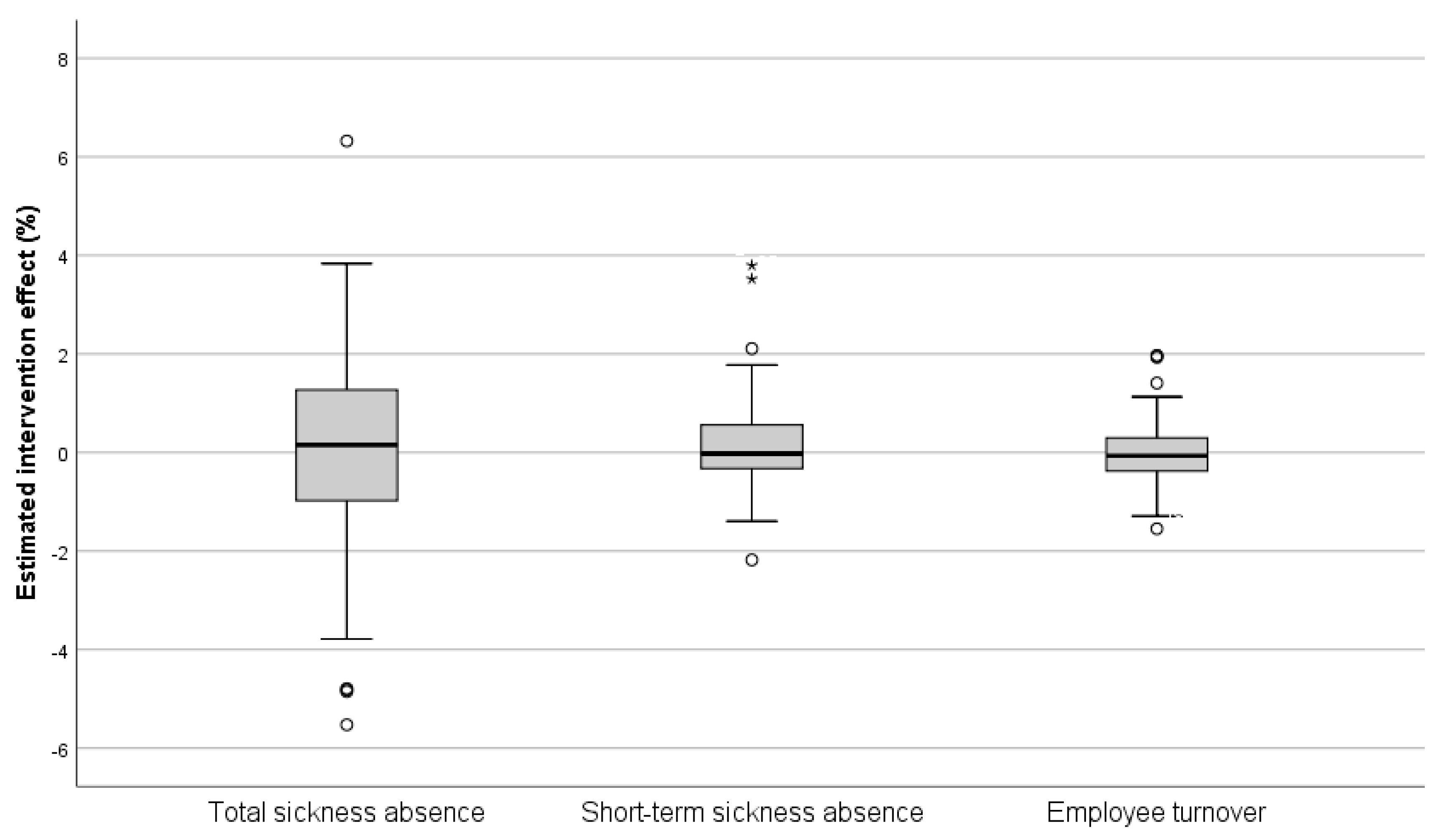
3.3. Overall Intervention Effects on Employee Turnover and Sickness Absence
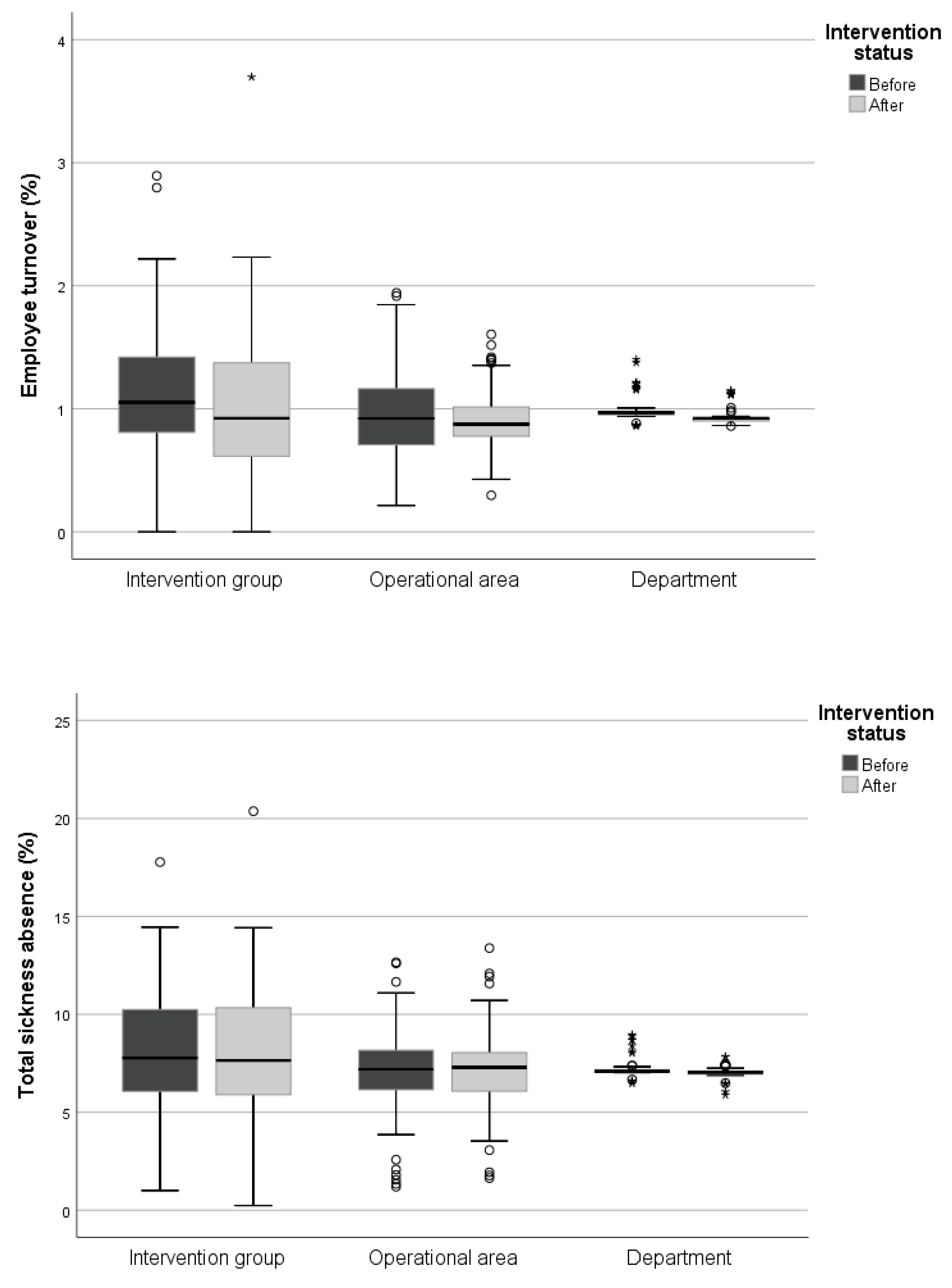
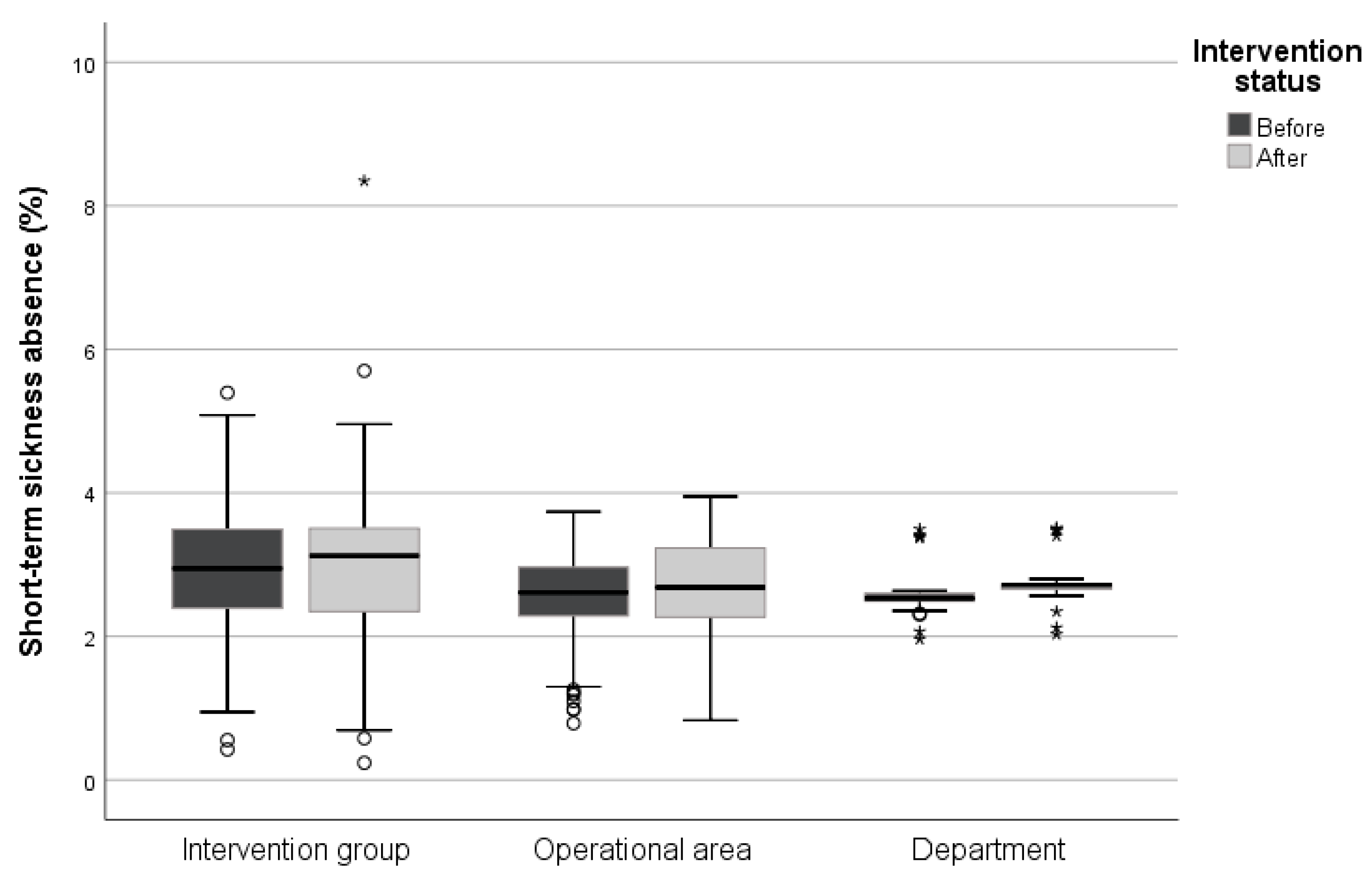
3.4. Workplace-Specific Intervention Effects on Sickness Absence and Employee Turnover
4. Discussion
4.1. Overall Intervention Effects
4.2. Factors Affecting the Intervention Effect
4.3. Methodological Considerations on Implementing and Evaluating Operational-Level Interventions
4.4. Strengths and Limitations
5. Conclusions and Practical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hannan, E.; Breslin, N.; Doherty, E.; McGreal, M.; Moneley, D.; Offiah, G. Burnout and stress amongst interns in Irish hospitals: Contributing factors and potential solutions. Ir. J. Med. Sci. 2018, 187, 301–307. [Google Scholar] [CrossRef]
- Qiao, Z.; Chen, L.; Chen, M.; Guan, X.; Wang, L.; Jiao, Y.; Yang, J.; Tang, Q.; Yang, X.; Qiu, X.; et al. Prevalence and factors associated with occupational burnout among HIV/AIDS healthcare workers in China: A cross-sectional study. BMC Public Health 2016, 16, 335. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Boone, S.; Tan, L.; Dyrbye, L.N.; Sotile, W.; Satele, D.; West, C.P.; Sloan, J.; Oreskovich, M.R. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch. Intern. Med. 2012, 172, 1377–1385. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Hasan, O.; Dyrbye, L.N.; Sinsky, C.; Satele, D.; Sloan, J.; West, C.P. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin. Proc. 2015, 90, 1600–1613. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Shi, L.; Gao, L.; Liu, W.; Chen, Z.; Tong, X.; Xu, W.; Peng, B.; Zhao, Y.; Fan, L. Determinate factors of mental health status in Chinese medical staff: A cross-sectional study. Medicine 2018, 97, e0113–e01139. [Google Scholar] [CrossRef]
- SSIA. Sjukfrånvaron På Svensk Arbetsmarknad [Sick Leave on the Swedish Labour Market]; Special Survivor Indemnity Allowance (SSIA): Stockholm, Sweden, 2018. [Google Scholar]
- Statistics Sweden. Trender och Prognoser 2017: Befolkningen, Utbildningen, Arbetsmarknaden Med Sikte På 2035 [Trends and forecasts 2017: Population, Education and the Labour Market in Sweden—Outlook to the Year 2035]; Statistics Sweden: Stockholm, Sweden, 2017.
- Aronsson, G.; Theorell, T.; Grape, T.; Hammarström, A.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Träskman-Bendz, L.; Hall, C. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health 2017, 17, 264. [Google Scholar] [CrossRef]
- de Vries, H.; Fishta, A.; Weikert, B.; Rodriguez Sanchez, A.; Wegewitz, U. Determinants of sickness absence and return to work among employees with common mental disorders: A scoping review. J. Occup. Rehabil. 2018, 28, 393–417. [Google Scholar] [CrossRef]
- Harvey, S.B.; Modini, M.; Joyce, S.; Milligan-Saville, J.S.; Tan, L.; Mykletun, A.; Bryant, R.A.; Christensen, H.; Mitchell, P.B. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup. Environ. Med. 2017, 74, 301–310. [Google Scholar] [CrossRef]
- Stansfeld, S.; Candy, B. Psychosocial work environment and mental health—A meta-analytic review. Scand. J. Work Environ. Health 2006, 32, 443–462. [Google Scholar] [CrossRef] [PubMed]
- Karanika-Murray, M.; Biron, C.; Saksvik, P.Ø. Organizational health interventions: Advances in evaluation methodology. Stress Health 2016, 32, 255–257. [Google Scholar] [CrossRef]
- Nielsen, K.; Randall, R.; Holten, A.-L.; González, E.R. Conducting organizational-level occupational health interventions: What works? Work Stress 2010, 24, 234–259. [Google Scholar] [CrossRef]
- Cox, T.; Karanika, M.; Griffiths, A.; Houdmont, J. Evaluating organizational-level work stress interventions: Beyond traditional methods. Work Stress 2007, 21, 348–362. [Google Scholar] [CrossRef]
- Giga, S.I.; Noblet, A.J.; Faragher, B.; Cooper, C.L. The UK perspective: A review of research on organisational stress management interventions. Aust. Psychol. 2003, 38, 158–164. [Google Scholar] [CrossRef]
- Kompier, M.A.J.; Kristensen, T.S. Organizational Work Stress Interventions in a Theoretical, Methodological and Practical Context. In Stress in the Workplace: Past, Present and Future; Dunham, J., Ed.; Whurr Publishers: London, UK, 2001. [Google Scholar]
- Nielsen, K.; Randall, R. Opening the black box: Presenting a model for evaluating organizational-level interventions. Eur. J. Work Organ. Psychol. 2013, 22, 601–617. [Google Scholar] [CrossRef]
- Hasson, D. Stress Management Interventions and Predictors of Long-Term Health: Prospectively Controlled Studies on Long-Term Pain Patients and a Healthy Sample from it- and Media Companies; Uppsala University: Uppsala, Sweden, 2005. [Google Scholar]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: A realist review. Int. J. Environ. Res. Public Health 2019, 16, 4396. [Google Scholar] [CrossRef] [PubMed]
- Montano, D.; Hoven, H.; Siegrist, J. Effects of organisational-level interventions at work on employees’ health: A systematic review. BMC Public Health 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- Ruotsalainen, J.H.; Verbeek, J.H.; Mariné, A.; Serra, C. Preventing occupational stress in healthcare workers. Cochrane Database Syst. Rev. 2014, 11, CD002892. [Google Scholar] [CrossRef]
- Semmer, N.K. Job stress interventions and the organization of work. Scand. J. Work Environ. Health 2006, 32, 515–527. [Google Scholar] [CrossRef]
- Egan, M.; Bambra, C.; Thomas, S.; Petticrew, M.; Whitehead, M.; Thomson, H. The psychosocial and health effects of workplace reorganisation. 1. A systematic review of organisational-level interventions that aim to increase employee control. J. Epidemiol. Community Health 2007, 61, 945–954. [Google Scholar] [CrossRef]
- Kristensen, T.S. Intervention studies in occupational epidemiology. Occup. Environ. Med. 2005, 62, 205–210. [Google Scholar] [CrossRef]
- Karasek, R.; Theorell, T. Healthy Work: Stress, Productivity and the Reconstruction of Working Life; Basic Books: New York, NY, USA, 1990. [Google Scholar]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Barling, J. Handbook of Work Stress; Barling, J., Kelloway, E.K., Frone, M.R., Eds.; Sage: Thousand Oaks, CA, USA, 2005. [Google Scholar]
- Bakker, A.B.; Demerouti, E.; de Boer, E.; Schaufeli, W.B. Job demands and job resources as predictors of absence duration and frequency. J. Vocat. Behav. 2003, 62, 341–356. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. The job demands—Resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. The job demands—Resources model of burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef] [PubMed]
- Hakanen, J.J.; Schaufeli, W.B.; Ahola, K. The job demands—Resources model: A three-year cross-lagged study of burnout, depression, commitment, and work engagement. Work Stress 2008, 22, 224–241. [Google Scholar] [CrossRef]
- Bakker, A.B.; van Veldhoven, M.; Xanthopoulou, D. Beyond the demand—Control model: Thriving on high job demands and resources. J. Pers. Psychol. 2010, 9, 3–16. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Bakker, A.B.; Schaufeli, W.B. Burnout and work engagement among teachers. J. Sch. Psychol. 2006, 43, 495–513. [Google Scholar] [CrossRef]
- van den Broeck, A.; Vansteenkiste, M.; de Witte, H.; Lens, W. Explaining the relationships between job characteristics, burnout, and engagement: The role of basic psychological need satisfaction. Work Stress 2008, 22, 277–294. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B. Job demands, job resources, and their relationship with burnout and engagement: A multi-sample study. J. Organ. Behav. 2004, 25, 293–315. [Google Scholar] [CrossRef]
- Arapovic-Johansson, B.; Jensen, I.; Wåhlin, C.; Björklund, C.; Kwak, L. Process evaluation of a participative organizational intervention as a stress preventive intervention for employees in Swedish primary health care. Int. J. Environ. Res. Public Health 2020, 17, 7285. [Google Scholar] [CrossRef] [PubMed]
- Di Tecco, C.; Nielsen, K.; Ghelli, M.; Ronchetti, M.; Marzocchi, I.; Persechino, B.; Iavicoli, S. Improving working conditions and job satisfaction in healthcare: A study concept design on a participatory organizational level intervention in psychosocial risks management. Int. J. Environ. Res. Public Health 2020, 17, 3677. [Google Scholar] [CrossRef]
- Härenstam, A.; Pousette, A.; Berntson, E. Improving organizational and working conditions for managers in the Swedish public sector: A conceptual model and evaluation of interventions. Econ. Ind. Democr. 2019. [Google Scholar] [CrossRef]
- Severin, J.; Björk, L.; Corin, L.; Jonsdottir, I.H.; Akerstrom, M. Process evaluation of an operational-level job stress intervention aimed at decreasing sickness absence among public sector employees in Sweden. Int. J. Environ. Res. Public Health 2021, 18, 1778. [Google Scholar] [CrossRef]
- Corbière, M.; Shen, J.; Rouleau, M.; Dewa, C.S. A systematic review of preventive interventions regarding mental health issues in organizations. Work 2009, 33, 81–116. [Google Scholar] [CrossRef] [PubMed]
- Johns, G. The essential impact of context on organizational behavior. Acad. Manage. Rev. 2006, 31, 386–408. [Google Scholar] [CrossRef]
- Lamontagne, A.D.; Keegel, T.; Louie, A.M.; Ostry, A.; Landsbergis, P.A. A systematic review of the job-stress intervention evaluation literature, 1990–2005. Int. J. Occup. Environ. Health 2007, 13, 268–280. [Google Scholar] [CrossRef] [PubMed]
- Grant, A.M.; Wall, T.D. The neglected science and art of quasi-experimentation: Why-to, when-to, and how-to advice for organizational researchers. Organ. Res. Methods 2009, 12, 653–686. [Google Scholar] [CrossRef]
- Mills, M.; van de Bunt, G.G.; de Bruijn, J. Comparative research: Persistent problems and promising solutions. Int. Sociol. 2006, 21, 619–631. [Google Scholar] [CrossRef]
- Box, G.E.P.; Jenkins, G.M. Time Series Analysis: Forecasting and Control; Holden-Day: San Francisco, CA, USA, 1976. [Google Scholar]
- Tabaschnick, B.; Fidell, L. Using Multivariate Statistics, 6th ed.; Pearson Education: Boston, MA, USA, 2013. [Google Scholar]
- Greasley, K.; Edwards, P. When do health and well-being interventions work? Managerial commitment and context. Econ. Ind. Democr. 2015, 36, 355–377. [Google Scholar] [CrossRef]
- Bhui, K.S.; Dinos, S.; Stansfeld, S.A.; White, P.D. A synthesis of the evidence for managing stress at work: A review of the reviews reporting on anxiety, depression, and absenteeism. J. Environ. Public Health 2012, 2012, 515874. [Google Scholar] [CrossRef]
- Augustsson, H.; von Thiele Schwarz, U.; Stenfors-Hayes, T.; Hasson, H. Investigating variations in implementation fidelity of an organizational-level occupational health intervention. Int. J. Behav. Med. 2015, 22, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Fagerlind Ståhl, A.-C.; Ståhl, C.; Smith, P. Longitudinal association between psychological demands and burnout for employees experiencing a high versus a low degree of job resources. BMC Public Health 2018, 18, 915. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, B. Between endless needs and limited resources: The gendered construction of a greedy organization. Gend. Work Organ. 2004, 11, 506–525. [Google Scholar] [CrossRef]
- Cerdas, S.; Härenstam, A.; Johansson, G.; Nyberg, A. Development of job demands, decision authority and social support in industries with different gender composition—Sweden, 1991–2013. BMC Public Health 2019, 19, 758. [Google Scholar] [CrossRef]
- Munch-Hansen, T.; Wieclaw, J.; Agerbo, E.; Westergaard-Nielsen, N.; Rosenkilde, M.; Bonde, J.P. Sickness absence and workplace levels of satisfaction with psychosocial work conditions at public service workplaces. Am. J. Ind. Med. 2009, 52, 153–161. [Google Scholar] [CrossRef]
- Pritchard, R.D.; Harrell, M.M.; DiazGranados, D.; Guzman, M.J. The productivity measurement and enhancement system: A meta-analysis. J. Appl. Psychol. 2008, 93, 540–567. [Google Scholar] [CrossRef]
- Nielsen, K.; Miraglia, M. What works for whom in which circumstances? On the need to move beyond the ‘what works?’ question in organizational intervention research. Hum. Relat. 2017, 70, 40–62. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E.; Sanz-Vergel, A.I. Burnout and work engagement: The JD—R approach. Annu. Rev. Organ. Psychol. Organ. Behav. 2014, 1, 389–411. [Google Scholar] [CrossRef]
- Ipsen, C.; Gish, L.; Poulsen, S. Organizational-level interventions in small and medium-sized enterprises: Enabling and inhibiting factors in the PoWRS program. Saf. Sci. 2015, 71, 264–274. [Google Scholar] [CrossRef]
- LaMontagne, A.D.; Noblet, A.J.; Landsbergis, P.A. Intervention Development and Implementation: Understanding and Addressing Barriers to Organizational-Level Interventions. In Improving Organizational Interventions for Stress and Well-Being: Addressing Process and Context; Biron, C., Karanika-Murray, M., Cooper, C., Eds.; Routledge/Taylor & Francis Group: New York, NY, USA, 2012; pp. 21–38. [Google Scholar]
- Mellor, N.; Smith, P.; Mackay, C.; Palferman, D. The “management standards” for stress in large organizations. Int. J. Workplace Health Manag. 2013, 6, 4–17. [Google Scholar] [CrossRef]
- Dellve, L.; Skagert, K.; Eklöf, M. The impact of systematic occupational health and safety management for occupational disorders and long-term work attendance. Soc. Sci. Med. 2008, 67, 965–970. [Google Scholar] [CrossRef]
- von Thiele Schwarz, U.; Hasson, H.; Lindfors, P. Applying a fidelity framework to understand adaptations in an occupational health intervention. Work 2015, 51, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Evans, R.E. What theory, for whom and in which context? Reflections on the application of theory in the development and evaluation of complex population health interventions. SSM Popul. Health 2017, 3, 132–135. [Google Scholar] [CrossRef] [PubMed]
- Rimer, B.K.; Kreuter, M.W. Advancing tailored health communication: A persuasion and message effects perspective. J. Commun. 2006, 56, S184–S201. [Google Scholar] [CrossRef]
- Andreasson, J.; Eriksson, A.; Dellve, L. Health care managers’ views on and approaches to implementing models for improving care processes. J. Nurs. Manag. 2016, 24, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Wikström, E.; Dellenborg, L.; Wallin, L.; Gillespie, B.M.; Erichsen Andersson, A. The safe hands study: Implementing aseptic techniques in the operating room: Facilitating mechanisms for contextual negotiation and collective action. Am. J. Infect. Control 2019, 47, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Eklöf, M. Psykosocial Arbetsmiljö: Begrepp, Bedömning och Utveckling; Studentlitteratur: Lund, Sweden, 2017. [Google Scholar]
- van Rhenen, W.; Blonk, R.W.B.; Schaufeli, W.B.; van Dijk, F.J.H. Can sickness absence be reduced by stress reduction programs: On the effectiveness of two approaches. Int. Arch. Occup. Environ. Health 2007, 80, 505–515. [Google Scholar] [CrossRef]
- Saastamoinen, P.; Laaksonen, M.; Lahelma, E.; Lallukka, T.; Pietiläinen, O.; Rahkonen, O. Changes in working conditions and subsequent sickness absence. Scand. J. Work Environ. Health 2014, 40, 82–88. [Google Scholar] [CrossRef]
- Christensen, K.B.; Nielsen, M.L.; Rugulies, R.; Smith-Hansen, L.; Kristensen, T.S. Workplace levels of psychosocial factors as prospective predictors of registered sickness absence. J. Occup. Environ. Med. 2005, 47, 933–940. [Google Scholar] [CrossRef]

| Effect Measures | Intervention Group | Operational Area a | Department a | |||
|---|---|---|---|---|---|---|
| β (95% CI) | p-Value | β (95% CI) | p-Value | β (95% CI) | p-Value | |
| Sickness absence (%) | −0.43 (−1.0–0.14) | 0.14 | −0.29 (−0.56–−0.015) | 0.04 | −0.17 (−0.26–−0.077) | <0.001 |
| Sickness absence ≤14 days (%) | −0.20 (−0.39–−0.007) | 0.04 | −0.13 (−0.23–−0.023) | 0.02 | −0.084 (−0.12–−0.046) | <0.001 |
| Employee turnover (%) | 0.071 (−0.18–0.32) | 0.58 | 0.050 (−0.079–0.18) | 0.45 | 0.030 (0.012–0.049) | 0.001 |
| Intervention Effects | Total Sickness Absence | Short-Term Sickness Absence | Employee Turnover | |||
|---|---|---|---|---|---|---|
| Total | Adjusted for Reference Groups | Total | Adjusted for Reference Groups | Total | Adjusted for Reference Groups | |
| Positive intervention effect (n) | 8 | 8 | 4 | 4 | 3 | 3 |
| Negative intervention effect (n) | 11 | 9 | 6 | 6 | 3 | 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akerstrom, M.; Corin, L.; Severin, J.; Jonsdottir, I.H.; Björk, L. Can Working Conditions and Employees’ Mental Health Be Improved via Job Stress Interventions Designed and Implemented by Line Managers and Human Resources on an Operational Level? Int. J. Environ. Res. Public Health 2021, 18, 1916. https://doi.org/10.3390/ijerph18041916
Akerstrom M, Corin L, Severin J, Jonsdottir IH, Björk L. Can Working Conditions and Employees’ Mental Health Be Improved via Job Stress Interventions Designed and Implemented by Line Managers and Human Resources on an Operational Level? International Journal of Environmental Research and Public Health. 2021; 18(4):1916. https://doi.org/10.3390/ijerph18041916
Chicago/Turabian StyleAkerstrom, Magnus, Linda Corin, Jonathan Severin, Ingibjörg H. Jonsdottir, and Lisa Björk. 2021. "Can Working Conditions and Employees’ Mental Health Be Improved via Job Stress Interventions Designed and Implemented by Line Managers and Human Resources on an Operational Level?" International Journal of Environmental Research and Public Health 18, no. 4: 1916. https://doi.org/10.3390/ijerph18041916
APA StyleAkerstrom, M., Corin, L., Severin, J., Jonsdottir, I. H., & Björk, L. (2021). Can Working Conditions and Employees’ Mental Health Be Improved via Job Stress Interventions Designed and Implemented by Line Managers and Human Resources on an Operational Level? International Journal of Environmental Research and Public Health, 18(4), 1916. https://doi.org/10.3390/ijerph18041916







