Process Evaluation of an Operational-Level Job Stress Intervention Aimed at Decreasing Sickness Absence among Public Sector Employees in Sweden
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Background
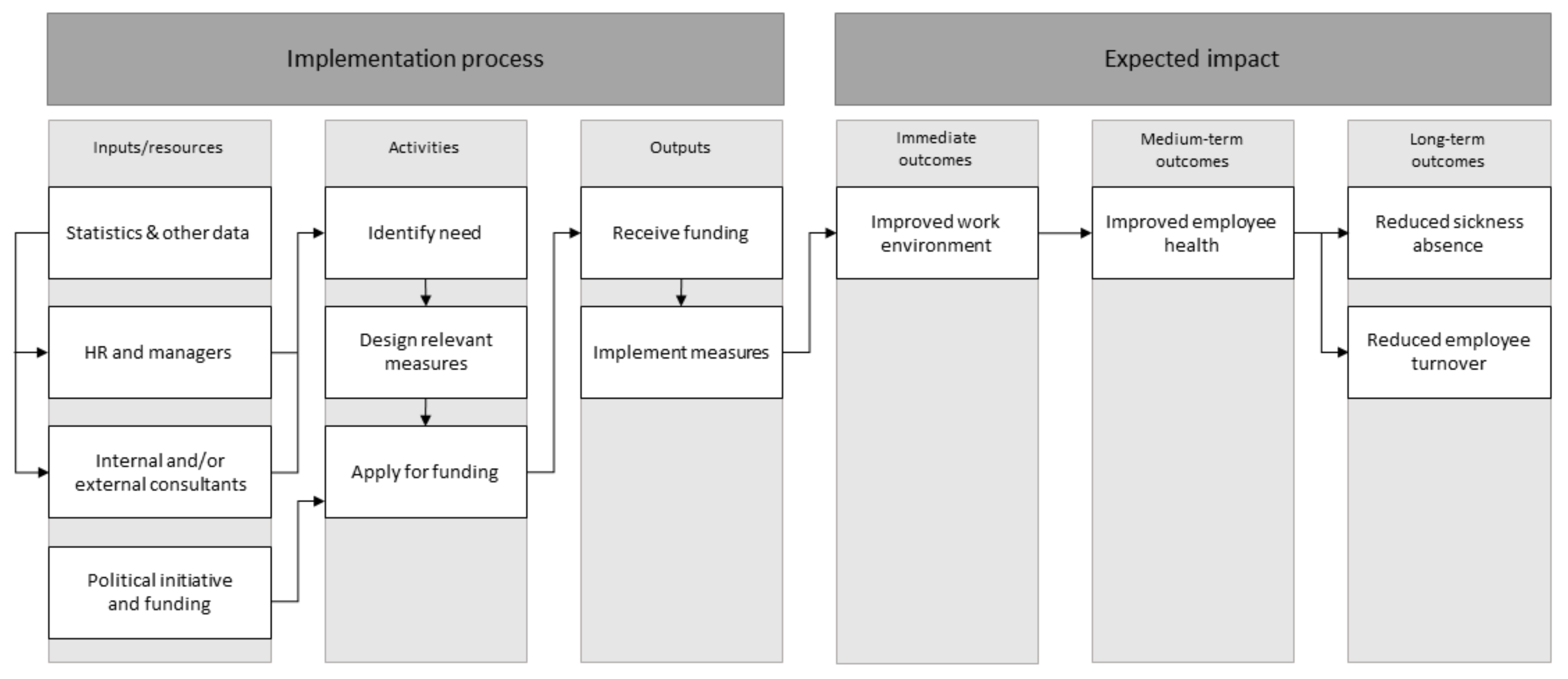
2.2. The Intervention
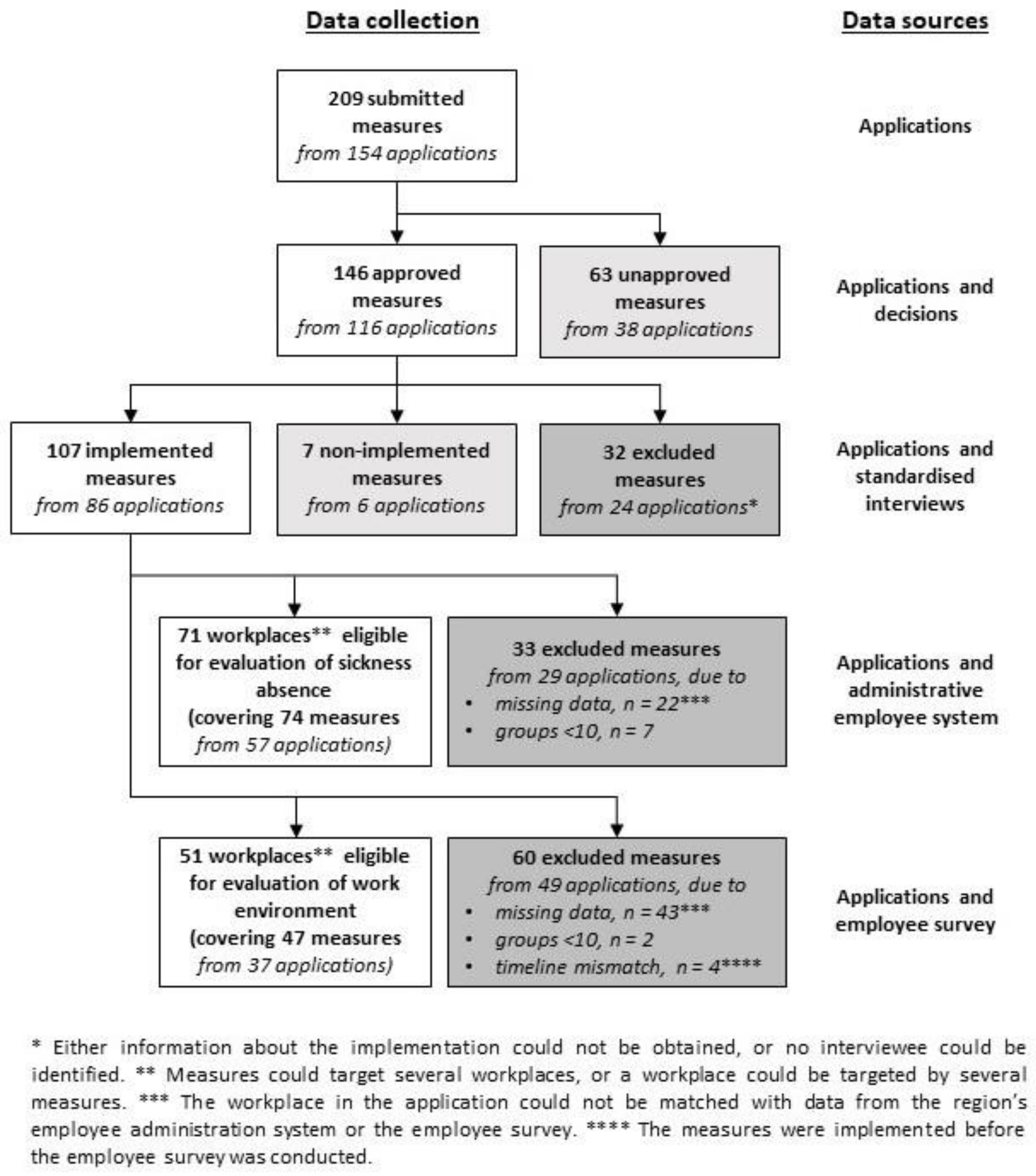
2.3. Data Sources and Data Collection
2.4. Data Analysis
3. Results
3.1. Comparison of Sickness Absence before the Intervention between the Intended Target Groups and Their Reference Groups
3.2. Comparison of Work Environment before the Intervention between the Intended Target Groups and Their Reference Groups
3.3. Description of the Work Environmental Challenges in the Applications
3.4. Description of Suggested Measures in the Applications
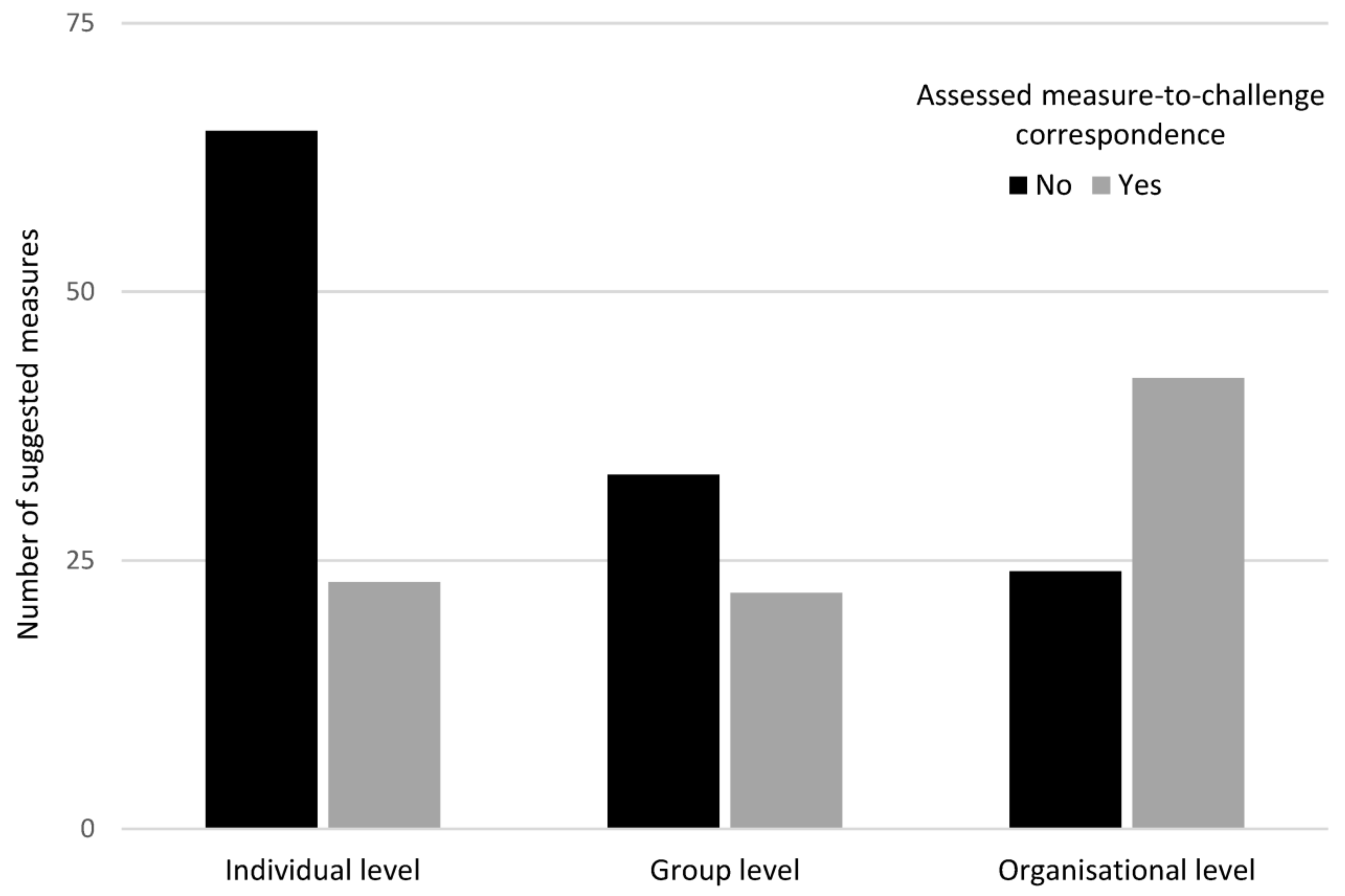
3.5. Motivation for Selecting Different Measures and Measure-To-Challenge Correspondence
3.6. Did Implemented Measures Differ from Non-Implemented Measures?
4. Discussion
4.1. Did the Intervention Reach the Target Group?
4.2. Did the Suggested Measures Correspond to the Work Environmental Challenges?
4.3. Were the Planned Measures Implemented?
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hassard, J.; Teoh, K.; Cox, T.; Cosmar, M.; Gründler, R.; Flemming, D.; Cosemans, B.; Van den Broek, K. Calculating the Cost of Work-Related Stress and Psychosocial Risks; European Agency for Safety and Health at Work: Bilbao, Spain, 2014. [Google Scholar]
- Skandia. Samhällsförlusten av Sjukskrivningar: 64 Miljarder Kronor; Livförsäkringsbolaget Skandia: Stockholm, Sweden, 2019. [Google Scholar]
- Försäkringskassan. Sjukfrånvaro i Psykiatriska Diagnoser—En Registerstudie av Sveriges Arbetande Befolkning i Åldern 20–69 år (Socialförsäkringsrapport 2020:8); Försäkringskassan: Stockholm, Sweden, 2020. [Google Scholar]
- Aronsson, G.; Theorell, T.; Grape, T.; Hammarström, A.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Träskman-Bendz, L.; Hall, C. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health 2017, 17, 264:1–264:13. [Google Scholar] [CrossRef] [PubMed]
- De Vries, H.; Fishta, A.; Weikert, B.; Sanchez, A.R.; Wegewitz, U. Determinants of sickness absence and return to work among employees with common mental disorders: A scoping review. J. Occup. Rehabil. 2018, 28, 393–417. [Google Scholar] [CrossRef]
- Stansfeld, S.; Candy, B. Psychosocial work environment and mental health—a meta-analytic review. Scand. J. Work Environ. Health 2006, 32, 443–462. [Google Scholar] [CrossRef]
- Nappo, N. Interpersonal Relationships on and outside of the Job and Satisfaction with Working Conditions in Europe. Int. J. Bus. Soc. Sci. 2019, 10, 14–25. [Google Scholar] [CrossRef]
- Nappo, N. Job stress and interpersonal relationships cross country evidence from the EU15: A correlation analysis. BMC Public Health 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Bonde, J.P.E. Psychosocial factors at work and risk of depression: A systematic review of the epidemiological evidence. Occup. Environ. Med. 2008, 65, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Giga, S.I.; Noblet, A.J.; Faragher, B.; Cooper, C.L. The UK perspective: A review of research on organisational stress management interventions. Aust. Psychol. 2003, 38, 158–164. [Google Scholar] [CrossRef]
- Kivimäki, M.; Head, J.; Ferrie, J.E.; Brunner, E.; Marmot, M.G.; Vahtera, J.; Shipley, M.J. Why is evidence on job strain and coronary heart disease mixed? An illustration of measurement challenges in the Whitehall II study. Psychosom. Med. 2006, 68, 398–401. [Google Scholar] [CrossRef]
- Kuper, H.; Marmot, M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J. Epidemiol. Community Health 2003, 57, 147–153. [Google Scholar] [CrossRef]
- Sauter, S.L.; Murphy, L.R. Work organization interventions: State of knowledge and future directions. Soz. Praventivmed. 2004, 49, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Waddell, G.; Burton, A.K. Is Work Good for Your Health and Well-Being? The Stationery Office: London, UK, 2006. [Google Scholar]
- Swedish Work Environment Authority. The Work Environment Act. Available online: https://www.av.se/en/work-environment-work-and-inspections/acts-and-regulations-about-work-environment/the-work-environment-act/ (accessed on 7 December 2020).
- Swedish Work Environment Authority. Organisational and Social Work Environment. Available online: http://www.av.se/en/work-environment-work-and-inspections/publications/foreskrifter/organisatorisk-och-social-arbetsmiljo-afs-20154-foreskrifter/ (accessed on 7 December 2020).
- Corin, L. Job Demands, Job Resources, and Consequences for Managerial Sustainability in the Public Sector–A Contextual Approach. Ph.D. Thesis, University of Gothenburg, Gothenburg, Sweden, 2016. [Google Scholar]
- Dollard, M.; Dormann, C.; Idris, M. Psychosocial Safety Climate—A New Work Stress Theory; Springer International Publishing AG: Cham, Switzerland, 2019. [Google Scholar]
- Bauer, G.; Davies, J.K.; Pelikan, J.; on behalf of the Euhpid Theory Working Group and the Euhpid Consortium. The EUHPID Health Development Model for the classification of public health indicators. Health Promot. Int. 2006, 21, 153–159. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Institute for Future Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Glanz, K.; Rimer, B.K. Theory at a Glance: A Guide for Health Promotion Practice; National Institutes of Health: Washington, DC, USA, 1997. [Google Scholar]
- Richardson, K.M.; Rothstein, H.R. Effects of occupational stress management intervention programs: A meta-analysis. J. Occup. Health Psychol. 2008, 13, 69–93. [Google Scholar] [CrossRef]
- Nielsen, K.; Randall, R. Opening the black box: Presenting a model for evaluating organizational-level interventions. Eur. J. Work Organ. Psychol. 2013, 22, 601–617. [Google Scholar] [CrossRef]
- Antonovsky, A. The salutogenic model as a theory to guide health promotion. Health Promot. Int. 1996, 11, 11–18. [Google Scholar] [CrossRef]
- Epp, J. Achieving health for all: A framework for health promotion. Health Promot. Int. 1986, 1, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Ivancevich, J.M.; Matteson, M.T.; Freedman, S.M.; Phillips, J.S. Worksite stress management interventions. Am. Psychol. 1990, 45, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Murphy, L.R. Managing job stress: An employee assistance/human resource management partnership. Pers. Rev. 1995, 24, 41–50. [Google Scholar] [CrossRef]
- Corbière, M.; Shen, J.; Rouleau, M.; Dewa, C.S. A systematic review of preventive interventions regarding mental health issues in organizations. Work 2009, 33, 81–116. [Google Scholar] [CrossRef]
- Wu, S.; Li, J.; Wang, M.; Wang, Z.; Li, H. Intervention on occupational stress among teachers in the middle schools in China. Stress Health 2006, 22, 329–336. [Google Scholar] [CrossRef]
- Cox, T.; Karanika, M.; Griffiths, A.; Houdmont, J. Evaluating organizational-level work stress interventions: Beyond traditional methods. Work Stress 2007, 21, 348–362. [Google Scholar] [CrossRef]
- Kompier, M.A.; Cooper, C.L.; Geurts, S.A. A multiple case study approach to work stress prevention in Europe. Eur. J. Work Organ. Psychol. 2000, 9, 371–400. [Google Scholar] [CrossRef]
- Nielsen, K.; Randall, R.; Holten, A.-L.; González, E.R. Conducting organizational-level occupational health interventions: What works? Work Stress 2010, 24, 234–259. [Google Scholar] [CrossRef]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Van Rhenen, W.; Blonk, R.W.; Schaufeli, W.B.; van Dijk, F.J. Can sickness absence be reduced by stress reduction programs: On the effectiveness of two approaches. Int. Arch Occup. Environ. Health 2007, 80, 505–515. [Google Scholar] [CrossRef]
- Grimani, A.; Bergström, G.; Casallas, M.I.R.; Aboagye, E.; Jensen, I.; Lohela-Karlsson, M. Economic evaluation of occupational safety and health interventions from the employer perspective: A systematic review. J. Occup. Environ. Med. 2018, 60, 147–166. [Google Scholar] [CrossRef]
- Tompa, E.; Dolinschi, R.; De Oliveira, C.; Amick, B.C.; Irvin, E. A systematic review of workplace ergonomic interventions with economic analyses. J. Occup. Rehabil. 2010, 20, 220–234. [Google Scholar] [CrossRef]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: A realist review. Int. J. Environ. Res. Public Health 2019, 16, 4396. [Google Scholar] [CrossRef] [PubMed]
- Montano, D.; Hoven, H.; Siegrist, J. Effects of organisational-level interventions at work on employees’ health: A systematic review. BMC Public Health 2014, 14, 135. [Google Scholar] [CrossRef]
- Ruotsalainen, J.H.; Verbeek, J.H.; Mariné, A.; Serra, C. Preventing occupational stress in healthcare workers. Cochrane Database Syst. Rev. 2015, 2015, CD002892:1–CD002892:127. [Google Scholar] [CrossRef] [PubMed]
- Semmer, N.K. Job stress interventions and the organization of work. Scand. J. Work Environ. Health 2006, 32, 515–527. [Google Scholar] [CrossRef]
- Greasley, K.; Edwards, P. When do health and well-being interventions work? Managerial commitment and context. Econ. Ind. Democr. 2015, 36, 355–377. [Google Scholar] [CrossRef]
- Härenstam, A.; Pousette, A.; Berntson, E. Improving organizational and working conditions for managers in the Swedish public sector: A conceptual model and evaluation of interventions. Econ. Ind. Democr. 2019, 10, 1–26. [Google Scholar] [CrossRef]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655:1–a1655:6. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258:1–h1258:7. [Google Scholar] [CrossRef] [PubMed]
- Steckler, A.B.; Linnan, L.; Israel, B. Process Evaluation for Public Health Interventions and Research; Jossey-Bass: San Francisco, CA, USA, 2002. [Google Scholar]
- W. K. Kellogg Foundation. WK Kellogg Foundation Logic Model Development Guide; WK Kellogg Foundation: Battle Creek, MI, USA, 2004. [Google Scholar]
- Moore, G.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Cooper, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T. Process evaluation in complex public health intervention studies: The need for guidance. J. Epidemiol. Community Health 2014, 68, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Saunders, R.P.; Evans, M.H.; Joshi, P. Developing a process-evaluation plan for assessing health promotion program implementation: A how-to guide. Health Promot. Pract. 2005, 6, 134–147. [Google Scholar] [CrossRef] [PubMed]
- Sveriges Kommuner och Regioner. Municipalities and Regions. Available online: https://skr.se/tjanster/englishpages/municipalitiesandregions.1088.html (accessed on 7 December 2020).
- LaMontagne, A.D.; Keegel, T.; Vallance, D. Protecting and promoting mental health in the workplace: Developing a systems approach to job stress. Health Promot. J. Austr. 2007, 18, 221–228. [Google Scholar] [CrossRef]
- Akerstrom, M.; Corin, L.; Severin, J.; Jonsdottir, I.H.; Björk, L. Can Working Conditions and Employees’ Mental Health be Improved via Job Stress Interventions Designed and Implemented by Line Managers and Human Resources on an Operational Level? Int. J. Environ. Res. Public Health 2021, 18, 1916. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Proper, K.I.; van Oostrom, S.H. The effectiveness of workplace health promotion interventions on physical and mental health outcomes—A systematic review of reviews. Scand. J. Work Environ. Health 2019, 45, 546–559. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Evans, R.E. What theory, for whom and in which context? Reflections on the application of theory in the development and evaluation of complex population health interventions. SSM Popul. Health 2017, 3, 132–135. [Google Scholar] [CrossRef]
- Rimer, B.K.; Kreuter, M.W. Advancing tailored health communication: A persuasion and message effects perspective. J. Commun. 2006, 56, S184–S201. [Google Scholar] [CrossRef]
- Andreasson, J.; Eriksson, A.; Dellve, L. Health care managers’ views on and approaches to implementing models for improving care processes. J. Nurs. Manag. 2016, 24, 219–227. [Google Scholar] [CrossRef]
- Wikström, E.; Dellenborg, L.; Wallin, L.; Gillespie, B.M.; Andersson, A.E. The Safe Hands Study: Implementing aseptic techniques in the operating room: Facilitating mechanisms for contextual negotiation and collective action. Am. J. Infect. Control 2019, 47, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Corin, L.; Björk, L. Job demands and job resources in human service managerial work an external assessment through work content analysis. Nord. J. Work. Life Stud. 2016, 6, 3–28. [Google Scholar] [CrossRef]
- Hammer, L.B.; Truxillo, D.M.; Bodner, T.; Pytlovany, A.C.; Richman, A. Exploration of the impact of organisational context on a workplace safety and health intervention. Work Stress 2019, 33, 192–210. [Google Scholar] [CrossRef]
- McFillen, J.M.; O’Neil, D.A.; Balzer, W.K.; Varney, G.H. Organizational diagnosis: An evidence-based approach. J. Chang. Manag. 2013, 13, 223–246. [Google Scholar] [CrossRef]
- Nielsen, K.; Randall, R. Assessing and Addressing the Fit of Planned Interventions to the Organizational Context. In Derailed Organizational Interventions for Stress and Well-Being: Confessions of Failure and Solutions for Success; Karanika-Murray, M., Biron, C., Eds.; Springer: Dordrecht, The Netherlands, 2015; pp. 107–113. [Google Scholar]
- Ipsen, C.; Gish, L.; Poulsen, S. Organizational-level interventions in small and medium-sized enterprises: Enabling and inhibiting factors in the PoWRS program. Saf. Sci. 2015, 71, 264–274. [Google Scholar] [CrossRef]
- LaMontagne, A.D.; Noblet, A.J.; Landsbergis, P.A. Intervention development and implementation: Understanding and addressing barriers to organizational-level interventions. In Improving Organizational Interventions for Stress and Well-Being: Addressing Process and Context; Biron, C., Karanika-Murray, M., Cooper, C., Eds.; Routledge/Taylor & Francis Group: New York, NY, USA, 2012; pp. 21–38. [Google Scholar]
- Mellor, N.; Smith, P.; Mackay, C.; Palferman, D. The “Management Standards” for stress in large organizations. Int. J. Workplace Health Manag. 2013, 6, 4–17. [Google Scholar] [CrossRef]
| Applications, n (%) | |
|---|---|
| Type of organization | |
| - Major hospital | 68 (44) |
| - Minor hospital | 56 (36) |
| - Primary care | 15 (10) |
| - Service and maintenance | 12 (8) |
| - Culture | 3 (2) |
| Type of workplace | |
| - Health care | 106 (69) |
| - Administration | 28 (18) |
| - Service | 12 (8) |
| - Management | 8 (5) |
| Targeted group in the application | |
| - All employees | 114 (74) |
| - Subgroup of employees | 30 (20) |
| - Managers only | 10 (6) |
| Role that initiated the application | |
| - Line manager and HR together | 97 (63) |
| - Line manager without HR | 31 (20) |
| - HR without the line manager | 26 (17) |
| Variable | Item Wording | Response Scale (Min–Max) | Intervention Groups * (n = 51) | Reference Groups * (Operational Areas) (n = 51) | |||
|---|---|---|---|---|---|---|---|
| Mean | Mean Range (Min–Max) | Mean | Mean Range (Min–Max) | p-Value (Difference in Mean) | |||
| Recovery | “I have scope for recovery during the working day through breaks and/or rests.” | 1 = Strongly disagree– 5 = Strongly agree | 3.22 | 1.91–4.09 | 3.27 | 1.91–4.06 | 0.96 |
| Stress ** | “Do you feel stressed currently? (Stress means a condition in which you feel tense, nervous, or uneasy, or are unable to sleep at night because you are thinking about problems the whole time).” | 1 = None–5 = Very much | 2.82 | 1.87–3.90 | 2.70 | 2.29–3.27 | 0.1 |
| Quantity of work | “The quantity of my work seems reasonable.” | 1 = Strongly disagree– 5 = Strongly agree | 3.13 | 1.72–4.18 | 3.19 | 1.94–4.11 | 0.9 |
| Looking forward to work | “I look forward to going to work.” | 1 = Strongly disagree– 5 = Strongly agree | 3.77 | 2.82–4.53 | 3.89 | 3.45–4.23 | 0.008 |
| Reflection | “I have time for reflection and consideration in my work.” | 1 = Strongly disagree– 5 = Strongly agree | 2.88 | 1.55–3.85 | 2.93 | 1.77–3.78 | <0.001 |
| Effectiveness | “How satisfied are you with the effectiveness of the work performed by your unit/department? (Effectiveness here means doing the right things in the right way in the right order and without any unnecessary waste of time).” | 1 = Very dissatisfied– 5 = Very satisfied | 3.35 | 2.56–3.98 | 3.27 | 2.31–4.0 | 0.2 |
| Work situation | “How satisfied are you with your current work situation?” | 1 = Very dissatisfied– 5 = Very satisfied | 3.49 | 1.91–4.4 | 3.60 | 2.75–4.22 | 0.08 |
| Reference Groups | ||||||
|---|---|---|---|---|---|---|
| Intervention Groups (n = 71) | Operational Areas (n = 67) * | Departments (n = 71) | ||||
| Mean | Mean Range (Min–Max) | Mean (p-Value between Intervention Groups and Operational Area) | Mean Range (Min–Max) | Mean (p-Value between Intervention Groups and Department) | Mean Range (Min–Max) | |
| Total sickness absence | ||||||
| 12 months | 8.3% | 0.7–17.9% | 7.0% (p = 0.008) | 1.3–12.6% | 7.1% (p = 0.001) | 6.3–9.1% |
| 6 months | 9.1% | 0.3–19.8% | 7.6% (p = 0.007) | 1.6–13.5% | 7.7% (p = 0.001) | 6.9–9.8% |
| 3 months | 9.3% | 0.6–22.1% | 7.8% (p = 0.012) | 1.3–14.1% | 8.0% (p = 0.001) | 7.4–9.7% |
| Short-term sickness absence (≤14 days) | ||||||
| 12 months | 2.9% | 0.4–4.8% | 2.5% (p = 0.003) | 1.1–3.7% | 2.6% (p < 0.001) | 2.1–3.4% |
| 6 months | 3.5% | 0.3–6.1% | 3.0% (p = 0.001) | 1.3–4.4% | 3.1% (p < 0.001) | 2.5–3.9% |
| 3 months | 3.9% | 0.6–8.1% | 3.3% (p = 0.005) | 1.3–5.1% | 3.4% (p < 0.001) | 2.9–4.4% |
| Level of Described Challenge | |||||
|---|---|---|---|---|---|
| Individual | Group | Organisational | Sum | ||
| Level of suggested measure | Individual | 0 (0%) | 0 (0%) | 87 (42%) | 87 (42%) |
| Group | 0 (0%) | 6 (3%) | 49 (23%) | 55 (26%) | |
| Organisational | 0 (0%) | 0 (0%) | 67 (32%) | 67 (32%) | |
| Sum | 0 (0%) | 6 (3%) | 203 (97%) | 209 (100%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Severin, J.; Björk, L.; Corin, L.; Jonsdottir, I.H.; Akerstrom, M. Process Evaluation of an Operational-Level Job Stress Intervention Aimed at Decreasing Sickness Absence among Public Sector Employees in Sweden. Int. J. Environ. Res. Public Health 2021, 18, 1778. https://doi.org/10.3390/ijerph18041778
Severin J, Björk L, Corin L, Jonsdottir IH, Akerstrom M. Process Evaluation of an Operational-Level Job Stress Intervention Aimed at Decreasing Sickness Absence among Public Sector Employees in Sweden. International Journal of Environmental Research and Public Health. 2021; 18(4):1778. https://doi.org/10.3390/ijerph18041778
Chicago/Turabian StyleSeverin, Jonathan, Lisa Björk, Linda Corin, Ingibjörg H. Jonsdottir, and Magnus Akerstrom. 2021. "Process Evaluation of an Operational-Level Job Stress Intervention Aimed at Decreasing Sickness Absence among Public Sector Employees in Sweden" International Journal of Environmental Research and Public Health 18, no. 4: 1778. https://doi.org/10.3390/ijerph18041778
APA StyleSeverin, J., Björk, L., Corin, L., Jonsdottir, I. H., & Akerstrom, M. (2021). Process Evaluation of an Operational-Level Job Stress Intervention Aimed at Decreasing Sickness Absence among Public Sector Employees in Sweden. International Journal of Environmental Research and Public Health, 18(4), 1778. https://doi.org/10.3390/ijerph18041778






