Identification of Growth Patterns in Low Birth Weight Infants from Birth to 5 Years of Age: Nationwide Korean Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Data Source
2.2. Statistical Analyses
2.3. Ethics Statement
3. Results
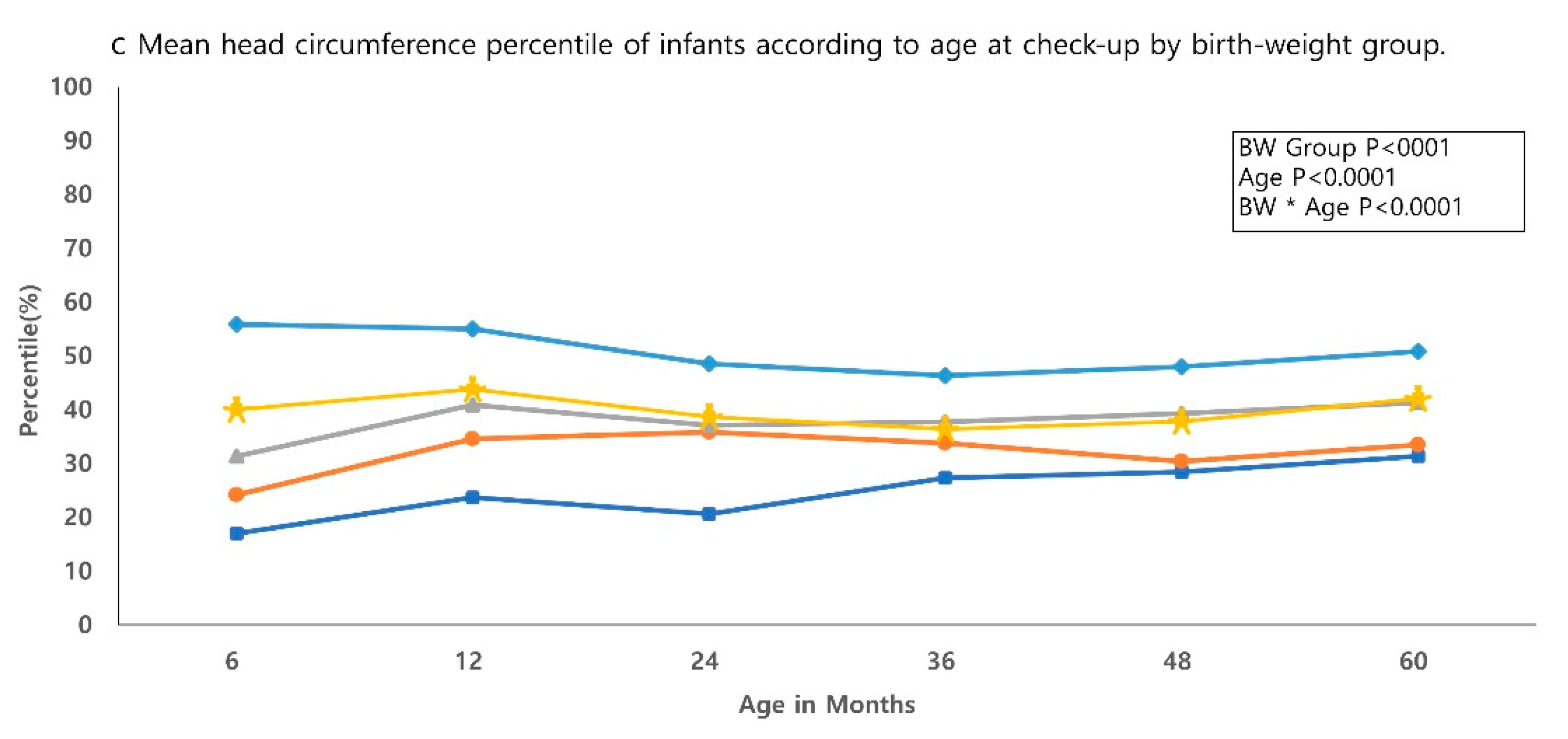
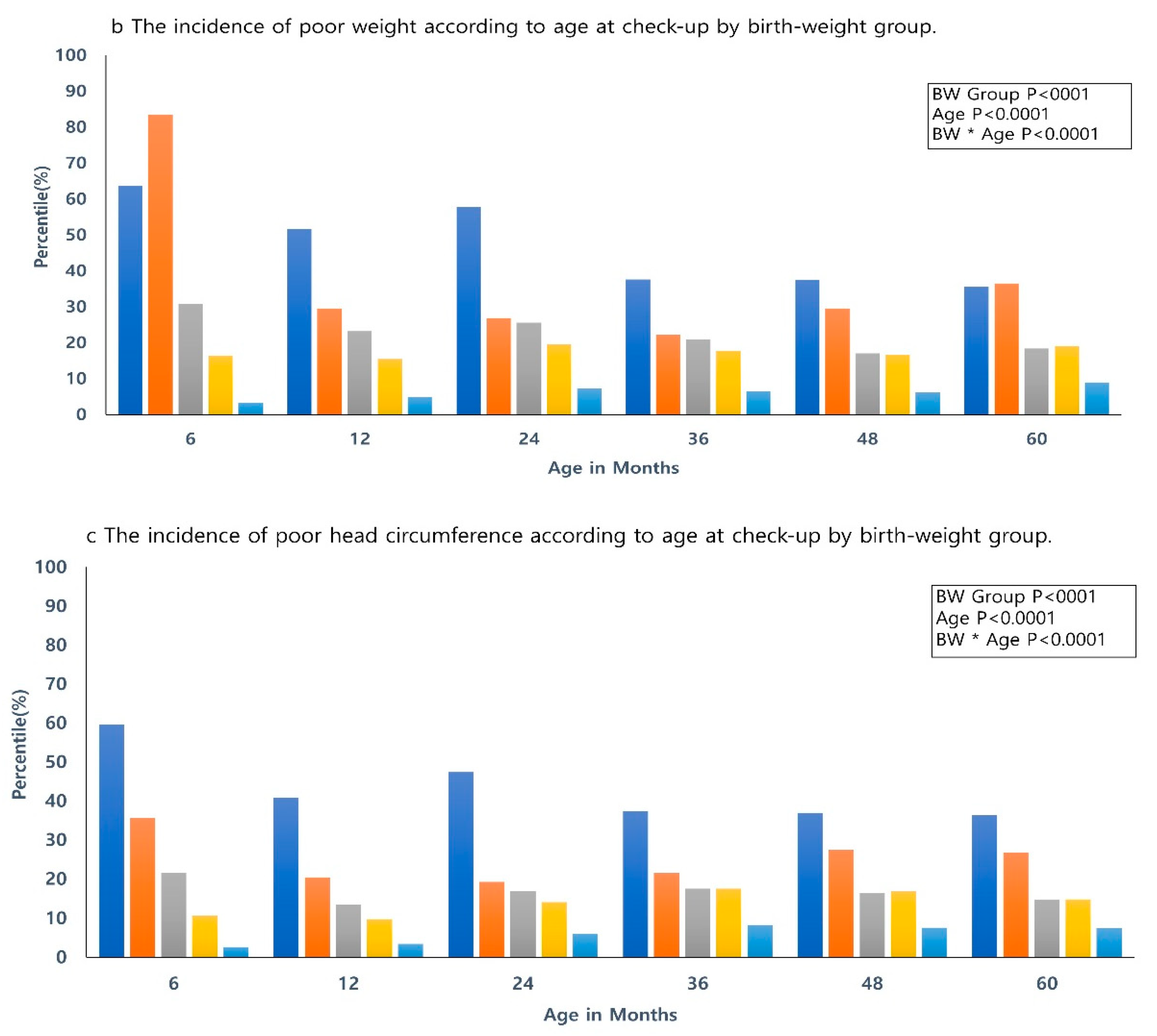
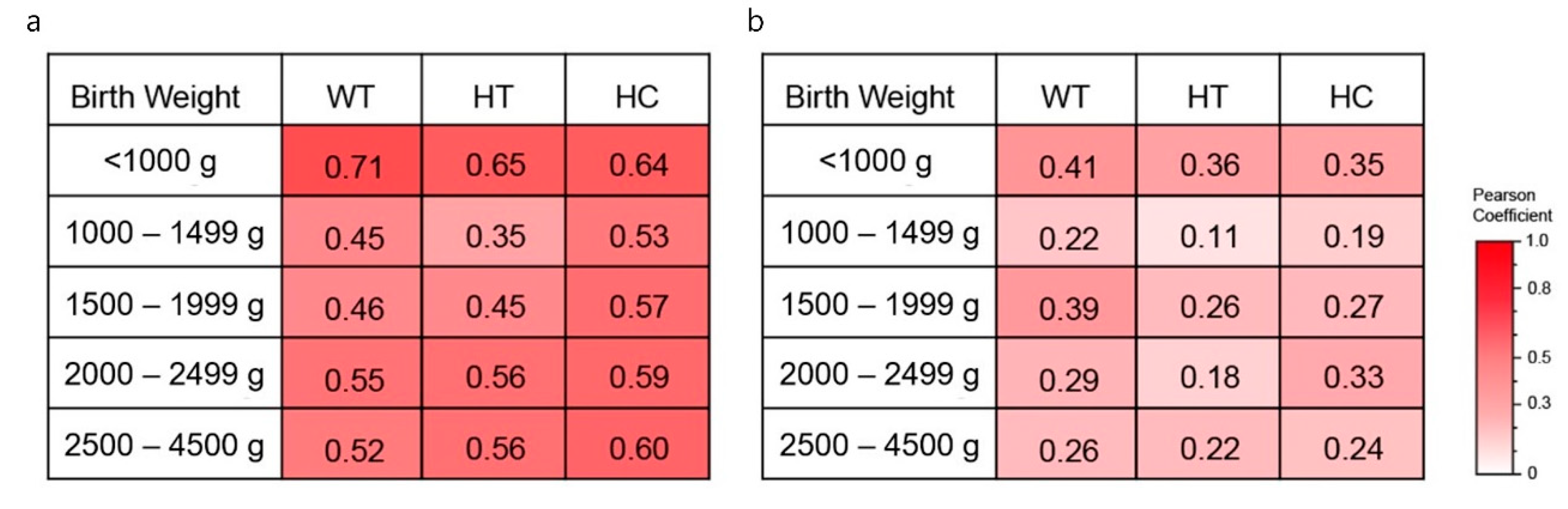
3.1. Growth Outcome
3.2. Developmental Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Deng, Y.; Yang, F.; Mu, D. First-year growth of 834 preterm infants in a Chinese population: A single-center study. BMC Pediatr. 2019, 19, 403–410. [Google Scholar] [CrossRef]
- Kunz, S.N.; Bell, K.; Belfort, M.B. Early Nutrition in Preterm Infants: Effects on Neurodevelopment and Cardiometabolic Health. NeoReviews 2016, 17, e386–e393. [Google Scholar] [CrossRef]
- Euser, A.; De Wit, C.; Finken, M.; Rijken, M.; Wit, J.M. Growth of Preterm Born Children. Horm. Res. Paediatr. 2008, 70, 319–328. [Google Scholar] [CrossRef]
- Guellec, I.; Lapillonne, A.; Marret, S.; Picaud, J.-C.; Mitanchez, D.; Charkaluk, M.-L.; Fresson, J.; Arnaud, C.; Flamand, C.; Cambonie, G.; et al. Effect of Intra- and Extrauterine Growth on Long-Term Neurologic Outcomes of Very Preterm Infants. J. Pediatr. 2016, 175, 93–99.e1. [Google Scholar] [CrossRef] [PubMed]
- Dotinga, B.M.; Eshuis, M.S.; Bocca-Tjeertes, I.F.; Kerstjens, J.M.; Van Braeckel, K.N.; Reijneveld, S.A.; Bos, A.F. Longitudinal Growth and Neuropsychological Functioning at Age 7 in Moderate and Late Preterms. Pediatrics 2016, 138, 138. [Google Scholar] [CrossRef] [PubMed]
- Saigal, S.; Stoskopf, B.; Streiner, D.L.; Paneth, N.S.; Pinelli, J.; Boyle, M. Growth Trajectories of Extremely Low Birth Weight Infants From Birth to Young Adulthood: A Longitudinal, Population-Based Study. Pediatr. Res. 2006, 60, 751–758. [Google Scholar] [CrossRef]
- Ong, K.K. Catch-up growth in small for gestational age babies: Good or bad? Curr. Opin. Endocrinol. Diabetes Obes. 2007, 14, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Icd-10 Version. 2019. Available online: https://icd.who.int/browse10/2019/en (accessed on 25 July 2020).
- KOrean Statistical Information Service. National Statistics. Available online: http://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ZTITLE&parmTabId=M_01_01#SelectStatsBoxDiv (accessed on 25 July 2020).
- Moon, J.S. Review of National Health Screening Program for Infant and Children in Korea. J. Korean Med. Assoc. 2010, 53, 377. [Google Scholar] [CrossRef]
- Jang, C.H.; Kim, S.W.; Jeon, H.R.; Jung, D.W.; Cho, H.E.; Kim, J.; Lee, J.W. Clinical Usefulness of the Korean Developmental Screening Test (K-DST) for Developmental Delays. Ann. Rehabil. Med. 2019, 43, 490–496. [Google Scholar] [CrossRef]
- Chung, H.J.; Yang, D.; Kim, G.-H.; Kim, S.K.; Kim, S.W.; Kim, Y.K.; Kim, J.S.; Kim, J.K.; Kim, C.; Sung, I.-K.; et al. Development of the Korean Developmental Screening Test for Infants and Children (K-DST). Clin. Exp. Pediatr. 2020, 63, 438–446. [Google Scholar] [CrossRef]
- Kim, C.Y.; Jung, E.; Lee, B.S.; Kim, K.-S.; Kim, E.A.-R. Validity of the Korean Developmental Screening Test for very-low-birth-weight infants. Korean J. Pediatr. 2019, 62, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Van de Pol, C.; Allegaert, K. Growth patterns and body composition in former extremely low birth weight (elbw) neonates until adulthood: A systematic review. Eur. J. Pediatr. 2020, 179, 757–771. [Google Scholar] [PubMed]
- Pilling, E.; Elder, C.; Gibson, A. Growth patterns in the growth-retarded premature infant. Best Pr. Res. Clin. Endocrinol. Metab. 2008, 22, 447–462. [Google Scholar] [CrossRef] [PubMed]
- Saenger, P.; Czernichow, P.; Hughes, I.; Reiter, E.O. Small for Gestational Age: Short Stature and Beyond. Endocr. Rev. 2007, 28, 219–251. [Google Scholar] [CrossRef] [PubMed]
- Toftlund, L.H.; Halken, S.; Agertoft, L.; Zachariassen, G. Catch-Up Growth, Rapid Weight Growth, and Continuous Growth from Birth to 6 Years of Age in Very-Preterm-Born Children. Neonatology 2018, 114, 285–293. [Google Scholar] [CrossRef]
- Liao, W.-L.; Lin, M.-C.; Wang, T.-M.; Chen, C.-H.; Taiwan Premature Infant Follow-up Network. Risk factors for postdischarge growth retardation among very-low-birth-weight infants: A nationwide registry study in Taiwan. Pediatr. Neonatol. 2019, 60, 641–647. [Google Scholar] [PubMed]
- Clayton, P.E.; Cianfarani, S.; Czernichow, P.; Johannsson, G.; Rapaport, R.; Rogol, A. Management of the Child Born Small for Gestational Age through to Adulthood: A Consensus Statement of the International Societies of Pediatric Endocrinology and the Growth Hormone Research Society. J. Clin. Endocrinol. Metab. 2007, 92, 804–810. [Google Scholar]
- Farooqi, A.; Hägglöf, B.; Sedin, G.; Gothefors, L.; Serenius, F. Growth in 10- to 12-Year-Old Children Born at 23 to 25 Weeks’ Gestation in the 1990s: A Swedish National Prospective Follow-up Study. Pediatrics 2006, 118, e1452–e1465. [Google Scholar] [CrossRef]
- Labarta, J.I.; Ruiz, J.A.; Molina, I.; De Arriba, A.; Mayayo, E.; Longás, A.F. Growth and growth hormone treatment in short stature children born small for gestational age. Pediatr. Endocrinol. Rev. 2009, 6, 350–357. [Google Scholar]
- Taine, M.; Charles, M.; Beltrand, J.; Rozé, J.-C.; Léger, J.; Botton, J.; Heude, B. Early postnatal growth and neurodevelopment in children born moderately preterm or small for gestational age at term: A systematic review. Paediatr. Périnat. Epidemiol. 2018, 32, 268–280. [Google Scholar] [CrossRef]
- Takeuchi, A.; Yorifuji, T.; Hattori, M.; Tamai, K.; Nakamura, K.; Nakamura, M.; Kageyama, M.; Kubo, T.; Ogino, T.; Kobayashi, K.; et al. Catch-up growth and behavioral development among preterm, small-for-gestational-age children: A nationwide Japanese population-based study. Brain Dev. 2019, 41, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Pylipow, M.; Spector, L.G.; Puumala, S.E.; Boys, C.; Cohen, J.; Georgieff, M.K. Early Postnatal Weight Gain, Intellectual Performance, and Body Mass Index at 7 Years of Age in Term Infants with Intrauterine Growth Restriction. J. Pediatr. 2009, 154, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Casey, P.H.; Whiteside-Mansell, L.; Barrett, K.; Bradley, R.H.; Gargus, R. Impact of Prenatal and/or Postnatal Growth Problems in Low Birth Weight Preterm Infants on School-Age Outcomes: An 8-Year Longitudinal Evaluation. Pediatrics 2006, 118, 1078–1086. [Google Scholar] [CrossRef] [PubMed]
- Andrews, E.T.; Ashton, J.J.; Pearson, F.; Beattie, R.M.; Johnson, M.J. Early postnatal growth failure in preterm infants is not inevitable. Arch. Dis. Child. Fetal Neonatal Ed. 2019, 104, F235–F241. [Google Scholar] [CrossRef]
- Ng, S.M.; Pintus, D.; Turner, M.A. Extreme premature small for gestational age infants have appropriate catch-up growth at term equivalence compared with extreme premature appropriate for gestational age infants. J. Clin. Res. Pediatr. Endocrinol. 2019, 11, 104–108. [Google Scholar]
- Morgan, C.; McGowan, P.; Herwitker, S.; Hart, A.E.; Turner, M.A. Postnatal Head Growth in Preterm Infants: A Randomized Controlled Parenteral Nutrition Study. Pediatrics 2013, 133, e120–e128. [Google Scholar] [CrossRef]
- Olbertz, D.M.; Mumm, R.; Wittwer-Backofen, U.; Fricke-Otto, S.; Pyper, A.; Otte, J.; Wabitsch, M.; Gottmann, P.; Schwab, K.O.; Scholten, M.; et al. Identification of growth patterns of preterm and small-for-gestational age children from birth to 4 years—Do they catch up? J. Périnat. Med. 2019, 47, 448–454. [Google Scholar] [CrossRef]
- Jung, H.; Rosilio, M.; Blum, W.F.; Drop, S.L.S. Growth hormone treatment for short stature in children born small for gestational age. Adv. Ther. 2008, 25, 951–978. [Google Scholar] [CrossRef]
- Arai, S.; Sato, Y.; Muramatsu, H.; Yamamoto, H.; Aoki, F.; Okai, Y.; Kataoka, S.; Hanada, Y.; Hamada, M.; Morimoto, Y.; et al. Risk factors for absence of catch-up growth in small for gestational age very low-birthweight infants. Pediatr. Int. 2019, 61, 889–894. [Google Scholar] [CrossRef]


| Age at Exam | Total Infants | <1000 g | 1000–1499 g | 1500–1999 g | 2000–2499 g | 2500–4500 g | Preterm |
|---|---|---|---|---|---|---|---|
| 6 months | 311,446 (72.3) | 137 (0.0) | 693 (0.2) | 2332 (0.7) | 11,539 (3.7) | 295,989 (95.0) | 11,398 (3.7) |
| 12 months | 313,235 (72.8) | 196 (0.1) | 819 (0.3) | 2487 (0.8) | 11,826 (3.8) | 297,151 (94.9) | 10,919 (3.5) |
| 24 months | 347,153 (80.6) | 314 (0.1) | 1376 (0.4) | 3050 (0.9) | 13,320 (3.8) | 328,176 (94.5) | 12,355 (3.6) |
| 36 months | 344,468 (80.0) | 643 (0.2) | 1959 (0.6) | 3495 (1.0) | 13,240 (3.8) | 324,086 (94.1) | 26,338 (7.6) |
| 48 months | 323,958 (75.2) | 606 (0.2) | 1425 (0.4) | 3747 (1.2) | 12,809 (4.0) | 304,361 (94.0) | 26,028 (8.0) |
| 60 months | 286,331 (66.5) | 662 (0.2) | 1174 (0.4) | 4584 (1.6) | 12,288 (4.3) | 266,669 (93.1) | 23,542 (8.2) |
| BW Group | Number of Infants | Further Evaluation | Follow-Up Test | Peer & High Level | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Gross Motor | Fine Motor | Cognition | Communication | Social Interaction | Self-Control | Total | Gros Motor | Fine Motor | Cognition | Communication | Social Interaction | Self-Control | |||
| <1000 g | 529 | 56 (11) | 48 | 48 | 45 | 47 | 39 | 42 | 91 (17) | 59 | 47 | 44 | 40 | 25 | 30 | 382 (72) |
| 1000–1499 g | 1067 | 63 (6) | 56 | 53 | 46 | 48 | 45 | 46 | 142 (13) | 65 | 62 | 54 | 57 | 35 | 53 | 862 (81) |
| 1500–1999 g | 2316 | 96 (4) | 68 | 64 | 65 | 72 | 59 | 56 | 285 (12) | 111 | 123 | 104 | 95 | 75 | 93 | 1935 (84) |
| 2000–2499 g | 9381 | 254 (3) | 143 | 168 | 184 | 198 | 156 | 127 | 947 (10) | 332 | 383 | 369 | 342 | 269 | 293 | 8180 (87) |
| 2500–4500 g | 263,579 | 4094 (2) | 2201 | 2603 | 2825 | 3089 | 2454 | 2111 | 22,930 (9) | 7394 | 8234 | 8848 | 8820 | 5938 | 7013 | 236,555 (89) |
| BW Group | Number of Infants | WT Poor | HT Poor | HC Poor |
|---|---|---|---|---|
| <1000 g | 147 | 96 (65) | 73 (50) | 86 (59) |
| 1000–1499 g | 205 | 71 (35) | 88 (43) | 83 (40) |
| 1500–1999 g | 381 | 112 (29) | 117 (31) | 146 (38) |
| 2000–2499 g | 1201 | 319 (27) | 342 (28) | 393 (33) |
| 2500–4500 g | 27,024 | 2520 (9) | 2663 (10) | 2958 (11) |
| Variable | OR (95% CI) | p Value |
|---|---|---|
| Poor HC at 60 months of age | 1.81 (1.66–1.98) | <0.001 |
| Poor HT at 60 months of age | 1.63 (1.48–1.80) | <0.001 |
| Poor WT at 60 months of age | 1.18 (1.07–1.30) | <0.001 |
| BW 1000 g vs. 2500–4500 g | 5.05 (3.79–6.73) | <0.001 |
| 1000–1499 g vs. 2500–4500 g | 3.05 (2.35–3.96) | |
| 1500–1999 g vs. 2500–4500 g | 2.37 (1.92–2.92) | |
| 2000–2499 g vs. 2500–4500 g | 1.64 (1.44–1.87) | |
| Male vs. Female | 2.02 (1.90–2.15) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, S.J.; Lim, J.; Han, J.H.; Shin, J.E.; Lee, S.M.; Eun, H.S.; Park, M.S.; Park, K.I. Identification of Growth Patterns in Low Birth Weight Infants from Birth to 5 Years of Age: Nationwide Korean Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 1206. https://doi.org/10.3390/ijerph18031206
Yoon SJ, Lim J, Han JH, Shin JE, Lee SM, Eun HS, Park MS, Park KI. Identification of Growth Patterns in Low Birth Weight Infants from Birth to 5 Years of Age: Nationwide Korean Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(3):1206. https://doi.org/10.3390/ijerph18031206
Chicago/Turabian StyleYoon, So Jin, Joohee Lim, Jung Ho Han, Jeong Eun Shin, Soon Min Lee, Ho Seon Eun, Min Soo Park, and Kook In Park. 2021. "Identification of Growth Patterns in Low Birth Weight Infants from Birth to 5 Years of Age: Nationwide Korean Cohort Study" International Journal of Environmental Research and Public Health 18, no. 3: 1206. https://doi.org/10.3390/ijerph18031206
APA StyleYoon, S. J., Lim, J., Han, J. H., Shin, J. E., Lee, S. M., Eun, H. S., Park, M. S., & Park, K. I. (2021). Identification of Growth Patterns in Low Birth Weight Infants from Birth to 5 Years of Age: Nationwide Korean Cohort Study. International Journal of Environmental Research and Public Health, 18(3), 1206. https://doi.org/10.3390/ijerph18031206






