Abstract
Background The promotion of Physical Activity (PA) is an important public health goal to reduce comorbidity and diseases associated with aging such as anxiety and depression. Aim: To investigate the association between level of PA, mental health and the consumption of medications among a representative cohort of Spanish pre-elderly people. Methods: Cross-sectional study with 5977 participants aged 50 to 64 years who participated in the National Health Survey in Spain 2017. The levels of PA were evaluated using the International Physical Activity Questionnaire and the mental conditions were measured by the Goldberg Health Questionnaire-12 (GHQ-12). The chi-square test was used for qualitative variables; Pearson’s correlation was conducted between GHQ-12 score with different quantitative variables; and a logistic regression was used to determine the association between PA and mental health with the sociodemographic characteristics. Results: The participants were 51.9% women and 48.1% men with a mean age of 56.79 years, and 35.5% of participants had a low level of PA. A low level of PA was associated with cases of mental health vulnerability, anxiety and depression (in women), the consumption of more medications and greater multimorbidity. Conclusion: It is important that people reach old age with an optimal health status in order to reduce age-related disability and morbidity. More than a third of the Spanish pre-elderly do not reach the levels of PA recommended by the WHO. People who had low level of PA consumed more medications and had higher mental health vulnerability and greater multimorbidity.
1. Introduction
The world’s population is aging faster than in recent decades [1,2]. In fact, 1 in 6 people in the world will be over 65 in 2050. In Spain, 25% of the population will be over 65 in 2030 and it will be the European country with the largest increase in the share of older persons by 2050 [1]. For this reason, increasing numbers of older adults are living with disabilities and health conditions that are preventable through lifestyle modifications [3]. For this, active aging is a very important issue for enabling individuals to reach retirement in the best possible health condition in this aging society.
Population aging is a public health success story, but at the same time it represents the challenge of maintaining the quality of life, functional capacity, and social participation of older adults [4]. In fact, there is an increasing incidence of mental disorders in the elderly, with depression and anxiety being the most commonly diagnosed mental disorders [5,6]. The World Health Organization (WHO) estimates that approximately 1 in 10 older adults may suffer from depression, with the prevalence increasing with age [7,8]. Depression is commonly treated with antidepressants in primary care. However, antidepressants can have adverse side effects, low treatment adherence, and there is a delay between the beginning of antidepressant use and improvements in mood [9]. In addition, the use of antidepressant medication is associated with recurrent falls in elderly individuals [7,10]. In the case of people with anxiety disorders, antidepressant drugs such as selective serotonin reuptake inhibitors (SSRIs) are the first-line treatments. However, one-third of patients do not respond to SSRIs [11]. Considering that depression is currently the leading cause of the disability burden worldwide and that its prevalence increases with age [12], it is necessary to act on the modifiable risk factors that are related to it, such as physical inactivity [13].
The aging process associated with sedentary lifestyles promotes mental, social and physical dependence, and is associated with all-cause mortality and premature death [6,14]. In fact, physical inactivity is the fourth leading risk factor for global mortality [15]. In contrast, there are several studies that have shown that physical activity (PA) protects from the emergence of depression and anxiety [9,16,17]. PA is a key determinant of physical, mental and social health in all age groups and it associated with improved health status [18]. Promoting and maintaining higher levels of PA in the older population is an imperative for active aging [3]. Achieving >150 min/week of moderate-intense aerobic exercise is associated with at least a 30% lower risk of morbidity, mortality, and functional dependence compared with being inactive [19]. Moreover, PA prevents and reduces the risk of osteoporosis, type 2 diabetes, hypertension obesity, stroke, heart disease, colon cancer, breast cancer and depression [3,15,20,21]. In addition, regularly performed PA is one of the main non-pharmacological strategies for healthier aging and is associated with the lower consumption of medications [22]. It is noteworthy that in the last decade in Spain, older people have decreased their levels of PA while the consumption of medications has increased [21,23]. In fact, recent studies show that people who do PA several times a week consume almost 20% less medication than people who never do PA [24].
The PA should be a common habit with the aim of having healthy aging and reaching retirement age with the best health and quality of life. A recent study in Poland suggests that physical inactivity begins at age 50 [25]. At this age, women also begin menopause, which can lead to a loss of aerobic fitness, muscle strength, and bone mineral density, as well as weight gain [26]. This increases the risk of many chronic diseases such as coronary heart disease, type 2 diabetes mellitus or osteoporotic fractures, especially in sedentary individuals [27]. To counteract the effects of this stage of life, PA plays an important role because it improves muscle strength, increases bone metabolism and functional capacity, prevents type 2 diabetes and decreases obesity and depression, thereby improving the quality of life and enabling people to reach old age with better health in general [21,26]. As a result, PA is an important public health objective to mitigate the burden of age-related diseases [28].
In Spain, there are programs for older people to promote PA with the aim of guaranteeing the Spanish population universal access to PA, reducing sedentarism and obesity and to promote healthy lifestyle habits [29]. In addition, these PA promotion programs also aim to improve mental health in the Spanish population. However, PA levels have decreased from 2009 to 2017, with an average of 1.32 h per week spent on moderate PA and 1.28 h per week on walking [21].
Therefore, PA could be an effective intervention both to improve mental health (mainly to reduce anxiety and depression) and to reduce the consumption of medications (including that associated with mental disorders as antidepressants, benzodiazepines, etc.). For this reason, it is important to evaluate the association between PA levels and anxiety and depression, because these aspects can slow down the symptoms associated with the prevalence of chronic degenerative diseases [6]. Although there are many studies about the benefits of PA in mental health in older people [5,6,9,16,17], to the best of our knowledge, there are no known studies that have been conducted on pre-elderly people (a stage that ranges from 50 to 64 years according to several authors [30,31,32]) that relates mental health to levels of PA and the consumption of medications. Our hypothesis is that pre-elderly people who do moderate or intense PA have better mental health (suffer fewer problems of depression and anxiety), less consumption of medications and have a better state of health than sedentary people.
Based on the afore, the objectives of this study were: (1) to investigate the association between PA levels, mental health and the consumption of medications among a representative cohort of Spanish pre-elderly people; (2) to know the prevalence and associated factors of level of PA in Spanish pre-elderly people.
2. Materials and Methods
2.1. Study Design and Participants
This is a cross-sectional study, performed with secondary data from the National Health Survey in Spain (NHSS) 2017 [33]. The NHSS was carried out through a personal interview by the National Statistics Institute (Instituto Nacional de Estadística—INE) and the Ministry of Health, Social Services and Equality (Ministerio de Salud, Servicios Sociales e Igualdad—MSSI). The NHSS use probabilistic multistage sampling with stratification of the first-stage units (census sections) and the second-stage units (main family dwellings), with the final units (individuals) being selected by means of random routes and sex- and age-based quotas. These data from the NHSS are available as anonymized data on the INE web. As we used public anonymized secondary data, the approval of an ethics committee was not necessary, according to Spanish legislation.
For the purpose of the current study, the study population was restricted to non-institutionalized individuals between 50 and 64 years of age, which is the pre-elderly stage age according several studies [30,31,32]. Thus, the number of participants included in the study was 5977.
2.2. Instruments and Variables
The data collection instruments used by the INE and MSSI, in a transverse way, was 2017 EHSS [33]. In this survey, participants are asked about the following variables:
- Sociodemographic variables: age, sex, marital status, level of education and social class (according to Domingo-Salvany et al. [34]: class I: directors and managers of companies with 10 or more employees and professionals with university degrees; class II: directors of companies with fewer than 10 employees and professionals with college diplomas; class III, intermediate occupations; class IV: workers in qualified technical occupations; class V: primary sector workers; and class VI: unskilled workers).
- Mental health variables: self-reported depression and anxiety in the last 12 months (with a medical diagnosis) and mental conditions (psychological morbidity and possible cases of non-psychotic psychiatric disorders).
- Health-related variables such as health self-perception, disease or chronic/long-term illnesses, multimorbidity (according to the WHO [35], multimorbidity is considered the coexistence of two or more chronic conditions in the same individual, and data were collected across 32 medical diagnoses), body mass index (BMI) (according to WHO criteria [36], BMI is categorised as follows:<18.5 kg/m2, underweight; 18.5–24.9 kg/m2, normal; 25.0–29.9 kg/m2, overweight; and ≥30 kg/m2, obese), the consumption of medications in the last 2 weeks (including the consumption of tranquilisers/relaxants/sleeping pills and the consumption of antidepressants/stimulants) and polypharmacy (according to the WHO [37], polypharmacy is considered the simultaneous consumption of 5 or more medications; our study referred to the last two weeks).
- Physical Activity variables: type of PA performed in the main activity, frequency with which they perform PA, PA performed in the last 7 days (intense/moderate), number of days a week in which they walk for at least 10 min, time spent walking per week and time spent doing physical exercise in leisure time.
The mental conditions were measured by the Goldberg Health Questionnaire-12 (GHQ-12), Spanish version [38], which is a self-administered screening instrument aimed at detecting psychological morbidity and possible cases of non-psychotic psychiatric disorders. The questionnaire consists of 12 items, and response options range from 0 (never) to 3 (more than usual). We transformed the typical Likert scale (0-1-2-3) into a dichotomy punctuation (0-0-1-1) in order to obtain a 12-point scale variable because the literature suggests that this is the most appropriate score [38,39]. In addition, we chose a cut-off score greater than 5 to detect cases of mental health vulnerability in the participants (GHQ-12 ≤ 5 = non case and GHQ-12 ≥ 6 = case) [40].
PA was measured by the short version of the International Physical Activity Questionnaire (IPAQ), Spanish version [41]. The IPAQ consists of 7 self-reported questions that assess the intensity (low, moderate or vigorous), frequency (days and hours per week) and duration or time spent on each of the activities. PA was defined as the level of self-reported engagement in moderate activity in a typical week: both days/week and h/week and walking for 10 min (days/week). Moderate activities were those that produce a slightly stronger than normal increase in breathing, heart rate and sweating for at least 10 min in a row, and may include carrying light weights, riding a bicycle at normal speed, participating in sports, or gardening. Vigorous activities were those that produced a much greater increase than the previous one in the same variables for at least 10 min [41,42,43]. Based on previous studies, weekly PA was measured in METs (unit of measurement for metabolic rate)-min per week (MMS) [41,44]. The MMS was calculated by multiplying the baseline MET values according to intensity (walking = 3.3 METs, moderate PA = 4 METs and vigorous PA = 8 METs) by the minutes and days spent walking, moderate PA and vigorous PA, i.e., MET-min per week: MET level x minutes of activity x events per week. Once these values were obtained, they were added together to find the total PA performed. According to the results, the participants were distributed into 3 activity categories [41,42,43]:
- Low: Participants who did not register activity or did not meet the criteria for moderate and high categories.
- Moderate: Participants who met one of these criteria:
- 3 or more days of vigorous PA for at least 20 min/day
- 5 or more days of moderate PA or walking for at least 30 min
- 5 or more days of any combination of walking, moderate or vigorous PA, achieving at least 600 MMS.
- High: Participants who met one of the following criteria:
- 3 or more days of vigorous PA or accumulating at least 1500 MMS
- 7 or more days of any combination of walking, moderate or vigorous PA, achieving a minimum of at least 3000 MMS.
2.3. Statistical Analysis
We calculated descriptive measures for all variables of interest by calculating counts (n) and proportions (%) for qualitative variables and by calculating means (m) and standard deviation (SD) for quantitative variables. The Kolmogorov–Smirnov test was used to test for data normality. The chi-square test (χ2) was used to compare categorical variables between groups. For quantitative variables, a Pearson’s correlation analysis (r) was performed. To control for the influence of sex and age, partial correlations were performed. The consumption of medications levels threshold that best discriminated the mental health vulnerability, depression, anxiety and multimorbidity was determined by using the receiver operating characteristic (ROC) curve. We generated multivariable logistic regression models to assess factors independently associated with a low level of PA. The Wald statistic was used, in which variables with p ≥ 0.15 were eliminated from the model. Unadjusted and adjusted odds ratios (ORs) were calculated with 95% confidence intervals. In addition, sex-stratified multivariable logistic regression models for low level of PA were calculated. All of the contrasts of hypotheses were bilateral and statistical significance was established at p < 0.05.
Data were analyzed using IBM SPSS Statistic v.24.0 (IBM Corp. Armonk, NY, USA), licensed by the University of Castilla La-Mancha.
3. Results
The total sample was 5977 pre-elderly (age between 50 and 64 years old), including 51.9% women and 48.1% men, with a mean age of 56.79 years (SD ± 4.31). Table 1 shows the characteristics of the sample by sex. Most of the participants were married (66.4%), had primary education (47.6%), and belonged to social class V (32.3%). The majority had no mental disease with an average score of 1.48 (SD ± 2.74) in GHQ-12. Overall, 51.8% of pre-elderly people perceived their health status as good, although 74.6% had a disease or chronic/long-term illness, 61.4% morbidity and 41.5 were overweight. The mean medication consumption was 1.84 (SD ± 1.89) and 10.1% present polypharmacy (≥5 medications consumed in the last 2 weeks). In total, 44.1% had a moderate level of PA.

Table 1.
Sociodemographic characteristics of Spanish pre-elderly (age between 50 and 64 years old) (n = 5977).
The prevalence of the different groups of medications consumed in the last 2 weeks by the pre-elderly is shown in Figure 1. The most commonly consumed medications in the Spanish pre-elderly were those for pain (34.8%) blood pressure (24.8%) and cholesterol (20.1%). Regarding the consumption of medicines for possible mental disorders, 15% consumed tranquilizers, relaxants or sleeping pills and 7.9% consumed anti-depressants.
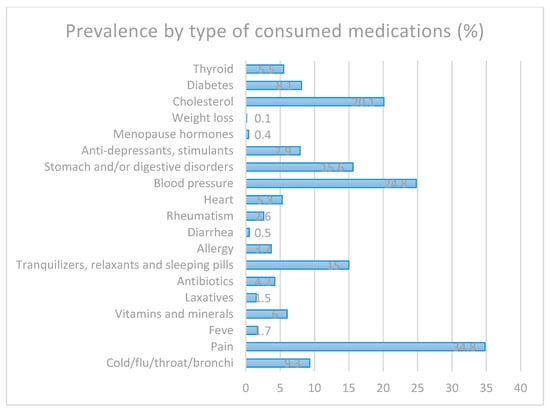
Figure 1.
Prevalence of the different groups of medications consumed by the Spanish pre-elderly.
Pre-elderly individuals who had low levels of PA consumed more drugs, as did people who had a case of mental health vulnerability or multimorbidity (p < 0.001). Figure 2 shows the ROC curve for cases of mental health vulnerability (Figure 2a) [area under the curve (AUC) = 0.775, 95% CI = 0.734–0.776; p < 0.001, the cut-off point was 1.5 drugs (sensitivity = 0.669, 1-specificity = 0.423)], depression in the last 12 months (Figure 2b) [AUC = 0.835, 95% CI = 0.818–0.853; p < 0.001, the cut-off point was 2.5 drugs (sensitivity = 0.755, 1-specificity = 0.233)], anxiety in the last 12 months (Figure 2c) [AUC = 0.803, 95% CI = 0.784–0.821; p < 0.001, the cut-off point was 1.5 drugs (sensitivity = 0.867, 1-specificity = 0.415)] and multimorbidity (Figure 2d) [AUC = 0.825, 95% CI = 0.815–0.835; p < 0.001, the cut-off point was 1.5 drugs (sensitivity = 0.669, 1-specificity = 0.127)] predicted by the number of medications consumed in the last 2 weeks.
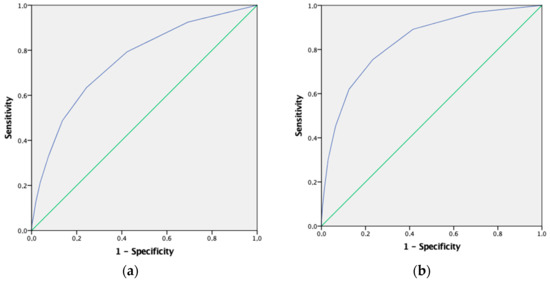
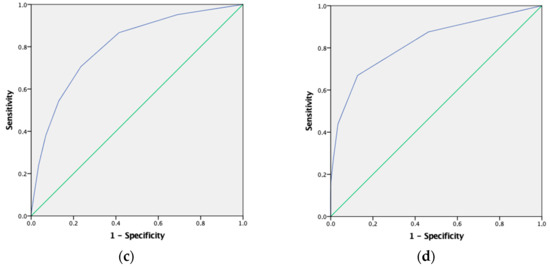
Figure 2.
ROC curve that summarizes the potential of the number of medications consumed in the last 2 weeks to identify cases of mental health vulnerability (a) depression in the last 12 months (b), anxiety in the last 12 months (c) and multimorbidity (d).
Table 2 shows the bivariate correlations and partial correlations between GHQ-12 score with MMS, the number of diseases (multimorbidity levels) and the number of medications consumed in the last 2 weeks. The GHQ-12 score was positively associated with the number of diseases and number of medications consumed. However, the GHQ-12 score was negatively associated with MMS. All of the correlations remained after adjusting for sex and age.

Table 2.
Bivariate correlations between GHQ-12 score with MMS, the number of diseases and number of medications consumed in the last 2 weeks.
Table 3 shows the sociodemographic characteristics of the participants by level of PA. All variables were significant when related to PA levels. Pre-elderly who had a mental disorder such as anxiety or depression had lower levels of PA (p < 0.001). The average score in GH1-12 of people who had low levels of PA was 2.03 (DS ± 3.28) unlike the 0.88 (DS ± 1.87) of people who had high levels of PA (p < 0.001). Similarly, people with polypharmacy showed lower levels of PA (p < 0.001). In fact, the average number of drugs consumed by people who had low levels of PA was 2.09 (DS ± 2.03) unlike the 1.83 (DS ± 1.88) reported for people who had high levels of PA (p < 0.001).

Table 3.
Characteristics of Spanish pre-elderly (age between 50 and 64 years old) by level of physical activity (n = 5.977).
Levels of PA and its relation to depression and anxiety can be seen in Figure 3 (p < 0.001).
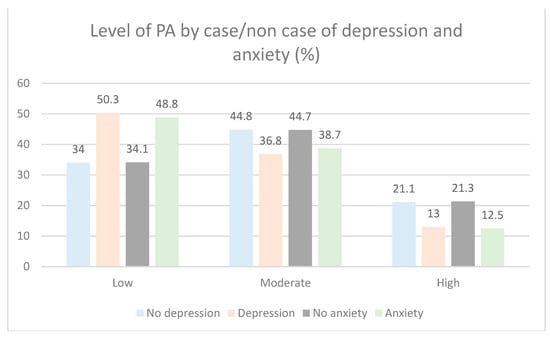
Figure 3.
Distribution of levels of PA at depression and anxiety in Spanish pre-elderly (n = 5977).
In the adjusted logistic regression analysis (Table 4), we observed that low levels of PA were positively associated with being married (adjusted odds ratio = AOR: 1.26, 95% confidence interval = CI: 1.07–1.48, p = 0.005), without studies (AOR: 1.63, 95% CI: 1.26–2.11, p < 0.001), having anxiety (AOR: 1.28, 95% CI: 1.05–1.55, p = 0.014), having mental health vulnerability (AOR: 1.44, 95% CI: 1.18–1.76, p < 0.001), bad/very bad self-perception of their health (AOR: 2.1, 95% CI: 1.72–2.57, p < 0.001) and obesity (AOR: 2.07, 95% CI: 1.18–2.63, p = 0.011). In addition, in sex-stratified analyses (Table 5) among women, belonging to social class V and VI (AOR: 1.28, 95% CI: 1.02–1.61, p = 0.034) and having depression (AOR: 1.42, 95% CI: 1.1–1.84, p = 0.007) were positively associated with low levels of PA.

Table 4.
Logistic regression model for the association between the low level of physical activity and sociodemographic and health characteristics of Spanish pre-elderly.

Table 5.
Logistic regression model for the association between the low level of physical activity and sociodemographic and health characteristics stratified by sex.
4. Discussion
To the best of our knowledge, this is the first study to analyze the relationship between the levels of PA, mental health conditions and the consumption of medications among the Spanish pre-elderly. The main findings were that low levels of PA were associated with mental health vulnerability, anxiety and depression (in case of women). In addition, people with low levels of PA consumed more medications than those with high levels of PA.
From a physiological point of view, the ageing process and advancing chronological age do not occur simultaneously. Ageing can be influenced by multiple factors in combination, including biological ageing, the occurrence of diseases and certain lifestyle patterns, such as a low level of PA [6]. Our results show that higher levels of PA are related to a lower prevalence of multimorbidity (no. of diseases), depression, anxiety and medication consumption. In line with another study carried out in Spain [45], it shows an inverse relationship between the consumption of certain medications for mental problems and levels of PA, and there may be a bidirectional relationship between these medications and PA. The results are in line with other studies indicating that PA confers considerable protection against chronic diseases (diabetes, hypertension and hypercholesterolaemia) as well as mental health problems such as anxiety and depression [3,4,20,21,46]. The practice of PA helps prevent depression where it is stated that performing flexibility exercises could reduce the risk of depression by up to 81% [47]. These results are in line with those obtained in the present study where an inverse relationship between PA and depression can be observed. In addition, the negative relationship found between MMS and medication consumption confirms how regular PA practice could reduce drug consumption, as in other studies [22].
The highest percentage of medications consumed was for cholesterol, blood pressure and pain, the consumption of which can be reduced through PA. A systematic review of randomized clinical trials showed that PA is an intervention with few adverse effects that reduces pain, provides physical and mental health benefits and improves quality of life [48]. Therefore, it can be said that a high level of PA, in addition to improving diseases, could reduce the consumption of medications and is associated with better overall health [6,22,46,49].
The WHO recommends undertaking at least 150 min of moderate PA, 75 min of vigorous PA or a combination of both every week, which corresponds to a moderate level of PA in our study [50]. However, our results show that more than a third of our population did not achieve these levels. This is a problem because PA can reduce the symptoms of depression and anxiety [49,50], a current issue in our society. This age range is important because it is on the verge of aging; therefore, the PA habits at this age are those that precede aging. In our study, it has been observed that PA levels are not met in this age range, as in the study by Biertnat et al. [25], where it was shown that people in this age range and retirees are the ones who undertake less PA. In our study, moderate levels of PA were lower than other study carried out with older people in Spain [41]. Moderate levels of PA should become a common habit in order to break the vicious circle of a sedentary lifestyle, obesity, depression, anxiety and incapacity [6]. Adequate levels of PA may improve mental health status [51]. According to the results obtained in the present study, it has been shown that PA has a positive influence on the prevention of depression, showing that if adults of this age range performed at least 1 h of exercise a week, new cases of depression could be prevented by up to 12% [52]. To achieve this, several systematic reviews show that eHealth interventions (such as interactive websites, smartphone applications, etc.) are effective in increasing PA levels in adults aged over 50 years [53,54]. The barriers that have been found to promote active aging have been described as a lack of time, organizational restrictions, limitations of being referred to adequate services, a lack of interest and support in prevention by administrators, a lack of incentives to participate, a lack of financial resources, too few personnel, and a lack of transportation, among others [5].
Furthermore, in line with previous studies, our results show that low levels of PA are related to being married [55], having a low educational level [14,24,56], anxiety [6,17], depression (in women) [6,14], low social class (in women) [55], worse self-perception of health status [14,21] and obesity [24,55]. In fact, a low educational level accompanied by a low socio-economic status (social classes V and VI) has been associated with a higher prevalence of obesity [24,55]. Therefore, understanding these factors is of particular interest when designing health policies aimed at promoting PA, especially in people with a lower level of PA.
Our results show a strong association between the number of diseases and drug consumption, which might seem obvious [23]. Nevertheless, in our logistic adjusted regression model, multimorbidity and disease or chronic/long-term illnesses were not associated with low levels of PA. Other studies have shown that physical function is related to the development and worsening of multimorbidity over time [57]. In high-income countries, the greatest increase in the prevalence of multimorbidity is recorded in two periods: between 50 and 60 years of age, and in old age [35], coinciding with the age of our participants. However, in agreement with another study, it appears that chronic disease is not the reason for the lower levels of PA observed [14,58]. On the contrary, self-perception of health status plays a more important role in low levels of PA than the mere presence of disease [14].
Finally, this study has some limitations. First, as it was a cross-sectional study, it was not possible to determine the causal direction between the associations found. Second, the measurement of PA levels and anthropometric data are self-reported and without objective measures. However, the present study has great strengths because the data were obtained from a national representative survey with a large number of participants and represents a step towards gaining knowledge of this problem in today’s society.
5. Conclusions
In conclusion, the Spanish pre-elderly do not reach the levels of PA recommended by the WHO. Low levels of PA were associated with being married, low educational levels, mental health vulnerability, anxiety and depression (in women), poor self-perception of health and low social class (in women). In addition, people with a low level of PA consumed more medications and had higher multimorbidity. The GHQ-12 score was positively associated with the number of diseases and number of medications consumed, and GHQ-12 score was negatively associated with MMS.
It is important that people reach old age with an optimal health status in order to reduce age-related disability and morbidity; this is possible with adequate levels of PA from earlier ages, such as pre-aging. Knowing the variables associated with low levels of PA allows us to direct health policies towards this population in order to improve their PA levels. Taking into account these variables, PA programs should be incorporated in the pre-elderly stage as this can prevent disease, reduce the consumption of medication and improve mental health, thus reducing visits to health services and the healthcare expenditure associated with the ageing of the population.
Author Contributions
Conceptualization, J.M.C.-T. and J.A.L.-A.; methodology, A.I.C.-C., J.M.C.-T. and J.A.L.-A.; software, J.M.C.-T.; validation, A.I.C.-C., J.M.C.-T. and J.A.L.-A.; formal analysis, J.M.C.-T.; investigation, J.M.C.-T., A.I.C.-C., D.P.P.-C., J.A.P.-M., P.Á.L.-R. and J.A.L.-A.; data curation, J.M.C.-T. and J.A.L.-A.; writing—original draft preparation, J.A.L.-A. and J.M.C.-T.; writing—review and editing, J.M.C.-T., A.I.C.-C., D.P.P.-C., J.A.P.-M., P.Á.L.-R. and J.A.L.-A.; visualization, J.M.C.-T., A.I.C.-C., D.P.P.-C., J.A.P.-M., P.Á.L.-R. and J.A.L.-A.; supervision, J.M.C.-T., A.I.C.-C., D.P.P.-C., J.A.P.-M., P.Á.L.-R. and J.A.L.-A.; project administration, J.M.C.-T. and J.A.L.-A.; funding acquisition, J.A.L.-A., J.M.C.-T. and A.I.C.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by a grant from the European Regional Development Fund (ERDF) [Fondo Europeo de Desarrollo Regional (FEDER) (DOCM 19/02/20)].
Institutional Review Board Statement
As we used public anonymized secondary data from the Instituto Nacional de Estadística, the approval of an ethics committee was not necessary, according to Spanish legislation.
Informed Consent Statement
Not applicable.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176783&menu=resultados&secc=1254736195295&idp=1254735573175#!tabs-1254736195295.
Acknowledgments
We are grateful to NHI of Spain (www.ine.es) and the Ministry of Health, Social Services and Equality of Spain (www.mscbs.gob.es/) for providing data for this study. We thank all participants and coordinators from the NHSS 2017.
Conflicts of Interest
The authors declare no conflict of interest.
References
- United Nations, Departement of Economic and Social Affairs, Population Division. World Population Ageing 2019–Highlights (ST/ESA/SER.A/430); United Nations: New York, NY, USA, 2019. [Google Scholar]
- Carmona-Torres, J.M.; Rodríguez-Borrego, M.A.; Laredo-Aguilera, J.A.; López-Soto, P.J.; Santacruz-Salas, E.; Cobo-Cuenca, A.I. Disability for basic and instrumental activities of daily living in older individuals. PLoS ONE 2019, 14, e0220157. [Google Scholar] [CrossRef]
- Olanrewaju, O.; Kelly, S.; Cowan, A.; Brayne, C.; Lafortune, L. Physical activity in community dwelling older people: A systematic review of reviews of interventions and context. PLoS ONE 2016, 11, e0168614. [Google Scholar] [CrossRef]
- Martina, M.; Ara, M.A.; Gutiérrez, C.; Nolberto, V.; Piscoya, J. Depression and associated factors in the Peruvian elderly population according to ENDES 2014-2015. An. Fac. Med. 2018, 78, 393. [Google Scholar] [CrossRef]
- Kenbubpha, K.; Higgins, I.; Chan, S.W.-C.; Wilson, A. Promoting active ageing in older people with mental disorders living in the community: An integrative review. Int. J. Nurs. Pract. 2018, 24, e12624. [Google Scholar] [CrossRef]
- de Oliveira, L.D.S.S.C.B.; Souza, E.C.; Rodrigues, R.A.S.; Fett, C.A.; Piva, A.B. The effects of physical activity on anxiety, depression, and quality of life in elderly people living in the community. Trends Psychiatry Psychother. 2019, 41, 36–42. [Google Scholar] [CrossRef]
- Kok, R.M.; Reynolds, C.F. Management of depression in older adults: A review. JAMA J. Am. Med. Assoc. 2017, 317, 2114–2122. [Google Scholar] [CrossRef]
- World Health Organization. Depression: Evidence-Based Recommendations for Management of Depression in Non-Specialized Health Settings. Available online: https://www.who.int/mental_health/mhgap/evidence/depression/en/ (accessed on 22 November 2020).
- Cooney, G.M.; Dwan, K.; Greig, C.A.; Lawlor, D.A.; Rimer, J.; Waugh, F.R.; McMurdo, M.; Mead, G.E. Exercise for depression. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef]
- Marcum, Z.A.; Perera, S.; Thorpe, J.M.; Switzer, G.E.; Castle, N.G.; Strotmeyer, E.S.; Simonsick, E.M.; Ayonayon, H.N.; Phillips, C.L.; Rubin, S.; et al. Antidepressant Use and Recurrent Falls in Community-Dwelling Older Adults: Findings From the Health ABC Study. Ann. Pharmacother. 2016, 50, 525–533. [Google Scholar] [CrossRef]
- De Vries, Y.A.; De Jonge, P.; Van Den Heuvel, E.; Turner, E.H.; Roest, A.M. Influence of baseline severity on antidepressant efficacy for anxiety disorders: Meta-analysis and meta-regression. Br. J. Psychiatry 2016, 208, 515–521. [Google Scholar] [CrossRef]
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Hallgren, M.; Stubbs, B.; Vancampfort, D.; Lundin, A.; Jääkallio, P.; Forsell, Y. Treatment guidelines for depression: Greater emphasis on physical activity is needed. Eur. Psychiatry 2017, 40, 1–3. [Google Scholar] [CrossRef]
- Souza, A.M.R.; Fillenbaum, G.G.; Blay, S.L. Prevalence and Correlates of Physical Inactivity among Older Adults in Rio Grande do Sul, Brazil. PLoS ONE 2015, 10, e0117060. [Google Scholar] [CrossRef]
- WHO. Global Recommendations on Physical Activity for Health. Available online: https://www.who.int/dietphysicalactivity/publications/9789241599979/en/ (accessed on 14 July 2020).
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; De Leon, A.P.; Dunn, A.L.; Deslandes, A.C.; et al. Physical activity and incident depression: A meta-analysis of prospective cohort studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef]
- Stubbs, B.; Vancampfort, D.; Rosenbaum, S.; Firth, J.; Cosco, T.; Veronese, N.; Salum, G.A.; Schuch, F.B. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: A meta-analysis. Psychiatry Res. 2017, 249, 102–108. [Google Scholar] [CrossRef]
- Crevenna, R.; Dorner, T.E. Association between fulfilling the recommendations for health-enhancing physical activity with (instrumental) activities of daily living in older Austrians. Wien. Klin. Wochenschr. 2019, 131, 265–272. [Google Scholar] [CrossRef]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef]
- Soares-Miranda, L.; Siscovick, D.S.; Psaty, B.M.; Longstreth, W.T.; Mozaffarian, D. Physical Activity and Risk of Coronary Heart Disease and Stroke in Older Adults. Circulation 2016, 133, 147–155. [Google Scholar] [CrossRef]
- Latorre-Román, P.Á.; Carmona-Torres, J.M.; Cobo-Cuenca, A.I.; Laredo-Aguilera, J.A. Physical activity, ability to walk, weight status, and multimorbidity levels in older spanish people: The National Health Survey (2009–2017). Int. J. Environ. Res. Public Health 2020, 17, 4333. [Google Scholar] [CrossRef]
- Moral-García, J.E.; González-Palomares, A.; García-Cantó, E.; Tárrega-López, P.J. Risk of dependence and self-esteem in elderly people according to physical activity and drug consumption. Rev. Esp. Salud Publica 2020, 94, e202008091. [Google Scholar]
- Carmona-Torres, J.M.; Cobo-Cuenca, A.I.; Recio-Andrade, B.; Laredo-Aguilera, J.A.; Martins, M.M.; Rodríguez-Borrego, M.A. Prevalence and factors associated with polypharmacy in the older people: 2006–2014. J. Clin. Nurs. 2018, 27. [Google Scholar] [CrossRef]
- Fernandez-Navarro, P.; Aragones, M.T.; Ley, V. Leisure-time physical activity and prevalence of non-communicable pathologies and prescription medication in Spain. PLoS ONE 2018, 13, e0191542. [Google Scholar] [CrossRef]
- Biernat, E.; Piatkowska, M. Stay active for life: Physical activity across life stages. Clin. Interv. Aging 2018, 13, 1341–1352. [Google Scholar] [CrossRef]
- Razzak, Z.A.; Khan, A.A.; Farooqui, S.I. Effect of aerobic and anaerobic exercise on estrogen level, fat mass, and muscle mass among postmenopausal osteoporotic females. Int. J. Health Sci. 2019, 13, 10–16. [Google Scholar]
- Asikainen, T.M.; Kukkonen-Harjula, K.; Miilunpalo, S. Exercise for health for early postmenopausal women: A systematic review of randomised controlled trials. Sports Med. 2004, 34, 753–778. [Google Scholar] [CrossRef]
- Hobbs, N.; Godfrey, A.; Lara, J.; Errington, L.; Meyer, T.D.; Rochester, L.; White, M.; Mathers, J.C.; Sniehotta, F.F. Are behavioral interventions effective in increasing physical activity at 12 to 36 months in adults aged 55 to 70 years? A systematic review and meta-analysis. BMC Med. 2013, 11, 75. [Google Scholar] [CrossRef]
- Consejo Superior de Deportes Plan Integral Para la Actividad Física y el Deporte. Plan A+D. Available online: http://www.planamasd.es/programas/mayores/objetivos.html (accessed on 21 January 2021).
- Lee, H.Y.; Kondo, N.; Oh, J. Medical expenditure and unmet need of the pre-elderly and the elderly according to job status in Korea: Are the elderly indeed most vulnerable? PLoS ONE 2018, 13. [Google Scholar] [CrossRef]
- Bani, N.A.; Hassan, M.Z.; Kaidi, H.M.; Hashim, N.F.M.; Dziyauddin, R.A.; Musa, R.; Suhot, M.A.; Usman, S.; Muhammad-Sukki, F.; Abu-Bakar, S.H.; et al. Assessment of Health Status of the Elderly and Pre-elderly at a Malaysia Elderly Care Centre. Int. J. Integr. Eng. 2018, 10. [Google Scholar] [CrossRef]
- Manjavong, M.; Limpawattana, P.; Mairiang, P.; Anutrakulchai, S. Prevalence of insomnia and related impact. Int. J. Psychiatry Med. 2016, 51, 544–553. [Google Scholar] [CrossRef]
- Ministerio de Sanidad Servicios Sociales e Igualdad; Instituto Nacional de Estadística. National Health Survey in Spain NHSS 2017; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2018. [Google Scholar]
- Domingo-Salvany, A.; Bacigalupe, A.; Carrasco, J.M.; Espelt, A.; Ferrando, J.; Borrell, C. Propuestas de clase social neoweberiana y neomarxista a partir de la Clasificación Nacional de Ocupaciones 2011. Gac. Sanit. 2013, 27, 263–272. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health. Available online: http://www.who.int/ageing/publications/world-report-2015/en/ (accessed on 23 January 2020).
- WHO. Diet, Nutrition and the Prevention of Chronic Diseases; World Health Organization: Geneva, Switzerland, 2003; Volume 916. [Google Scholar]
- World Health Organization. Medication Safety in Polypharmacy (No. WHO/UHC/SDS/2019.11); World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Sánchez-López, M.P.; Dresch, V. The 12-Item General Health Questionnaire (GHQ-12): Reliability, External Validity and Factor Structure in the Spanish Population. Psicothema 2008, 20, 839–843. [Google Scholar]
- Rocha, K.B.; Pérez, K.; Rodríguez-Sanz, M.; Borrell, C.; Obiols, J.E. Propiedades psicométricas y valores normativos del General Health Questionnaire (GHQ-12) en población general española. Int. J. Clin. Health Psychol. 2011, 11, 125–139. [Google Scholar]
- Villa, I.C.; Zuluaga Arboleda, C.; Restrepo Roldan, L.F. Psychometric properties of the General health Goldberg GHQ-12 questionnaire applied at a hospital facility in the city of Medellin. Av. Psicol. Latinoam. 2013, 31, 532–545. [Google Scholar]
- Rubio Castañeda, F.J.; Tomas Aznar, C.; Muro Baquero, C. Validity, Reliability and Associated Factors of the International Physical Activity Questionnaire Adapted to Elderly (IPAQ-E). Rev. Esp. Salud Pública 2017, 91, 1–12. [Google Scholar]
- The IPAQ Group. International Physical Activity Questionnaire. Available online: https://sites.google.com/site/theipaq/scoring-protocol (accessed on 28 January 2020).
- Mantilla Toloza, S.C.; Gómez-Conesa, A. El Cuestionario Internacional de Actividad Física. Un instrumento adecuado en el seguimiento de la actividad física poblacional. Rev. Iberoam. Fisioter. Kinesiol. 2007, 10, 48–52. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Perez-Cruzado, D.; Cuesta-Vargas, A.; Vera-Garcia, E.; Mayoral-Cleries, F. Medication and physical activity and physical fitness in severe mental illness. Psychiatry Res. 2018, 267, 19–24. [Google Scholar] [CrossRef]
- Laredo-Aguilera, J.A.; Carmona-Torres, J.M.; García-Pinillos, F.; Latorre-Román, P.Á. Effects of a 10-week functional training programme on pain, mood state, depression, and sleep in healthy older adults. Psychogeriatrics 2018. [Google Scholar] [CrossRef]
- Byeon Relationship between Physical Activity Level and Depression of Elderly People Living Alone. Int. J. Environ. Res. Public Health 2019, 16, 4051. [CrossRef]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 2017, CD011279. [Google Scholar]
- López-Torres Hidalgo, J.; Aguilar Salmerón, L.; Boix Gras, C.; Campos Rosa, M.; Escobar Rabadán, F.; Escolano Vizcaíno, C.; Estellés Belenguer, J.L.; Fernández Martín, J.; Ferrer López, V.; Legido García, A.; et al. Effectiveness of physical exercise in the treatment of depression in older adults as an alternative to antidepressant drugs in primary care. BMC Psychiatry 2019, 19. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Izawa, K.P.; Watanabe, S.; Oka, K.; Hiraki, K.; Morio, Y.; Kasahara, Y.; Osada, N.; Omiya, K.; Shimizu, H. Association between mental health and physical activity in patients with chronic heart failure. Disabil. Rehabil. 2014, 36, 250–254. [Google Scholar] [CrossRef]
- Harvey, S.B.; Overland, S.; Hatch, S.L.; Wessely, S.; Mykletun, A.; Hotopf, M. Exercise and the prevention of depression: Results of the HUNT cohort study. Am. J. Psychiatry 2018, 175, 28–36. [Google Scholar] [CrossRef] [PubMed]
- de Arenas-Arroyo, S.N.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Sequí-Domínguez, I.; Reina-Gutiérrez, S.; Martínez-Vizcaíno, V. Effect of eHealth to increase physical activity in healthy adults over 55 years: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2020, sms.13903. [Google Scholar] [CrossRef] [PubMed]
- Kwan, R.Y.C.; Salihu, D.; Lee, P.H.; Tse, M.; Cheung, D.S.K.; Roopsawang, I.; Choi, K.S. The effect of e-health interventions promoting physical activity in older people: A systematic review and meta-analysis. Eur. Rev. Aging Phys. Act. 2020, 17, 7. [Google Scholar] [CrossRef] [PubMed]
- Laredo-Aguilera, J.A.; Cobo-Cuenca, A.I.; Santacruz-Salas, E.; Martins, M.M.; Rodríguez-Borrego, M.A.; López-Soto, P.J.; Carmona-Torres, J.M. Levels of physical activity, obesity and related factors in young adults aged 18–30 during 2009–2017. Int. J. Environ. Res. Public Health 2019, 16. [Google Scholar] [CrossRef]
- Marques, A.; Sarmento, H.; Martins, J.; Saboga Nunes, L. Prevalence of physical activity in European adults–Compliance with the World Health Organization’s physical activity guidelines. Prev. Med. 2015, 81, 333–338. [Google Scholar] [CrossRef]
- Ryan, A.; Murphy, C.; Boland, F.; Galvin, R.; Smith, S.M. What is the impact of physical activity and physical function on the development of multimorbidity in older adults over time? A population-based cohort study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018. [Google Scholar] [CrossRef]
- Dogra, S. Better self-perceived health is associated with lower odds of physical inactivity in older adults with chronic disease. J. Aging Phys. Act. 2011, 19, 322–335. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).