Comparison of Effects of N95 Respirators and Surgical Masks to Physiological and Psychological Health among Healthcare Workers: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Demographic Characteristics of Healthcare Workers
2.4. Measurement of Physiological Parameters
2.5. Symptoms Evaluation after Wearing Facemasks
2.6. Statistical Analysis
2.7. Ethics
3. Results
3.1. Physiological Data of Healthcare Workers after Wearing N95 Respirators
3.2. Physiological Data of Healthcare Workers after Wearing Surgical Masks
3.3. Physiological Data Comparison of Healthcare Workers between Wearing N95 Respirators and Wearing Surgical Masks
3.4. Symptoms of Healthcare Workers after Wearing N95 Respirators or Surgical Masks
4. Discussion
4.1. Main Finding of This Study
4.2. Facemasks for Healthcare Workers
4.3. Comparison with Other Literature Studies
4.4. Strength of This Study
4.5. Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 15 September 2020).
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus—Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Chughtai, A.A.; Seale, H.; MacIntyre, C.R. Availability, consistency and evidence-base of policies and guidelines on the use of mask and respirator to protect hospital health care workers: A global analysis. BMC Res. Notes 2013, 6, 216. [Google Scholar] [CrossRef] [Green Version]
- National Institute for Occupational Safety and Health (NIOSH). Workplace Safety and Health Topics: Aerosols; US Centers for Disease Control and Prevention: Atlanta, GA, USA, 2010. Available online: www.cdc.gov/niosh/topics/aerosols/ (accessed on 10 December 2014).
- Centers for Disease Control and Prevention (CDC). COVID-19 Transmission 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prepare/transmission.html (accessed on 15 March 2020).
- The National Personal Protective Technology Laboratory (NPPTL). Respirator Trusted Source Information. 26 January 2018. Available online: https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/respsource3healthcare.html (accessed on 17 March 2020).
- World Health Organization (WHO). Rational Use of Personal Protective Equipment for Coronavirus Disease 2019 (COVID-19). 27 February 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf (accessed on 17 March 2020).
- Public Health Agency of Canada (PHAC). Coronavirus Disease (COVID-19): For Health Professionals. Available online: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals.html#i (accessed on 18 March 2020).
- Centers for Disease Control and Prevention (CDC). Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. 10 March 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html (accessed on 17 March 2020).
- European Centre for Disease Prevention and Control. Guidance for Wearing and Removing Personal Protective Equipment in Healthcare Settings for the Care of Patients with Suspected or Confirmed COVID-February 2020. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-guidance-wearing-and-removing-personal-protective-equipment-healthcare-settings-updated.pdf (accessed on 17 March 2020).
- Scheid, J.L.; Lupien, S.P.; Ford, G.S.; West, S.L. Commentary: Physiological and Psychological Impact of Face Mask Usage during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 6655. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.C.H.; Seet, R.C.S.; Lee, K.-H.; Wilder-Smith, E.; Chuah, B.Y.S.; Ong, B.K.C. Headaches and the N95 face-mask amongst healthcare providers. Acta Neurol. Scand. 2006, 113, 199–202. [Google Scholar] [CrossRef]
- Ong, J.J.; Bharatendu, C.; Goh, Y.; Tang, J.Z.; Sooi, K.W.; Tan, Y.L.; Tan, B.Y.; Teoh, H.; Ong, S.T.; Allen, D.M.; et al. Headaches Associated with Personal Protective Equipment—A Cross-Sectional Study Among Frontline Healthcare Workers during COVID-19. Headache J. Head Face Pain 2020, 60, 864–877. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rebmann, T.; Carrico, R.; Wang, J. Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. Am. J. Infect. Control 2013, 41, 1218–1223. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Vemuganti, R. Mechanisms of Parkinson’s disease-related proteins in mediating secondary brain damage after cerebral ischemia. Br. J. Pharmacol. 2017, 37, 1910–1926. [Google Scholar] [CrossRef] [Green Version]
- Smith, J.D.; MacDougall, C.C.; Johnstone, J.; Copes, R.A.; Schwartz, B.; Garber, G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: A systematic review and meta-analysis. Can. Med. Assoc. J. 2016, 188, 567–574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Health Topics/Coronavirus Disease (COVID-19)/Symptoms. Available online: https://www.who.int/health-topics/coronavirus (accessed on 5 July 2021).
- Smulyan, H.; Safar, M.E. Blood Pressure Measurement: Retrospective and Prospective Views. Am. J. Hypertens. 2011, 24, 628–634. [Google Scholar] [CrossRef]
- Apparatus for Obtaining and Electronically Interpreting Digital Images of Liquids, Solids and Combinations on Liquids and Solids. 2020. Available online: https://patents.google.com/patent/US7728873B2/en (accessed on 5 July 2021).
- Optical Sensor Device and Image Processing Unit for Measuring Chemical Concentrations, Chemical Saturations and Biophysical Parameters. 2012. Available online: https://patents.google.com/patent/US9402546B2/un (accessed on 5 July 2021).
- Finger Deployed Device for Measuring Blood and Physiological Characteristics. Available online: https://patents.google.com/patent/CN101721215A/en (accessed on 5 July 2021).
- Segman, Y.J. New Method for Computing Optical Hemodynamic Blood Pressure. J. Clin. Exp. Cardiol. 2016, 7, 12. [Google Scholar] [CrossRef] [Green Version]
- Yannan, F. Case study for two non-invasive devices measuring hemoglobin. J. Clin. Med. Case Study 2017, 2, 1–4. [Google Scholar]
- Segman, Y.J.; Trahtemberg, U. Oximeter behavior while using a tourniquet. J. Clin. Exp. Cardiol. 2016, 7, 480. [Google Scholar] [CrossRef] [Green Version]
- Vainshelboim, B. Retracted: Facemasks in the COVID-19 era: A health hypothesis. Med. Hypotheses. 2020, 146, 110411. [Google Scholar] [CrossRef]
- Taiwan Centers for Disease Control. Diseases and Conditions/Important Diseases/Coronavirus Disease 2019(COVID-19)/Press Releases/2021-05-15. Available online: https://www.cdc.gov.tw/En/Bulletin/Detail/R1K7gSjoYa7Wojk54nW7fg?typeid=158 (accessed on 15 May 2021).
- World Health Organization (WHO). Shortage of Personal Protective Equipment Endangering Health Workers Worldwide. 2020. Available online: https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed on 15 March 2020).
- Kao, T.W.; Huang, K.C.; Huang, Y.L.; Tsai, T.J.; Hsieh, B.S.; Wu, M.S. The Physiological Impact of Wearing an N95 Mask during Hemo-Dialysis as a Precaution against SARS in Patients with End-Stage Renal Disease. J. Formos. Med. Assoc. 2004, 103, 624–628. Available online: https://www.ncbi.nlm.nih.gov/pubmed/15340662 (accessed on 6 July 2021).
- Shein, S.L.; Whitticar, S.; Mascho, K.K.; Pace, E.; Speicher, R.; Deakins, K. The effects of wearing facemasks on oxygenation and ventilation at rest and during physical activity. PLoS ONE 2021, 16, e0247414. [Google Scholar] [CrossRef] [PubMed]
- Roberge, R.J.; Coca, A.; Williams, W.J.; Powell, J.B.; Palmiero, A.J. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir. Care 2010, 55, 569–577. [Google Scholar] [PubMed]
- Bharatendu, C.; Ong, J.J.; Goh, Y.; Tan, B.Y.; Chan, A.C.; Tang, J.Z.; Leow, A.S.; Chin, A.; Sooi, K.W.; Tan, Y.L.; et al. Powered Air Purifying Respirator (PAPR) restores the N95 face mask induced cerebral hemodynamic alterations among Healthcare Workers during COVID-19 Outbreak. J. Neurol. Sci. 2020, 417, 117078. [Google Scholar] [CrossRef]
- Rhee, M.S.M.; Lindquist, C.D.; Silvestrini, M.T.; Chan, A.C.; Ong, J.J.Y.; Sharma, V.K. Carbon dioxide increases with face masks but remains below short-term NIOSH limits. BMC Infect. Dis. 2021, 21, 354. [Google Scholar] [CrossRef]
- Özdemir, L.; Azizoğlu, M.; Yapıcı, D. Respirators used by healthcare workers due to the COVID-19 outbreak increase end-tidal carbon dioxide and fractional inspired carbon dioxide pressure. J. Clin. Anesth. 2020, 66, 109901. [Google Scholar] [CrossRef]
- Fletcher, S.J.; Clark, M.; Stanley, P.J. Carbon dioxide re-breathing with close fitting face respirator masks. Anaesthesia 2006, 61, 910. [Google Scholar] [CrossRef]
- Ross, R.M.; Corry, D.B. Software for interpreting cardiopulmonary exercise tests. BMC Pulm. Med. 2007, 7, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician’s Guide to Cardiopulmonary Exercise Testing in Adults: A scientific statement from the American Heart Association. Circulation. Circulation 2010, 122, 191–225. [Google Scholar] [CrossRef] [Green Version]
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and Health: Psychological, Behavioral, and Biological Determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607–628. [Google Scholar] [CrossRef] [Green Version]
- Thoits, P.A. Stress and Health: Major Findings and Policy Implications. J. Health Soc. Behav. 2010, 51, S41–S53. [Google Scholar] [CrossRef] [Green Version]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef] [PubMed]
- Das, R.; Yunus, M.; Deb, P.; Bhattacharyya, P. Significant physiological impact of wearing PPE inside operation theatre: A challenging scenario in this COVID-19 pandemic. J. Fam. Med. Prim. Care 2021, 10, 561–563. [Google Scholar] [CrossRef] [PubMed]
| Subject | N95 Respirator (n = 34) Mean ± SD or n (%) | Surgical Mask (n = 34) Mean ± SD or n (%) | p-Value |
|---|---|---|---|
| Age (years) | 41.2 ± 8.5 | 40.2 ± 8.4 | 0.595 |
| Sex | 0.567 | ||
| Male | 27 (79%) | 25 (74%) | |
| Female | 7 (21%) | 9 (26%) | |
| Role in healthcare | 0.417 | ||
| Nurse | 26 (76%) | 23 (68%) | |
| Doctor | 8 (24%) | 11 (32%) | |
| Duty of work | <0.001 | ||
| Triage station | 10 (29%) | 5 (15%) | |
| Visiting zone | 2 (6%) | 21 (62%) | |
| Critical zone | 22 (65%) | 8 (23%) |
| N95 Respirator (n = 34) | Surgical Mask (n = 34) | N95 Respirator vs. Surgical Mask | |||||||
|---|---|---|---|---|---|---|---|---|---|
| LS-Means (SE) | Change from Baseline LS-Means (SE) | † p-Value | LS-Means (SE) | Change from Baseline LS-Means (SE) | † p-Value | * Adjusted Difference of LS-Means (SE; 95% CI) | † p-Value | ‡ P-for-Interaction | |
| § SpO2 | |||||||||
| Baseline | 96.59 (0.13) | Reference | 96.79 (0.14) | Reference | Reference | ||||
| 2 h | 96.82 (0.15) | 0.24 (0.17) | 0.1708 | 97.03 (0.16) | 0.24 (0.19) | 0.2066 | 0.00 (0.25; −0.50 to 0.50) | 1.0000 | |
| 4 h | 96.97 (0.17) | 0.38 (0.17) | 0.0258 | 96.85 (0.15) | 0.06 (0.17) | 0.7312 | 0.32 (0.24; −0.15 to 0.80) | 0.1819 | |
| 6 h | 96.62 (0.11) | 0.03 (0.13) | 0.8271 | 96.85 (0.14) | 0.06 (0.19) | 0.7515 | −0.03 (0.23; −0.48 to 0.42) | 0.8980 | |
| 8 h | 96.85 (0.16) | 0.26 (0.16) | 0.1038 | 96.76 (0.14) | −0.03 (0.13) | 0.8271 | 0.29 (0.21; −0.12 to 0.71) | 0.1638 | 0.3518 |
| Baseline to 8 h | 0.03 (0.04) | 0.3953 | −0.02 (0.03) | 0.4240 | 0.06 (0.05; −0.04 to 0.15) | 0.2454 | 0.2501 | ||
| ¶ PaO2 | |||||||||
| Baseline | 85.26 (1.11) | Reference | 87.41 (1.30) | Reference | Reference | ||||
| 2 h | 86.79 (1.31) | 1.53 (1.52) | 0.3147 | 88.50 (1.26) | 1.09 (1.52) | 0.4753 | 0.44 (2.15; −3.78 to 4.66) | 0.8377 | |
| 4 h | 88.03 (1.49) | 2.76 (1.40) | 0.0477 | 87.91 (1.39) | 0.50 (1.55) | 0.7478 | 2.26 (2.09; −1.83 to 6.36) | 0.2785 | |
| 6 h | 85.38 (0.94) | 0.12 (1.23) | 0.9238 | 87.26 (1.29) | −0.15 (1.74) | 0.9327 | 0.26 (2.13; −3.92 to 4.44) | 0.9012 | |
| 8 h | 88.09 (1.43) | 2.82 (1.54) | 0.0664 | 86.59 (1.22) | −0.82 (1.20) | 0.4941 | 3.65 (1.95; −0.18 to 7.48) | 0.0619 | 0.3239 |
| Baseline to 8 h | 0.42 (0.34) | 0.2160 | −0.29 (0.28) | 0.3082 | 0.71 (0.44; −0.16 to 1.58) | 0.1090 | 0.1156 | ||
| ‖ PCO2 | |||||||||
| Baseline | 37.09 (0.24) | Reference | 36.76 (0.26) | Reference | Reference | ||||
| 2 h | 36.59 (0.24) | −0.50 (0.30) | 0.0995 | 36.29 (0.27) | −0.47 (0.31) | 0.1245 | −0.03 (0.43; −0.87 to 0.82) | 0.9456 | |
| 4 h | 35.35 (0.98) | −1.74 (0.95) | 0.0673 | 36.65 (0.25) | −0.12 (0.28) | 0.6792 | −1.62 (0.99; −3.57 to 0.32) | 0.1021 | |
| 6 h | 37.00 (0.25) | −0.09 (0.26) | 0.7353 | 36.74 (0.24) | −0.03 (0.36) | 0.9343 | −0.06 (0.44; −0.92 to 0.81) | 0.8941 | |
| 8 h | 36.56 (0.28) | −0.53 (0.29) | 0.0640 | 36.71 (0.26) | −0.06 (0.24) | 0.8082 | −0.47 (0.37; −1.21 to 0.26) | 0.2092 | 0.2940 |
| Baseline to 8 h | −0.06 (0.07) | 0.3373 | 0.03 (0.06) | 0.5618 | −0.10 (0.09; −0.27 to 0.07) | 0.2674 | 0.2717 | ||
| ** SBP | |||||||||
| Baseline | 133.68 (2.37) | Reference | 129.26 (2.19) | Reference | Reference | ||||
| 2 h | 132.21 (2.30) | −1.47 (1.71) | 0.3897 | 131.76 (1.81) | 2.50 (2.04) | 0.2193 | −3.97 (2.66; −9.18 to 1.24) | 0.1352 | |
| 4 h | 130.94 (2.10) | −2.74 (1.73) | 0.1146 | 127.29 (1.59) | −1.97 (1.61) | 0.2199 | −0.76 (2.36; −5.40 to 3.87) | 0.7463 | |
| 6 h | 130.71 (2.51) | −2.97 (2.07) | 0.1513 | 127.97 (2.06) | −1.29 (1.4) | 0.3546 | −1.68 (2.50; −6.57 to 3.22) | 0.5021 | |
| 8 h | 130.53 (2.26) | −3.15 (1.41) | 0.0259 | 129.00 (2.29) | −0.26 (1.70) | 0.8764 | −2.88 (2.21; −7.22 to 1.45) | 0.1926 | 0.5603 |
| Baseline to 8 h | −0.78 (0.34) | 0.0224 | −0.43 (0.39) | 0.2682 | −0.35 (0.52; −1.36 to 0.67) | 0.5034 | 0.5048 | ||
| †† DBP | |||||||||
| Baseline | 83.82 (1.76) | Reference | 80.79 (1.75) | Reference | Reference | ||||
| 2 h | 82.71 (1.82) | −1.12 (1.35) | 0.4078 | 83.53 (1.38) | 2.74 (1.61) | 0.0889 | −3.85 (2.10; −7.97 to 0.26) | 0.0665 | |
| 4 h | 82.06 (1.70) | −1.76 (1.36) | 0.1942 | 79.62 (1.33) | −1.18 (1.51) | 0.4358 | −0.59 (2.03; −4.57 to 3.39) | 0.7722 | |
| 6 h | 82.24 (1.95) | −1.59 (1.46) | 0.2782 | 79.91 (1.49) | −0.88 (1.23) | 0.4737 | −0.71 (1.91; −4.46 to 3.04) | 0.7122 | |
| 8 h | 81.59 (1.64) | −2.24 (1.29) | 0.0820 | 80.56 (1.63) | −0.24 (1.14) | 0.8364 | −2.00 (1.72; −5.37 to 1.37) | 0.2442 | 0.3968 |
| Baseline to 8 h | −0.49 (0.29) | 0.0853 | −0.41 (0.26) | 0.1117 | −0.09 (0.39; −0.84 to 0.67) | 0.8249 | 0.8249 | ||
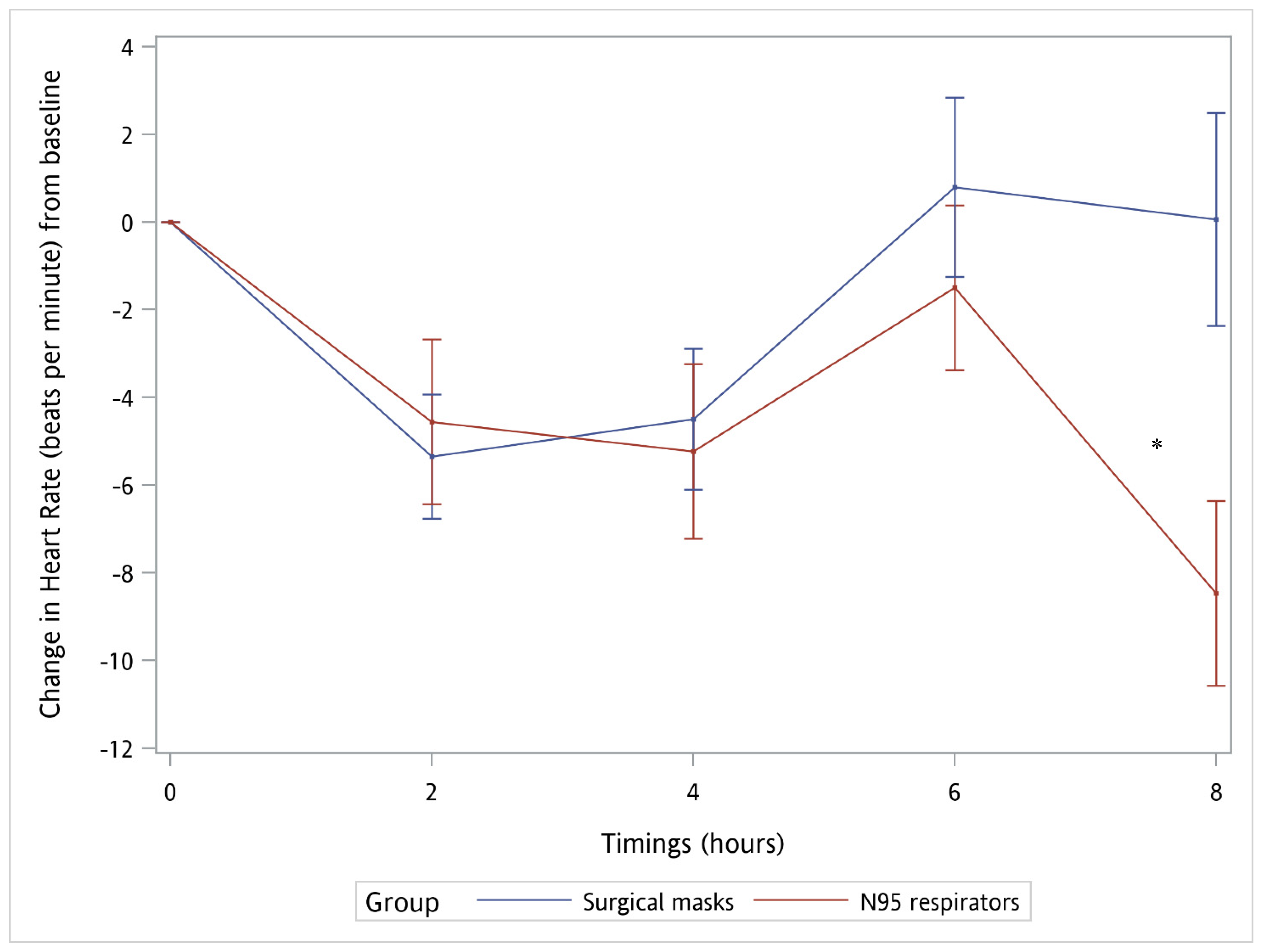
| ‡‡ HR | |||||||||
| Baseline | 88.91 (1.84) | Reference | 85.71 (2.19) | Reference | Reference | ||||
| 2 h | 84.35 (2.04) | −4.56 (1.88) | 0.0152 | 80.35 (2.15) | −5.35 (1.42) | 0.0002 | 0.79 (2.35; −3.82 to 5.41) | 0.7357 | |
| 4 h | 83.68 (2.15) | −5.24 (1.99) | 0.0086 | 81.21 (1.96) | −4.50 (1.61) | 0.0052 | −0.74 (2.56; −5.76 to 4.29) | 0.7741 | |
| 6 h | 87.41 (1.91) | −1.50 (1.88) | 0.4258 | 86.50 (2.26) | 0.79 (2.05) | 0.6983 | −2.29 (2.78; −7.75 to 3.16) | 0.4097 | |
| 8 h | 80.44 (2.14) | −8.47 (2.10) | <0.0001 | 85.76 (2.32) | 0.06 (2.42) | 0.9806 | −8.53 (3.21; −14.82 to −2.24) | 0.0079 | 0.0924 |
| Baseline to 8 h | −1.39 (0.53) | 0.0087 | 0.63 (0.58) | 0.2830 | −2.01 (0.79; −3.56 to −0.47) | 0.0105 | 0.0146 | ||
| Symptoms | N95 Respirator (n = 34) n (%) | Surgical Mask (n = 34) n (%) | p-Value |
|---|---|---|---|
| Shortness of breath | 15 (44%) | 1 (3%) | <0.001 |
| Anxiety | 1 (3%) | 0 | 0.500 |
| Headache | 6 (18%) | 0 | 0.012 |
| Dizziness | 5 (15%) | 0 | 0.027 |
| Difficulty talking | 18 (53%) | 0 | <0.001 |
| Fatigue | 9 (27%) | 0 | 0.001 |
| Depression | 3 (9%) | 0 | 0.119 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, C.-Y.; Peng, C.-Y.; Liu, H.-L.; Yeh, I.-J.; Lee, C.-W. Comparison of Effects of N95 Respirators and Surgical Masks to Physiological and Psychological Health among Healthcare Workers: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 13308. https://doi.org/10.3390/ijerph182413308
Su C-Y, Peng C-Y, Liu H-L, Yeh I-J, Lee C-W. Comparison of Effects of N95 Respirators and Surgical Masks to Physiological and Psychological Health among Healthcare Workers: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(24):13308. https://doi.org/10.3390/ijerph182413308
Chicago/Turabian StyleSu, Che-Yu, Chiung-Yu Peng, Hsin-Liang Liu, I-Jeng Yeh, and Chi-Wei Lee. 2021. "Comparison of Effects of N95 Respirators and Surgical Masks to Physiological and Psychological Health among Healthcare Workers: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 24: 13308. https://doi.org/10.3390/ijerph182413308
APA StyleSu, C.-Y., Peng, C.-Y., Liu, H.-L., Yeh, I.-J., & Lee, C.-W. (2021). Comparison of Effects of N95 Respirators and Surgical Masks to Physiological and Psychological Health among Healthcare Workers: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(24), 13308. https://doi.org/10.3390/ijerph182413308






