Tools for Assessing Cardiovascular Disease Risk Factors in Underserved Young Adult Populations: A Systematic Review
Abstract
1. Introduction
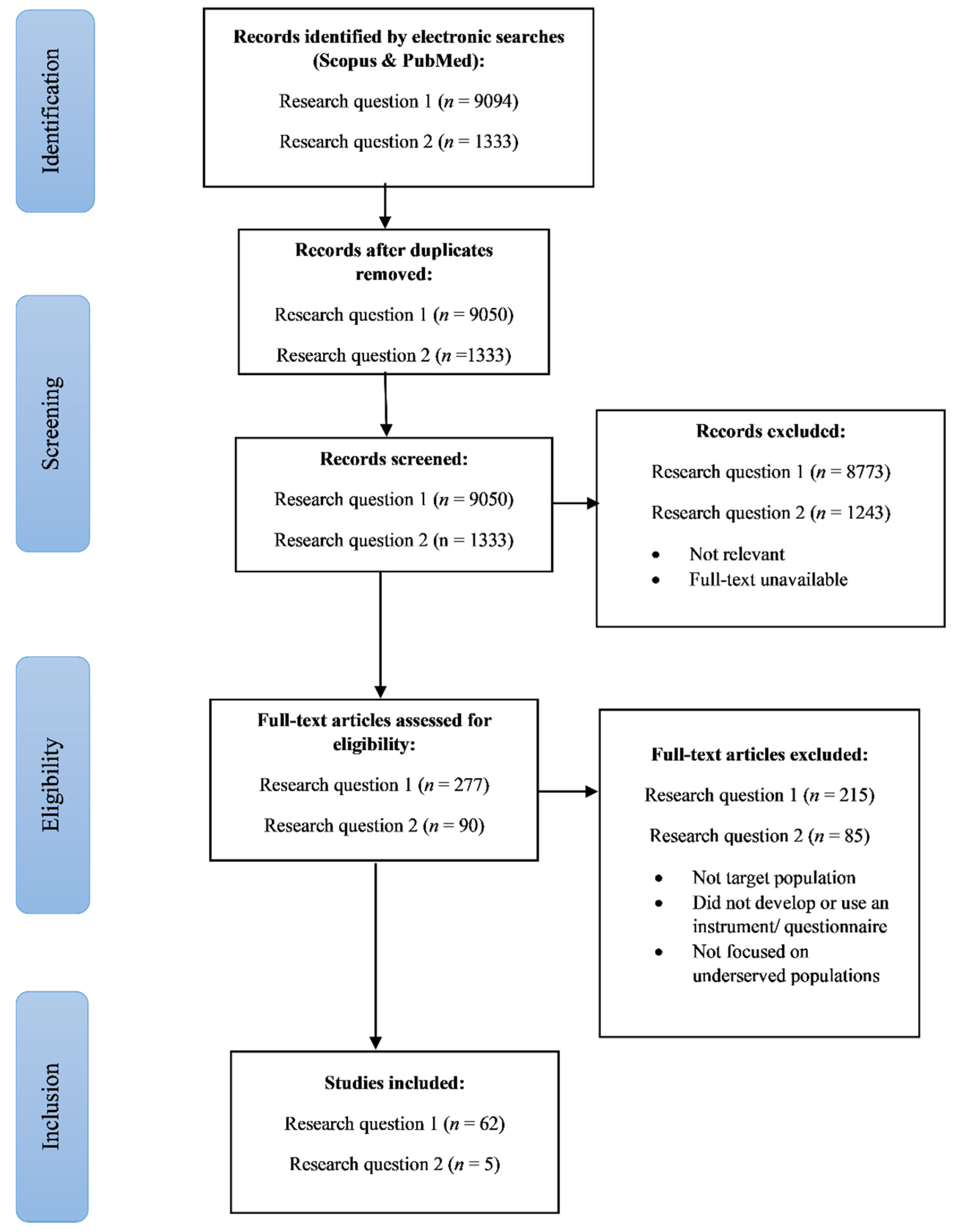
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Analyses of Results
3. Results
3.1. Studies Assessing CVD Risks in the General Young Adult Population
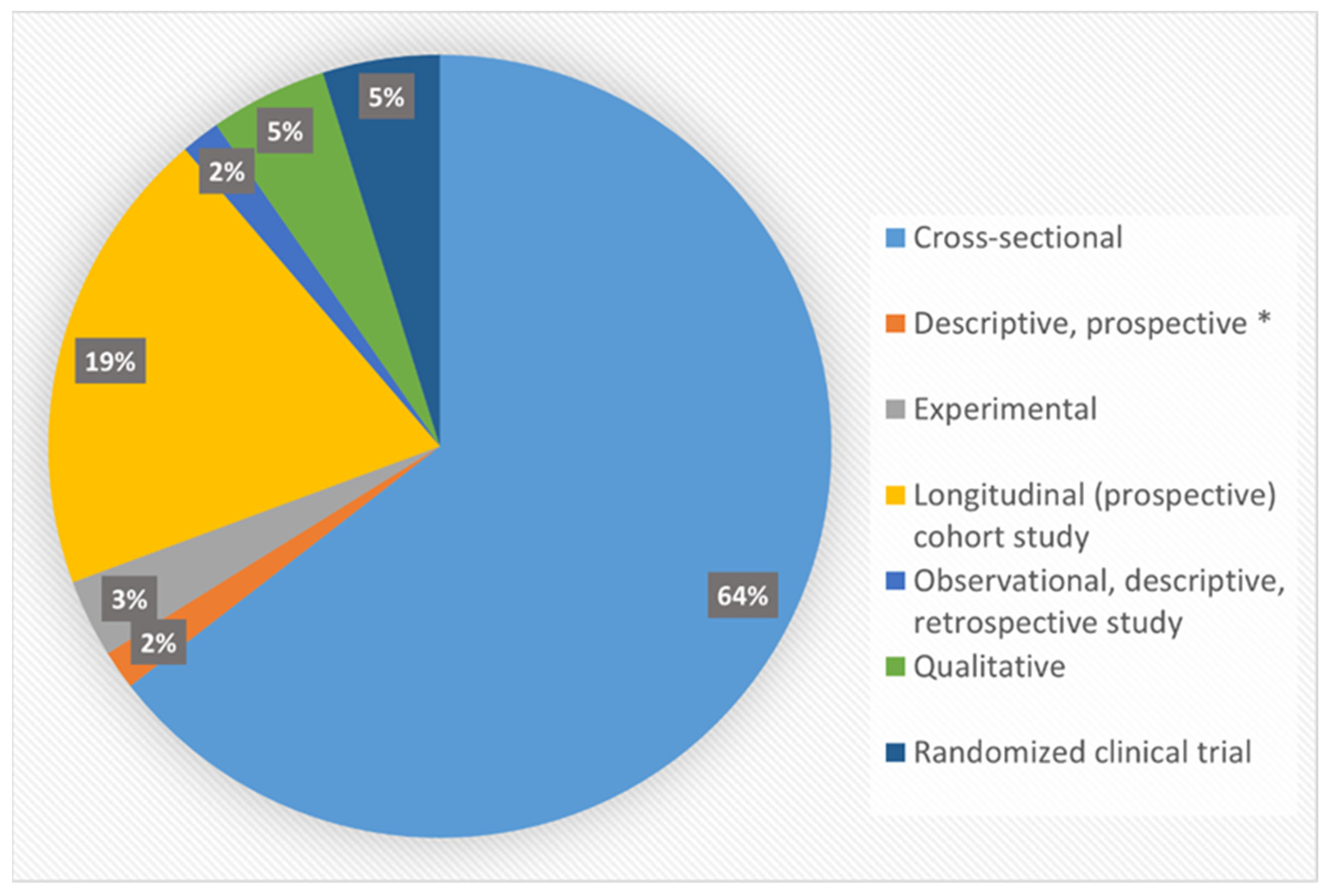
3.1.1. Study Designs and Populations
3.1.2. CVD Outcomes
3.1.3. Risk Assessment Tools/Models/Measures
3.1.4. Sample Size
3.2. Studies Assessing CVD Risks in the Underserved Young Adult Populations
3.2.1. Study Designs and Populations
3.2.2. CVD Outcomes
3.2.3. Risk Assessment Tools/Models/Measures
3.2.4. Sample Size
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity and Severe Obesity among Adults: United States, 2017–2018 NCHS Data Brief, No 360; National Center for Health Statistics: Hyattsville, MD, USA, 2020. [Google Scholar]
- Kumanyika, S.K.; Obarzanek, E.; Stettler, N.; Bell, R.; Field, A.E.; Fortmann, S.P.; Franklin, B.A.; Gillman, M.W.; Lewis, C.E.; Poston, W.C., II; et al. Population-Based Prevention of Obesity: The Need for Comprehensive Promotion of Healthful Eating, Physical Activity, and Energy Balance: A Scientific Statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation 2008, 118, 428–464. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; De Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics’2017 Update: A Report from the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef]
- Sandmaier, M. The Healthy Heart Handbook for Women; National Heart, Lung, & Blood Institute: Bethesda, MD, USA, 2007; pp. 1–127. [Google Scholar]
- Ferdinand, K.C.; Armani, A. Cardiovascular Disease in Racial and Ethnic Minorities. Totowa, N.J., Ed.; Humana Press: New York, NY, USA, 2006; pp. 1–21. [Google Scholar] [CrossRef]
- Pletcher, M.J.; Moran, A.E. Cardiovascular Risk Assessment. Med. Clin. N. Am. 2017, 101, 673–688. [Google Scholar] [CrossRef]
- Gooding, H.C.; de Ferranti, S.D. Cardiovascular Risk Assessment and Cholesterol Management in Adolescents: Getting to the Heart of the Matter. Curr. Opin. Pediatr. 2010, 22, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Goff, D.; Lloyd-Jones, D.; Bennett, G.; Coady, S.; D’Agostino, R.; Gibbons, R.; Greenland, P.; Lackland, D.; Levy, D.; O’Donnell, C.; et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129, S49–S73. [Google Scholar] [CrossRef]
- Alssema, M.; Newson, R.S.; Bakker, S.J.L.; Stehouwer, C.D.A.; Heymans, M.W.; Nijpels, G.; Hillege, H.L.; Hofman, A.; Witteman, J.C.M.; Gansevoort, R.T.; et al. One Risk Assessment Tool for Cardiovascular Disease, Type 2 Diabetes, and Chronic Kidney Disease. Diabetes Care 2012, 35, 741–749. [Google Scholar] [CrossRef]
- Ofori, S.; Odia, O. Risk Assessment in the Prevention of Cardiovascular Disease in Low-Resource Settings. Indian Heart J. 2016, 68, 391–398. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Prevention of Cardiovascular Disease: Guidelines for Assessment and Management of Total Cardiovascular Risk; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- McFayden, E. Key Factors Influencing Health Disparities Among African Americans. Race Gend. Class New Orleans 2009, 16, 120–133. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Surveillance of Health Status in Minority Communities—Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. Morb. Mortal. Wkly. Rep. Surveill. Summ. 2011, 60, 1–44. [Google Scholar]
- Sacramento-Pacheco, J.; Duarte-Clíments, G.; Gómez-Salgado, J.; Romero-Martín, M.; Sánchez-Gómez, M.B. Cardiovascular Risk Assessment Tools: A Scoping Review. Aust. Crit. Care 2019, 32, 540–559. [Google Scholar] [CrossRef]
- Matheny, M.; McPheeters, M.; Glasser, A.; Mercaldo, N.; Weaver, R.; Jerome, R.; Walden, R.; McKoy, J.; Pritchett, J.; Tsai, C. Systematic Review of Cardiovascular Disease Risk Assessment Tools; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2011. [Google Scholar]
- Cooney, M.-T.; Dudina, A.L.; Graham, I.M. Value and Limitations of Existing Scores for the Assessment of Cardiovascular Risk: A Review for Clinicians. J. Am. Coll. Cardiol. 2009, 54, 1209–1227. [Google Scholar] [CrossRef]
- Chamnan, P.; Simmons, R.K.; Sharp, S.J.; Griffin, S.J.; Wareham, N.J. Cardiovascular Risk Assessment Scores for People with Diabetes: A Systematic Review. Diabetologia 2009, 52, 2001–2015. [Google Scholar] [CrossRef]
- Gaziano, T.A.; Abrahams-Gessel, S.; Alam, S.; Alam, D.; Ali, M.; Bloomfield, G.; Carrillo-Larco, R.M.; Dorairaj, P.; Gutierrez, L.; Irazola, V.; et al. Comparison of Nonblood-Based and Blood-Based Total CV Risk Scores in Global Populations. Glob. Heart 2016, 11, 37–46.e2. [Google Scholar] [CrossRef]
- Prinsen, C.A.C.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; de Vet, H.C.W.; Terwee, C.B. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual. Life Res. 2018, 27, 1147–1157. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bloomfield, G.S.; Mwangi, A.; Chege, P.; Simiyu, C.J.; Aswa, D.F.; Odhiambo, D.; Obala, A.A.; Ayuo, P.; Khwa-Otsyula, B. Multiple Cardiovascular Risk Factors in Kenya: Evidence from a Health and Demographic Surveillance System Using the WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance. Heart 2013, 99, 1323–1330. [Google Scholar] [CrossRef]
- Altenburg, T.M.; de Kroon, M.L.A.; Renders, C.M.; Hirasing, R.; Chinapaw, M.J.M. TV Time but Not Computer Time Is Associated with Cardiometabolic Risk in Dutch Young Adults. PLoS ONE 2013, 8, e57749. [Google Scholar]
- Baragou, S.; Djibril, M.; Atta, B.; Damorou, F.; Pio, M.; Balogou, A. Prevalence of Cardiovascular Risk Factors in an Urban Area of Togo: A WHO STEPS-Wise Approach in Lome, Togo. Cardiovasc. J. Afr. 2012, 23, 309–313. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhang, H.; Rodriguez-Monguio, R. Racial Disparities in the Risk of Developing Obesity-Related Diseases: A Cross-Sectional Study. Ethn. Dis. 2012, 22, 308–317. [Google Scholar] [PubMed]
- Hamarneh, N.Y.A.; Crealey, G.E.; McElnay, J.C. Coronary Heart Disease: Health Knowledge and Behaviour. Int. J. Clin. Pharm. 2011, 33, 111–124. [Google Scholar] [CrossRef]
- Sanderson, S.C.; Waller, J.; Jarvis, M.J.; Humphries, S.E.; Wardle, J. Awareness of Lifestyle Risk Factors for Cancer and Heart Disease among Adults in the UK. Patient Educ. Couns. 2009, 74, 221–228. [Google Scholar] [CrossRef]
- Williamson, W.; Lewandowski, A.J.; Forkert, N.D.; Griffanti, L.; Okell, T.W.; Betts, J.; Boardman, H.; Siepmann, T.; McKean, D.; Huckstep, O.; et al. Association of Cardiovascular Risk Factors with MRI Indices of Cerebrovascular Structure and Function and White Matter Hyperintensities in Young Adults. J. Am. Med. Assoc. 2018, 320, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Tran, D.M.T.; Zimmerman, L.M.; Kupzyk, K.A. Validation of the Knowledge and Perception of Cardiovascular Risk Factors Questionnaires for College Students. J. Nurs. Meas. 2016, 24, 202–214. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, R.J.J.; Fesahazion, R.G.; Parker, L.; Wilder, T.; Rooks, R.N.; Bowie, J.V.; Bell, C.N.; Szanton, S.L.; LaVeist, T.A. Accelerated Health Declines among African Americans in the USA. J. Urban Health 2016, 93, 808–820. [Google Scholar] [CrossRef]
- Lai, H.L.; Ward, R.; Bolin, P. Cardiovascular Health of North Carolina Undergraduates. N. C. Med. J. 2015, 76, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Mark, A.E.; Riley, D.L.; McDonnell, L.A.; Pipe, A.L.; Reid, R.D. Healthy Eating Opinion Survey for Individuals at Risk for Cardiovascular Disease. Health Psychol. 2014, 33, 904–912. [Google Scholar] [CrossRef]
- Schmitz, R.; Jordan, S.; Müters, S.; Neuhauser, H. Population-Wide Use of Behavioural Prevention and Counselling Programmes for Lifestyle-Related Cardiovascular Risk Factors in Germany. Eur. J. Prev. Cardiol. 2012, 19, 849–857. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koura, M.R.; Al-Dabal, B.; Rasheed, P.; Al-Sowielem, L.; Makki, S.M. Prehypertension among Young Adult Females in Dammam, Saudi Arabia. East. Mediterr. Health J. 2012, 18, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Foulds, H.J.A.; Bredin, S.S.D.; Warburton, D.E.R. An Evaluation of the Physical Activity and Health Status of British Columbian Aboriginal Populations. Appl. Physiol. Nutr. Metab. 2012, 127–137. [Google Scholar] [CrossRef]
- Chan, C.W.; Leung, S.F. Differences in Perceptions of Coronary Disease among Hong Kong Chinese: Implications for the Societal Readiness in Disease Prevention. Psychol. Health Med. 2012, 17, 366–376. [Google Scholar] [CrossRef]
- Maniadakis, N.; Kourlaba, G.; Fragoulakis, V. Self-Reported Prevalence of Atherothrombosis in a General Population Sample of Adults in Greece; a Telephone Survey. BMC Cardiovasc. Disord. 2011, 11, 16. [Google Scholar] [CrossRef]
- Kuklina, E.V.; Yoon, P.W.; Keenan, N.L. Prevalence of Coronary Heart Disease Risk Factors and Screening for High Cholesterol Levels among Young Adults, United States, 1999–2006. Ann. Fam. Med. 2010, 8, 327–334. [Google Scholar] [CrossRef]
- Wamala, J.F.; Karyabakabo, Z.; Ndungutse, D.; Guwatudde, D. Prevalence Factors Associated with Hypertension in Rukungiri District, Uganda—A Community-Based Study. Afr. Health Sci. 2009, 9, 153–161. [Google Scholar] [PubMed]
- Bjartveit, K.; Tverdal, A. Health Consequences of Sustained Smoking Cessation. Tob. Control 2009, 18, 197–206. [Google Scholar] [CrossRef]
- Tucker, A.M.; Vogel, R.A.; Lincoln, A.E.; Dunn, R.E.; Ahrensfield, D.C.; Allen, T.W.; Castle, L.W.; Heyer, R.A.; Pellman, E.J.; Strollo, P.J.; et al. Prevalence of Cardiovascular Disease Risk Factors among National Football League Players. J. Am. Med. Assoc. 2009, 301, 2111–2119. [Google Scholar] [CrossRef] [PubMed]
- Jamil, H.; Dallo, F.; Fakhouri, M.; Templin, T.; Khoury, R.; Fakhouri, H. The Prevalence of Self-Reported Chronic Conditions among Arab, Chaldean, and African Americans in Southeast Michigan. Ethn. Dis. 2009, 19, 293–301. [Google Scholar]
- Ammouri, A.A.; Neuberger, G. The Perception of Risk of Heart Disease Scale: Development and Psychometric Analysis. J. Nurs. Meas. 2008, 16, 83–98. [Google Scholar] [CrossRef]
- Wagner, J.; Lacey, K.; Chyun, D.; Abbott, G. Development of a Questionnaire to Measure Heart Disease Risk Knowledge in People with Diabetes: The Heart Disease Fact Questionnaire. Patient Educ. Couns. 2005, 58, 82–87. [Google Scholar] [CrossRef]
- Tovar, E.G.; Rayens, M.K.; Clark, M.; Nguyen, H. Development and Psychometric Testing of the Health Beliefs Related to Cardiovascular Disease Scale: Preliminary Findings. J. Adv. Nurs. 2010, 66, 2772–2784. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO STEPS Surveillance Manual: The WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Doom, J.R.; Mason, S.M.; Suglia, S.F.; Clark, C.J. Pathways between Childhood/Adolescent Adversity, Adolescent Socioeconomic Status, and Long-Term Cardiovascular Disease Risk in Young Adulthood. Soc. Sci. Med. 2017, 188, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Abshire, D.A.; Lennie, T.A.; Moser, D.K.; Mudd-Martin, G.T. Perceptions Related to Cardiovascular Disease Risk in Caucasian College Males. Am. J. Mens. Health 2016, 10, N136–N144. [Google Scholar] [CrossRef]
- Wickrama, K.A.S.; Bae, D.; O’Neal, C.W. Black-White Disparity in Young Adults’ Disease Risk: An Investigation of Variation in the Vulnerability of Black Young Adults to Early and Later Adversity. J. Adolesc. Health 2016, 59, 209–215. [Google Scholar] [CrossRef]
- Khan, R.J.; Stewart, C.P.; Davis, S.K.; Harvey, D.J.; Leistikow, B.N. The Risk and Burden of Smoking Related Heart Disease Mortality among Young People in the United States. Tob. Induc. Dis. 2015, 13, 16. [Google Scholar] [CrossRef] [PubMed]
- Pencina, M.J.; D’Agostino Sr, R.B.; Larson, M.G.; Massaro, J.M.; Vasan, R.S. Predicting the 30-Year Risk of Cardiovascular Disease: The Framingham Heart Study. Circulation 2009, 119, 3078–3084. [Google Scholar] [CrossRef]
- Kariuki, J.K.; Stuart-Shor, E.M.; Leveille, S.G.; Hayman, L.L. Evaluation of the Performance of Existing Non-Laboratory Based Cardiovascular Risk Assessment Algorithms. BMC Cardiovasc. Disord. 2013, 13, 123. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino Sr, R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General Cardiovascular Risk Profile for Use in Primary Care: The Framingham Heart Study. Circulation 2008, 117, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Gaziano, T.A.; Young, C.R.; Fitzmaurice, G.; Atwood, S.; Gaziano, J.M. Laboratory-Based versus Non-Laboratory-Based Method for Assessment of Cardiovascular Disease Risk: The NHANES I Follow-up Study Cohort. Lancet 2008, 371, 923–931. [Google Scholar] [CrossRef]
- Mendis, S.; Lindholm, L.H.; Mancia, G.; Whitworth, J.; Alderman, M.; Lim, S.; Heagerty, T. World Health Organization (WHO) and International Society of Hypertension (ISH) Risk Prediction Charts: Assessment of Cardiovascular Risk for Prevention and Control of Cardiovascular Disease in Low and Middle-Income Countries. J. Hypertens. 2007, 25, 1578–1582. [Google Scholar] [CrossRef]
- May, M.; Lawlor, D.A.; Brindle, P.; Patel, R.; Ebrahim, S. Cardiovascular Disease Risk Assessment in Older Women: Can We Improve on Framingham? British Women’s Heart and Health Prospective Cohort Study. Heart 2006, 92, 1396–1402. [Google Scholar] [CrossRef]
- Berry, J.D.; Lloyd-Jones, D.M.; Garside, D.B.; Greenland, P. Framingham Risk Score and Prediction of Coronary Heart Disease Death in Young Men. Am. Heart J. 2007, 154, 80–86. [Google Scholar] [CrossRef]
| Cardiovascular Disease | Risk Assessment | Tool | Young Adult | Vulnerable Populations | |
|---|---|---|---|---|---|
| MeSH terms/subheadings | Cardiovascular Diseases | Risk Assessment | Surveys and questionnaires, patient-reported outcome measures, healthcare surveys | Young Adult | Vulnerable populations, medically underserved area |
| Text words | cardiovascular AND diseases, “cardiovascular diseases”, cardiovascular AND disease OR “cardiovascular disease” heart diseases, heart disease, cerebrovascular diseases, hypertension, myocardial ischemia, myocardial infarction, heart attack, cardiovascular stroke, cerebral hemorrhage, cerebral stroke, stroke, brain ischemia | Risk Assessments, Health Risk Assessment, Health Risk Assessments, Risk Factors, Risk Prediction, Risk Models, Risk Prediction Models | Tools, instrumentation, instruments, community surveys, surveys, questionnaires, “surveys and questionnaires,” measures, outcomes assessment, outcome measures | young adult, young adults | Disadvantaged, Underserved Patients, Underserved Populations, Sensitive Population Groups, Sensitive Populations, Medically Underserved Population, vulnerable, limited [All Fields] AND health resources [mh] |
| Component | Included | Excluded |
|---|---|---|
| Participants |
|
|
| Intervention | Studies designed to increase CVD risk awareness or prevent CVD by altering one or more SNAP risk factors or at least one CVD outcome. | |
| Comparators | Any comparators/controls | |
| Outcome | The main outcome was objective and/or self-reported measure(s) for the non-clinical assessment of modifiable CVD risk factors by evaluating the SNAP risk factors. Studies that:
| Articles without full text. |
| Study design | Observational, experimental, and trial studies. | Review/meta-analyses |
| No. | Author(s); Year of Publication | Study Population | Country | Sample Size | Age (Years) | Gender | Modifiable CVD Risk Factors Assessed (Smoking, Nutrition/Diet, Alcohol Use, or Physical Activity) | Risk Assessment Measure/Tool |
|---|---|---|---|---|---|---|---|---|
| 1 | Williamson W et al., 2018 [27] | Young adults without clinical evidence of cerebrovascular disease | U.K | 125 | 18–40 | 49% female | Smoking, alcohol use, physical activity | Detailed questionnaire on medical history, socioeconomic status, and self-reported behaviors such as nutritional intake, smoking, and alcohol consumption. |
| 2 | Tran D-T et al., 2016 [28] | College students at a Midwestern institution | U.S.A. | 100 | 19–39 | Male & female * | None | Heart Disease Fact Questionnaire; The Health Beliefs Related to Cardiovascular Disease |
| 3 | Thorpe RJ et al., 2016 [29] | Participants from 2000–2009 National Health Interview Surveys | U.S.A. | 619,130 | 18–75+ | 52.1% female | Physical activity | Health survey |
| 4 | Lai HL et al., 2015 [30] | East Carolina University undergraduates | U.S.A | 525 | 16–23 | 60.7% female | Smoking, physical activity | Health survey (internally validated) |
| 5 | Mark AE et al., 2014 [31] | Individuals at risk for coronary heart disease | U.S.A. | 388 | 22–78 | 60.6% female | Nutrition/diet | Questionnaire (the Healthy Eating Opinion Survey) |
| 6 | Bloomfield GS et al., 2013 [21] | Adults [Health and Demographic Surveillance System] | Kenya | 4037 | 18–>64 | 61% female | Smoking, nutrition/diet, alcohol use, physical activity | Home-based survey using the WHO STEPwise approach to chronic disease risk factor surveillance (WHO STEPS) |
| 7 | Schmitz R et al., 2012 [32] | Non-institutionalized adult population (National health interview [GEDA 2009] respondents. | Germany | 21,262 | 18–≥65 | 51.5% female | Nutrition/diet, physical activity | Self-reported physician-diagnosed disease |
| 8 | Koura MR et al., 2012 [33] | Young adult females | Saudi Arabia | 370 | Mean = 19.9 ± 1.4 | 100% female | Smoking, nutrition/diet, physical activity | WHO-STEPS |
| 9 | Baragou S et al., 2012 [23] | The general adult population | Togo | 2000 | 18–98 | 55.1% female | Smoking, nutrition/diet, alcohol use, physical activity | WHO STEPS |
| 10 | Foulds HJA et al., 2012 [34] | Aboriginal adult population (participants from the Hearts in Training and Health Beat physical activity training programs) | Canada | 882 | 16–77 | 75.2% female | Smoking, physical activity | Multiple-choice questions |
| 11 | Chan CW et al., 2012 [35] | Hong Kong Chinese population | Hong Kong | 236 | 18–91 | 66.5% female | None | Survey |
| 12 | Maniadakis N et al., 2011 [36] | General adult population | Greece | 3007 | 18–>65 | 51.7% female | None | Survey |
| 13 | Al Hamarneh YN et al., 2011 [25] | General adult population | Northern Ireland | 1000 | 20–79 | 46% females | Smoking, nutrition/diet, alcohol use, physical activity | Questionnaire |
| 14 | Kuklina EV et al., 2010 [37] | Participants from the National Health and Nutrition Examination Survey (NHANES) | U.S.A. | 2587 | 20–35 (male); 20–45 (female) | 61.2% female | Smoking | Survey |
| 15 | Wamala JF et al., 2009 [38] | Adult population | Uganda | 842 | 20–>75 | 48% female | Smoking, alcohol use, physical activity | Questionnaire |
| 16 | Bjartveit K et al., 2009 [39] | Individuals surveyed for CVD risk factors | Norway | 48,682 | 20–49 | 51.6% female | Smoking, physical activity | Questionnaire |
| 17 | Tucker AM et al., 2009 [40] | Veteran football players | U.S.A. | 504 | 23–35 | 100% male | Smoking | Survey instrument |
| 18 | Sanderson SC et al., 2009 [26] | Respondents from the Office of National Statistics Omnibus Survey | U.K. | 1747 | 16–75 | 47% female | Smoking, nutrition/diet, alcohol use, physical activity | Questionnaire |
| 19 | Jamil H et al., 2009 [41] | Respondents from the Health Assessment Survey | U.S.A. | 3280 | 18–75 | 71.9% female | Smoking, nutrition/diet, physical activity | Health survey |
| 20 | Ammouri AA et al., 2008 [42] | General population | Jordan | 295 | 15–75 | 51% female | None | Questionnaire (The Perception of Risk of Heart Disease Scale) |
| No. | Author(s); Year of Publication | Study Population | Country | Sample Size | Age (Years) | Gender | Modifiable CVD Risk Factors Assessed (Smoking, Nutrition/Diet, Alcohol Use, or Physical Activity) | Risk Assessment Measure/Tool |
|---|---|---|---|---|---|---|---|---|
| 1 | Doom JR et al., 2017 [46] | Add Health study participants | U.S.A. | 14,493 | 24–34 | 48.9% female | Smoking, nutrition/diet, alcohol use, physical activity | 30 year Framingham CVD Risk Score |
| 2 | Abshire DA et al., 2016 [47] | Undergraduate Caucasian males recruited from a public, 4 year university through purposive and snowball sampling; free of CVD and not enrolled in a health-related major. | U.S.A. | 10 | 18–25 | 100% male | None | Interview guide |
| 3 | Wickrama KAS et al., 2016 [48] | Add Health study participants | U.S.A. | 8824 | 24–32 | Male & female * | None | None; biomarkers assessed |
| 4 | Khan RJ et al., 2015 [49] | 1997–2004 data from National Health Interview Survey | U.S.A. | 121,284 | 18–44 | 54.5% female | Smoking, physical activity | None |
| 5 | Jamil H et al., 2009 [41] | Respondents from the Health Assessment Survey | U.S.A. | 3280 | 18–75 | 71.9% female | Smoking, nutrition/diet, physical activity | Health survey |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Opoku-Acheampong, A.A.; Rosenkranz, R.R.; Adhikari, K.; Muturi, N.; Logan, C.; Kidd, T. Tools for Assessing Cardiovascular Disease Risk Factors in Underserved Young Adult Populations: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 13305. https://doi.org/10.3390/ijerph182413305
Opoku-Acheampong AA, Rosenkranz RR, Adhikari K, Muturi N, Logan C, Kidd T. Tools for Assessing Cardiovascular Disease Risk Factors in Underserved Young Adult Populations: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(24):13305. https://doi.org/10.3390/ijerph182413305
Chicago/Turabian StyleOpoku-Acheampong, Audrey A., Richard R. Rosenkranz, Koushik Adhikari, Nancy Muturi, Cindy Logan, and Tandalayo Kidd. 2021. "Tools for Assessing Cardiovascular Disease Risk Factors in Underserved Young Adult Populations: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 24: 13305. https://doi.org/10.3390/ijerph182413305
APA StyleOpoku-Acheampong, A. A., Rosenkranz, R. R., Adhikari, K., Muturi, N., Logan, C., & Kidd, T. (2021). Tools for Assessing Cardiovascular Disease Risk Factors in Underserved Young Adult Populations: A Systematic Review. International Journal of Environmental Research and Public Health, 18(24), 13305. https://doi.org/10.3390/ijerph182413305







