Differences in the Impact of COVID-19 on Pathology Laboratories and Cancer Diagnosis in Girona
Abstract
:1. Introduction
2. Methodology
Statistical Analysis
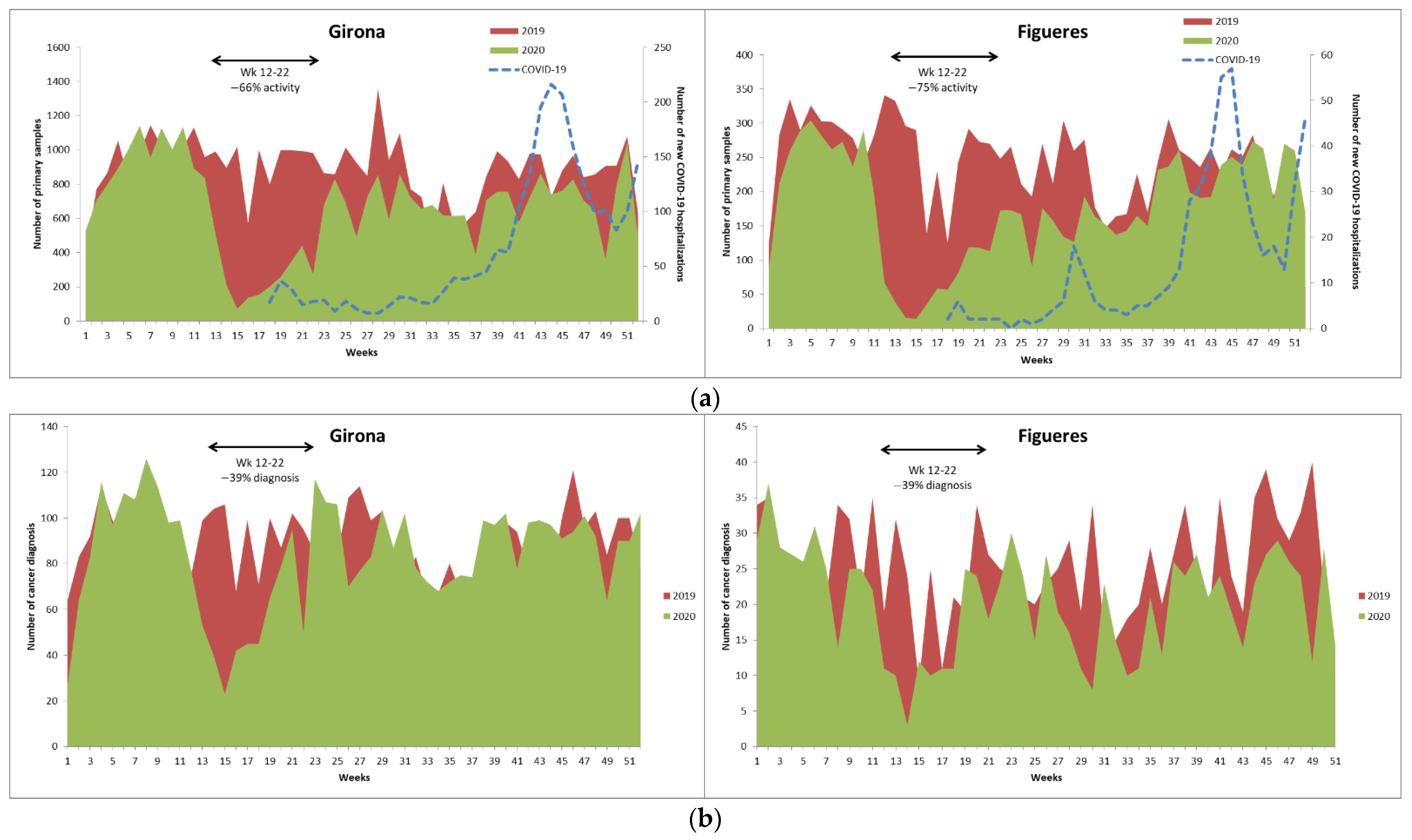
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ministerio de Sanidad. Enfermedad Por Nuevo Coronavirus, COVID-19. 2020. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/ (accessed on 27 April 2021).
- The Lancet Public Health. COVID-19 in Spain: A predictable storm? Lancet Public Health 2020, 5, e568. [Google Scholar] [CrossRef]
- Horton, R. Offline: COVID-19 is not a pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef]
- REDECAN-Red Española de Registros de Cáncer. Available online: https://redecan.org/redecan.org/es/index.html (accessed on 4 February 2021).
- Jazieh, A.R.; Akbulut, H.; Curigliano, G.; Rogado, A.; Alsharm, A.A.; Razis, E.D.; Mula-Hussain, L.; Errihani, H.; Khattak, A.; De Guzman, R.B.; et al. Impact of the COVID-19 Pandemic on Cancer Care: A Global Collaborative Study. JCO Glob. Oncol. 2020, 6, 1428–1438. [Google Scholar] [CrossRef]
- Serraino, D. COVID-19 and cancer: Looking for evidence. Eur. J. Surg. Oncol. 2020, 46, 929–930. [Google Scholar] [CrossRef] [PubMed]
- Sharpless, N.E. COVID-19 and cancer. Science 2020, 368, 1290. [Google Scholar] [CrossRef] [PubMed]
- Spencer, K.; Jones, C.M.; Girdler, R.; Roe, C.; Sharpe, M.; Lawton, S.; Miller, L.; Lewis, P.; Evans, M.; Sebag-Montefiore, D.; et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: A population-based study. Lancet Oncol. 2021, 22, 309–320. [Google Scholar] [CrossRef]
- Pollán, M.; Pérez-Gómez, B.; Pastor-Barriuso, R.; Oteo, J.; Hernán, M.; Pérez-Olmeda, M.; Sanmartín, J.L.; Fernández-García, A.; Cruz, I.; Fernández de Larrea, N.; et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): A nationwide, population-based seroepidemiological study. Lancet 2020, 396, 535–544. [Google Scholar] [CrossRef]
- Instituto de Salud Carlos III; Ministerio de Ciencia e Innovación y Ministerio de Sanidad (España). Estudio ENE-COVID: Cuarta Ronda Estudio Nacional de Sero-Epidemiología de la Infección Por SARS-COV-2 en España; 2020. 2021. Available online: Moz-extension://138143b5-5de3-4711-a327-450bbb282e22/enhanced-reader.html?openApp&pdf=https%3A%2F%2Fwww.mscbs.gob.es%2FgabinetePrensa%2FnotaPrensa%2Fpdf%2F15.12151220163348113.pdf (accessed on 27 April 2021).
- Sanz, X.; Pareja, L.; Rius, A.; Rodenas, P.; Abdón, N.; Gálvez, J.; Esteban, L.; Escribà, J.M.; Borràs, J.M.; Ribes, J. Definition of a SNOMED CT pathology subset and microglossary, based on 1.17 million biological samples from the Catalan Pathology Registry. J. Biomed. Inform. 2018, 78, 167–176. [Google Scholar] [CrossRef]
- Sanz, X.; Pareja, L.; Rius, A.; Gálvez, J.; Escribà, J.M.; Esteban, L.; Borràs, J.M.; Ribes, J. How cancer registries can detect neoplasms in pathology laboratories that code with SNOMED CT terminology? An actual, simple and flexible solution. Int. J. Med. Inform. 2020, 141. [Google Scholar] [CrossRef]
- Fritz, A.; Percy, C.; Jack, A.; Shanmugaratnam, K.; Sobin, L.; Parkin, D.M.; Whelan, S. ICD-O International Classification of Diseases for Oncology First Revision; World Health Organization: Geneva, Switzerland, 2013.
- Generalitat de Catalunya. Dades Obertes de Catalunya. Available online: https://analisi.transparenciacatalunya.cat/ca/ (accessed on 27 April 2021).
- Ruiz-Medina, S.; Gil, S.; Jimenez, B.; Rodriguez-Bazzarola, P.; Diaz-Redondo, T.; Cazorla, M.; Muños-Ayllon, M.; Ramos, I.; Reyna, C.; Bermejo, M.J.; et al. Significant Decrease in Annual Cancer Diagnoses in Spain during the COVID-19 Pandemic: A Real-Data Study. Cancers 2021, 13, 3215. [Google Scholar] [CrossRef]
- Vardhanabhuti, V.; Ng, K.S. Differential Impact of COVID-19 on Cancer Diagnostic Services Based on Body Regions: A Public Facility-Based Study in Hong Kong. Int. J. Radiat. Oncol. 2021, 111, 331–336. [Google Scholar] [CrossRef]
- London, J.W.; Fazio-Eynullayeva, E.; Palchuk, M.B.; Sankey, P.; McNair, C. Effects of the COVID-19 Pandemic on Cancer-Related Patient Encounters. JCO Clin. Cancer Inform. 2020, 4, 657–665. [Google Scholar] [CrossRef]
- Coma, E.; Guiriguet, C.; Mora, N.; Marzo-Castillejo, M.; Benítez, M.; Méndez-Boo, L.; Fina, F.; Fàbregas, M.; Mercadé, A.; Medina, M. Impact of the COVID-19 pandemic and related control measures on cancer diagnosis in Catalonia: A time-series analysis of primary care electronic health records covering about five million people. BMJ Open 2021, 11, e047567. [Google Scholar] [CrossRef]
- Purushotham, A.; Roberts, G.; Haire, K.; Dodkins, J.; Harvey-Jones, E.; Han, L.; Rigg, A.; Twinn, C.; Pramesh, C.; Ranganathan, P.; et al. The impact of national non-pharmaceutical interventions (‘lockdowns’) on the presentation of cancer patients. Ecancermedicalscience 2021, 15, 1180. [Google Scholar] [CrossRef]
- Petrova, D.; Pérez-Gómez, B.; Pollán, M.; Sánchez, M.-J. Implications of the COVID-19 pandemic for cancer in Spain. Med. Clín. 2020, 155, 263–266. [Google Scholar] [CrossRef]
- Kutikov, A.; Weinberg, D.S.; Edelman, M.J.; Horwitz, E.M.; Uzzo, R.G.; Fisher, R.I. A War on Two Fronts: Cancer Care in the Time of COVID-19. Ann. Intern. Med. 2020, 172, 756–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amador, M.; Matias-Guiu, X.; Sancho-Pardo, G.; Contreras Martínez, J.; de la Torre-Montero, J.C.; Peñuelas Saiz, A.; Garrido, P.; García-Sanz, R.; Rodríguez-Lescure, Á.; Paz-Ares, L. Impact of the COVID-19 pandemic on the care of cancer patients in Spain. ESMO Open 2021, 6, 100157. [Google Scholar] [CrossRef]
- Tagliamento, M.; Agostinetto, E.; Bruzzone, M.; Ceppi, M.; Saini, K.S.; de Azambuja, E.; Punie, K.; Westphalen, C.B.; Morgan, G.; Pronzatp, P.; et al. Mortality in adult patients with solid or hematological malignancies and SARS-CoV-2 infection with a specific focus on lung and breast cancers: A systematic review and meta-analysis. Crit Rev. Oncol. Hematol. 2021, 163, 103365. [Google Scholar] [CrossRef]
- Saini, K.S.; Tagliamento, M.; Lambertini, M.; McNally, R.; Romano, M.; Leone, M.; Curigliano, G.; de Azambuja, E. Mortality in patients with cancer and coronavirus disease 2019: A systematic review and pooled analysis of 52 studies. Eur. J. Cancer 2020, 139, 43–50. [Google Scholar] [CrossRef]
- Saini, K.S.; Martins-Branco, D.; Tagliamento, M.; Vidal, L.; Singh, N.; Punie, K.; Lamba Saini, M.; Chico, I.; Curigliano, G.; de Azambuja, E.; et al. Emerging issues related to COVID-19 vaccination in patients with cancer. Oncol. Ther. 2021, 9, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, S.; Negbenebor, N.; Sadoughifar, R.; Ahmad, S.; Kroumpouzos, G. Global impact on dermatology practice due to the COVID-19 pandemic. Clin. Dermatol. 2021, 39, 479–487. [Google Scholar] [CrossRef]
- Recalcati, S. Cutaneous manifestations in COVID-19: A first perspective. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e212–e213. [Google Scholar] [CrossRef]
- O’Connor, E.; O’Dowd, G.; Phelan, S. Impact of COVID-19 on small biopsy diagnostic procedures and cancer resection surgeries in the North-West of Ireland. J. Clin. Pathol. 2021. [Google Scholar] [CrossRef]
- Hofman, P.; Ilié, M.; Chamorey, E.; Brest, P.; Schiappa, R.; Nakache, V.; Antoine, M.; Barberis, M.; Begueret, H.; Bibeau, F.; et al. Clinical and molecular practice of European thoracic pathology laboratories during the COVID-19 pandemic. The past and the near future. ESMO Open 2021, 6, 100024. [Google Scholar] [CrossRef]
- He, J.; Yang, L.; Tao, Z.; Yang, J.; Zhou, Y.; Wang, R.; Zhang, Y.; Huang, Y.; Zhou, L.; Sun, B.; et al. Impact of the 2019 Novel Coronavirus Disease (COVID-19) Epidemic on Radiotherapy-Treated Patients with Cancer: A Single-Center Descriptive Study. Cancer Manag. Res. 2021, 13, 37–43. [Google Scholar] [CrossRef]
- Puricelli Perin, D.M.; Elfström, K.M.; Bulliard, J.-L.; Burón, A.; Campbell, C.; Flugelman, A.A.; Giordano, L.; Kamineni, A.; Ponti, A.; Rabeneck, L.; et al. Early assessment of the first wave of the COVID-19 pandemic on cancer screening services: The International Cancer Screening Network COVID-19 survey. Prev. Med. 2021, 151, 106642. [Google Scholar] [CrossRef]
- Eijkelboom, A.H.; de Munck, L.; Lobbes, M.B.I.; van Gils, C.H.; Wesseling, J.; Westened, P.J.; Guerrero Paez, C.; Pijnappel, R.M.; Verkooijen, H.M.; Broeders, M.J.M.; et al. Impact of the suspension and restart of the Dutch breast cancer screening program on breast cancer incidence and stage during the COVID-19 pandemic. Prev. Med. 2021, 151, 106602. [Google Scholar] [CrossRef]
- Walker, M.J.; Meggetto, O.; Gao, J.; Espino-Hernández, G.; Jembere, N.; Bravo, C.A.; Rey, M.; Aslam, U.; Sheppard, A.J.; Lofters, A.K.; et al. Measuring the impact of the COVID-19 pandemic on organized cancer screening and diagnostic follow-up care in Ontario, Canada: A provincial, population-based study. Prev. Med. 2021, 151, 106586. [Google Scholar] [CrossRef]
- DeGroff, A.; Miller, J.; Sharma, K.; Sun, J.; Helsel, W.; Kammerer, W.; Rockwell, T.; Sheu, A.; Melillo, S.; Uhd, J.; et al. COVID-19 impact on screening test volume through the National Breast and Cervical Cancer early detection program, January–June 2020, in the United States. Prev. Med. 2021, 151, 106559. [Google Scholar] [CrossRef]
- Suárez, J.; Mata, E.; Guerra, A.; Jiménez, G.; Montes, M.; Arias, F.; Ciga, M.A.; Ursúa, E.; Ederra, M.; Arín, B.; et al. Impact of the COVID-19 pandemic during Spain’s state of emergency on the diagnosis of colorectal cancer. J. Surg. Oncol. 2021, 123, 32–36. [Google Scholar] [CrossRef]
- Yekedüz, E.; Karcloglu, A.M.; Utkan, G.; Ürün, Y. A clinical dilemma amid COVID-19 pandemic: Missed or encountered diagnosis of cancer? Future Oncol. 2020, 16, 1879–1881. [Google Scholar] [CrossRef]
- Kempf, E.; Lamé, G.; Layese, R.; Priou, S.; Chatellier, G.; Chaieb, H.; Benderra, M.A.; Bellamine, A.; Bey, R.; Bréant, S.; et al. New cancer cases at the time of SARS-Cov2 pandemic and related public health policies: A persistent and concerning decrease long after the end of the national lockdown. Eur. J. Cancer 2021, 150, 260–267. [Google Scholar] [CrossRef]
- Culp, M.B.B.; Soerjomataram, I.; Efstathiou, J.A.; Bray, F.; Jemal, A. Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates. Eur. Urol. 2020, 77, 38–52. [Google Scholar] [CrossRef]
- Sud, A.; Jones, M.E.; Broggio, J.; Loveday, C.; Torr, B.; Garrett, A.; Nicol, D.L.; Jhanji, S.; Boyce, S.A.; Gronthoud, F.; et al. Collateral damage: The impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann. Oncol. 2020, 31, 1065–1074. [Google Scholar] [CrossRef]
- Liu, Z.; Jiang, Y.; Yuan, H.; Fang, Q.; Cai, N.; Suo, C.; Jin, L.; Zhang, T.; Chen, X. The trends in incidence of primary liver cancer caused by specific etiologies: Results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J. Hepatol. 2019, 70, 674–683. [Google Scholar] [CrossRef]
- Valery, P.C.; Laversanne, M.; Clark, P.J.; Petrick, J.L.; McGlynn, K.A.; Bray, F. Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology 2018, 67, 600–611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muñoz-Martínez, S.; Sapena, V.; Forner, A.; Nault, J.C.; Sapisochin, G.; Rimassa, L.; Sangro, B.; Bruix, J.; Sanduzzi-Zamparelli, M.; Holówko, W.; et al. Assessing the impact of COVID-19 on liver cancer management (CERO-19). JHEP Rep. 2021, 3, 100260. [Google Scholar] [CrossRef]
- Debord, C.; Wuillème, S.; Eveillard, M.; Theisen, O.; Godon, C.; Le Bris, Y.; Béné, M. Flow cytometry in the diagnosis of mature B-cell lymphoproliferative disorders. Int. J. Lab. Hematol. 2020, 42, 113–120. [Google Scholar] [CrossRef]
- Redondo-Sánchez, D.; Marcos-Gragera, R.; Carulla, M.; Lopez de Munain, A.; Sabater Gregori, C.; Jimenez Chillarón, R.; Guevara, M.; Nuñez, O.; Fernández-Navarro, P.; Sánchez, M.J.; et al. Lung, breast and colorectal cancer incidence by socioeconomic status in spain: A population-based multilevel study. Cancers 2021, 13, 2820. [Google Scholar] [CrossRef]
- Weinberg, B.D.; Kuruva, M.; Shim, H.; Mullins, M.E. Clinical Applications of Magnetic Resonance Spectroscopy in Brain Tumors: From Diagnosis to Treatment. Radiol. Clin. N. Am. 2021, 59, 349–362. [Google Scholar] [CrossRef]
- Hamilton, A.C.; Donnelly, D.W.; Loughrey, M.B.; Turkington, R.C.; Fox, C.; Fitzpatrick, D.; O’Neill, C.E.; Gavin, A.T.; Coleman, H.G. Inequalities in the decline and recovery of pathological cancer diagnoses during the first six months of the COVID-19 pandemic: A population-based study. Br. J. Cancer 2021, 125, 798–805. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.D.; Meghal, T.; Murthy, P.; Mo, L.; D’Silva, A.; Huang, Y.; Xu, Y. Chemotherapy Treatment Modifications During the COVID-19 Outbreak at a Community Cancer Center in New York City. JCO Glob. Oncol. 2020, 6, 1298–1305. [Google Scholar] [CrossRef] [PubMed]

| Girona | Figueres | |||
|---|---|---|---|---|
| 2019 N = 46,107 | 2020 N = 34,410 | 2019 N = 12,664 | 2020 N = 9179 | |
| Type of analysis | ||||
| Autopsy | 58 (0.1) | 51 (0.1) | 17 (0.1) | 21 (0.2) |
| Biopsy | 20,178 (44) | 16,212 (47) | 6243 (49) | 4740 (52) |
| Cytology | 19,981 (43) | 13,336 (39) | 6285 (50) | 4289 (47) |
| Molecular pathology/Immunohistochemistry | 5890 (13) | 4811 (14) | 119 (0.9) | 129 (1.4) |
| Girona | Figueres | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | Differential 2020 vs. 2019 | 2019 | 2020 | Differential 2020 vs. 2019 | |||||
| N | % | N | % | % | N | % | N | % | % | |
| Lip, oral cavity, and pharynx (C00–C14) | 95 | 2.0 | 85 | 1.9 | −10 | 6 | 0.5 | 3 | 0.3 | −50 |
| Esophagus (C15) | 39 | 0.8 | 39 | 0.9 | 0 | 9 | 0.7 | 4 | 0.4 | −56 |
| Stomach (C16) | 101 | 2.2 | 77 | 1.8 | −24 | 3 | 0.2 | 5 | 0.5 | 67 |
| Colon, rectum, anus (C18–C21) | 530 | 11 | 443 | 10 | −16 | 81 | 6.2 | 65 | 6.3 | −20 |
| Liver (C22) | 85 | 1.8 | 89 | 2.0 | 4.7 | 9 | 0.7 | 10 | 1.0 | 11 |
| Biliary tract and gallbladder (C23–C24) | 14 | 0.3 | 18 | 0.4 | 29 | 13 | 1.0 | 7 | 0.7 | −46 |
| Pancreas (C25) | 30 | 0.6 | 35 | 0.8 | 17 | 42 | 3.2 | 30 | 2.9 | −29 |
| Larynx (C32) | 61 | 1.3 | 48 | 1.1 | −21 | 4 | 0.3 | 1 | 0.1 | −75 |
| Trachea, bronchus, and lung (C33–C34) | 443 | 9.5 | 412 | 9.5 | −7.0 | 99 | 7.6 | 120 | 12 | 21 |
| Bones (C40–C41) | 12 | 0.3 | 22 | 0.5 | 83 | 4 | 0.3 | 1 | 0.1 | −75 |
| Skin, melanoma | 44 | 0.9 | 39 | 0.9 | −11 | 16 | 1.2 | 10 | 1.0 | −37 |
| Hematologic (C42, C77) | 391 | 8.4 | 367 | 8.4 | −6.1 | 32 | 2.4 | 34 | 3.3 | 6.2 |
| Breast (C50) | 494 | 11 | 528 | 12 | 6.9 | 179 | 14 | 154 | 15 | −14 |
| Cervix uteri (C53) | 23 | 0.5 | 24 | 0.5 | 4.3 | 8 | 0.6 | 10 | 1.0 | 25 |
| Corpus uteri (C54) | 37 | 0.8 | 44 | 1.0 | 19 | 0 | 0 | 0 | 0 | - |
| Ovary (C56) | 28 | 0.6 | 45 | 1.0 | 61 | 18 | 1.4 | 12 | 1.2 | −33 |
| Prostate gland (C61) | 259 | 5.6 | 165 | 3.8 | −36 | 36 | 2.7 | 34 | 3.3 | −5.6 |
| Testis (C62) | 5 | 0.1 | 0 | 0 | −100 | 2 | 0.1 | 2 | 0.2 | 0 |
| Kidney and urinary tract (C64–C66, C68) | 106 | 2.3 | 90 | 2.1 | −15 | 26 | 2.0 | 22 | 2.1 | −15 |
| Bladder (C67) | 136 | 2.9 | 154 | 3.5 | 13 | 76 | 5.8 | 73 | 7.0 | −3.9 |
| Central nervous system (C70–C72) | 86 | 1.8 | 67 | 1.5 | −22 | 0 | 0 | 0 | 0 | - |
| Thyroid gland (C73) | 65 | 1.4 | 39 | 0.9 | −40 | 6 | 0.5 | 3 | 0.3 | −50 |
| Other (rest of codes) | 1149 | 25 | 1127 | 26 | −1.9 | 612 | 47 | 397 | 38 | −36 |
| Unknown primary site (C80) | 428 | 9.2 | 386 | 8.9 | −9.8 | 28 | 2.1 | 41 | 3.9 | 46 |
| Total | 4661 | 100 | 4343 | 100 | −6.8 | 1309 | 100 | 1038 | 100 | −21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanvisens, A.; Puigdemont, M.; Rubió-Casadevall, J.; Vidal-Vila, A.; López-Bonet, E.; Martín-Romero, F.; Marcos-Gragera, R. Differences in the Impact of COVID-19 on Pathology Laboratories and Cancer Diagnosis in Girona. Int. J. Environ. Res. Public Health 2021, 18, 13269. https://doi.org/10.3390/ijerph182413269
Sanvisens A, Puigdemont M, Rubió-Casadevall J, Vidal-Vila A, López-Bonet E, Martín-Romero F, Marcos-Gragera R. Differences in the Impact of COVID-19 on Pathology Laboratories and Cancer Diagnosis in Girona. International Journal of Environmental Research and Public Health. 2021; 18(24):13269. https://doi.org/10.3390/ijerph182413269
Chicago/Turabian StyleSanvisens, Arantza, Montse Puigdemont, Jordi Rubió-Casadevall, Anna Vidal-Vila, Eugeni López-Bonet, Ferran Martín-Romero, and Rafael Marcos-Gragera. 2021. "Differences in the Impact of COVID-19 on Pathology Laboratories and Cancer Diagnosis in Girona" International Journal of Environmental Research and Public Health 18, no. 24: 13269. https://doi.org/10.3390/ijerph182413269
APA StyleSanvisens, A., Puigdemont, M., Rubió-Casadevall, J., Vidal-Vila, A., López-Bonet, E., Martín-Romero, F., & Marcos-Gragera, R. (2021). Differences in the Impact of COVID-19 on Pathology Laboratories and Cancer Diagnosis in Girona. International Journal of Environmental Research and Public Health, 18(24), 13269. https://doi.org/10.3390/ijerph182413269







