Meaningful Activities and Psychosomatic Functions in Japanese Older Adults after Driving Cessation
Abstract
:1. Introduction
2. Materials and Methods
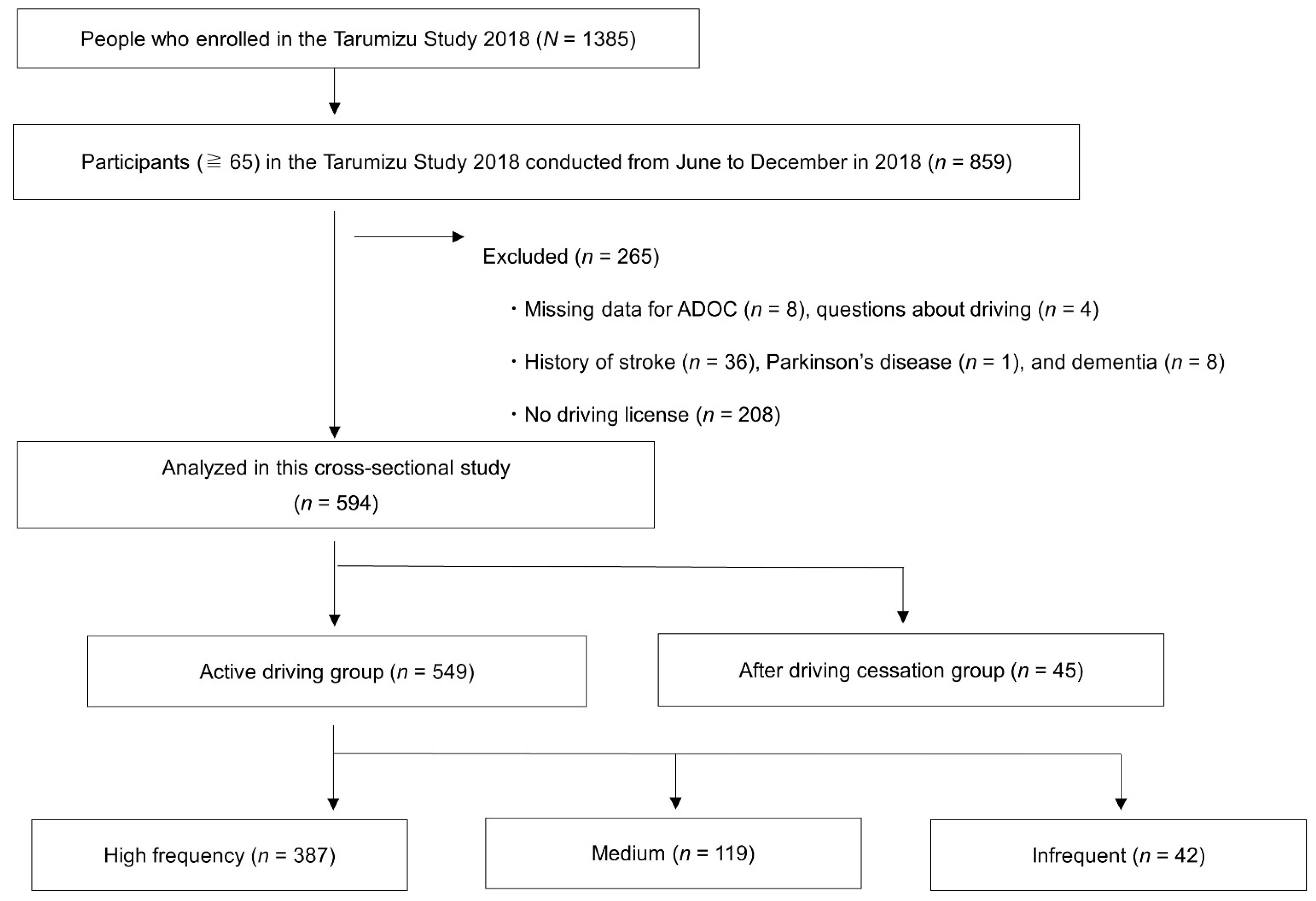
2.1. Participants
2.2. Meaningful Activity
2.3. Psychosomatic Functions
2.4. Statistical Analysis
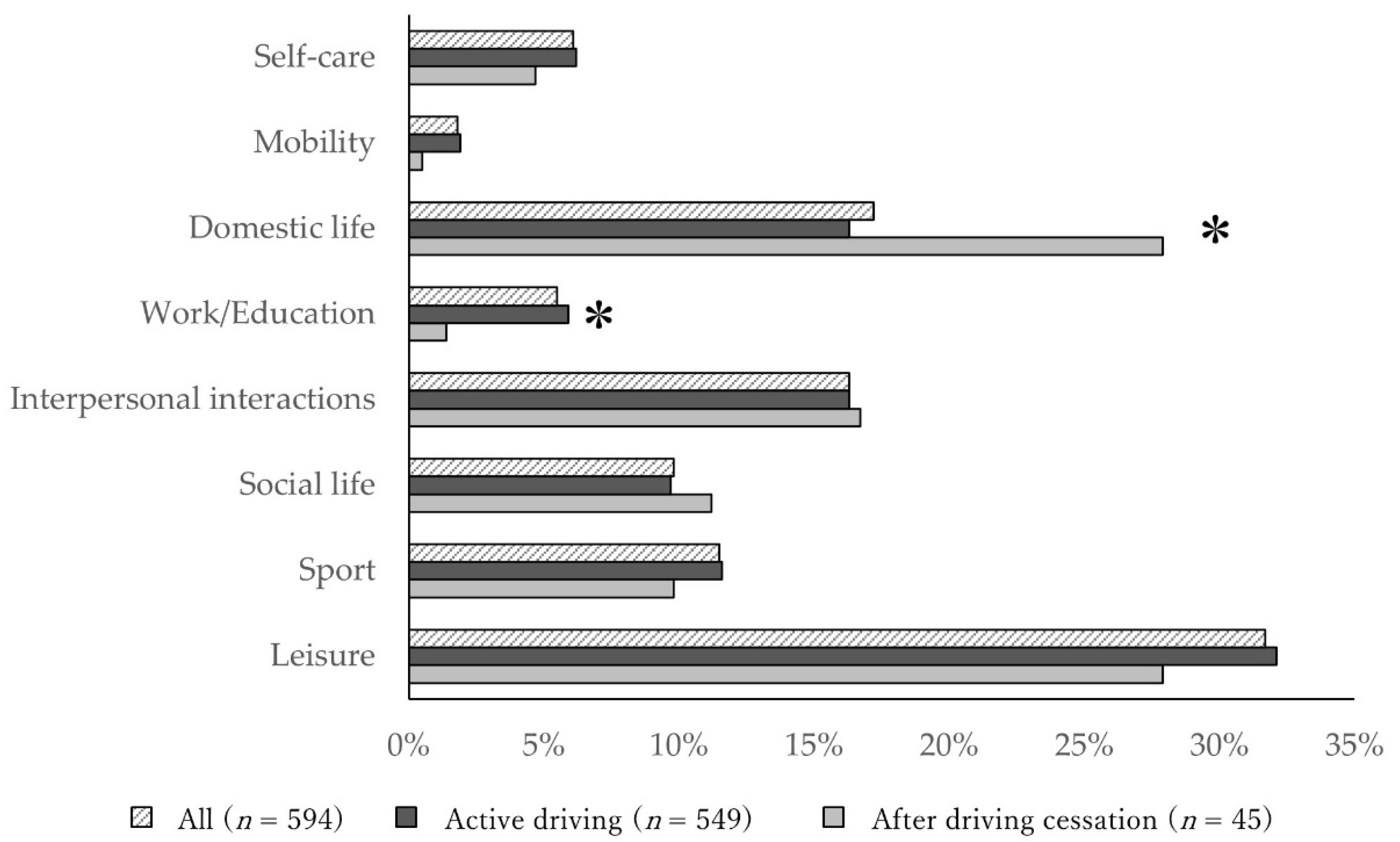
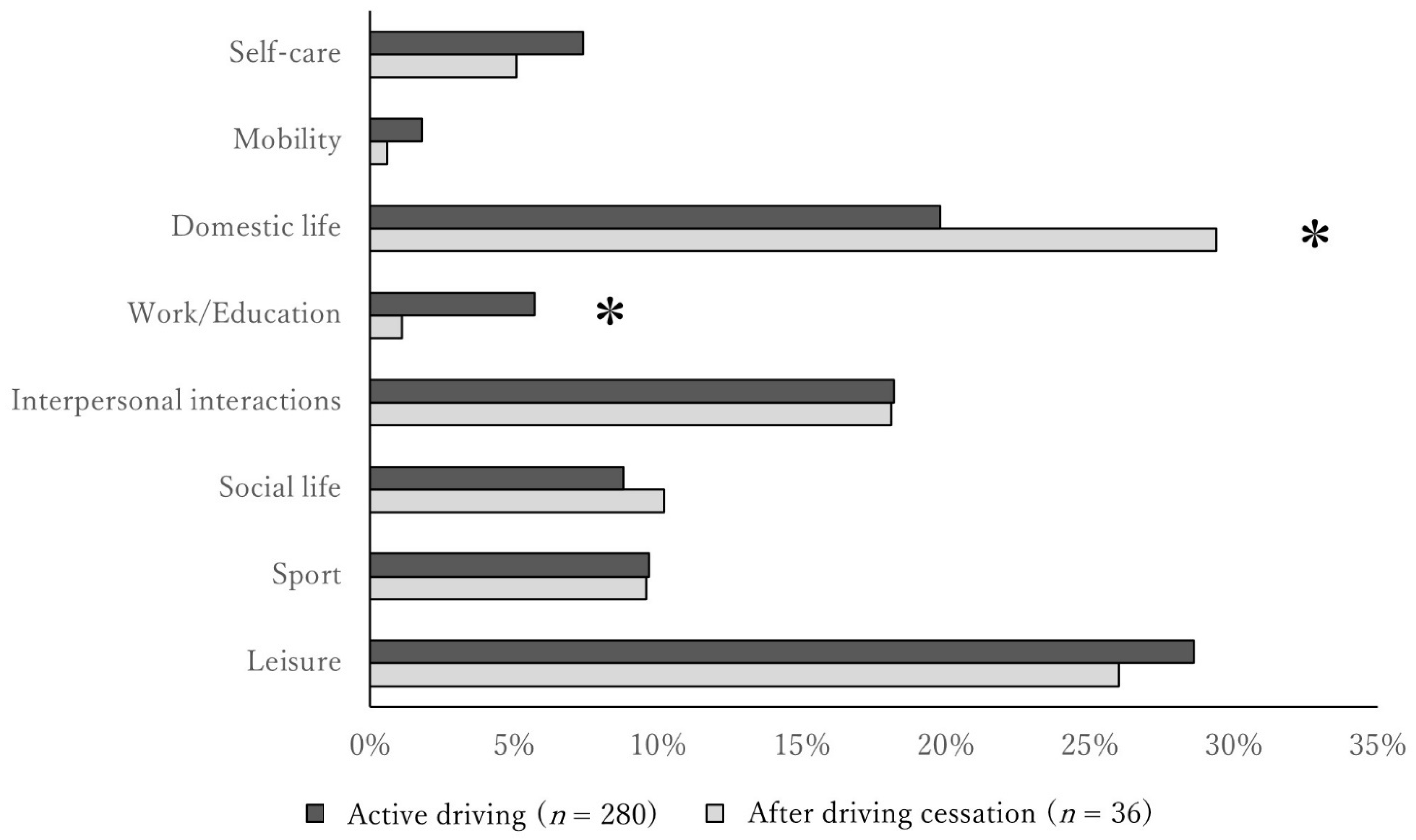
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- About the Characteristics of Traffic Accidents. Available online: https://www.npa.go.jp/publications/statistics/koutsuu/toukeihyo.html (accessed on 28 September 2020).
- Huisingh, C.; McGwin, G., Jr.; Owsley, C. Association of visual sensory function and higher-order visual processing skills with incident driving cessation. Clin. Exp. Opt. 2016, 99, 441–448. [Google Scholar] [CrossRef] [Green Version]
- Seiler, S.; Schmidt, H.; Lechner, A.; Benke, T.; Sanin, G.; Ransmayr, G.; Lehner, R.; Dal-Bianco, P.; Santer, P.; Linortner, P.; et al. Driving cessation and dementia: Results of the prospective registry on dementia in Austria (PRODEM). PLoS ONE 2012, 7, e52710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Edwards, J.D.; Lunsman, M.; Perkins, M.; Rebok, G.W.; Roth, D.L. Driving cessation and health trajectories in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 1290–1295. [Google Scholar] [CrossRef] [Green Version]
- Shimada, H.; Makizako, H.; Tsutsumimoto, K.; Hotta, R.; Nakakubo, S.; Doi, T. Driving and incidence of functional limitation in older people: A prospective population-based study. Gerontology 2016, 62, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Hirai, H.; Ichikawa, M.; Kondo, N.; Kondo, K. The risk of functional limitations driving cessation among older Japanese adults: The JAGES cohort study. J. Epidemiol. 2020, 30, 332–337, JE20180260. [Google Scholar] [CrossRef] [Green Version]
- Choi, M.; Lohman, M.C.; Mezuk, B. Trajectories of cognitive decline by driving mobility: Evidence from the Health and Retirement Study. Int. J. Geriatr. Psychiatry 2014, 29, 447–453. [Google Scholar] [CrossRef] [Green Version]
- Marottoli, R.A.; de Leon, C.F.M.; Glass, T.A.; Williams, C.S.; Cooney, L.M., Jr.; Berkman, L.F.; Tinetti, M.E. Driving cessation and increased depressive symptoms: Prospective evidence from the New Haven EPESE. J. Am. Geriatr. Soc. 1997, 45, 202–206. [Google Scholar] [CrossRef]
- Chihuri, S.; Mielenz, T.J.; DiMaggio, C.J.; Betz, M.E.; DiGuiseppi, C.; Jones, V.C.; Li, G. Driving cessation and health outcomes in older adults. J. Am. Geriatr. Soc. 2016, 64, 332–341. [Google Scholar] [CrossRef]
- Ragland, D.R.; Satariano, W.A.; MacLeod, K.E. Driving cessation and increased depressive symptoms. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 399–403. [Google Scholar] [CrossRef] [Green Version]
- Crowe, C.L.; Kannoth, S.; Andrews, H.; Strogatz, D.; Li, G.; DiGuiseppi, C.; Hill, L.; Eby, D.W.; Molnar, L.J.; Mielenz, T.J. Associations of frailty status with low-mileage driving and driving cessation in a cohort of older drivers. Geriatrics 2020, 5, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lenardt, M.H.; Cechinel, C.; Binotto, M.A.; Kolb Carneiro, N.H.; Lourenço, T.M. Physical frailty and fitness of older driver. Colomb. Med. 2017, 48, 41–46. [Google Scholar] [CrossRef] [Green Version]
- Edwards, J.D.; Perkins, M.; Ross, L.A.; Reynolds, S.L. Driving status and three-year mortality among community-dwelling older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 300–305. [Google Scholar] [CrossRef] [Green Version]
- Al-Hassani, S.B.; Alotaibi, N.M. The impact of driving cessation on older Kuwaiti adults: Implications to occupational therapy. Occup. Ther. Health Care 2014, 28, 264–276. [Google Scholar] [CrossRef]
- Mezuk, B.; Rebok, G.W. Social integration and social support among older adults following driving cessation. J. Gerontol. B Psychol. Sci. Soc. Sci. 2008, 63, S298–S303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curl, A.L.; Stowe, J.D.; Cooney, T.M.; Proulx, C.M. Giving up the keys: How driving cessation affects engagement in later life. Gerontologist 2014, 54, 423–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eakman, A.M.; Carlson, M.E.; Clark, F.A. The meaningful activity participation assessment: A measure of engagement in personally valued activities. Int. J. Aging Hum. Dev. 2010, 70, 299–317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rantanen, T.; Pynnönen, K.; Saajanaho, M.; Siltanen, S.; Karavirta, L.; Kokko, K.; Karvonen, A.; Kauppinen, M.; Rantalainen, T.; Rantakokko, M.; et al. Individualized counselling for active aging: Protocol of a single-blinded, randomized controlled trial among older people (the AGNES intervention study). BMC Geriatr. 2019, 19, 5:1–5:14. [Google Scholar] [CrossRef]
- W.H.O. Active Ageing: A Policy Framework; World Health Organization: Geneva, Swizerland, 2002. [Google Scholar]
- Moyers, P.A. The guide to occupational therapy practice. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 1999, 53, 247–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maruta, M.; Makizako, H.; Ikeda, Y.; Miyata, H.; Nakamura, A.; Han, G.; Shimokihara, S.; Tokuda, K.; Kubozono, T.; Ohishi, M.; et al. Associations between depressive symptoms and satisfaction with meaningful activities in community-dwelling Japanese older adults. J. Clin. Med. 2020, 9, 795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eakman, A.M.; Carlson, M.E.; Clark, F.A. Factor structure, reliability and convergent validity of the engagement in meaningful activities survey for older adults. OTJR (Thorofare N. J.) 2010, 30, 111–121. [Google Scholar] [CrossRef]
- Castelblanque, E.M.; Cunat, V.A.; Martinez, J.A. Life-style activities in older people without intellectual impairment: A population-based study. Rural. Remote Health 2005, 5, 344. [Google Scholar] [CrossRef]
- Marottoli, R.A.; de Leon, C.F.M.; Glass, T.A.; Williams, C.S.; Cooney, L.M., Jr.; Berkman, L.F. Consequences of driving cessation: Decreased out-of-home activity levels. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000, 55, S334–S340. [Google Scholar] [CrossRef]
- Strogatz, D.; Mielenz, T.J.; Johnson, A.K.; Baker, I.R.; Robinson, M.; Mebust, S.P.; Andrews, H.F.; Betz, M.E.; Eby, D.W.; Johnson, R.M.; et al. Importance of Driving and Potential Impact of Driving Cessation for Rural and Urban Older Adults. J. Rural. Health 2020, 36, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Tomori, K.; Uezu, S.; Kinjo, S.; Ogahara, K.; Nagatani, R.; Higashi, T. Utilization of the iPad application: Aid for decision-making in occupation choice. Occup. Ther. Int. 2012, 19, 88–97. [Google Scholar] [CrossRef]
- Suto, M. Leisure in occupational therapy. Can. J. Occup. Ther. 1998, 65, 271–278. [Google Scholar] [CrossRef]
- Levack, W.; Tomori, K.; Takahashi, K.; Sherrington, A.J. Development of an English-language version of a Japanese iPad application to facilitate collaborative goal setting in rehabilitation: A Delphi study and field test. BMJ Open 2018, 8, e018908. [Google Scholar] [CrossRef] [PubMed]
- Tomori, K.; Saito, Y.; Nagayama, H.; Seshita, Y.; Ogahara, K.; Nagatani, R.; Higashi, T. Reliability and validity of individualized satisfaction score in aid for decision-making in occupation choice. Disabil. Rehabil. 2013, 35, 113–117. [Google Scholar] [CrossRef]
- Nagayama, H.; Tomori, K.; Ohno, K.; Takahashi, K.; Ogahara, K.; Sawada, T.; Uezu, S.; Nagatani, R.; Yamauchi, K. Effectiveness and Cost-effectiveness of occupation-based occupational therapy using the Aid for Decision Making in Occupation Choice (ADOC) for older residents: Pilot cluster randomized controlled trial. PLoS ONE 2016, 11, e0150374. [Google Scholar] [CrossRef] [Green Version]
- Ally, B.A.; Waring, J.D.; Beth, E.H.; McKeever, J.D.; Milberg, W.P.; Budson, A.E. Aging memory for pictures: Using high-density event-related potentials to understand the effect of aging on the picture superiority effect. Neuropsychologia 2008, 46, 679–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herrmann, N.; Rapoport, M.J.; Sambrook, R.; Hébert, R.; McCracken, P.; Robillard, A. Predictors of driving cessation in mild-to-moderate dementia. Cmaj 2006, 175, 591–595. [Google Scholar] [CrossRef] [Green Version]
- Yesavage, J.A. Geriatric depression scale. Psychopharmacol. Bull. 1988, 24, 709–711. [Google Scholar]
- Bertens, A.S.; Moonen, J.E.F.; de Waal, M.W.M.; Foster-Dingley, J.C.; de Ruijter, W.; Gussekloo, J.; van der Mast, R.C.; de Craen, A.J.M. Validity of the three apathy items of the Geriatric Depression Scale (GDS-3A) in measuring apathy in older persons. Int. J. Geriatr. Psychiatry 2017, 32, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Marin, R.S. Differential diagnosis and classification of apathy. Am. J. Psychiatry 1990, 147, 22–30. [Google Scholar] [CrossRef] [Green Version]
- Borson, S.; Scanlan, J.; Brush, M.; Vitaliano, P.; Dokmak, A. The mini-cog: A cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int. J. Geriatr. Psychiatry 2000, 15, 1021–1027. [Google Scholar] [CrossRef]
- Borson, S.; Scanlan, J.M.; Watanabe, J.; Tu, S.P.; Lessig, M. Simplifying detection of cognitive impairment: Comparison of the Mini-Cog and Mini-Mental State Examination in a multiethnic sample. J. Am. Geriatr. Soc. 2005, 53, 871–874. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Doi, T.; Tsutsumimoto, K.; Suzuki, T. Impact of physical frailty on disability in community-dwelling older adults: A prospective cohort study. BMJ Open 2015, 5, e008462. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Park, H.; Doi, T.; Yoshida, D.; Uemura, K.; Tsutsumimoto, K.; Suzuki, T. Evaluation of multidimensional neurocognitive function using a tablet personal computer: Test-retest reliability and validity in community-dwelling older adults. Geriatr. Gerontol. Int. 2013, 13, 860–866. [Google Scholar] [CrossRef]
- Shimada, H.; Doi, T.; Lee, S.; Makizako, H.; Chen, L.; Arai, H. Cognitive frailty predicts incident dementia among community-dwelling older people. J. Clin. Med. 2018, 7, 250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makizako, H.; Shimada, H.; Tsutsumimoto, K.; Lee, S.; Doi, T.; Nakakubo, S.; Hotta, R.; Suzuki, T. Social frailty in community-dwelling older adults as a risk factor for disability. J. Am. Med. Dir. Assoc. 2015, 16, 1003.e7–1003.e11. [Google Scholar] [CrossRef] [PubMed]
- Iwasa, H.; Masui, Y.; Inagaki, H.; Yoshida, Y.; Shimada, H.; Otsuka, R.; Kikuchi, K.; Nonaka, K.; Yoshida, H.; Yoshida, H.; et al. Development of the Japan Science and Technology Agency Index of Competence to assess functional capacity in older adults: Conceptual definitions and preliminary items. Gerontol. Geriatr. Med. 2015, 1, 2333721415609490. [Google Scholar] [CrossRef] [Green Version]
- Iwasa, H.; Masui, Y.; Inagaki, H.; Yoshida, Y.; Shimada, H.; Otsuka, R.; Kikuchi, K.; Nonaka, K.; Yoshida, H.; Yoshida, H.; et al. Assessing competence at a higher level among older adults: Development of the Japan Science and Technology Agency Index of Competence (JST-IC). Aging Clin. Exp. Res. 2018, 30, 383–393. [Google Scholar] [CrossRef]
- Minami, U.; Nishi, M.; Fukaya, T.; Hasebe, M.; Nonaka, K.; Koike, T.; Suzuki, H.; Murayama, Y.; Uchida, H.; Fujiwara, Y. Effects of the change in working status on the health of older people in Japan. PLoS ONE 2015, 10, e0144069. [Google Scholar] [CrossRef] [Green Version]
- Abe, T.; Okuyama, K.; Kamada, M.; Yano, S.; Toyama, Y.; Isomura, M.; Nabika, T.; Sakane, N.; Ando, H.; Miyazaki, R. Social participation and physical prefrailty in older Japanese adults: The Shimane CoHRE study. PLoS ONE 2020, 15, e0243548. [Google Scholar] [CrossRef]
- Jolly, S.; Griffith, K.A.; DeCastro, R.; Stewart, A.; Ubel, P.; Jagsi, R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann. Intern. Med. 2014, 160, 344–353. [Google Scholar] [CrossRef] [Green Version]
- Windsor, T.D.; Anstey, K.J. Interventions to reduce the adverse psychosocial impact of driving cessation on older adults. Clin. Interv. Aging 2006, 3, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Slims, R.V.; Ahmed, A.; Sawyer, P.; Alman, R.M. Self-reported health and driving cessation in community-dwelling older drivers. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 789–793. [Google Scholar] [CrossRef]
- Gill, T.M.; Gahbauer, E.A.; Murphy, T.E.; Han, L.; Allore, H.G. Risk factors and precipitants of long-term disability in community mobility: A cohort study of older persons. Ann. Intern. Med. 2012, 17, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Mielenz, T.J.; Durbin, L.L.; Cisewski, J.A.; Guralnik, J.M.; Li, G. Select physical performance measures and driving outcomes in older adults. Inj. Epidemiol. 2017, 4, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musselwhite, C.B.A.; Shergold, I. Examining the process of driving cessation in later life. Eur. J. Ageing 2013, 10, 89–100. [Google Scholar] [CrossRef] [Green Version]
- Albert, G.; Lotan, T.; Weiss, P.; Shiftan, Y. The challenge of safe driving among elderly drivers. Healthc. Technol. Lett. 2018, 5, 45–48. [Google Scholar] [CrossRef] [PubMed]
| Group | p Value | ||
|---|---|---|---|
| Active Driving (n = 549) | After Driving Cessation (n = 45) | ||
| Age (Years) | 73.1 ± 5.6 | 77.1 ± 6.5 | <0.001 a |
| Women, n (%) | 280 (51.0) | 36 (80.0) | <0.001 b |
| Education (Years) | 11.5 ± 2.4 | 11.0 ± 1.8 | 0.131 a |
| Medication (Numbers) | 3.56 ± 4.4 | 5.51 ± 4.3 | 0.005 a |
| BMI (kg/m2) | 23.4 ± 3.2 | 23.3 ± 3.4 | 0.871 a |
| Grip strength (kg) | 27.0 ± 7.0 | 21.8 ± 6.8 | <0.001 a |
| JST-IC (Points) | 12.1 ± 2.9 | 9.96 ± 2.7 | <0.001 a |
| GDS (Points) | 2.32 ± 2.4 | 2.95 ± 2.6 | 0.118 a |
| Depression, n (%) | 80 (14.6) | 10 (22.7) | 0.147 b |
| Apathy, n (%) | 115 (20.9) | 17 (37.8) | 0.009 b |
| Poor Cognition, n (%) | 92 (16.8) | 7 (15.6) | 0.835 b |
| Living Alone, n (%) | 119 (20.9) | 18 (40.0) | 0.003 b |
| Physical frailty, n (%) | 7 (1.3) | 5 (11.1) | 0.001 b |
| Cognitive frailty, n (%) | 47 (8.6) | 7 (15.6) | 0.102 b |
| Social frailty, n (%) | 61 (11.1) | 12 (26.7) | 0.002 b |
| Satisfaction with Activity | 4.0 (4.0–5.0) | 4.0 (3.3–5.0) | 0.266 c |
| Performance of Activity | 8.0 (7.0–10.0) | 8.0 (7.0–10.0) | 0.655 c |
| No. | Active Driving Group (n = 549) | After Driving Cessation Group (n = 45) | ||
|---|---|---|---|---|
| Domestic life | 1 | Cooking meals (27.0%) | 1 | Cooking meals (36.7%) |
| 2 | Collecting information (14.7%) | 2 | Shopping (11.6%) | |
| 3 | Shopping (14.5%) | Laundry (11.6%) | ||
| 4 | Cleaning (11.5%) | 4 | Cleaning (10.0%) | |
| 5 | Laundry (10.6%) | 5 | Collecting information (8.3%) | |
| 6 | Child Care (6.0%) | 6 | Management of property (6.7%) | |
| 7 | Assisting old people/patients (4.0%) | 7 | Making and repairing clothes (5.0%) | |
| 8 | Household maintenance (3.5%) | Child Care (5.0%) | ||
| 9 | Management of property (3.0%) | 9 | Household maintenance (1.7%) | |
| 10 | Maintaining vehicles/appliances (2.5%) | Assisting old people/patients (1.7%) | ||
| 11 | Makeup (1.4%) | Barbershop (1.7%) | ||
| 12 | Making and repairing clothes (0.9%) | |||
| 13 | Writing a letter/document (0.2%) | |||
| Barbershop (0.2%) | ||||
| Work/Education | 1 | Remunerative employment (56.4%) | 1 | Remunerative employment (66.7%) |
| 2 | Non-remunerative employment (38.5%) | 2 | Non-remunerative employment (33.3%) | |
| 3 | Informal education (4.5%) | |||
| 4 | School education (0.6%) |
| Group | p Value | ||
|---|---|---|---|
| Active Driving (n = 280) | After Driving Cessation (n = 36) | ||
| Age (Years) | 72.1 ± 5.0 | 77.6 ± 6.6 | <0.001 a |
| Education (Years) | 11.3 ± 1.9 | 10.9 ± 1.7 | 0.243 a |
| Medication (Number) | 3.18 ± 3.5 | 5.5 ± 4.2 | <0.001 a |
| BMI (kg/m2) | 23.1 ± 3.4 | 23.8 ± 3.5 | 0.273 a |
| Grip strength (kg) | 22.3 ± 4.2 | 19.6 ± 4.1 | <0.001 a |
| JST-IC (Points) | 12.6 ± 2.6 | 10.2 ± 2.5 | <0.001 a |
| GDS (Points) | 2.4 ± 2.4 | 3.0 ± 2.5 | 0.181 a |
| Depression, n (%) | 43 (15.4) | 8 (22.9) | 0.256 b |
| Apathy, n (%) | 68 (24.3) | 14 (38.9) | 0.060 b |
| Poor Cognition, n (%) | 35 (12.5) | 4 (11.1) | 0.534 b |
| Living Alone, n (%) | 73 (26.1) | 14 (38.9) | 0.105 b |
| Physical frailty, n (%) | 1 (0.4) | 3 (8.3) | 0.005 b |
| Cognitive frailty, n (%) | 14 (5.0) | 5 (13.9) | 0.051 b |
| Social frailty, n (%) | 24 (8.6) | 8 (22.2) | 0.018 b |
| Satisfaction with Activity | 4.0 (4.0–5.0) | 4.0 (3.3–5.0) | 0.178 c |
| Performance of Activity | 7.0 (7.0–10.0) | 10.0 (8.0–10.0) | 0.281 c |
| Group | p Value | |||
|---|---|---|---|---|
| High-Frequency (n = 387) | Medium (n = 119) | Infrequent (n = 42) | ||
| Age, mean ± SD (Years) | 73.1 ± 5.5 | 73.2 ± 5.6 | 73.7 ± 6.5 | 0.745 a |
| Women, n (%) | 185 (47.8) | 70 (58.8) | 25 (59.5) | 0.057 b |
| Education, mean ± SD (Years) | 11.5 ± 2.4 | 11.6 ± 2.2 | 11.6 ± 2.5 | 0.721 a |
| Medication ± SD (Number) | 3.7 ± 4.8 | 3.2 ± 3.4 | 3.0 ± 3.4 | 0.319 a |
| BMI, mean ± SD (Kg/m2) | 23.1 ± 3.4 | 23.8 ± 3.5 | 23.1 ± 4.0 | 0.273 a |
| Grip strength, mean ± SD (Kg) | 27.5 ± 7.1 | 26.0 ± 7.1 | 25.0 ± 4.7 | 0.007 a |
| JST-IC, mean ± SD (Points) | 12.1 ± 2.9 | 12.2 ± 2.8 | 11.6 ± 3.0 | 0.445 a |
| GDS, mean ± (Points) | 2.2 ± 2.3 | 2.6 ± 2.7 | 2.8 ± 2.4 | 0.124 a |
| Depression, n (%) | 48 (12.4) | 22 (18.5) | 10 (23.8) | 0.055 b |
| Apathy, n (%) | 66 (17.1) | 33 (27.7) | 16 (38.1) | 0.001 b |
| Poor Cognition, n (%) | 71 (18.3) | 15 (12.6) | 6 (14.3) | 0.309 b |
| Living Alone, n (%) | 81 (20.9) | 27 (22.7) | 7 (16.7) | 0.711 b |
| Physical frailty, n (%) | 4 (1.0) | 2 (1.7) | 1 (2.4) | 0.690 b |
| Cognitive frailty, n (%) | 30 (7.8) | 16 (34.0) | 1 (2.4) | 0.050 b |
| Social frailty, n (%) | 35 (9.0) | 17 (14.3) | 9 (21.4) | 0.025 b |
| Satisfaction with Activity, Median (IQR) | 4.0 (4.0–5.0) | 4.0 (4.0–5.0) | 4.0 (3.0–5.0) | 0.289 c |
| Performance of Activity, Median (IQR) | 8.0 (7.0–10.0) | 8.0 (7.0–10.0) | 9.0 (7.0–10.0) | 0.642 c |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakamura, A.; Maruta, M.; Makizako, H.; Miyata, M.; Miyata, H.; Han, G.; Ikeda, Y.; Shimokihara, S.; Tokuda, K.; Kubozono, T.; et al. Meaningful Activities and Psychosomatic Functions in Japanese Older Adults after Driving Cessation. Int. J. Environ. Res. Public Health 2021, 18, 13270. https://doi.org/10.3390/ijerph182413270
Nakamura A, Maruta M, Makizako H, Miyata M, Miyata H, Han G, Ikeda Y, Shimokihara S, Tokuda K, Kubozono T, et al. Meaningful Activities and Psychosomatic Functions in Japanese Older Adults after Driving Cessation. International Journal of Environmental Research and Public Health. 2021; 18(24):13270. https://doi.org/10.3390/ijerph182413270
Chicago/Turabian StyleNakamura, Atsushi, Michio Maruta, Hyuma Makizako, Masaaki Miyata, Hironori Miyata, Gwanghee Han, Yuriko Ikeda, Suguru Shimokihara, Keiichiro Tokuda, Takuro Kubozono, and et al. 2021. "Meaningful Activities and Psychosomatic Functions in Japanese Older Adults after Driving Cessation" International Journal of Environmental Research and Public Health 18, no. 24: 13270. https://doi.org/10.3390/ijerph182413270
APA StyleNakamura, A., Maruta, M., Makizako, H., Miyata, M., Miyata, H., Han, G., Ikeda, Y., Shimokihara, S., Tokuda, K., Kubozono, T., Ohishi, M., & Tabira, T. (2021). Meaningful Activities and Psychosomatic Functions in Japanese Older Adults after Driving Cessation. International Journal of Environmental Research and Public Health, 18(24), 13270. https://doi.org/10.3390/ijerph182413270








