COVID-19 Vaccine Early Skepticism, Misinformation and Informational Needs among Essential Workers in the USA
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
3.1. Sample Characteristics
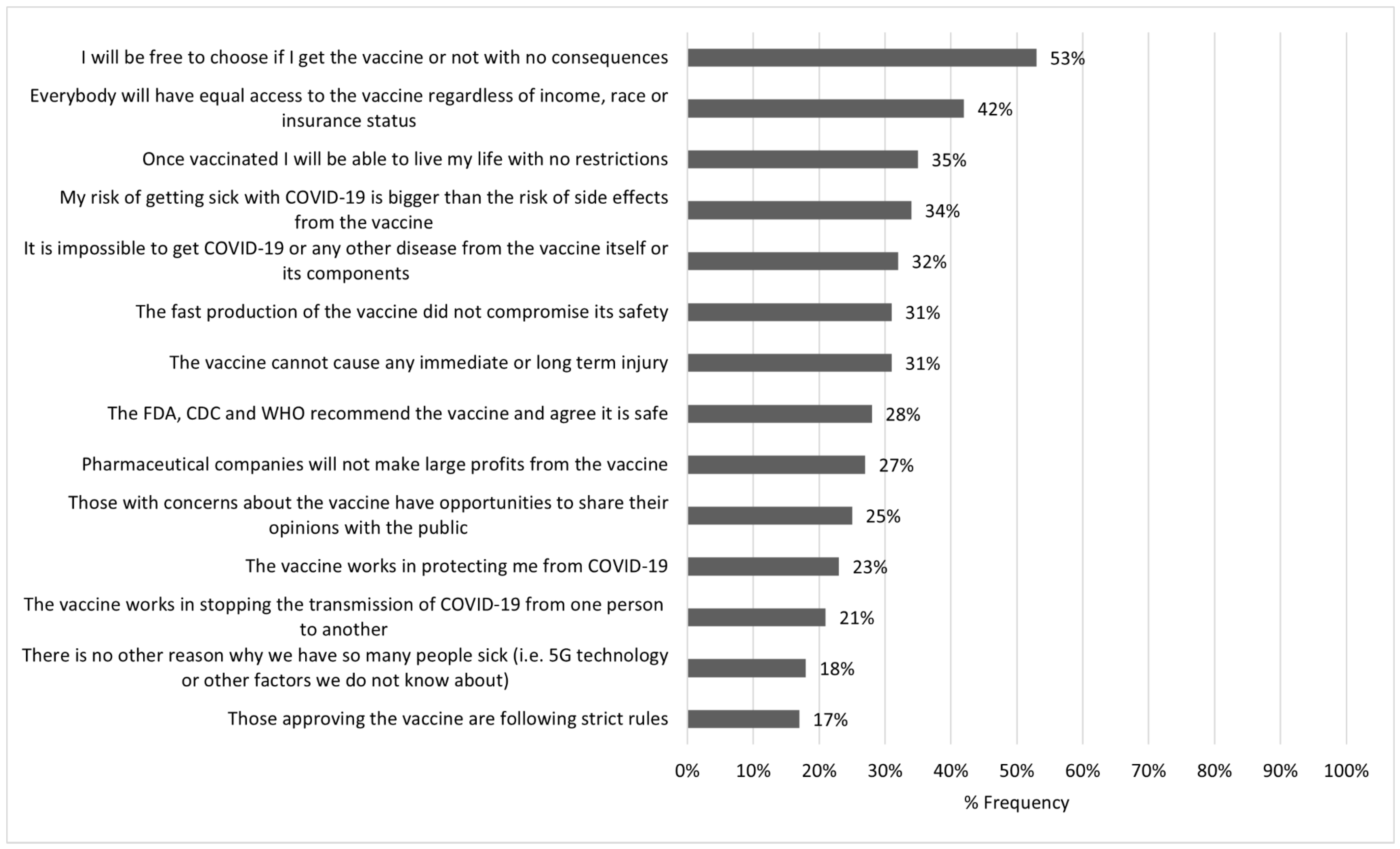
3.2. Top Informational Needs
3.3. Informational Needs on the COVID-19 Vaccine Safety and Effectivenes
3.3.1. Informational Needs on Safety and Effectiveness by Vaccine Acceptance
3.3.2. Informational Needs on Safety and Effectiveness by Sociodemographics
3.3.3. Informational Needs on Safety and Effectiveness by Use of Social Media
3.4. Informational Needs on the COVID-19 Vaccine Policies
3.4.1. Informational Needs on Vaccine Policies by Vaccine Acceptance
3.4.2. Informational Needs on Vaccine Policies by Sociodemographics
3.4.3. Informational Needs on Vaccine Policies by Use of Social Media
3.4.4. Informational Needs Found to Be Positively Associated with Vaccine Acceptance in the Univariate Analysis
3.5. Logistic Regression Model
4. Discussion
4.1. Limitations
4.2. Recommendations for Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- SteelFisher, G.K.; Blendon, R.J.; Caporello, H. An Uncertain Public—Encouraging Acceptance of Covid-19 Vaccines. N. Engl. J. Med. 2021, 384, 1483–1487. [Google Scholar] [CrossRef] [PubMed]
- CDC COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (accessed on 9 August 2021).
- Identifying Critical Infrastructure during COVID-19. Available online: https://www.cisa.gov/identifying-critical-infrastructure-during-covid-19 (accessed on 9 August 2021).
- Baker, M.G.; Peckham, T.K.; Seixas, N.S. Estimating the burden of United States workers exposed to infection or disease: A key factor in containing risk of COVID-19 infection. PLoS ONE 2020, 15, e0232452. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. The plight of essential workers during the COVID-19 pandemic. Lancet 2020, 395, 1587. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Guidance on the Essential Critical Infrastructure Workforce. Available online: https://www.cisa.gov/publication/guidance-essential-critical-infrastructure-workforce (accessed on 29 July 2021).
- Dooling, K.; McClung, N.; Chamberland, M.; Marin, M.; Wallace, M.; Bell, B.P.; Lee, G.M.; Talbot, H.K.; Romero, J.R.; Oliver, S.E. The Advisory Committee on Immunization Practices’ Interim Recommendation for Allocating Initial Supplies of COVID-19 Vaccine—United States, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1857–1859. [Google Scholar] [CrossRef] [PubMed]
- Dooling, K.; Marin, M.; Wallace, M.; McClung, N.; Chamberland, M.; Lee, G.M.; Talbot, H.K.; Romero, J.R.; Bell, B.P.; Oliver, S.E. The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine—United States, December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 69, 1657–1660. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, K.H.; Srivastav, A.; Razzaghi, H.; Williams, W.; Lindley, M.C.; Jorgensen, C.; Abad, N.; Singleton, J.A. COVID-19 Vaccination Intent, Perceptions, and Reasons for Not Vaccinated among Groups Prioritized for Early Vaccination—United States, September and December 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Cantor, J.; Simon, K.I.; Bento, A.I.; Wing, C.; Whaley, C.M. Vaccinations Against COVID-19 May Have Averted Up To 140,000 Deaths in the United States. Health Aff. 2021, 40, 1465–1472. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Vaccines and Herd Immunity. Available online: https://ccdd.hsph.harvard.edu/2020/12/17/covid-19-vaccines-and-herd-immunity/ (accessed on 19 August 2021).
- KFF COVID-19 Vaccine Monitor: Vaccine Attitudes among Essential Workers. Available online: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-vaccine-attitudes-among-essential-workers/ (accessed on 9 August 2021).
- Centola, D. The spread of behavior in an online social network experiment. Science 2010, 329, 1194–1197. [Google Scholar] [CrossRef] [PubMed]
- CERC: Psychology of a Crisis. Centers for Disease Control and Prevention. Available online: https://emergency.cdc.gov/cerc/ppt/CERC_Psychology_of_a_Crisis.pdf (accessed on 13 July 2021).
- COVID-19 Vaccination Program Interim Playbook for Jurisdictional Operations. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/vaccines/imz-managers/downloads/COVID-19-Vaccination-Program-Interim_Playbook.pdf (accessed on 11 January 2021).
- Categories of Essential Workers: COVID-19 Vaccination. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/vaccines/covid-19/categories-essential-workers.html (accessed on 9 August 2021).
- Hughes, B.; Miller-Idriss, C.; Piltch-Loeb, R.; Goldberg, B.; White, K.; Criezis, M.; Savoia, E. Development of a Codebook of Online Anti-Vaccination Rhetoric to Manage COVID-19 Vaccine Misinformation. Int. J. Environ. Res. Public Health 2021, 18, 7556. [Google Scholar] [CrossRef] [PubMed]
- Savoia, E.; Piltch-Loeb, R.; Goldberg, B.; Miller-Idriss, C.; Hughes, B.; Montrond, A.; Kayyem, J.; Testa, M.A. Predictors of COVID-19 Vaccine Hesitancy: Socio-Demographics, Co-Morbidity, and Past Experience of Racial Discrimination. Vaccines 2021, 9, 767. [Google Scholar] [CrossRef] [PubMed]
- Piltch-Loeb, R.; Savoia, E.; Goldberg, B.; Hughes, B.; Verhey, T.; Kayyem, J.; Miller-Idriss, C.; Testa, M. Examining the effect of information channel on COVID-19 vaccine acceptance. PLoS ONE 2021, 16, e0251095. [Google Scholar] [CrossRef] [PubMed]
- Public Health Emergency Preparedness and Response Capabilities: National Standards for State, Local, Tribal, and Territorial Public Health. Available online: https://www.cdc.gov/cpr/readiness/capabilities.htm (accessed on 13 July 2021).
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef] [PubMed]
- Jamison, A.M.; Quinn, S.C.; Freimuth, V.S. “You don’t trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. Soc. Sci. Med. 2019, 221, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Hamel, L.; Kirzinger, A.; Munana, C.; Brodie, M. KFF COVID-19 Vaccine Monitor. Press Release. December 2020. Available online: https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/?utm_campaign=KFF-2020-polling-surveys&utm_medium=email&_hsmi=2&_hsenc=p2ANqtz-9EpdM8wscJHy__FjpP9PJ67CUSXfk4f_VyZdVC652V5zIy4qBzDeO-0b5iDXeDertNU8W0VOp6xcGENlKJvugasI_0OA&utm_content=2&utm_source=hs_email (accessed on 8 January 2021).
- Largent, E.A.; Persad, G.; Sangenito, S.; Glickman, A.; Boyle, C.; Emanuel, E.J. US Public Attitudes Toward COVID-19 Vaccine Mandates. JAMA Netw. Open 2020, 3, e2033324. [Google Scholar] [CrossRef] [PubMed]
- Steffens, M.S.; Dunn, A.G.; Leask, J.; Wiley, K.E. Using social media for vaccination promotion: Practices and challenges. Digit. Health 2020, 9, 1126. [Google Scholar] [CrossRef]
- Hilbert, M.; Vásquez, J.; Halpern, D.; Valenzuela, S.; Arriagada, E. One step, two step, network step? Complementary perspectives on communication flows in Twittered citizen protests. Soc. Sci. Comput. Rev. 2017, 35, 444–461. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.; Lustria, M.L.A.; Burke, D.; Kwon, N. Predictors of cancer information overload: Findings from a national survey. Inf. Res. 2007, 12, 12–14. [Google Scholar]
| Demographics/Characteristics | n (%) |
|---|---|
| Age | |
| 18–24 | 212 (13.3) |
| 25–34 | 518 (32.6) |
| 35–44 | 539 (33.9) |
| 45–54 | 199 (12.5) |
| 55+ | 123 (7.7) |
| Gender (N = 1581) | |
| Male | 874 (55.3) |
| Female | 707 (44.7) |
| Race/ethnicity | |
| White, Non-H | 1048 (65.9) |
| Black, Non-H | 242 (15.2) |
| Hispanic | 119 (7.5) |
| Non-H Asian | 73 (4.6) |
| Multi/Other | 109 (6.9) |
| Education (N = 1584) | |
| HS/less | 375 (23.7) |
| Some college | 326 (20.6) |
| Bachelor’s degree | 363 (22.9) |
| Postgraduate degree | 520 (32.8) |
| Vaccine Acceptance | |
| I would not take it within 2 months | 188 (11.8) |
| Very unlikely | 339 (21.3) |
| Somewhat unlikely | 153 (9.6) |
| I am not sure | 388 (24.4) |
| Somewhat likely | 523 (32.9) |
| Get most information about COVID-19 vaccine from social media? * (N = 1334) | |
| No | 925 (69.3) |
| Yes | 409 (30.7) |
| Job category (multiple choice question) | |
| Hospital and emergency department workers | 624 (23.5) |
| Nursing home, long-term care, and home healthcare workers | 413 (15.6) |
| Public health workers | 284 (10.7) |
| Grocery store workers | 283 (10.7) |
| Teachers and school staff | 251 (9.5) |
| Food processing workers | 222 (8.4) |
| Emergency medical services workers | 186 (7.0) |
| Other healthcare workers | 170 (6.4) |
| Volunteer (i.e., CERT, MRC, Red Cross, etc.) | 168 (6.3) |
| Private transportation workers | 156 (5.9) |
| Sanitation workers | 131 (4.9) |
| Vaccine manufacturing workers | 121 (4.6) |
| Postal and shipping workers | 120 (4.5) |
| Pharmacy workers | 117 (4.4) |
| Correctional facilities workers | 116 (4.4) |
| Police or firefighters | 116 (4.4) |
| Vaccine distribution workers | 95 (3.6) |
| Other first responders | 93 (3.5) |
| Public transportation workers | 90 (3.4) |
| What Would Be Important for You to Know to Make You More Likely to Take the COVID-19 Vaccine? (N = 1591) | |
|---|---|
| Vaccine Acceptance | My risk of getting sick with COVID-19 is bigger than the risk of side effects from the vaccine. n (%) *,† |
| I would not take it within 2 months | 56 (29.8) |
| Very unlikely | 75 (22.1) ▼ |
| Somewhat unlikely | 56 (36.6) |
| I am not sure | 147 (37.9) |
| Somewhat likely | 206 (39.4) ▲ |
| Vaccine Acceptance | The vaccine cannot cause any immediate or long-term injury. n (%) *,† |
| I would not take it within 2 months | 74 (39.4) ▼ |
| Very unlikely | 116 (34.2) |
| Somewhat unlikely | 36 (23.5) |
| I am not sure | 126 (32.5) |
| Somewhat likely | 136 (26.0) |
| Vaccine Acceptance | There is no other reason why we have so many people sick (i.e., 5G technology or other logy or other factors we do not know about). n (%) † |
| I would not take it within 2 months | 32 (17.0) |
| Very unlikely | 49 (14.5) |
| Somewhat unlikely | 34 (22.2) |
| I am not sure | 69 (17.8) |
| Somewhat likely | 95 (18.2) |
| Vaccine Acceptance | The vaccine works in protecting me from COVID-19. n (%) *,† |
| I would not take it within 2 months | 44 (23.4) |
| Very unlikely | 58 (17.1) ▼ |
| Somewhat unlikely | 35 (22.9) |
| I am not sure | 84 (21.6) |
| Somewhat likely | 145 (27.7) ▲ |
| Vaccine Acceptance | The vaccine works in stopping the transmission of COVID-19 from one person to another. n (%) * |
| I would not take it within 2 months | 42 (22.3) |
| Very unlikely | 69 (20.4) |
| Somewhat unlikely | 17 (11.1) ▼ |
| I am not sure | 83 (21.4) |
| Somewhat likely | 118 (22.6) |
| Vaccine Acceptance | It is impossible to get COVID-19 or any other disease from the vaccine itself or its components. n (%) † |
| I would not take it within 2 months | 57 (30.3) |
| Very unlikely | 97 (28.6) |
| Somewhat unlikely | 42 (27.5) |
| I am not sure | 120 (30.9) |
| Somewhat likely | 193 (36.9) |
| Gender (N = 1581) | The vaccine cannot cause any immediate or long-term injury. n (%) * |
| Male | 288 (33.0) |
| Female | 196 (27.7) |
| Education (N = 1584) | The vaccine works in protecting me from COVID-19. n (%) † |
| HS/less | 95 (25.3) |
| Some college | 78 (23.9) |
| Bachelor’s degree | 92 (25.3) |
| Postgraduate degree | 100 (19.2) |
| Get most information about COVID-19 vaccine from social media? (N = 1334) | The fast production of the vaccine did not compromise its safety. n (%) * |
| No | 155 (37.9) ▲ |
| Yes | 271 (29.3) |
| Get most information about COVID-19 vaccine from social media? (N = 1334) | My risk of getting sick with COVID-19 is bigger than the risk of side effects from the vaccine. n (%) * |
| No | 164 (40.1) ▲ |
| Yes | 293 (31.7) |
| Get most information about COVID-19 vaccine from social media? (N = 1334) | The vaccine works in protecting me from COVID-19. n (%) * |
| No | 113 (27.6) |
| Yes | 194 (21.0) |
| Get most information about COVID-19 vaccine from social media? (N = 1334) | The vaccine works in stopping the transmission of COVID-19 from one person to another. n (%) * |
| No | 106 (25.9) ▲ |
| Yes | 170 (18.4) |
| Get most information about COVID-19 vaccine from social media? (N = 1334) | It is impossible to get COVID-19 or any other disease from the vaccine itself or its components. n (%) * |
| No | 149 (36.4) |
| Yes | 277 (29.9) |
| What Would Be Important for You to Know to Make You More Likely to Take the COVID-19 Vaccine? (N = 1591). | |||||||
|---|---|---|---|---|---|---|---|
| Demographics/Characteristics | Those Approving the Vaccine Are Following Strict Rules | The FDA, CDC and WHO Recommend the Vaccine and Agree It Is Safe | Once Vaccinated I Will Be Able To Live My Life With No Restrict-Ions (General Freedom) | Those With Concerns About the Vaccine Have Opportunities To Share Their Opinions With the Public (Freedom of Speech) | Pharmaceutical Companies Will Not Make Large Profits From the Vaccine | Everybody Will Have Equal Access to the Vaccine Regardless of Income, Race or Insurance Status (Equal Access) | I Will Be Free To Choose if I Receive the Vaccine or Not With No Consequences (Freedom of Health Choices) |
| Vaccine Acceptance n (%) *,† | n (%) *,† | n (%) *,† | n (%) | n (%) | n (%) *,† | n (%) *,† | |
| I would not take it within 2 months | 53 (28.2) ▲ | 51 (27.1) | 62 (33.0) | 55 (29.3) | 54 (28.7) | 83 (44.1) | 101 (53.7) |
| Very unlikely | 64 (18.9) | 64 (18.9) ▼ | 94 (27.7) ▼ | 96 (28.3) | 81 (23.9) | 103 (30.4) ▼ | 197 (58.1) |
| Somewhat unlikely | 22 (14.4) | 30 (19.6) | 49 (32.0) | 31 (20.3) | 40 (26.1) | 48 (31.4) ▼ | 85 (55.6) |
| I am not sure | 68 (17.5) | 122 (31.4) | 140 (36.1) | 103 (26.5) | 90 (23.2) | 168 (43.3) | 204 (52.6) |
| Somewhat likely | 70 (13.4) ▼ | 177 (33.8) ▲ | 214 (40.9) ▲ | 120 (22.9) | 158 (30.2) | 267 (51.1) ▲ | 249 (47.6) |
| Education (N = 1584) | † | *,† | * | ||||
| HS/less | 62 (16.5) | 119 (31.7) | 134 (35.7) | 106 (28.3) | 95 (25.3) | 162 (43.2) | 202 (53.9) |
| Some college | 59 (18.1) | 98 (30.1) | 104 (31.9) | 103 (31.6) ▲ | 93 (28.5) | 151 (46.3) | 156 (47.9) |
| Bachelor’s degree | 59 (16.3) | 94 (25.9) | 135 (37.2) | 80 (22.0) | 89 (24.5) | 155 (42.7) | 212 (58.4) |
| Postgraduate degree | 96 (18.5) | 132 (25.4) | 184 (35.4) | 115 (22.1) | 145 (27.9) | 200 (38.5) | 263 (50.6) |
| Get most information about COVID-19 vaccine from social media? (N = 1334) | |||||||
| No | 68 (16.6) | 138 (33.7) ▲ | 168 (41.1) | 112 (27.4) | 124 (30.3) | 219 (53.5) ▲ | 222 (54.3) |
| Yes | 157 (17.0) | 238 (25.7) | 320 (34.6) | 224 (24.2) | 223 (24.1) | 344 (37.2) ▼ | 481 (52.0) |
| How Likely Are You to Take a COVID-19 Vaccine If Offered to You at No Cost within Two Months (Very Likely, Somewhat Likely, I Would Not Take It within Two Months but Consider It Later, Not Sure, Somewhat Unlikely, Very Unlikely) | What Would Be Important for You to Know to Make You More Likely to Take the COVID-19 Vaccine? |
|---|---|
| Respondents reporting somewhat likely |
|
| I would not take it within two months but consider it later |
|
| Variable | OR | 95% C.I. |
|---|---|---|
| Age | 0.97 | 0.88–1.08 |
| Gender (Female versus Male) | 0.99 | 0.79–1.26 |
| White non-Hispanic versus other races | 0.89 | 0.70–1.15 |
| Education | ||
| Less than high school | - | - |
| High school/GED | 1.15 | 0.59–2.27 |
| Some college | 1.07 | 0.54–2.11 |
| Bachelor’s degree | 1.06 | 0.54–2.08 |
| Postgraduate degree | 1.33 | 0.69–2.60 |
| Social media as main source of COVID-19 vaccine information versus traditional media/mixed media | 1.18 | 0.91–1.52 |
| Informational needs (need of additional information in at least one of the seven topics selected versus no need of additional information) | 0.02 | 0.01–0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savoia, E.; Su, M.; Piltch-Loeb, R.; Masterson, E.; Testa, M.A. COVID-19 Vaccine Early Skepticism, Misinformation and Informational Needs among Essential Workers in the USA. Int. J. Environ. Res. Public Health 2021, 18, 13244. https://doi.org/10.3390/ijerph182413244
Savoia E, Su M, Piltch-Loeb R, Masterson E, Testa MA. COVID-19 Vaccine Early Skepticism, Misinformation and Informational Needs among Essential Workers in the USA. International Journal of Environmental Research and Public Health. 2021; 18(24):13244. https://doi.org/10.3390/ijerph182413244
Chicago/Turabian StyleSavoia, Elena, Maxwell Su, Rachael Piltch-Loeb, Evelyn Masterson, and Marcia A. Testa. 2021. "COVID-19 Vaccine Early Skepticism, Misinformation and Informational Needs among Essential Workers in the USA" International Journal of Environmental Research and Public Health 18, no. 24: 13244. https://doi.org/10.3390/ijerph182413244
APA StyleSavoia, E., Su, M., Piltch-Loeb, R., Masterson, E., & Testa, M. A. (2021). COVID-19 Vaccine Early Skepticism, Misinformation and Informational Needs among Essential Workers in the USA. International Journal of Environmental Research and Public Health, 18(24), 13244. https://doi.org/10.3390/ijerph182413244






