Exercise Training for Multiple Sclerosis: A Narrative Review of History, Benefits, Safety, Guidelines, and Promotion
Abstract
:1. Introduction
2. What We Know about Exercise in MS, Including a History of Benefits and Safety
2.1. Early Cases of Exercise in MS
“A gentleman aged 34, of a slender make and very active habits, was affected in the summer of 1815 with numbness and diminished sensibility of all extremities…along with diminution of muscular power. He could walk a considerable distance, though he did so with a feeling of insecurity and unsteadiness; but he could not …perform running leaping or very quick walking. He was in other respects in good health. Various remedies were employed, without benefit. He became determined to try the effect of violent exercise. For this purpose, he walked as hard as he was able, 5 or 6 miles in a warm evening, and returned home fatigued. Next morning he had severe pains in the calves of his legs, but his other complaints were much diminished, and in a few days disappeared. He has ever since enjoyed very good health”.
“(Hammond employed) the same therapies as others used. His approach was to give repeated courses of chloride of barium, iron, hyoscyamus, strychnine, nitrate of silver, and cod liver oil, in addition to recommending two glasses of wine daily and moderate exercise.”
“Patients with neurological disease were often treated with water therapy, spas, baths and douching. Commonly used physical measures for MS were galvanic and faradic stimulation, (physical treatments were) used throughout the 19th century.”
2.2. Dawn of the Randomised Controlled Exercise Trials
2.3. Growth of Clinical Trials and Expanding Knowledge of Benefits
2.4. Exercise Safety
3. What We Recommend Neurologists and MS Healthcare Providers Prescribe for Exercise Based on Recent Guidelines
3.1. Current Recommendation Guidelines
3.2. Understanding Theory to Overcome Exercise Barriers
4. Recommendations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Feys, P.; Giovannoni, G.; Dijsselbloem, N.; Centonze, D.; Eelen, P.; Lykke Andersen, S. The importance of a multi-disciplinary perspective and patient activation programmes in MS management. Mult. Scler. J. 2016, 22, 34–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, R. Atlas of MS 3rd Edition. PART 1: Mapping Multiple Sclerosis around the World Key Epidemiology Findings; Multiple Sclerosis International Federation: London, UK, 2020. [Google Scholar]
- Dobson, R.; Giovannoni, G. Multiple sclerosis—A review. Eur. J. Neurol. 2019, 26, 27–40. [Google Scholar] [CrossRef] [Green Version]
- Klaren, R.; Motl, R.W.; Dlugonski, D.; Sandroff, B.M.; Pilutti, L.A. Objectively Quantified Physical Activity in Persons with Multiple Sclerosis. Int. J. MS Care 2013, 94, 2342–2348. [Google Scholar] [CrossRef]
- Kinnett-Hopkins, D.; Adamson, B.; Rougeau, K.; Motl, R.W. People with MS are less physically active than healthy controls but as active as those with other chronic diseases: An updated meta-analysis. Mult. Scler. Relat. Disord. 2017, 13, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Casey, B.; Coote, S.; Galvin, R.; Donnelly, A. Objective physical activity levels in people with multiple sclerosis: Meta-analysis. Scand. J. Med. Sci. Sports 2018, 28, 1960–1969. [Google Scholar] [CrossRef]
- Marck, C.H.; Learmonth, Y.C.; Chen, J.; van der Mei, I. Physical activity, sitting time and exercise types, and associations with symptoms in Australian people with multiple sclerosis. Disabil. Rehabil. 2020. [Google Scholar] [CrossRef] [PubMed]
- Asche, C.V.; Singer, M.E.; Jhaveri, M.; Chung, H.; Miller, A. All-Cause Health Care Utilization and Costs Associated with Newly Diagnosed Multiple Sclerosis in the United States. J. Manag. Care Pharm. 2010, 16, 703–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. Wash. DC 1974 1985, 100, 126–131. [Google Scholar]
- Mahalakshmi, B.; Maurya, N.; Lee, S.-D.; Bharath Kumar, V. Possible Neuroprotective Mechanisms of Physical Exercise in Neurodegeneration. Int. J. Mol. Sci. 2020, 21, 5895. [Google Scholar] [CrossRef]
- Dalgas, U.; Langeskov-Christensen, M.; Stenager, E.; Riemenschneider, M.; Hvid, L.G. Exercise as Medicine in Multiple Sclerosis—Time for a Paradigm Shift: Preventive, Symptomatic, and Disease-Modifying Aspects and Perspectives. Curr. Neurol. Neurosci. Rep. 2019, 19, 1–12. [Google Scholar] [CrossRef]
- Gentile, A.; Musella, A.; De Vito, F.; Rizzo, F.R.; Fresegna, D.; Bullitta, S.; Vanni, V.; Guadalupi, L.; Stampanoni Bassi, M.; Buttari, F. Immunomodulatory effects of exercise in experimental multiple sclerosis. Front. Immunol. 2019, 10, 2197. [Google Scholar] [CrossRef] [PubMed]
- Negaresh, R.; Motl, R.W.; Zimmer, P.; Mokhtarzade, M.; Baker, J.S. Effects of exercise training on multiple sclerosis biomarkers of central nervous system and disease status: A systematic review of intervention studies. Eur. J. Neurol. 2019, 26, 711–721. [Google Scholar] [CrossRef]
- Kjølhede, T.; Siemonsen, S.; Wenzel, D.; Stellmann, J.-P.; Ringgaard, S.; Pedersen, B.G.; Stenager, E.; Petersen, T.; Vissing, K.; Heesen, C.; et al. Can resistance training impact MRI outcomes in relapsing-remitting multiple sclerosis? Mult. Scler. J. 2018, 24, 1356–1365. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.W.; Mowry, E.M.; Ehde, D.M.; LaRocca, N.G.; Smith, K.E.; Costello, K.; Shinto, L.; Ng, A.V.; Sullivan, A.B.; Giesser, B.; et al. Wellness and multiple sclerosis: The National MS Society establishes a Wellness Research Working Group and research priorities. Mult. Scler. Houndmills Basingstoke Engl. 2018, 24, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Learmonth, Y.C.; Adamson, B.C.; Balto, J.M.; Chiu, C.-Y.; Molina-Guzman, I.; Finlayson, M.L.; Riskin, B.J.; Motl, R.W. Multiple sclerosis patients need and want information on exercise promotion from healthcare providers: A qualitative study. Health Expect. 2017, 20, 574–583. [Google Scholar] [CrossRef]
- McCabe, M. A Needs Analysis of Australians with MS; Multiple Sclerosis Research Australia: North Sydney, Australia, 2012. [Google Scholar]
- Dunn, M.; Bhargava, P.; Kalb, R. Your patients with multiple sclerosis have set wellness as a high priority-and the National Multiple Sclerosis Society is responding. US Neurol. 2015, 11, 80–86. [Google Scholar] [CrossRef]
- Riemann-Lorenz, K.; Wienert, J.; Streber, R.; Motl, R.W.; Coote, S.; Heesen, C. Long-term physical activity in people with multiple sclerosis: Exploring expert views on facilitators and barriers. Disabil. Rehabil. 2020, 42, 3059–3071. [Google Scholar] [CrossRef]
- Sweet, S.N.; Perrier, M.-J.; Podzyhun, C.; Latimer-Cheung, A.E. Identifying physical activity information needs and preferred methods of delivery of people with multiple sclerosis. Disabil. Rehabil. 2013, 35, 1–8. [Google Scholar] [CrossRef]
- Learmonth, Y.C.; Chan, Z.; Correia, H.; Hathorn, D.; Kermode, A.; Smith, C.; Walker, D. Exercise participation and promotion in the multiple sclerosis community; perspectives across varying socio-ecological levels. Disabil. Rehabil. 2020, 43, 3623–3638. [Google Scholar] [CrossRef]
- Learmonth, Y.C.; Adamson, B.C.; Balto, J.M.; Chiu, C.-Y.; Molina-Guzman, I.; Finlayson, M.; Riskin, B.J.; Wynn, D.R.; Motl, R.W. Investigating the needs of healthcare providers for promoting exercise in persons with multiple sclerosis: A qualitative study. Disabil. Rehabil. 2018, 40, 2172–2180. [Google Scholar] [CrossRef]
- Richardson, E.V.; Barstow, E.; Fifolt, M.; Motl, R.W. Evaluation of a Conceptual Model Regarding Exercise Promotion Through the Patient-Provider Interaction in Multiple Sclerosis: Health Care Provider Perspectives. Qual. Health Res. 2018, 30, 1262–1274. [Google Scholar] [CrossRef]
- Kalb, R.; Brown, T.R.; Coote, S.; Costello, K.; Dalgas, U.; Garmon, E.; Giesser, B.; Halper, J.; Karpatkin, H.; Keller, J.; et al. Exercise and lifestyle physical activity recommendations for people with multiple sclerosis throughout the disease course. Mult. Scler. J. 2020, 26, 1459–1469. [Google Scholar] [CrossRef] [PubMed]
- Marck, C.; Hunter, A.; Heritage, B.; Gibbs, L.; Kermode, A.G.; Learmonth, Y. The effect of the Australian bushfires and the COVID-19 pandemic on health behaviours in people with multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 53, 103042. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.W.; McAuley, E.; Snook, E.M. Physical activity and multiple sclerosis: A meta-analysis. Mult. Scler. 2005, 11, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Murray, T. Multiple Sclerosis: The History of a Disease; Demos Medical Publishing: New York, NY, USA, 2004; ISBN 978-1-934559-27-7. [Google Scholar]
- Abercrombie, J. Pathological and Practical Researches and the Spinal Cord; Carey, Lea & Blanchard: Philadelphia, PA, USA, 1938. [Google Scholar]
- Charcot, J. Lectures on the Diseases of the Nervous System Delivered at La Salpêtrière; New Sydenham Society: London, UK, 1877. [Google Scholar]
- Hammond, W. A treatise on diseases of the nervous system. Ch. VII. In Multiple Cerebrospinal Sclerosis; D. Appleton and Co.: New York, NY, USA, 1871; pp. 637–653. [Google Scholar]
- Pearce, J.M.S. Early Observations on Optic Neuritis and Uhthoff’s Sign. Eur. Neurol. 2010, 63, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Dana, C.; Jelliffe, S.; Riley, H.; Tilney, F.; Timme, W. Multiple Sclerosis (Disseminated Sclerosi) an Investigation by the Association for Research in Nervous and Mental Diseases; Report of the Papers and Discussions at the Meeting of the Association; Paul, B., Ed.; Hoeber: New York, NY, USA, 1921. [Google Scholar]
- McAlpine, D.; Compston, A. Atitudes to the treatment of multiple sclerosis 1809–1983. In McAlpine’s Multiple Sclerosis; Elsevier Health Sciences: Amsterdam, The Netherlands, 2005; pp. 62–68. ISBN 978-0-443-07271-0. [Google Scholar]
- Schapiro, R.T.; Petajan, J.H.; Kosich, D.; Molk, B.; Feeney, J. Role of Cardiovascular Fitness in Multiple Sclerosis: A Pilot Study. J. Neurol. Rehabil. 1998, 2, 43–49. [Google Scholar] [CrossRef]
- Petajan, J.H.; Gappmaier, E.; White, A.T.; Spencer, M.K.; Mino, L.; Hicks, R.W. Impact of aerobic training on fitness and quality of life in multiple sclerosis. Ann. Neurol. 1996, 39, 432–441. [Google Scholar] [CrossRef]
- Lai, B.; Young, H.-J.; Bickel, C.S.; Motl, R.W.; Rimmer, J.H. Current Trends in Exercise Intervention Research, Technology, and Behavioral Change Strategies for People with Disabilities: A Scoping Review. Am. J. Phys. Med. Rehabil. 2017, 96, 748–761. [Google Scholar] [CrossRef]
- Edwards, T.; Pilutti, L.A. The effect of exercise training in adults with multiple sclerosis with severe mobility disability: A systematic review and future research directions. Mult. Scler. Relat. Disord. 2017, 16, 31–39. [Google Scholar] [CrossRef]
- Langeskov-Christensen, M.; Heine, M.; Kwakkel, G.; Dalgas, U. Aerobic capacity in persons with multiple sclerosis: A systematic review and meta-analysis. Sports Med. Auckl. NZ 2015, 45, 905–923. [Google Scholar] [CrossRef]
- Platta, M.E.; Ensari, I.; Motl, R.W.; Pilutti, L.A. Effect of Exercise Training on Fitness in Multiple Sclerosis: A Meta-Analysis. Arch. Phys. Med. Rehabil. 2016, 97, 1564–1572. [Google Scholar] [CrossRef]
- Andreu-Caravaca, L.; Ramos-Campo, D.J.; Chung, L.H.; Rubio-Arias, J.Á. Dosage and Effectiveness of Aerobic Training on Cardiorespiratory Fitness, Functional Capacity, Balance, and Fatigue in People With Multiple Sclerosis: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2021, 102, 1826–1839. [Google Scholar] [CrossRef] [PubMed]
- Pearson, M.; Dieberg, G.; Smart, N. Exercise as a therapy for improvement of walking ability in adults with multiple sclerosis: A meta-analysis. Arch. Phys. Med. Rehabil. 2015, 96, 1339–1348. [Google Scholar] [CrossRef] [PubMed]
- Learmonth, Y.C.; Ensari, I.; Motl, R.W. Physiotherapy and walking outcomes in adults with multiple sclerosis: Systematic review and meta-analysis. Phys. Ther. Rev. 2016, 21, 160–172. [Google Scholar] [CrossRef]
- Mañago, M.M.; Glick, S.; Hebert, J.R.; Coote, S.; Schenkman, M. Strength Training to Improve Gait in People with Multiple Sclerosis: A Critical Review of Exercise Parameters and Intervention Approaches. Int. J. MS Care 2019, 21, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Cruickshank, T.M.; Reyes, A.R.; Ziman, M.R. A systematic review and meta-analysis of strength training in individuals with multiple sclerosis or Parkinson disease. Medicine 2015, 94, e411. [Google Scholar] [CrossRef] [PubMed]
- Paltamaa, J.; Sjögren, T.; Peurala, S.H.; Heinonen, A. Effects of physiotherapy interventions on balance in multiple sclerosis: A systematic review and meta-analysis of randomized controlled trials. J. Rehabil. Med. Off. J. UEMS Eur. Board Phys. Rehabil. Med. 2012, 44, 811–823. [Google Scholar] [CrossRef] [Green Version]
- Martino Cinnera, A.; Bisirri, A.; Leone, E.; Morone, G.; Gaeta, A. Effect of dual-task training on balance in patients with multiple sclerosis: A systematic review and meta-analysis. Clin. Rehabil. 2021, 35, 1399–1412. [Google Scholar] [CrossRef]
- Sandroff, B.M.; Motl, R.W.; Scudder, M.R.; DeLuca, J. Systematic, Evidence-Based Review of Exercise, Physical Activity, and Physical Fitness Effects on Cognition in Persons with Multiple Sclerosis. Neuropsychol. Rev. 2016, 26, 271–294. [Google Scholar] [CrossRef]
- Harrison, A.M.; Safari, R.; Mercer, T.; Picariello, F.; van der Linden, M.L.; White, C.; Moss-Morris, R.; Norton, S. Which exercise and behavioural interventions show most promise for treating fatigue in multiple sclerosis? A network meta-analysis. Mult. Scler. J. 2021, 27, 1657–1678. [Google Scholar] [CrossRef]
- Taul-Madsen, L.; Connolly, L.; Dennett, R.; Freeman, J.; Dalgas, U.; Hvid, L.G. Is Aerobic or Resistance Training the Most Effective Exercise Modality for Improving Lower Extremity Physical Function and Perceived Fatigue in People With Multiple Sclerosis? A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2021, 102, 2032–2048. [Google Scholar] [CrossRef]
- Moss-Morris, R.; Harrison, A.M.; Safari, R.; Norton, S.; van der Linden, M.L.; Picariello, F.; Thomas, S.; White, C.; Mercer, T. Which behavioural and exercise interventions targeting fatigue show the most promise in multiple sclerosis? A systematic review with narrative synthesis and meta-analysis. Behav. Res. Ther. 2021, 137, 103464. [Google Scholar] [CrossRef]
- Torres-Costoso, A.; Martínez-Vizcaíno, V.; Reina-Gutiérrez, S.; Álvarez-Bueno, C.; Guzmán-Pavón, M.J.; Pozuelo-Carrascosa, D.P.; Fernández-Rodríguez, R.; Sanchez-López, M.; Cavero-Redondo, I. Effect of Exercise on Fatigue in Multiple Sclerosis: A Network Meta-analysis Comparing Different Types of Exercise. Arch. Phys. Med. Rehabil. 2021. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, S.; Shen, J.; Yang, H.; Xu, W.; Shao, M.; Pan, F. Effect of Exercise on Fatigue in Multiple Sclerosis Patients: A Network Meta-analysis. Int. J. Sports Med. 2021. [Google Scholar] [CrossRef]
- Razazian, N.; Kazeminia, M.; Moayedi, H.; Daneshkhah, A.; Shohaimi, S.; Mohammadi, M.; Jalali, R.; Salari, N. The impact of physical exercise on the fatigue symptoms in patients with multiple sclerosis: A systematic review and meta-analysis. BMC Neurol. 2020, 20, 93. [Google Scholar] [CrossRef]
- Dalgas, U.; Stenager, E.; Sloth, M.; Stenager, E. The effect of exercise on depressive symptoms in multiple sclerosis based on a meta-analysis and critical review of the literature. Eur. J. Neurol. Off. J. Eur. Fed. Neurol. Soc. 2015, 22, 443-e34. [Google Scholar] [CrossRef] [PubMed]
- Ensari, I.; Motl, R.W.; Pilutti, L.A. Exercise training improves depressive symptoms in people with multiple sclerosis: Results of a meta-analysis. J. Psychosom. Res. 2014, 76, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Adamson, B.C.; Ensari, I.; Motl, R.W. The effect of exercise on depressive symptoms in adults with neurological disorders: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2015, 96, 1329. [Google Scholar] [CrossRef]
- Latimer-Cheung, A.E.; Pilutti, L.A.; Hicks, A.L.; Martin Ginis, K.A.; Fenuta, A.; Mackibbon, K.A.; Motl, R.W. The effects of exercise training on fitness, mobility, fatigue, and health related quality of life among adults with multiple sclerosis: A systematic review to inform guideline development. Arch. Phys. Med. Rehabil. 2013, 94, 1800–1828. [Google Scholar] [CrossRef]
- Alphonsus, K.B.; Su, Y.; D’Arcy, C. The effect of exercise, yoga and physiotherapy on the quality of life of people with multiple sclerosis: Systematic review and meta-analysis. Complement. Ther. Med. 2019, 43, 188–195. [Google Scholar] [CrossRef]
- Leavitt, V.M.; Cirnigliaro, C.; Cohen, A.; Farag, A.; Brooks, M.; Wecht, J.M.; Wylie, G.R.; Chiaravalloti, N.D.; DeLuca, J.; Sumowski, J.F. Aerobic exercise increases hippocampal volume and improves memory in multiple sclerosis: Preliminary findings. Neurocase 2014, 20, 695–697. [Google Scholar] [CrossRef] [PubMed]
- Sandroff, B.M.; Johnson, C.L.; Motl, R.W. Exercise training effects on memory and hippocampal viscoelasticity in multiple sclerosis: A novel application of magnetic resonance elastography. Neuroradiology 2017, 59, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Pilutti, L.A.; Dlugonski, D.; Sandroff, B.M.; Klaren, R.; Motl, R.W. Randomized controlled trial of a behavioral intervention targeting symptoms and physical activity in multiple sclerosis. Mult. Scler. Houndmills Basingstoke Engl. 2014, 20, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi Bahmani, D.; Kesselring, J.; Papadimitriou, M.; Bansi, J.; Pühse, U.; Gerber, M.; Shaygannejad, V.; Holsboer-Trachsler, E.; Brand, S. In Patients With Multiple Sclerosis, Both Objective and Subjective Sleep, Depression, Fatigue, and Paresthesia Improved After 3 Weeks of Regular Exercise. Front. Psychiatry 2019, 3, 265. [Google Scholar] [CrossRef] [Green Version]
- Ranadive, S.M.; Yan, H.; Weikert, M.; Lane, A.D.; Linden, M.A.; Baynard, T.; Motl, R.W.; Fernhall, B. Vascular dysfunction and physical activity in multiple sclerosis. Med. Sci. Sports Exerc. 2012, 44, 238–243. [Google Scholar] [CrossRef]
- Wens, I.; Eijnde, B.; Hansen, D. Muscular, cardiac, ventilatory and metabolic dysfunction in patients with multiple sclerosis: Implications for screening, clinical care and endurance and resistance exercise therapy, a scoping review. J. Neurol. Sci. 2016, 367, 107–121. [Google Scholar] [CrossRef]
- Ewanchuk, B.W.; Gharagozloo, M.; Peelen, E.; Pilutti, L.A. Exploring the role of physical activity and exercise for managing vascular comorbidities in people with multiple sclerosis: A scoping review. Mult. Scler. Relat. Disord. 2018, 26, 19–32. [Google Scholar] [CrossRef]
- Pilutti, L.A.; Platta, M.E.; Motl, R.W.; Latimer-Cheung, A.E. The safety of exercise training in multiple sclerosis: A systematic review. J. Neurol. Sci. 2014, 343, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Tallner, A.; Waschbisch, A.; Wenny, I.; Schwab, S.; Hentschke, C.; Pfeifer, K.; Mäurer, M. Multiple sclerosis relapses are not associated with exercise. Mult. Scler. Houndmills Basingstoke Engl. 2012, 18, 232–235. [Google Scholar] [CrossRef] [Green Version]
- Motl, R.W.; Dlugonski, D.; Pilutti, L.; Sandroff, B.; McAuley, E. Premorbid physical activity predicts disability progression in relapsing-remitting multiple sclerosis. J. Neurol. Sci. 2012, 323, 123–127. [Google Scholar] [CrossRef]
- Motl, R.W.; Pilutti, L.A. The benefits of exercise training in multiple sclerosis. Nat. Rev. Neurol. 2012, 8, 487–497. [Google Scholar] [CrossRef]
- Motl, R.W.; Sandroff, B.M.; Kwakkel, G.; Dalgas, U.; Feinstein, A.; Heesen, C.; Feys, P.; Thompson, A.J. Exercise in patients with multiple sclerosis. Lancet Neurol. 2017, 16, 848–856. [Google Scholar] [CrossRef]
- Learmonth, Y.C.; Pilutti, L.A.; Herring, M.P.; Motl, R.W.; Chan, B.; Metse, A.P. Safety of exercise training in multiple sclerosis: A protocol for an updated systematic review and meta-analysis. Syst. Rev. 2021, 10, 208. [Google Scholar] [CrossRef] [PubMed]
- Latimer-Cheung, A.E.; Martin Ginis, K.A.; Hicks, A.L.; Motl, R.; Pilutti, L.; Duggan, M.; Wheeler, G.; Persad, R.; Smith, K. Development of evidence-informed physical activity guidelines for adults with Multiple Sclerosis. Arch. Phys. Med. Rehabil. 2013, 94, 1829–1836. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lai, B.; Mehta, T.; Thirumalai, M.; Padalabalanarayanan, S.; Rimmer, J.H.; Motl, R.W. Exercise Training Guidelines for Multiple Sclerosis, Stroke, and Parkinson Disease: Rapid Review and Synthesis. Am. J. Phys. Med. Rehabil. 2019, 98, 613. [Google Scholar] [CrossRef]
- Smith, C.M.; Hale, L.A.; Olson, K.; Baxter, G.D.; Schneiders, A.G. Healthcare provider beliefs about exercise and fatigue in people with multiple sclerosis. J. Rehabil. Res. Dev. 2013, 50, 733. [Google Scholar] [CrossRef] [Green Version]
- World Confederation for Physical Therapy Policy Statement: Description of Physical Therapy|World Confederation for Physical Therapy. Available online: https://world.physio/policy/ps-descriptionPT (accessed on 2 September 2019).
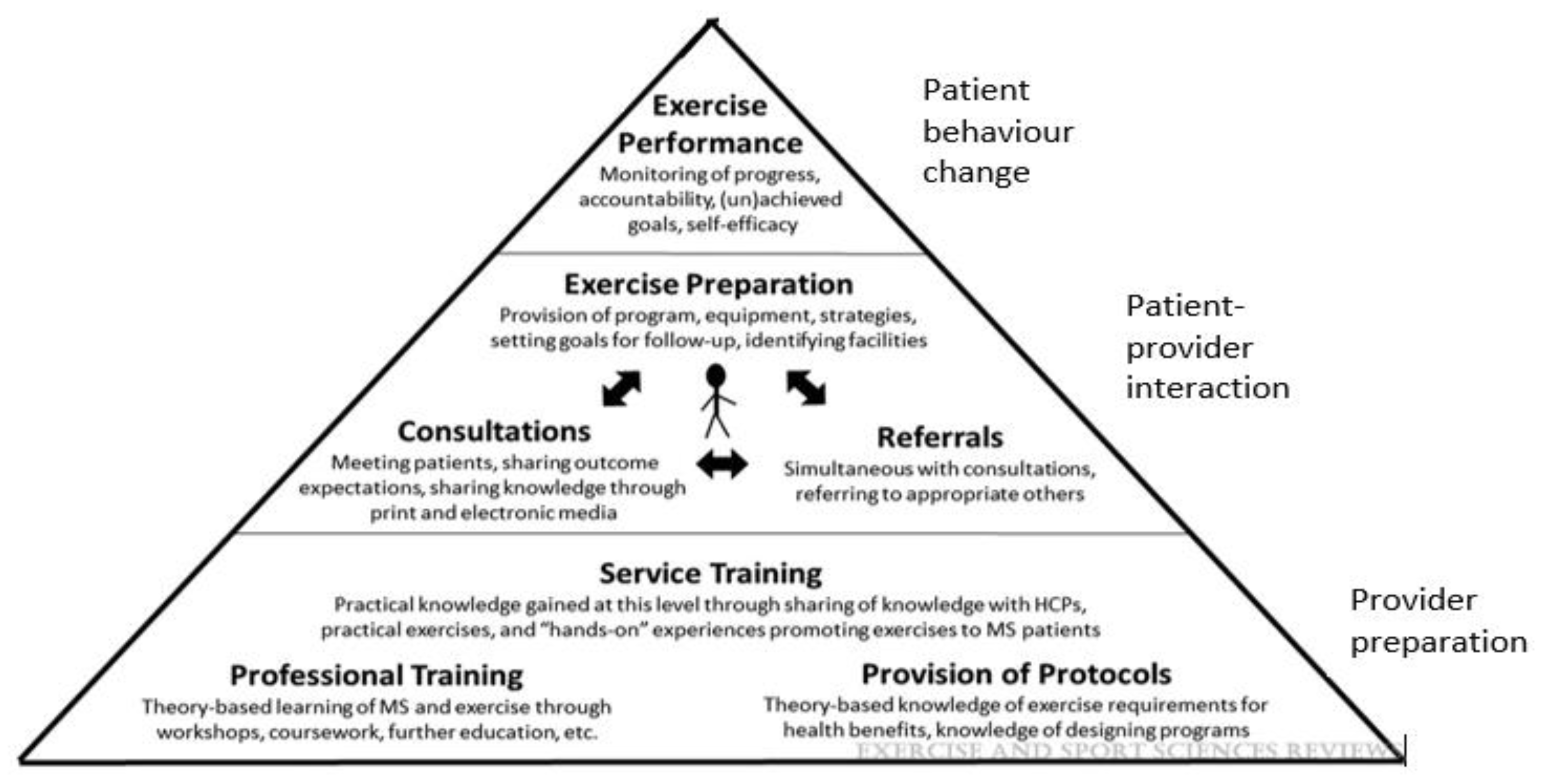
- Motl, R.W.; Barstow, E.A.; Blaylock, S.; Richardson, E.; Learmonth, Y.C.; Fifolt, M. Promotion of exercise in multiple sclerosis through health care providers. Exerc. Sport Sci. Rev. 2018, 46, 105–111. [Google Scholar] [CrossRef]
- Sangelaji, B.; Smith, C.M.; Paul, L.; Sampath, K.K.; Treharne, G.J.; Hale, L.A. The effectiveness of behaviour change interventions to increase physical activity participation in people with multiple sclerosis: A systematic review and meta-analysis. Clin. Rehabil. 2016, 30, 559–576. [Google Scholar] [CrossRef] [PubMed]
- Coulter, E.H.; Bond, S.; Dalgas, U.; Paul, L. The effectiveness of interventions targeting physical activity and/or sedentary behaviour in people with Multiple Sclerosis: A systematic review. Disabil. Rehabil. 2020, 42, 594–612. [Google Scholar] [CrossRef]
- Riemenschneider, M.; Hvid, L.G.; Stenager, E.; Dalgas, U. Is there an overlooked “window of opportunity” in MS exercise therapy? Perspectives for early MS rehabilitation. Mult. Scler. J. 2018, 24, 886–894. [Google Scholar] [CrossRef]
- Huynh, T.L.T.; Silveira, S.L.; Motl, R.W. Systematic review of participant characteristics in theory-based bahavior change interventions for physical activity in multiple sclerosis: Are we missing those with the greatest potential for lifelong benefits? Disabil. Rehabil. 2021, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Ploughman, M. Breaking down the barriers to physical activity among people with multiple sclerosis—A narrative review. Phys. Ther. Rev. 2017, 22, 124–132. [Google Scholar] [CrossRef]
- Learmonth, Y.C.; Motl, R.W. Physical activity and exercise training in multiple sclerosis: A review and content analysis of qualitative research identifying perceived determinants and consequences. Disabil. Rehabil. 2016, 38, 1227–1242. [Google Scholar] [CrossRef] [PubMed]
| General Aerobic Activity | Advanced Aerobic Activity * | Strength Training | |
|---|---|---|---|
| How often? | 2/3 times per week | 5 times per week | 2/3 times per week |
| How much? | Gradually increase your activity towards being able to complete 30 min of aerobic activity during each workout session | Increase your activity towards being able to complete 40 min of aerobic activity during each workout session | Repetitions are the number of times you lift and lower a weight Try to do 10–15 repetitions of each exercise. This counts as 1 set Gradually work up to doing 2 sets of 10–15 repetitions of each exercise |
| How hard? | The activities should be performed at a moderate intensity. Moderate intensity physical activity is usually between 11 and 13 on the 20-point RPE scale, and it causes your heart rate to go up. Another rule of thumb, if you are doing moderate-intensity activity you can talk, but not sing a song, during the activity An alternative way of measuring moderate intensity of exercise is 40–60% VO2peak or HRpeak | The activities should be performed at a moderate to vigorous intensity. Intensity of exercise can approach 15 on the 20-point RPE scale. Another rule of thumb, if you are doing vigorous-intensity activity you can only say a few words while doing your activity. An alternative way of measuring moderate intensity of exercise is 70–80% VO2peak or HRpeak | Choose a resistance (using free weights, cable pulleys, bands etc) heavy enough that you can barely, but safely, finish 10–15 repetitions of each exercise You should rest for 1–2 min between each set and exercise, or alternate with a different resistance exercise (e.g., upper body then lower body) |
| How to? | Options should be feasible and sustainable, and might include | ||
Some options for general aerobic activities include
| Some options for advanced aerobic activities include
| Strength training activities
| |
Other types of exercise that may bring benefits
| |||
| Special considerations |
| ||
| Actions and Resource Development | Target Audience |
|---|---|
| Service Training (i.e., sharing of knowledge between exercise- specialist healthcare providers with non-exercise specialist healthcare providers or behaviour change specialist healthcare providers with non-behaviour change specialist providers) to deliver evidenced guideline-based exercise promotion to patients/clients, ideally for use at initial consultations and review consultations thereafter | Neurologists and the multidisciplinary healthcare team, and healthcare team systems |
| Professional Training (i.e., theory based education) to deliver evidenced guideline-based exercise promotion to patients/clients, ideally undertaken at graduate level and post-graduate continual education | Neurologists and the multidisciplinary healthcare team, educational establishments and national MS advocacy organisations |
| Evidenced guideline-based resources or protocols to apply exercise health benefits and knowledge to design, or refer for design (by appropriate exercise specialist healthcare provider), patient/client specific programmes | Neurologists and the multidisciplinary healthcare team |
| Initial and ongoing consultations where exercise outcome expectations and goal discussion are salient and where knowledge can be shared in client-accessible print and electronic materials (with consideration of health-literacy and language capacity) | Neurologists and the multidisciplinary healthcare team, persons with MS, carers. |
| Cross-referral pathways between exercise-specialist healthcare providers/behaviour change specialist healthcare providers with non-exercise/non-behaviour change specialist healthcare providers should be developed to ensure appropriate and comprehensive content and acknowledgement ofMS symptoms (e.g., fatigue, mobility-disability, depression and cognitive impairment), personal circumstances and community circumstances which may prevent engagement in exercise. | MS healthcare providers Neurologists and the multidisciplinary healthcare team systems and national MS advocacy organisations |
| Exercise and behaviour change preparation through appropriate provision of exercise programme explanations, equipment and faciliries, and use of evidenced behavioral strategies, goal discussion, sequestering of barriers and mastery of life-long exercise behaviours | MS Exercise specialist providers and MS Behavioural specialist providers |
| Monitoring of exercise behaviour performance ideally at initial consultation and review consultations thereafter. Inclusive of monitoring functional progress, client accountability toward exercise behaviour, exercise behavioural (un) achievement and goal discussion updates. | Neurologists and the multidisciplinary healthcare team |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Learmonth, Y.C.; Motl, R.W. Exercise Training for Multiple Sclerosis: A Narrative Review of History, Benefits, Safety, Guidelines, and Promotion. Int. J. Environ. Res. Public Health 2021, 18, 13245. https://doi.org/10.3390/ijerph182413245
Learmonth YC, Motl RW. Exercise Training for Multiple Sclerosis: A Narrative Review of History, Benefits, Safety, Guidelines, and Promotion. International Journal of Environmental Research and Public Health. 2021; 18(24):13245. https://doi.org/10.3390/ijerph182413245
Chicago/Turabian StyleLearmonth, Yvonne Charlotte, and Robert Wayne Motl. 2021. "Exercise Training for Multiple Sclerosis: A Narrative Review of History, Benefits, Safety, Guidelines, and Promotion" International Journal of Environmental Research and Public Health 18, no. 24: 13245. https://doi.org/10.3390/ijerph182413245
APA StyleLearmonth, Y. C., & Motl, R. W. (2021). Exercise Training for Multiple Sclerosis: A Narrative Review of History, Benefits, Safety, Guidelines, and Promotion. International Journal of Environmental Research and Public Health, 18(24), 13245. https://doi.org/10.3390/ijerph182413245






