Sleep Disorders in Cancer—A Systematic Review
Abstract
:1. Introduction
2. State-of-the-Art
2.1. Sleep Disturbances in the Case of Cancer-Related Fatigue (CrF)
2.2. Insomnia in Cancer
2.3. Sleep-Related Breathing Disorder (SRBD)/Obstructive Sleep Apnea Syndrome (OSAS) in Cancer
2.4. Narcolepsy in Cancer
2.5. Restless Legs Syndrome (RLS) in Cancer
2.6. REM Sleep Behavior Disorder in Cancer
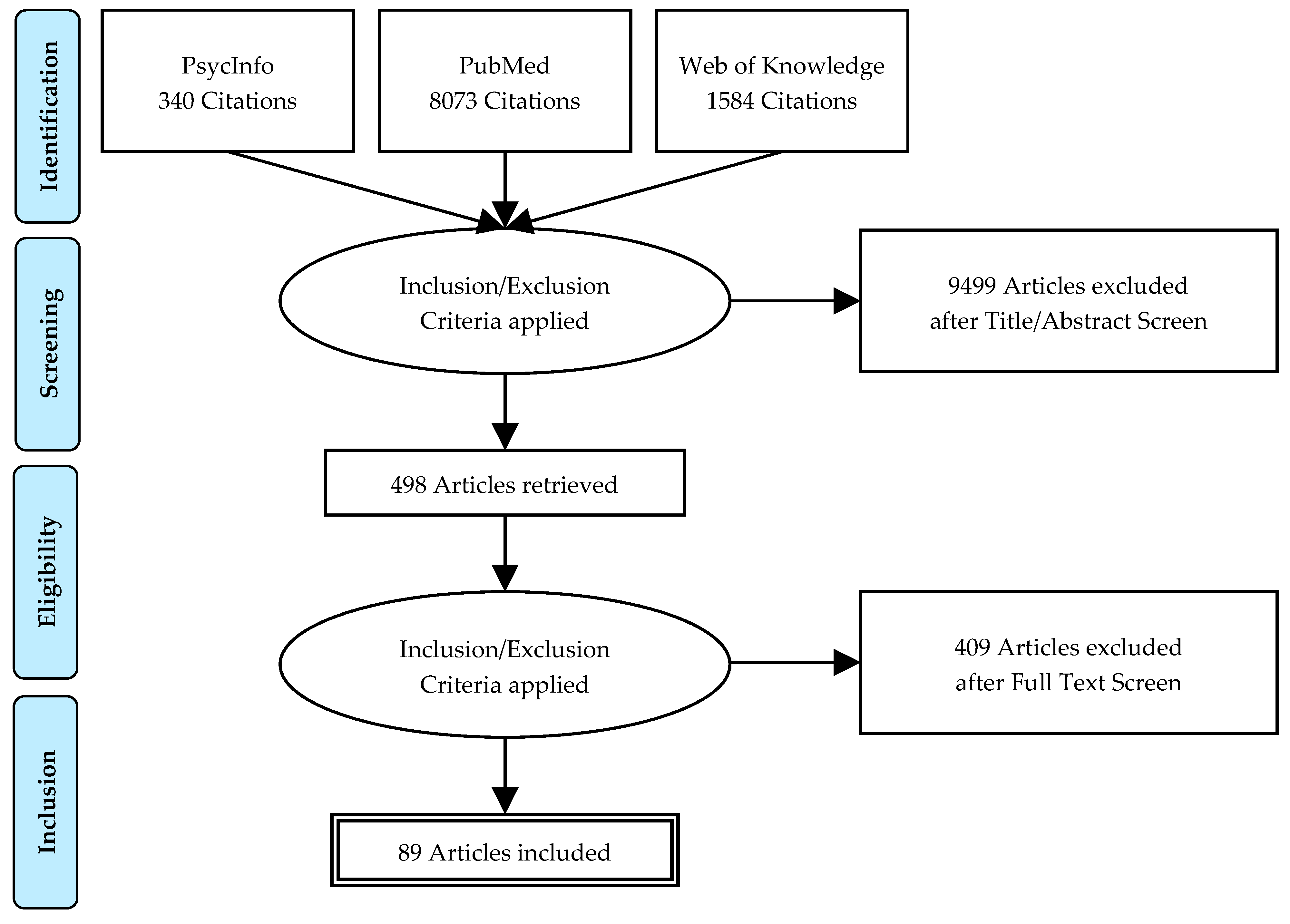
3. Method
3.1. Data Sources
3.2. Types of Studies
3.3. Types of Participants
3.4. Types of Intervention
3.5. Types of Outcomes
3.5.1. Primary Outcomes
- 1.
- The prevalence and/or the incidence of sleep disturbences and/or sleep disorders in cancer were evaluated firstly by objective measurements—polysomnography (PSG)/gold standard and polygraphy (PG) for OSAS or actigraphy. The important sleep parameters included total sleep time (TST), time in bed (TIB), sleep efficiency (SE), sleep quality (SQ), sleep onset latency (SOL), wake after sleep onset or total waking time (WASO).
- 2.
- The prevalence and/or the incidence of sleep disturbences and/or sleep disorders in cancer are measured secondly by subjective measurements—by scales or indices for the sleep quality (e.g., the Pittsburgh Sleep Quality Index (PSQI)) or special sleep disorders: insomnia (e.g., Insomnia Severity Index (ISI), Athens Insomnia Scale (ASI)), OSAS (e.g., Berlin questionnaire), Narcolepsy (e.g., Narcolepsy Symptom Questionnaire (NSQ)) or RLS (International Restless Legs Syndrome Study Group rating scale (IRLS)).
3.5.2. Secondary Outcomes
3.6. Selection of Studies and Data Extraction
4. Results
5. Discussion
5.1. Expert Recommendations
5.2. References Classification
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Disorders | |
| CA | Carcinoma |
| CrF | Cancer-related Fatigue |
| CRFS | Cancer-related Fatigue Syndrome |
| CRSD | Cancer-Related Sleep Disorders |
| OSA(S) | Obstructive Sleep Apnea (Syndrome) |
| REM-SBD | REM-Sleep Behavior Disorder |
| RLS | Restless Legs Syndrome |
| SRBD | Sleep-Related Breathing Disorder |
| Measurements | |
| MESAM | Madaus Electronic Sleep Apnea Monitor |
| MRI | Magnetic Resonance Imaging |
| OSP | Objective Sleep Parameters |
| PG | Polygraphy |
| PSG | Polysomnography |
| SSP | Subjective Sleep Parameters |
| Anthropomeric and Clinical Data | |
| CRP | C-Reactive Protein |
| IFN-γ | Interferon gamma |
| IL-6/-1β | Interleukin-6/Interleukin-1-beta |
| IL-1RA | Interleukin-1 Receptor Antagonist |
| QoL | Quality of Life |
| TNF | Tumor Necrosis Factor |
| Therapies | |
| AeT | Aerobic Treatment |
| AT | Autogenic Training |
| BT | Behavioral Therapy |
| CBT | Cognitive Behavior Therapy |
| CPPT | Cool Pad Pillow Topper |
| CPAP | Continuous Positive Airway Pressure |
| CT | Combined Multimodal-Aerobic Treatment |
| EA | Electro-Acupuncture |
| ISPP | Individualized Sleep Promotion Plan |
| MBSR | Mindfulness-Based Stress Reduction |
| MT | Multimodal Treatment |
| PMR | Progressive Muscle Relaxation |
| PCBT | Professionally administered CBT |
| SHUTi | Sleep Healthy Using the Internet |
| SC | Standard Care |
| TCC | Tai Chi Chi |
| VCBT | Video-based CBT |
| Sleep Parameters | |
| TST | Total Sleep Time |
| TIB | Time in Bed |
| SE | Sleep Efficiency |
| SQ | Sleep Quality |
| SOL | Sleep*Onset*Latency |
| SWS | Slow Wave Sleep |
| WASO | Wake after Sleep*Onset or Total Waking Time |
| Questionnaires | |
| ABS | Adherence to Behavioral Strategies |
| ASI | Athens Insomnia Scale |
| BCPT | Breast Cancer Prevention Trial |
| BDI | Becks Depression Inventory |
| BDSS | Blood Deficiency Scoring System |
| BFI | Brief Fatigue Inventory |
| CES-D | Center for Epidemiologic Studies—Depression Scale |
| CFS-D | Cancer Fatigue Scale |
| C-LSEQ | Chonnam National University Hospital—Leeds Sleep Evaluation Questionnaire |
| CrQoL | Cancer-Related Quality of Life |
| CTCAE | Common Terminology Criteria for Adverse Events |
| DBAS | Dysfunctional Beliefs and Attitudes about Sleep Scale |
| ESS | Epworth Sleepiness Scale |
| EQ-5D | Euro QoL |
| FACT | Functional Assessment Cancer Therapy |
| FOSQ | Functional Outcomes of Sleep Questionnaire |
| FSI | Fatigue Symptom Inventory |
| GSDS | General Sleep Disturbance Scale |
| HADS | Hospital Anxiety and Depression Scale |
| HDI | Hamilton Depression Inventory |
| NCCTG | North Central Cancer Treatment Group |
| PSQI | Pittsburgh Sleep Quality Index |
| IES-R | Revised Impact of Event Scale |
| IIS | Insomnia Interview Schedule |
| ISI | Insomnia Severity Index |
| IRLS | International Restless Legs Syndrome Study Group rating scale |
| MADRS | Montgomery-Asberg Depression Rating Scale |
| MFSI-SF | Multidimensional Fatigue Symptom Inventory |
| MoCA | Montreal Cognitive Assessment |
| MOS | Medical Outcomes Study |
| MOOS | Medical Outcomes Survey Sleep |
| MSAS | Memorial Symptom Assessment Scale |
| NRS | Numerical Rating Scales (Pain intensity) |
| PANAS | Positive and Negative Affect Scale |
| POMS | Profile of Mood States |
| PROMIS | Problem Index Patient-reported Outcomes Measurement Information System |
| PSQ | Physical Symptoms Questionnaire |
| QLQ-C30+ 3 | European Organization for Research and Treatment of Cancer Quality of Life Questionnaire |
| SF-12/-36 | Short Form of Health Survey |
| STAI | State Trait Anxiety Inventory |
| TAPQ | Therapeutic Alliance Perception Questionnaire |
| TEPCQ | Treatment Expectancies and Perceived Credibility Questionnaire |
| TNAS | Toxicity Numeric Analogue Scale |
| UQ | Internet Intervention Utility Questionnaire |
References
- Ancoli-Israel, S.; Moore, P.J.; Jones, V. The relationship between fatigue and sleep in cancer patients: A review. Eur. J. Cancer Care 2001, 10, 245–255. [Google Scholar] [CrossRef] [Green Version]
- Ancoli-Israel, S.; Liu, L.; Marler, M.R.; Parker, B.A.; Jones, V.; Sadler, G.R.; Dimsdale, J.; Cohen-Zion, M.; Fiorentino, L. Fatigue, sleep, and circadian rhythms prior to chemotherapy for breast cancer. Support. Care Cancer 2006, 14, 201–209. [Google Scholar] [CrossRef] [Green Version]
- Ancoli-Israel, S.; Liu, L.; Rissling, M.; Natarajan, L.; Neikrug, A.B.; Palmer, B.; Mills, P.J.; Parker, B.A.; Sadler, G.R.; Maglione, J. Sleep, fatigue, depression, and circadian activity rhythms in women with breast cancer before and after treatment: A 1-year longitudinal study. Support. Care Cancer 2014, 22, 2535–2545. [Google Scholar] [CrossRef]
- Banthia, R.; Malcarne, V.L.; Ko, C.M.; Varni, J.W.; Sadler, G.R. Fatigued breast cancer survivors: The role of sleep quality, depressed mood, stage and age. Psychol. Heal. 2009, 24, 965–980. [Google Scholar] [CrossRef] [Green Version]
- Berger, A.M.; Farr, L. The influence of daytime inactivity and nighttime restlessness on cancer-related fatigue. Oncol. Nurs. Forum 1999, 26, 1663–1671. [Google Scholar] [PubMed]
- Chang, V.T.; Hwang, S.S.; Feuerman, M.; Kasimis, B.S. Symptom and quality of life survey of medical oncology patients at a Veterans Affairs medical center. Cancer 2000, 88, 1175–1183. [Google Scholar] [CrossRef]
- Cimprich, B. Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nurs. 1999, 22, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Clevenger, L.; Schrepf, A.; Christensen, D.; DeGeest, K.; Bender, D.; Ahmed, A.; Goodheart, M.J.; Penedo, F.; Lubaroff, D.M.; Sood, A.K.; et al. Sleep disturbance, cytokines, and fatigue in women with ovarian cancer. Brain Behav. Immun. 2012, 26, 1037–1044. [Google Scholar] [CrossRef] [Green Version]
- Engstrom, C.A.; Strohl, R.A.; Rose, L.; Lewandowski, L.; Stefanek, M.E. Sleep alterations in cancer patients. Cancer Nurs. 1999, 22, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Fiorentino, L.; Rissling, M.; Liu, L.; Ancoli-Israel, S. The symptom cluster of sleep, fatigue and depressive symptoms in breast cancer patients: Severity of the problem and treatment options. Drug Discov. Today Dis. Model. 2011, 8, 167–173. [Google Scholar] [CrossRef] [Green Version]
- Gotts, Z.M.; Deary, V.; Newton, J.; Van der Dussen, D.; De Roy, P.; Ellis, J.G. Are there sleep-specific phenotypes in patients with chronic fatigue syndrome? A cross-sectional poly-somnography analysis. BMJ Open 2013, 3, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Illi, J.; Miaskowski, C.; Cooper, B.; Levine, J.D.; Dunn, L.; West, C.; Dodd, M.; Dhruva, A.; Paul, S.M.; Baggott, C.; et al. Association between pro- and anti-inflammatory cytokine genes and a symptom cluster of pain, fatigue, sleep disturbance, and depression. Cytokine 2012, 58, 437–447. [Google Scholar] [CrossRef] [Green Version]
- Kaye, J.; Kaye, K.; Madow, L. Sleep pattern in patients with cancer and cardiac disease. J. Psychol. 1983, 114, 107–113. [Google Scholar] [CrossRef]
- Liu, L.; Fiorentino, L.; Natarajan, L.; Parker, B.A.; Mills, P.J.; Sadler, G.R.; Dimsdale, J.E.; Rissling, M.; He, F.; Ancoli-Israel, S. Pre-treatment symptom cluster in breast cancer patients is associated with worse sleep, fatigue and depression during chemotherapy. Psycho Oncol. 2009, 18, 187–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L.; Rissling, M.; Natarajan, L.; Fiorentino, L.; Mills, P.J.; Dimsdale, J.E.; Sadler, G.R.; Parker, B.A.; Ancoli-Israel, S. The Longitudinal Relationship between Fatigue and Sleep in Breast Cancer Patients Undergoing Chemothera-py. Sleep 2012, 35, 237–245. [Google Scholar] [CrossRef]
- Liu, L.; Mills, P.J.; Rissling, M.; Fiorentino, L.; Natarajan, L.; Dimsdale, J.E.; Sadler, G.R.; Parker, B.A.; Ancoli-Israel, S. Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav. Immun. 2012, 26, 706–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miaskowski, C.h.; Lee, K.A. Pain, Fatigue, and Sleep Disturbances in Oncology Outpatients Receiving Radiation Therapy for Bone Metastasis: A Pilot Study. J. Pain Symptom Manag. 1999, 17, 320–332. [Google Scholar] [CrossRef]
- Mormont, M.C.; De Prins, J.; Levi, F. Study of circadian rhythms of activity by actometry: Preliminary results in 30 patients with metastat-ic colorectal cancer. Pathol. Biol. (Paris) 1996, 44, 165–171. [Google Scholar]
- Mormont, M.C.; Waterhouse, J.; Bleuzen, P.; Giacchetti, S.; Jami, A.; Bogdan, A.; Lellouch, J.; Misset, J.L.; Touitou, Y.; Lévi, F. Marked 24-h rest/activity rhythms are associated with better quality of life, better response, and longer survival in patients with metastatic colorectal cancer and good performance status. Clin. Cancer Res. 2000, 6, 3038–3045. [Google Scholar] [PubMed]
- Roscoe, J.A.; Morrow, G.R.; Hickok, J.T.; Bushunow, P.; Matteson, S.; Rakita, D.; Andrews, P.L. Temporal interrelationships among fatigue, circadian rhythm and de-pression in breast cancer patients undergoing chemotherapy treatment. Support Care Cancer 2002, 10, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Mustian, K.M.; Sprod, L.K.; Janelsins, M.; Peppone, L.J.; Mohile, S. Exercise Recommendations for Cancer-Related Fatigue, Cognitive Impairment, Sleep problems, Depression, Pain, Anxiety, and Physical Dysfunction: A Review. Oncol. Hematol. Rev. (US) 2012, 8, 81–88. [Google Scholar] [CrossRef] [Green Version]
- Owen, D.C.; Parker, K.P.; McGuire, D.B. Comparison of subjective sleep quality in patients with cancer and healthy subjects. Oncol. Nurs. Forum 1999, 26, 1649–1651. [Google Scholar]
- Palesh, O.G.; Roscoe, J.A.; Mustian, K.M.; Roth, T.; Savard, J.; Ancoli-Israel, S.; Heckler, C.; Purnell, J.; Janelsins, M.C.; Morrow, G.R. Prevalence, Demographics, and Psychological Associations of Sleep Disruption in Patients with Cancer: University of Rochester Cancer Center–Community Clinical Oncology Program. J. Clin. Oncol. 2010, 28, 292–298. [Google Scholar] [CrossRef]
- Reyes-Gibby, C.C.; Wu, X.; Spitz, M.; Kurzrock, R.; Fisch, M.; Bruera, E.; Shete, S. Molecular epidemiology, cancer-related symptoms, and cytokines pathway. Lancet Oncol. 2008, 9, 777–785. [Google Scholar] [CrossRef] [Green Version]
- Roscoe, J.A.; Kaufman, M.E.; Matteson-Rusby, S.E.; Palesh, O.G.; Ryan, J.L.; Kohli, S.; Perlis, M.L.; Morrow, G.R. Cancer-Related Fatigue and Sleep Disorders. Oncol. 2007, 12, 35–42. [Google Scholar] [CrossRef] [Green Version]
- Silberfarb, P.M.; Hauri, P.J.; Oxman, E.T.; Schnurr, P. Assessment of sleep in patients with lung cancer and breast cancer. J. Clin. Oncol. 1993, 11, 997–1004. [Google Scholar] [CrossRef]
- Davidson, J.R.; MacLean, A.W.; Brundage, M.D.; Schulze, K. Sleep disturbance in cancer patients. Soc. Sci. Med. 2002, 54, 1309–1321. [Google Scholar] [CrossRef]
- Barton, D.L.; Atherton, P.J.; Bauer, B.A.; Moore, D.F., Jr.; Mattar, B.I.; LaVasseur, B.I.; Rowland, K.M., Jr.; Zon, R.T.; Lelindqwister, N.A.; Nagargoje, G.G.; et al. The Use of Valeriana Officinalis (Valerian) in Improving Sleep in Patients Who Are Undergoing Treatment for Cancer: A Phase III Randomized, Placebo-Controlled, Double-Blind Study: NCCTG Trial, N01C5. J. Support. Oncol. 2011, 9, 24–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berger, A.M.; Kuhn, B.R.; Farr, L.A.; Lynch, J.C.; Agrawal, S.; Chamberlain, J.; Von Essen, S.G. Behavioral therapy intervention trial to improve sleep quality and cancer-related fatigue. Psycho Oncol. 2008, 18, 634–646. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.Y.; Giobbie-Hurder, A.; Gantman, K.; Savoie, J.; Scheib, R.; Parker, L.M.; Schernhammer, E.S. A randomized, placebo-controlled trial of melatonin on breastcancer survivors: Impact on sleep, mood, and hot flashes. Breast Cancer Res Treat. 2014, 145, 381–388. [Google Scholar] [CrossRef] [Green Version]
- Choi, T.-Y.; Kim, J.I.; Lim, H.-J.; Lee, M.S. Acupuncture for Managing Cancer-Related Insomnia: A Systematic Review of Randomized Clinical Trials. Integr. Cancer Ther. 2017, 16, 135–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dupont, A.; Bower, J.E.; Stanton, A.L.; Ganz, P.A. Cancer-related intrusive thoughts predict behavioral symptoms following breast cancer treatment. Heal. Psychol. 2014, 33, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Epstein, D.R.; Dirksen, S.R. Randomized Trial of a Cognitive-Behavioral Intervention for Insomnia in Breast Cancer Survivors. Oncol. Nurs. Forum 2007, 34, 51–59. [Google Scholar] [CrossRef]
- Espie, C.A.; Fleming, L.; Cassidy, J.; Samuel, L.; Taylor, L.M.; White, C.A.; Douglas, N.J.; Engleman, H.M.; Kelly, H.L.; Paul, J.; et al. Randomized Controlled Clinical Effectiveness Trial of Cognitive Behavior Therapy Compared with Treat-ment As Usual for Persistent Insomnia in Patients with Cancer. J. Clin. Oncol. 2008, 26, 4651–4658. [Google Scholar] [CrossRef]
- Fiorentino, L.; McQuaid, J.R.; Liu, L.; Natarajan, L.; He, F.; Cornejo, M.; Lawton, S.; Parker, B.A.; Sadler, G.R.; Ancoli-Israel, S.; et al. Individual cognitive behavioral therapy for insomnia in breast cancer survivors: A randomized con-trolled crossover pilot study. Nature and Science of Sleep 2010, 2, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Fleming, L.; Randell, K.; Harvey, C.-J.; Espie, C.A. Does cognitive behaviour therapy for insomnia reduce clinical levels of fatigue, anxiety and depression in cancer patients? Psycho Oncol. 2014, 23, 679–684. [Google Scholar] [CrossRef] [Green Version]
- Garland, S.N.; Carlson, L.; Antle, M.C. I-CAN SLEEP: Rationale and design of a non-inferiority RCT of Mindfulness-based Stress Reduction and Cognitive Behavioral Therapy for the treatment of Insomnia in CANcer survivors. Contemp. Clin. Trials 2011, 32, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Garland, S.N.; Carlson, L.E.; Stephens, A.J.; Antle, M.C.; Samuels, C.; Campbell, T.S. Mindfulness-Based Stress Reduction Compared with Cognitive Behavioral Therapy for the Treatment of Insomnia Comorbid with Cancer: A Randomized, Partially Blinded, Noninferiority Trial. J. Clin. Oncol. 2014, 32, 1–9. [Google Scholar] [CrossRef]
- Garland, S.N.; Johnson, J.A.; Savard, J.; Gehrman, P.; Perlis, M.; Carlson, L.; Campbell, T. Sleeping well with cancer: A systematic review of cognitive behavioral therapy for insomnia in cancer patients. Neuropsychiatr. Dis. Treat. 2014, 10, 1113–1124. [Google Scholar] [PubMed] [Green Version]
- Garland, S.N.; Rouleau, C.R.; Campbell, T.; Samuels, C.; Carlson, L.E. The Comparative Impact of Mindfulness-Based Cancer Recovery (MBCR) and Cognitive Behavior Therapy for Insomnia (CBT-I) on Sleep and Mindfulness in Cancer Patients. Explore (N Y) 2015, 11, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Garland, S.N.; Gehrman, P.; Barg, F.K.; Xie, S.X.; Mao, J.J. CHoosing Options for Insomnia in Cancer Effectively (CHOICE): Design of a patient centered com-parative effectiveness trial of acupuncture and cognitive behavior therapy for insomnia. Contemp. Clin. Trials 2016, 47, 349–355. [Google Scholar] [CrossRef]
- Garland, S.N.; Roscoe, J.A.; Heckler, C.E.; Barilla, H.; Gehrman, P.; Findley, J.C.; Peoples, A.R.; Morrow, G.R.; Kamen, C.; Perlis, M.L.; et al. Effects of armodafinil and cognitive behavior therapy for insomnia on sleep continuity and daytime sleepiness in cancer survivors. Sleep Med. 2016, 20, 18–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graci, G. Pathogenesis and management of cancer-related insomnia. J. Support. Oncol. 2005, 3, 349–359. [Google Scholar] [PubMed]
- Heckler, C.E.; Garland, S.N.; Peoples, A.R.; Perlis, M.L.; Shayne, M.; Morrow, G.R.; Kamen, C.; Hoefler, J.; Roscoe, J.A. Cognitive behavioral therapy for insomnia, but not armodafinil, improves fatigue in cancer survivors with insomnia: A randomized placebo-controlled trial. Supportive Care Cancer 2016, 24, 2059–2066. [Google Scholar] [CrossRef] [PubMed]
- Howell, D.; Oliver, T.K.; Keller-Olaman, S.; Davidson, J.R.; Garland, S.; Samuels, C.; Savard, J.; Harris, C.; Aubin, M.; Olson, K.; et al. Sleep disturbance in adults with cancer: A systematic review of evidence for best practices in assessment and management for clinical practice. Ann. Oncol. 2014, 25, 791–800. [Google Scholar] [CrossRef]
- Irwin, M.R.; Olmstead, R.; Breen, E.C.; Witarama, T.; Carrillo, C.; Sadeghi, N.; Arevalo, J.M.G.; Ma, J.; Nicassio, P.; Ganz, P.A.; et al. Tai Chi, Cellular Inflammation, and Transcriptome Dynamics in Breast Cancer Survivors with Insomnia: A Randomized Controlled Trial. J. Natl. Cancer Inst. Monogr. 2014, 2014, 295–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.; Kim, J.-E.; Lee, H.-Y.; Kim, A.-R.; Park, H.-J.; Kwon, O.-J.; Kim, B.-K.; Cho, J.H.; Kim, J.-H. Electroacupuncture for treating insomnia in patients with cancer: A study protocol for a randomised pilot clinical trial. BMJ Open 2017, 7, e016269. [Google Scholar] [CrossRef]
- Kim, S.-W.; Shin, I.-S.; Kim, J.-M.; Kim, Y.-C.; Kim, K.-S.; Kim, K.-M.; Yang, S.-J.; Yoon, J.-S. Effectiveness of mirtazapine for nausea and insomnia in cancer patients with depression. Psychiatry Clin. Neurosci. 2008, 62, 75–83. [Google Scholar] [CrossRef]
- Kröz, M.; Reif, M.; Glinz, A.; Berger, B.; Nikolaou, A.; Zerm, R.; Brinkhaus, B.; Girke, M.; Büssing, A.; Gutenbrunner, C.; et al. Impact of a combined multimodal-aerobic and multimodal intervention compared to standard aerobic treatment in breast cancer survivors with chronic cancer-related fatigue—Results of a three-armed pragmatic trial in a com-prehensive cohort design. BMC Cancer 2017, 17, 166. [Google Scholar] [CrossRef] [Green Version]
- Lengacher, C.A.; Reich, R.R.; Paterson, C.L.; Jim, H.S.; Ramesar, S.; Alinat, C.B.; Budhrani-Shani, P.; Farias, J.R.; Shelton, M.M.; Moscoso, M.S.; et al. The effects of mindfulness-based stress reduction on objective and subjective sleep parameters in women with breast cancer: A randomized controlled trial. Psycho Oncol. 2014, 24, 424–432. [Google Scholar] [CrossRef] [Green Version]
- Marshall-McKenna, R.; Morrison, A.; Stirling, L.; Hutchison, C.; Rice, A.M.; Hewitt, C.; Paul, J.; Rodger, M.; MacPherson, I.R.; McCartney, E. A randomised trial of the cool pad pillow topper versus standard care for sleep disturbance and hot flushes in women on endocrine therapy for breast cancer. Support. Care Cancer 2015, 24, 1821–1829. [Google Scholar] [CrossRef]
- Mendoza, M.; Capafons, A.; Gralow, J.; Syrjala, K.; Suárez-Rodríguez, J.; Fann, J.; Jensen, M. Randomized controlled trial of the Valencia model of waking hypnosis plus CBT for pain, fatigue, and sleep management in patients with cancer and cancer survivors. Psycho-Oncology 2016, 26, 1832–1838. [Google Scholar] [CrossRef]
- Minton, O.; Stone, P. A comparison of cognitive function, sleep and activity levels in disease-free breast cancer patients with or without cancer-related fatigue syndrome. BMJ Support. Palliat. Care 2012, 2, 231–238. [Google Scholar] [CrossRef] [Green Version]
- Park, B.; Youn, S.; Hann, C.W.C.; Yi, K.; Lee, S.; Lee, J.S.; Chung, S. Prevalence of Insomnia among Patients with the Ten Most Common Cancers in South Korea: Health Insur-ance Review and Assessment Service-National Patient Sample. Sleep Med. Res. 2016, 7, 48–54. [Google Scholar] [CrossRef]
- Peoples, A.R.; Garland, S.; Perlis, M.L.; Savard, J.; Heckler, C.E.; Kamen, C.S.; Ryan, J.L.; Mustian, K.M.; Janelsins, M.C.; Peppone, L.J.; et al. Effects of cognitive behavioral therapy for insomnia and armodafinil on quality of life in cancer survivors: A randomized placebo-controlled trial. J. Cancer Surviv. 2017, 11, 401–409. [Google Scholar] [CrossRef]
- Ritterband, L.M.; Bailey, E.T.; Thorndike, F.P.; Lord, H.R.; Farrell-Carnahan, L.; Baum, L.D. Initial evaluation of an Internet intervention to improve the sleep of cancer survivors with insomnia. Psycho Oncol. 2012, 21, 695–705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roscoe, J.A.; Garland, S.; Heckler, C.E.; Perlis, M.L.; Peoples, A.R.; Shayne, M.; Savard, J.; Daniels, N.P.; Morrow, G.R. Randomized Placebo-Controlled Trial of Cognitive Behavioral Therapy and Armodafinil for Insomnia After Cancer Treatment. J. Clin. Oncol. 2015, 33, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Savard, J.; Simard, S.; Blanchet, J.; Ivers, H.; Morin, C.M. Prevalence, Clinical Characteristics, and Risk Factors for Insomnia in the Context of Breast Cancer. Sleep 2001, 24, 583–590. [Google Scholar] [CrossRef] [Green Version]
- Quesnel, C.; Savard, J.; Simard, S.; Ivers, H.; Morin, C.M. Efficacy of cognitive-behavioral therapy for insomnia in women treated for nonmetastatic breast cancer. J. Consult. Clin. Psychol. 2003, 71, 189–200. [Google Scholar] [CrossRef]
- Savard, J.; Davidson, J.R.; Ivers, H.; Quesnel, C.; Rioux, D.; Dupéré, V.; Lasnier, M.; Simard, S.; Morin, C.M. The association between nocturnal hot flashes and sleep in breast cancer survivors. J. Pain Symptom Manag. 2004, 27, 513–522. [Google Scholar]
- Savard, J.; Simard, S.; Ivers, H.; Morin, C.M. Randomized Study on the Efficacy of Cognitive-Behavioral Therapy for Insomnia Secondary to Breast Cancer, Part I: Sleep and Psychological Effects & Part II: Immunologic Effects. JCO 2005, 23, 6097–6106. [Google Scholar]
- Tremblay, V.; Savard, J.; Ivers, H. Predictors of the effect of cognitive behavioral therapy for chronic insomnia comorbid with breast cancer. J. Consult. Clin. Psychol. 2009, 77, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Savard, J.; Villa, J.; Ivers, H.; Simard, S.; Morin, C.M. Prevalence, Natural Course, and Risk Factors of Insomnia Comorbid with Cancer Over a 2-Month Period. J. Clin. Oncol. 2009, 27, 5233–5239. [Google Scholar] [CrossRef]
- Savard, J.; Ivers, H.; Villa, J.; Caplette-Gingras, A.; Morin, C.M. Natural Course of Insomnia Comorbid with Cancer: An 18-Month Longitudinal Study. J. Clin. Oncol. 2011, 29, 3580–3586. [Google Scholar] [CrossRef] [PubMed]
- Savard, J.; Hervouet, S.; Ivers, H. Prostate cancer treatments and their side effects are associated with increased insomnia. Psycho-Oncology 2012, 22, 1381–1388. [Google Scholar] [CrossRef] [PubMed]
- Casault, L.; Savard, J.; Ivers, H.; Savard, M.-H. A randomized-controlled trial of an early minimal cognitive-behavioural therapy for insomnia comorbid with cancer. Behav. Res. Ther. 2013, 67, 45–54. [Google Scholar] [CrossRef]
- Savard, J.; Savard, H.-M. Insomnia and Cancer. Prevalence, Nature, and Nonpharmacologic Treatment. Sleep Med. Clin. 2013, 8, 373–387. [Google Scholar] [CrossRef]
- Savard, J.; Ivers, H.; Savard, M.H.; Morin, C.M. Is a Video-Based Cognitive Behavioral Therapy for Insomnia as Efficacious as a Professionally Adminis-tered Treatment in Breast Cancer? Results of a Randomized Controlled Trial. Sleep 2014, 37, 1305–1314. [Google Scholar] [CrossRef]
- Savard, J.; Ivers, H.; Savard, M.-H.; Morin, C.M. Long-Term Effects of Two Formats of Cognitive Behavioral Therapy for Insomnia Comorbid with Breast Cancer. Sleep 2016, 39, 813–823. [Google Scholar] [CrossRef] [Green Version]
- Simeit, R.; Deck, R.; Conta-Marx, B. Sleep management training for cancer patients with insomnia support care. Support Care Cancer 2004, 12, 176–183. [Google Scholar] [CrossRef]
- Zhou, E.S.; Vrooman, L.M.; Manley, P.E.; Crabtree, V.M.; Recklitis, C.J. Adapted Delivery of Cognitive-Behavioral Treatment for Insomnia in Adolescent and Young Adult Cancer Survivors: A Pilot Study. Behav. Sleep Med. 2016, 15, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Campos-Rodriguez, F.; Martinez-Garcia, M.A.; Martinez, M.; Duran-Cantolla, J.; Peña, M.D.L.; Masdeu, M.J.; Gonzalez, M.; Campo, F.D.; Gallego, I.; Marin, J.M.; et al. Association between Obstructive Sleep Apnea and Cancer Incidence in a Large Multicenter Spanish Cohort. Am. J. Respir. Crit Care Med. 2013, 187, 99–105. [Google Scholar] [CrossRef] [Green Version]
- Cao, J.; Feng, J.; Li, L.; Chen, B. Obstructive sleep apnea promotes cancer development and progression: A concise review. Sleep Breath. 2015, 19, 453–457. [Google Scholar] [CrossRef]
- Dewan, N.A.; Nieto, F.J.; Somers, V.K. Intermittent hypoxemia and OSA: Implications for comorbidities. Chest 2015, 147, 266–274. [Google Scholar] [CrossRef] [Green Version]
- Faiz, S.A.; Balachandran, D.; Hessel, A.C.; Lei, X.; Beadle, B.M.; William, N.W.; Bashoura, L. Sleep-Related Breathing Disorders in Patients with Tumors in the Head and Neck Region. Oncologist 2014, 19, 1200–1206. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Merino, E.; Arriero, J.M.; Chiner, E.; Signes-Costa, J.; Marco, J. Obstructive Sleep Apnea Syndrome as First Manifestation of Pharyngeal Non-Hodgkin’s Lym-phoma. Respiration 2003, 70, 107–109. [Google Scholar] [CrossRef]
- Kendzerska, T.; Leung, R.S.; Hawker, G.; Tomlinson, G.; Gershon, A.S. Obstructive sleep apnea and the prevalence and incidence of cancer. Can. Med. Assoc. J. 2014, 186, 985–992. [Google Scholar] [CrossRef] [Green Version]
- Marshall, N.S.; Wong, K.K.; Cullen, S.R.; Knuiman, M.W.; Grunstein, R.R. Sleep Apnea and 20-Year Follow-Up for All-Cause Mortality, Stroke, and Cancer Incidence and Mortal-ity in the Busselton Health Study Cohort. JCSM 2014, 10, 355–362. [Google Scholar] [CrossRef] [Green Version]
- Martínez-García, M.Á.; Campos-Rodriguez, F.; Farre, R. Sleep apnoea and cancer: Current insights and future perspectives. Eur. Respir. J. 2012, 40, 1315–1317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nieto, F.J.; Peppard, P.E.; Young, T.; Finn, L.; Hla, K.M.; Farré, R. Sleep-disordered Breathing and Cancer Mortality Results from the Wisconsin Sleep Cohort Study. Am. J. Respir Crit Care Med. 2012, 186, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Partinen, M.; Jamieson, A.; Guilleminault, C. Long-term Outcome for Obstructive Sleep Apnea Syndrome Patients. Chest 1988, 94, 1200–1204. [Google Scholar] [CrossRef]
- Seidell, J. Waist circumference and waist/hip ratio in relation to all-cause mortality, cancer and sleep apnea. Eur. J. Clin. Nutr. 2009, 64, 35–41. [Google Scholar] [CrossRef] [Green Version]
- Adams, C.; McKeon, A.; Silber, M.H.; Kumar, R. Narcolepsy, REM sleep behavior disorder, and supranuclear gaze palsy associated with Ma1 and Ma2 antibodies and tonsillar carcinoma. Arch. Neurol. 2011, 68, 521–524. [Google Scholar] [CrossRef] [Green Version]
- Landolfi, J.C.; Nadkarni, M. Paraneoplastic limbic encephalitis and possible narcolepsy in a patient with testicular cancer: Case study. Neuro Oncol. 2003, 5, 214–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tseng, C.-M.; Chen, Y.-T.; Tao, C.-W.; Ou, S.-M.; Hsiao, Y.-H.; Li, S.-Y.; Chen, T.-J.; Perng, D.-W.; Chou, K.-T. Adult narcoleptic patients have increased risk of cancer: A nationwide population-based study. Cancer Epidemiology 2015, 39, 793–797. [Google Scholar] [CrossRef]
- Saini, A.; Berruti, A.; Strambi, L.F.; Castronovo, V.; Rametti, E.; Giuliano, P.L.; Ramassotto, B.; Picci, R.L.; Negro, M.; Campagna, S.; et al. Restless Legs Syndrome as a Cause of Sleep Disturbances in Cancer Patients Receiving Chemotherapy. J. Pain Symptom Manag. 2013, 46, 56–64. [Google Scholar] [CrossRef]
- Jianhua, C.; Xiuqin, L.; Quancai, C.; Heyang, S.; Yan, H. Rapid Eye Movement Sleep Behavior Disorder in a Patient with Brainstem Lymphoma. Intern. Med. 2013, 52, 617–621. [Google Scholar] [CrossRef] [Green Version]
- Shinno, H.; Kamei, M.; Maegawa, T.; Satake, A.; Inami, Y.; Horiguchi, J.; Nakamura, Y. Three Patients with Cancer Who Developed Rapid-Eye-Movement Sleep Behavior Disorder. J. Pain Symptom Manag. 2010, 40, 449–452. [Google Scholar] [CrossRef] [PubMed]
- Acker, J.G.; Becker-Carus, C.; Büttner-Teleaga, A.; Cassel, W.; Danker-Hopfe, H.; Dück, A.; Frohn, C.; Hein, H.; Penzel, T.; Rodenbeck, A.; et al. The role of actigraphy in sleep medicine. Somnologie Schlafforschung Schlafmed. 2021, 25, 89–98. [Google Scholar] [CrossRef]
- Acker, J.; Golubnitschaja, O.; Büttner-Teleaga, A.; Richter, K. Wrist actigraphic approach in primary, secondary and tertiary care based on the principles of predictive, preventive and personalised (3P) medicine. EPMA J. 2021, 12, 349–363. [Google Scholar] [CrossRef]
- Translator Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Peter, L.; Reindl, R.; Zauter, S.; Hillemacher, T.; Richter, K. Effectiveness of an Online CBT-I Intervention and a Face-to-Face Treatment for Shift Work Sleep Disorder: A Comparison of Sleep Diary Data. Int. J. Environ. Res. Public Heal. 2019, 16, 3081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| First Phenotype |
|
| Second Phenotype |
|
| Third Phenotype |
|
| Fourth Phenotype |
|
| Author | Sample | Fatigue-Measurement | Sleep-/Rhythm-Measurement | Results |
|---|---|---|---|---|
| Ancoli-Israel et al., Eur J Cancer Care 2001; 10 (4): 245–255 [1] | Metaanalysis of existing research: Sleep & Fatigue | |||
| Ancoli-Israel et al., Support Care Cancer 2006; 14 (3): 201–209 [2] | 85 Mamma CA/stages I–IIIA | Multidimen. Fatigue Symptom Inventory (MFSI-SF) | Actigraphy; Sleep diary PSQI; FOSQ |
|
| Ancoli-Israel et al., Support Care Cancer 2014; 22: 2535–2545 [3] | 68 Mamma CA/stages I–III 60 Controls Data collection at three times: (1) baseline/before chemo (2) end of cycle 4 (3) 1 year post-chemo | Multidimen. Fatigue Symptom Inventory (MFSI-SF) | Actigraphy; PSQI |
|
| Banthia et al., Psychol Health 2009; 24 (8): 965–980 [4] | 70 Mamma CA/stages I-IV | 5 dimensions CrF (general, physical, mental, emotional fatigue + vigor) Multidimen. Fatigue Symptom Inventory (MFSI-SF) | PSQI; CES-D |
|
| Berger & Farr, Oncol Nurs Forum 1999; 26 (10): 1663–1671 [5] | 72 Mamma CA/stages I-II | Piper Fatigue Scale | Actigraphy |
|
| Chang et al., Cancer 2000; 88 (5): 1175–1183 [6] | 240 CA | Memorial Symptom Assessment Scale (MSAS)/Item “Lack of Energy” | Functional Assessment Cancer Therapy (FACT-G)/Skala GF/Item Sleep | ↑ Fatigue leads to ↑ sleep problems ↑ pain |
| Cimprich, Cancer Nurs 1999; 22 (3): 185–194 [7] | 74 Mamma CA | Symptom Distress Scale; POMS | no |
|
| Clevenger et al., Brain Behav Immun 2012; 26 (7): 1037–1044 [8] | 136 Ovarian CA – Interleukin-6 (IL-6) | POMS-SF; Multidimen. Fatigue Symptom Inventory (MFSI); Fatigue Symptom Inventory (FSI) | PSQI; Sleep diary | before surgery higher IL-6 → significant relationship (↑ Sleep disorders & ↑ Fatigue) after surgery lower IL-6 → significant relationship (↓ Sleep disorders & ↓ Fatigue) |
| Engstrom et al., Cancer Nurs 1999; 22(2): 143–148 [9] | 150 CA – Phase I 42 CA – Phase II | no | Telefon Interview | Phase I: Report—44% poorly sleep Phase II: Report—45% sleep problems (1/2 severe; main problems: nightly awake, ↓ TST, difficulty to fall asleep) |
| Fiorentino et al., Drug Discov Today Dis Models 2011; 8 (4): 167–173 [10] | 40 Mamma CA/stages I–III | Multidimen. Fatigue Symptom Inventory (MFSI-SF) | Actigraphy | later sleep time & later morning awakening (rhythm shift) leads to ↑ Fatigue |
| Illi et al., Cytokine 2012; 58 (3): 437–447 [12] | 168 CA Patients 85 Caring relatives – Interleukin-4 (IL-4) | Lee Fatigue Scale | General Sleep Disturbance Scale (GSDS) | phenotype for disease behaviour → role of IL-4 in symptom clusters → 3 classes |
| Kaye et al., 1983; 114: 107–113 [13] | 30 CA28 Cardiological Patients24 Controls | no | Sleep Behaviour Questionnaire |
|
| Liu et al., Psychooncology 2009; 18 (2): 187–194 [14] | 76 Mamma CA /stages I–III | Multidimen. Fatigue Symptom Inventory (MFSI-SF) | PSQI | significant correlation between Fatigue & Sleep parameters |
| Liu et al., Sleep 2012a; 35 (2): 237–245 [15] | 97 Mamma CA/stages I–III | Multidimen. Fatigue Symptom Inventory (MFSI-SF) | Actigraphy; PSQI | comparison T0 & Chemotherapy: → Fatigue ↑ & ↓ SQ → Relationship: + CrF & subjective sleep (PSQI) + CrF & objective sleep (Actigraphy)/TST - CrF & objective sleep (Actigraphy) /Wake daytime |
| Liu et al., Brain Behav Immun 2012b; 26 (5): 706–713 [16] | 53 Mamma CA/stages I–III – Interleukin-6 (IL-6) – Interleukin-1 Receptor Antagonist (IL-1RA) – C-Reactive Protein (CRP) | Multidimen. Fatigue Symptom Inventory (MFSI-SF) | PSQI | comparison T0 & Chemotherapie:
underlie biochemical mechanism |
| Miaskowski & Lee, Journal of Pain and Symptom Management 1999; 17 (5): 320–332 [17] | 24 Bone metastases patients | Lee Fatigue Scale | Actigraphy | Fatigue: ↑ at evening & ↓ at morning; Sleep: ↓ SE; Fatigue associated with
|
| Mormont et al., Pathol Biol 1996; 44(3): 165–171 [18] | 30 Colorectal CA | no | Actigraphy | < difference in rest/activity between day & night |
| Mormont et al., Clin Cancer Res 2000; 6 (8): 3038–3045 [19] | 200 Colorectal CA | no | Actigraphy | 2-years-survivors 5x higher than those with changes in activity rhythms |
| Morrow, G.R. et al., ???, 1999 (look: at Roscoe et al., Support Care Cancer 2002; 10: 329–336) [20] | 78 Mamma CA | Multidimentional Assessment of Fatigue; Fatigue Symptom Checklist; POMS | Actigraphy | robust & consistent Circadian rhythms associated with ↓ Fatigue (even after depression) |
| Mustian et al., Oncol Hematol Rev 2012; 8 (2): 81–88 [21] | Overview Prevalence: i.e., Fatigue & Sleep | |||
| Owen et al., Oncol Nurs Forum 1999; 26 (10): 1649–1651 [22] | 15 CA | no | Self-Report; PSQI | CA Patients significant ↓ SQ, ↓ SE & ↑ SOL |
| Palesh et al., J Clin Oncol 2009; 28 (2): 292–298 [23] | 823 CA (after Chemo) | POMS/Fatigue Inactivity; POMS/Energy; Fatigue Symptom Checklist; Multidimen. Assessment of Fatigue | Hamilton Depression Inventory (HDI) |
|
| Reyes-Gibby et al., Lancet Oncol 2008; 9 (8): 777–785 [24] | Overview: Cytokines as markers for Cancer-Related Symptoms | Memorial Symptom Assessment Scale (MSAS)/Item “Lack of Energy” | Functional Assessment Cancer Therapy (FACT-G)/Scale GF/ Item Sleep | Polymorphism in different Cytokine Genes = Potential markers for genetic susceptibility
|
| Roscoe et al., The Oncologist 2007; 12 (suppl 1): 35–42 [25] | Review: Cancer-Related Fatigue and Sleep Disorders | |||
| Silberfarb et al., J. Clin Oncol 1993; 11 (5): 997- 1004 [26] | 15 Mamma CA 17 Lung CA 32 Insomnics 32 Controls | no | PSG (SE, SOL, WASO) | Lung CA ↓ SE, ↑ SOL & ↑ WASO compared with Mamma CA & Controls |
| Author | Sample | Measuring Instrument | Measuring Time | Results |
|---|---|---|---|---|
| Davidson et al., Social Science & Medicine 2002; 54: 1309–1321 [27] | 982 Cancer patients 303 Breast 108 Gastrointestinal (GI) 155 Genitourinary (GU) 180 Gynecologic (GYN) 114 Lung 123 Skin | Sleep Survey Questionnaire
| 3 months cross-sectional survey study | analyses of sleep disorders pevalence
|
| Methods: (1) prevalence of reported sleep problems/six clinics (2) sleep problem prevalence in relation to cancer treatment (3) nature of insomnia (type, duration & associated factors) |
| Author | Sample | Measuring Instrument(s) | Measuring Time(s) | Results |
|---|---|---|---|---|
| Graci, J Support Oncol 2005; 3 (5): 349–359 [43] | Review: Pathogenesis & Management of Cancer-Related Insomnia | |||
| Howell et al., Annals of Oncology 2014; 25: 791–800 [45] | Review: grey literature data sources and empirical databases from 2004 to 2012 | Review includes:
| ||
| Minton & Stone, BMJ S&P Care 2012; 2: 231–238 [53] | 114 Mamma CA - 69 Controls - 45 CRFS | Actigraphy; Insomnia Severity Index (ISI) | between 3 months and 2 years after cancer therapy | Insomnia prevalence significant > in CRFS < in Controls (effect ISI > Actigraphy !) |
| Park et al., Sleep Med Res 2016; 7(2): 48–54 [54] | 1248,914 patients analyzed 33,262 were diagnosed with cancer | ICD-10 | 1-year cross-sectional study | Insomnia was prevalent in 8.21%: 15.2% lung cancer 9.2% non-Hodgkin’s lymphoma 8.8% bladder cancer 8.6% colorectal cancer 8.0% stomach cancer 7.8% prostate, breast & cervix cancer 6.6% liver cancer 5.8% thyroid cancer |
| Savard et al., Sleep 2001; 24 (5): 583–590 [58] | 300 Mamma CA | Insomnia Interview Schedule (IIS)—Revised | one time | 19% Insomnia syndrome 95% chronic 33% onset of insomnia followed by breast cancer diagnosis 58% cancer either caused or aggravated the sleep difficulties factors associated with an increased risk for insomnia were:
|
| Savard et al., J Clin Oncol 2009; 27: 5233–5239 [63] | 991 CA 466 Mamma 269 Prostata 118 Gynecological | Self-Report Scales; Insomnia Diagnostic Interview | T1—Baseline T2—2 months Tx—6, 10, 14 & 18 months | total: 59.5% 28.5% Insomnia 31.0% Insomnia symptoms; Mamma & Gynecological > Prostata; Insomnia ↓ Therapy course |
| Savard et al., J Clin Oncol 2011; 29: 3580–3586 [64] | 856 CA 426 Mamma 235 Prostata 96 Gynecological | Insomnia Interview Schedule (IIS) | T1—Baseline Tx—2, 6, 10 & 14 months T6—18 months | total: 59% 28% Insomnia 31% Insomnia symptoms; Mamma & Gynecological > Prostata; Insomnia ↓ Therapy course |
| Savard & Savard, Sleep Med Clin 2013; 8: 373–387 [67] | Review: Insomnia – Cancer – Prevalence – Risk factors – Nonpharmacologic treatment | |||
| Author | Sample | Measuring Instrument(s) | Measuring Time(s) & Method(s) | Results |
|---|---|---|---|---|
| Barton et al., J Sup- port Oncol 2011; 9 (1) 24–31 [28] | 227 (202) Cancer patients 130 Breast 14 Colon 4 Prostate 52 Other | PSQI; FOSQ (Functional Outcomes of Sleep Questionnaire); BFI (Brief Fatigue Inventory); POMS (Profile of Mood States); TNAS (Toxicity Numeric Analogue Scale); CTCAE (Common Terminology Criteria for Adverse Events) | T1—Baseline T2—Follow-up (4 weeks) T3—Follow-up (8 weeks) |
|
| Methods: - RCT, dopple-blind - 450 mg Valerian (Herbal Medicine versus Placebo) | ||||
| Berger et al., Psycho-oncology 2009; 18 (6): 634–646 [29] | 219 Cancer patients/ stages I–III | Actigraphy; PSQI; Sleep Diary (SOL, WASO, TIB, TST, SE) | T1—Baseline T2—Follow-up (within 7 days) T3—Follow-up (30 days) |
|
| Methods: - RCT - BT versus Controls (Behavioural Therapy [Individualized Sleep Promotion Plan (ISPP)]) | ||||
| Chen et al., Breast Cancer Res Treat 2014; 145 (2): 381–388 [30] | 95 Postmenopausal Breast CA/stages 0–III | PSQI; CES-D (Center for Epidemiologic Studies – Depression Scale); NCCTG (North Central Cancer Treatment Group) | T1—Baseline T2—Follow-up (4 months) |
|
| Methods: - RCT, dopple-blind - 3 mg Melatonin versus Placebo | ||||
| Choi et al., Integrative Cancer Therapies 2017; 16 (2) 135–146 [31] | A Systematic Review of Randomized Clinical Trials: Acupuncture for Managing Cancer-Related Insomnia | |||
| Dupont et al., Health Psychol 2014; 33 (2): 155–163 [32] | 558 Mamma CA | SF-36 (partly); IES-R (Revised Impact of Event Scale); CES-D (Center for Epidemiologic Studies—Depression Scale); PANAS (Positive and Negative Affect Scale) FSI (Fatigue Symptom Inventory); MOS (Medical Outcomes Study); BCPT (Breast Cancer Prevention Trial) | T1—Baseline T2—Post-Treatment (4 weeks) T3—Follow-up (2 months) T4—Follow-up (6 months) T5—Follow-up (12 months) |
|
| Methods: three types of information: (1) print material (2) print material & peer- modeling videotape (3) print material, videotape, 2 education sessions & information workbook | ||||
| Epstein & Dirksen, Oncology Nursing Forum 2007; 34 (5); 51–59 [33] | 81 Mamma CA - 40 Controls - 41 CBT-I | Actigraphy; Sleep Diary (SOL, WASO, TIB, TST, SE) PFS (Piper Fatigue Scale) | T1—Baseline T2—Post-CBT-I (6 weeks) T3—Follow-up (12 weeks) |
|
Methods:
| ||||
| Espie et al., J of Clinical Oncology 2008; 26: 4651–4658 [34] | 150 CA 87 Mamma 34 Prostate 24 Colorectal 5 Gynecological (110 CBT/50 TAU) | PSQI; ESS; Sleep Diary (SOL, WASO, TST, SE); HADS; FSI (Fatigue Symptom Inventory); CrQoL (Cancer-Related Quality of Life); FACT-G (Functional Assessment of Cancer Therapy Scale – General) | T1—Baseline T2—Post-Treatment T3—Follow-up (6 months) |
|
Methods:
| ||||
| Fiorentino et al., Nature and Science of Sleep 2010; 2: 1–8 [35] | 21 Mamma CA - 11 IND-CBT-I - 10 Controls | Actigraphy; PSQI; Insomnia Severity Index (ISI); Sleep Diary (SOL, WASO, TIB, TST, SE) | T1—Baseline T2—Post-CBT-I (6 weeks) T3—Follow-up (12 weeks) |
|
Methods:
| ||||
| Fleming (Espie) et al., Psychooncology 2014; 23 (6): 679–684 [36] | 113 Cancer patients with Insomnia - 73 CBT-I - 40 Controls | PSQI; Sleep Diary (SOL, WASO, TIB, TST, SE) HADS; FSI (Fatigue Symptom Inventory) | T1—Baseline T2—Post-Treatment T3—Follow-up (6 months) |
|
Methods:
| ||||
| Garland et al., Contemporary Clinical Trials 2011; 32 (5): 747–754 [37] | ??? | Actigraphy; Sleep Diary (SOL, WASO, TST, SE) ??? | T1—Baseline T2—Post-Treatment (2 months) T3—Follow-up (3 months) |
|
| Methods: CBT-I versus MBSR (Mindfulness-Based Stress Reduction) | ||||
| Garland et al., J Clin Oncol 2014; 32: 1–9 [38] | 327 screened CA 111 randomly assigned 53 Breast 12 Prostate 11 Blood/lymph 10 Female Genitourinary 9 Head & Neck 7 Colon/GI 7 Lung 2 Skin CBT-I: n = 47 MBSR: n = 64 | Actigraphy; PSQI; Insomnia Severity Index (ISI); Sleep Diary (SOL, WASO, TST, SE) | T1—Baseline T2—Post-Treatment (2 months) T3—Follow-up (5 months) |
|
| Methods: CBT-I versus MBSR (Mindfulness-Based Stress Reduction) | ||||
| Garland et al., Neuropsychiatric Disease and Treatment 2014; 10: 1113–1124 [39] | Review: Efficency of CBT-I in cancer Inclusion of 4 studies |
→ clinically improvements in subjective sleep outcomes improved sleep → Improvement in:
| ||
| Garland et al., Explore (N.Y.) 2015; 11 (6): 445–454 [40] | 72 Cancer patients MBCR: n = 32 CBT-I: n = 40 | ??? | T1—Baseline T2—Post-Treatment (? months) T3—Follow-up (3 months) |
|
| Methods: CBT-I versus MBCR (Mindfulness-Based Cancer Recovery) | ||||
| Garland et al., Contemporary Clinical Trials 2016; 47: 349- 355 [41] | 160 Cancer patients with Insomnia | ??? | T1—Baseline T2—Mid-Treatment (4 weeks) T3—Post-Treatment (8 weeks) T4—Follow-up (3 months) | ??? |
Methods:
| ||||
| Garland et al., Sleep Medicine 2016; 20: 18–24 [42] | 88 Cancer patients with Insomnia | ESS; Sleep Diary (SOL, WASO, TST, SE) | T1—Baseline T2—Post-Treatment (7 weeks) T3—Follow-up (3 months) |
|
| Methods: (RCT) (1) CBT-I + P (CBT-I and Placebo) (2) CBT-I + A (CBT-I and Armodafinil) (3) ARM (Armodafinil alone) (4) PLA (Placebo alone) | ||||
| Heckler (Garland) et al., Supportive Care in Cancer 2016; 24 (5): 2059–2066 [44] | 96 Cancer patients with Insomnia | Insomnia Severity Index (ISI); BFI (Brief Fatigue Inventory); FACIT-Fatigue scale | T1—Baseline T2—Post-Treatment (7 weeks) T3—Follow-up (3 months) |
|
| Methods: (RCT) (1) CBT-I + P (CBT-I and Placebo) (2) CBT-I + A (CBT-I and Armodafinil) (3) ARM (Armodafinil alone) (4) PLA (Placebo alone) | ||||
| Irwin et al., JNCIM 2014; No. 50; 295–301 [46] | 90 Mamma CA random subsample (n = 48) | Blood samples: - C-Reactive Protein (CRP) - Interleukin-6 (IL-6) - Tumor Necrosis Factor-α (TNF) subsample analyzed by genome-wide transcriptional profiling | T1—Baseline T2—Post-Treatment (3 months) |
|
| Methods: CBT-I versus TCC (Tai Chi Chih) | ||||
| Kim M. et al., BMJ open, 2017; 7 (8): 1- 10 [47] | 45 Cancer patients | Actigraphy; Insomnia Severity Inventory (ISI); PSQI; Sleep Diary (SOL, WASO, TIB, TST, SE) BDSS (Blood Deficiency Scoring System); EA (Electroacupuncture); FACT-F (Functional Assessment of Cancer Therapy- Fatigue); MoCA (Montreal Cognitive Assessment) | T1—Baseline T2—Treatment (3 weeks) T2—Post-Treatment (5 weeks) T2—Post-Treatment (9 weeks) | Without results !!! „The result of this study will be published in peer-reviewed journals or presented at academic conferences.“ |
| Methods: (4 weeks) EA versus Sham-EA (Electroaccupuncture) versus TAU (Treatment As Usual) | ||||
| Kim S.W. et al., Psychiatry and Clinical Neurosciences 2008; 62: 75–83 [48] | 45 Cancer patients 25 Lung 5 Breast 6 Gastrointestinal tract 3 Hepatobiliary tract 3 Other malignancy | C-LSEQ (Chonnam National University Hospital- Leeds Sleep Evaluation Questionnaire) SF-36; MADRS (Montgomery-Asberg Depression Rating Scale); EuroQoL (EQ) -5D | T1—Baseline T2—Post-Treatment (4 weeks) | mirtazapine rapidly improved sleep disturbance, nausea, pain and quality of life, as well as depression in cancer patients Sleep ↑: ↑ TST, ↓ SOL, ↓ SQ |
Methods:
| ||||
| Kröz et al., BMC cancer 2017; 17 (1), 166: 1–13 [49] | 126 Mamma CA | PSQI; CFS-D (Cancer Fatigue Scale) | T1—Baseline T2—Post-Treatment (10 weeks) T3—Follow-up (6 months) |
|
| Methods: (RCT) (a) MT (Multimodal Treatment) (b) CT (MT + AeT) (Combined Treatment) (c) AeT (Aerobic Training) | ||||
| Lengacher et al., Psychooncology 24 (4): 424–432 [50] | 79 Mamma CA /stages 0-III | OSP (Objective Sleep Parameters): - Actigraphy SSP (Subjective Sleep Parameters): - PSQI; - Sleep diary | T1—Baseline T2—Treatment (6 weeks) T2—Post-Treatment (12 weeks) |
|
| Methods: (RCT) MBSR (BC) vs. UC (Mindfulness-Based Stress Reduction [Breast Cancer]) (Usual Care) | ||||
| Marshall-McKenna et al., Supportive Care in Cancer 2016; 24 (4): 1821–1829 [51] | 74 Mamma CA with Insomnia - 68.9 % pre-menopausal - 31.1% post-menopausal | HADS; FACT-B (Functional Assessment of Cancer Therapy - Breast) sleep/hot flush diaries (over 2-week periods) | T1—Baseline T2—Treatment (x weeks) T3—Post-Treatment (x weeks) |
|
| Methods: (RCT) - Intervention Arm: CPPT + SC (Cool Pad Pillow Topper + Standard Care) vs. - Control Arm: SC (Standard Care) | ||||
| Mendoza et al., Psychooncology 2017; 26 (11): 1832–1838 [52] | 44 Cancer patients | MOOS (Medical Outcomes Survey Sleep); PROMIS (Fatigue) (Problem Index Patient-reported Outcomes Measurement Information System); NRS (Pain intensity) (Numerical Rating Scales) | T1—Baseline T2—Treatment (3 weeks) T3—Post-Treatment (3 months) | VMWH-CBT vs. Controls → beneficial effects of the VMWH-CBT - sleep problems - fatigue - average pain intensity |
| Methods: - RCT, cross-over - VMWH-CBT vs. Controls (Valencia model of Waking Hypnosis with Cognitive-Behavioural Therapy) | ||||
| Peoples (Garland) et al., Journal of Cancer Survivorship 2017; 11 (3): 401–409 [55] | 95 Cancer patients with Insomnia | Insomnia Severity Index (ISI); FACT-G (QoL) (Functional Assessment of Cancer Therapy - General) | T1—Baseline T2—Post-Treatment (7 weeks) T3—Follow-up (3 months) |
|
| Methods: (RCT) (1) CBT-I + P (CBT-I and Placebo) (2) CBT-I + A (CBT-I and Armodafinil) (3) ARM (Armodafinil alone) (4) PLA (Placebo alone) | ||||
| Ritterband et al., Psychooncology 2012; 21 (7): 695–705 [56] | 28 Cancer patients with Insomnia | Insomnia Severity Index (ISI); Sleep Diary (SOL, WASO, TIB, TST, SE) MFSI-SF (Multidimensional Fatigue Symptom Inventory - Short Form); UQ (Internet Intervention Utility Questionnaire); HADS; SF-12 | T1—Baseline T2—Post-Treatment (3 months) | SHUTi vs. Controls → beneficial effects of the SHUTi - ↓ ISI - ↓ HADS - ↑ SF-12 - Sleep Diary: ↑ SE, ↑ TST, ↓ SOL & ↓ WASO (Controls improved a little too: SE & WASO) |
Methods:
| ||||
| Roscoe, J.A., (Garland, Sh.N.) et al., Journal of Clinical Oncology 2015; 33 (2): 165–171 [57] | 96 Cancer patients with Insomnia | PSQI; Insomnia Severity Index (ISI) | T1—Baseline T2—Post-Treatment (7 weeks) T3—Follow-up (3 months) | CBT-I + A & CBT-I + P: → CBT-I improves Insomnia Severity (ISI) → CBT-I improves Sleep Quality (PSQI) → Armodafinil no effect on Insomnia & SQ |
| Methods: (RCT) (1) CBT-I + P (CBT-I and Placebo) (2) CBT-I + A (CBT-I and Armodafinil) (3) ARM (Armodafinil alone) (4) PLA (Placebo alone) | ||||
| Savard (Quesnel) et al., JCCP 2003; 71 (1): 189–200 [59] | 10 Mamma CA | PSG; Insomnia Severity Inventory (ISI); Sleep Diary (SOL, WASO, TIB, TST, SE) MFI (Multidimensional Fatigue Inventory); BDI & STAI; QLQ-C30+ 3 (European Organization for Research & Treatment of Ca. Quality of Life Questionnaire) | T1—Baseline T2—Post-Treatment (3 months) T3—Follow-up (6 months) | CBT was associated with - ↓ ISI: = ↓ Insomnia severity - ↑ PSG & ↑ Sleep Diary: = ↑ SE, ↑ TST, ↓ SOL & ↓ WASO |
| Savard et al., Journal of Pain and Symptom Management 2004; 27 (6): 513–522 [60] | 24 Mamma CA | PSG; Skin conductance | ??? |
|
| Methods: CBT | ||||
| Savard et al., JCO 2005 I & II; 23 (25): 6083–6096 & 6097- 6106 [61] | 57 women with insomnia caused or aggravated by breast cancer | PSG; Insomnia Severity Inventory (ISI); Sleep Diary (SOL, WASO, TIB, TST, SE) MFI (Multidimensional Fatigue Inventory); HADS; QLQ-C30+ 3 (European Organization for Research & Treatment of Ca. Quality of Life Questionnaire); Immune measures: enumeration of blood cell counts (i.e., WBCs, monocytes, lymphocytes, CD3, CD4, CD8, CD16/CD56) & cytokine product. (Interleukin-1-beta [IL-1β], Interferon gamma [IFN-γ]) | T0—Pre-Waiting T1—Baseline T2—Post-Treatment T3—Follow-up (3 months) T4—Follow-up (6 months) T5—Follow-up (12 months) | CBT was associated with (post-treatment vs. control patients) - ↓ ISI: = ↓ Insomnia severity - ↑ PSG & ↑ Sleep Diary: = ↑ SE, ↑ TST, ↓ SOL & ↓ WASO - higher secretion and/or level of IFN-γ & IL-1β - lower increase of lymphocytes |
| Methods: CBT versus WLC (Waiting-List Control) | ||||
| Savard (Tremblay) et al., JCCP 2009; 77 (4): 742–750 [62] | 57 Mamma CA | PSG; Insomnia Severity Inventory (ISI); Sleep Diary (SOL, WASO, TIB, TST, SE) DBAS (Dysfunctional Beliefs and Attitudes about Sleep Scale); ABS (Adherence to Behavioural Strategies) TEPCQ (Treatment Expectancies and Perceived Credibility Questionnaire); TAPQ (Therapeutic Alliance Perception Questionnaire); HADS | T1—Baseline T2—Post-Treatment (2 months) T3—Follow-up (6 months) |
|
| Methods: CBT versus WLC (Waiting-List Control) | ||||
| Savard et al., Psycho-Oncology 2013; 22 (6): 1381–1388 [65] | 60 Prostate CA | Insomnia Severity Index (ISI); PSQ (Physical Symptoms Questionnaire) | T1—Baseline Tx—1, 2, 4, 6, 8 & 12 months T8—16 months |
|
| Methods: ADT (Androgen Deprivation Therapy) RTH (Radiation therapy) | ||||
| Savard (Casault) et al., Behaviour Research and Therapy 2013; 67: 45–54 [66] | 83 Cancer patients | ??? | T1—Baseline T2—Post-Treatment T3—Follow-up (3 months) T4—Follow-up (6 months) |
|
| Methods: mCBT versus no Treatment (minimal CBT) | ||||
| Savard et al., Sleep 2014; 37 (8): 1305- 1314 [68] | 242 Mamma CA | Actigraphy; Insomnia Severity Index (ISI); Sleep Diary (SOL, WASO, TIB, TST, SE) | T1—Baseline T2—Post-Treatment (6 weeks) |
- ↓ Insomnia severity - ↓ Early Morning Awakenings (EMA) - ↓ depression - ↓ fatigue - ↓ dysfunctional beliefs about sleep
- 71.3% vs. 44.3%, p < 0.005 |
| Methods: (RCT) (1) Professionally administered CBT-I (PCBT-I; n = 81) (2) Video-based CBT-I (VCBT-I; n = 80) (3) no treatment (CTL; n = 81) | ||||
| Savard et al., Sleep 2016; 39 (4): 813–823 [69] | 242 Mamma CA | Insomnia Severity Index (ISI); Insomnia Interview Schedule (IIS); Sleep Diary (SOL, WASO, TIB, TST, SE) MFI (Multidimensional Fatigue Inventory) EORTC QLQ-C30; HADS; DBAS-16 (Dysfunctional Beliefs & Attitudes about Sleep Scale – Abbreviated version); | T1—Baseline T2—Post-Treatment (6 weeks) T3—Follow-up (3 months) T4—Follow-up (6 months) T5—Follow-up (12 months) |
- ↓ Insomnia severity (ISI, IIS) - ↓ Early Morning Awakenings (EMA) - ↓ depression - ↓ anxiety - ↓ dysfunctional beliefs about sleep - ↑ QoL
VCBT-I and CTL: e.g., 12 month FU - 67% vs. 59% vs. 48%, p < 0.100 |
| Methods: (RCT) (1) Professionally administered CBT-I (PCBT-I; n = 81) (2) Video-based CBT-I (VCBT-I; n = 80) (3) no treatment (CTL; n = 81) | ||||
| Simeit et al., Suppor-tive Care in Cancer 2004; 12 (3): 176–183 [70] | 229 Cancer patients (breast, kidney or prostate) | ??? | T1—Baseline T2—Post-Treatment (3-4 weeks) T3—Follow-up (6 months) |
- sleep latency (p < 0.001) - sleep duration (p < 0.001) - sleep efficiency (p < 0.001) - sleep quality (p < 0.001) - sleep medication (p < 0.050) - daytime dysfunction (p < 0.050) - quality-of-life
|
| Methods: (RCT) (1) Progressive Muscle Relaxation (PMR; n = 80) (2) Autogenic Training (AT; n = 71) (3) Control Group (CG; n = 78) | ||||
| Zhou et al., Behavioral Sleep Medicine 2017; 15 (4): 288–301 [71] | 10 (12) Cancer patients | Insomnia Severity Index (ISI); PSQI; Sleep logs [SL]; (SOL, WASO, TIB, TST, SE); SF-12 | T1—Baseline T2—Post-Treatment (20 days) T3—Follow-up (2 months after T2) |
↑ SE, ↓ SOL, ↓ WASO & ↓ EMA - ↓ Insomnia severity (ISI) - ↓ Sleep Quality (PSQI)
- QoL |
| Methods: - Adapted CBT-I 3 x intervention in person (6) and via videoconference (6) | ||||
| Author | Sample | Measuring Instrument(s) | Measuring Time(s) | Results |
|---|---|---|---|---|
| Campos-Rodrigues et al., Am J Respir Crit Care Med 2013; 187 (1): 99–105 [72] | 4910 Patients (Multicentric Cohort Study) | PSG/PG | T—Baseline T2—4.5 years | ↓ TSat<90% vs. ↑ CA Incidence ↑ AHI vs. ↑ CA Incidence → higher Risk: 1. < 65 years; 2. ♂; 3. no CPAP |
| Cao et al., Sleep Breath 2015; 19 (2): 453–457 [73] | Obstructive Sleep Apnea promotes Cancer development and progression (Animal studies) | OSAS = Risk factor
→ activation of HIF-1 & VEGF pathways → tumor growth → aggressive cancer behaviour | ||
| Dewan et al., Chest 2015; 147 (1): 266–274 [74] | Intermittent hypoxemia and OSA: Implications for comorbidities (Animal & Human studies) | Intermittent hypoxemia promotes → Oxidative stress → Inflammation → Increased sympathetic activation → Progression of cancer → Effect of CPAP !!! | ||
| Faiz et al., The Oncologist 2014; 19: 1200–1206 [75] | 56 Patients with tumors in the head and neck region | PSG | Retrospective review from 2006 to 2011 | 1. SRBD = common in patients with tumors in the head/ neck region → caused by sleep disruption 2. Architectural changes from tumor and/or therapy lead to OSA |
| Gomez-Merino et al., Respiration 2003; 70: 107–109 [76] | Case study: 55 years old man non-Hodgkin-Lymphoma | Symptom development:
| ||
| Kendzerska et al., CMAJ 2014; 186 (13): 985–992 [77] | 10,149 Patients | PSG all patients AHI ≥ 5 or suspected OSAS (but AHI < 5) | A) from 1994 to 2010 B) from 1991 to 2013 | Methods:
link between OSA & Cancer development or progression through chronic hypoxemia |
| Marshall et al., JCSM 2014; 10 (4): 355–362 [78] | 400 OSAS-Patients | PG/MESAM IV | T1—Baseline 1990 T2—20 years 2010 (Follow-up) | Follow-up: 397 people removed n = 4 with a previous stroke from the mortality/ CVD/CHD/stroke analyses (n = 393) n = 7 with cancer history from the cancer analyses (n = 390) 20 years Follow-up
1. moderate-severe OSA was significantly associated with - all-cause mortality (HR = 4.2; 95% CI: 1.9, 9.2) - cancer mortality (HR = 3.4; 95% CI: 1.1, 10.2) - incident cancer (HR = 2.5; 95% CI: 1.2, 5.0) - stroke (HR = 3.7; 95% CI: 1.2, 11.8) but not significantly with - CVD incidence (HR = 1.9; 95% CI: 0.75, 4.6) - CHD incidence (HR = 1.1; 95% CI: 0.24, 4.6) 2. mild OSA was associated with a halving in - mortality (HR = 0.5; 95% CI: 0.27, 0.99) |
| Martinez-Garcia et al., Eur Respir J 2012; 40: 1315–1317 [79] | --- Special Article | current insights and perspectives:
→ Cerbrovakular diseases → Metabolic diseases → Systemic inflammatory diseases important role in regulating the various stages of tumor development and progression | ||
| Nieto et al., Am J Respir Crit Care Med 2012; 186 (2): 190–194 [80] | 1522 Patients (Background: Wisconsin Sleep Cohort Study) | PSG | T1—Baseline T2—22 years | SRBD = associat. with ↑ CA Mortality → higher Risk in ↑ SRBD: 1. ↑ AHI; 2. ↓ Tsat<90% |
| Partinen et al., Chest 1988: 94 (6): 1200–1204 [81] | 198 OSAS Patients (Tracheostomy vs. Weight loss) | PG | Retrospective review from 1972 to 1980 | ↑ BMI & ↑ AHI → lead to Vascular death
→ no answer !!! |
| Seidell, Eur J of Clinical Nutrition 2010; 64: 35–41 [82] | Review: Waist circumference and Waist/Hip ratio in relation to all-cause Mortality, Cancer and Sleep Apnea (Human studies) | BMI ↑ → Risk of Cancer ↑ → Risk of OSA ↑ Waist circumference & Waist/Hip ratio → better indicator of all-cause mortality than BMI Relationship Cancer & OSA ??? → no answer !!! |
| Author | Sample | Measuring Instrument(s) | Measuring Time(s) | Results |
|---|---|---|---|---|
| Adams et al., Arch Neurol 2011; 68 (4): 521–524 [83] | Case study: 35 years old man Testicular cancer | Symptom development:
2.2 min. sleep latency with 5 episodes REM*Onset | ||
| Landolfi & Nadkarni, Neuro-Oncology 2003; 5: 214–216 [84] | Case study: 55 years old man Tonsil cancer | Symptom development:
MSLT: 9 min. sleep latency with 2 episodes REM*Onset | ||
| Tseng et al., Cancer Epidemiol 2015; 39 (6): 793–797 [85] | 2,833 Narcoleptics | ??? | from 2000 to 2009/National Health Insurance Research Database | adult narcoleptic patients → higher cancer risk (74 Cancer/SIR 1.32; 95% CI, 1.04–1.66, p = 0.0248) → ♀ = higher Risk: (SIR 1.52; 95% CI, 1.05–2.13, p = 0.026) 1. ↑ Head & Neck CA (SIR 6.17; 95% CI, 1.66–15.80, p = 0.009) 2. ↑ Gastric CA (SIR 4.87; 95% CI, 1.31–12.48, p = 0.020) → underlying mechanism unclear |
| Author | Sample | Measuring Instrument(s) | Measuring Time(s) | Results |
|---|---|---|---|---|
| Saini et al., J Pain Symptom Manage 2013; 46: 56–64 [86] | 173 CA different entities 32.4% Colorectal 17.3% Mamma 7.5% Prostata 6.4% Ovary 5.8% - Bladder - Gastroenteropancreatic Neuroendocrine 3.5 % - Pancreas - Testis - Stomach 2.9% - Lung - Adrenal cortical 2.3% - Uterus - Kidney 1.7% Head & Neck 1.2% Thymus 0.6% - Esophagus - Thyroid | Pittsburgh Sleep Quality Index (PSQI); International Restless Legs Syndrome Study Group rating scale (IRLS); Functional Assessment of Cancer Therapy-General (FACT-G); Hospital Anxiety and Depression Scale (HADS) | T0—before Chemotherapy T1—after Chemotherapy | 58.8% Sleep problems (PSQI > 5) 20.0% RLS positive screened
|
| Author | Sample | Measuring Instrument(s) | Measuring Time(s) | Results |
|---|---|---|---|---|
| Adams et al., Arch Neurol 2011; 68 (4): 521–524 [83] | Case study: 35 years old man Testicular cancer | PSG | Polysomnogram:
| |
| Jianhua, Ch. et al., Intern Med 2013; 52: 617–621 [87] | Case study: 30 years old man Brainstem lymphoma (diffuse large B-cell) | PSG; MRI | Polysomnogram (Sleep Rhythm Disorder):
| |
| Shinno, H. et al., J Pain Symptom Manage 2010; 40 (3): 449–452 [88] | Case study: 3 cases 70–76 years old patients 2 males & 1 femal Advanced cancer (1 x kidney; 2 x stomach) | PSG | Polysomnogram:
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Büttner-Teleagă, A.; Kim, Y.-T.; Osel, T.; Richter, K. Sleep Disorders in Cancer—A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 11696. https://doi.org/10.3390/ijerph182111696
Büttner-Teleagă A, Kim Y-T, Osel T, Richter K. Sleep Disorders in Cancer—A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(21):11696. https://doi.org/10.3390/ijerph182111696
Chicago/Turabian StyleBüttner-Teleagă, Antje, Youn-Tae Kim, Tiziana Osel, and Kneginja Richter. 2021. "Sleep Disorders in Cancer—A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 21: 11696. https://doi.org/10.3390/ijerph182111696
APA StyleBüttner-Teleagă, A., Kim, Y.-T., Osel, T., & Richter, K. (2021). Sleep Disorders in Cancer—A Systematic Review. International Journal of Environmental Research and Public Health, 18(21), 11696. https://doi.org/10.3390/ijerph182111696








