Parental Psychological Flexibility as a Mediating Factor of Post-Traumatic Stress Disorder in Children after Hospitalization or Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Measures
2.2.1. Demographic Questionnaire
2.2.2. Acceptance and Action Questionnaire (AAQ)
2.2.3. Parental Psychological Flexibility Questionnaire (PPF)
2.2.4. UCLA PTSD Reaction Index for DSM-5 Parent/Caregiver Version for Children Aged 6 Years and Younger
2.2.5. Young Child PTSD Checklist (YCPC)
2.2.6. Post-Traumatic Stress Diagnostic Scale (PDS)
2.3. Data Analysis
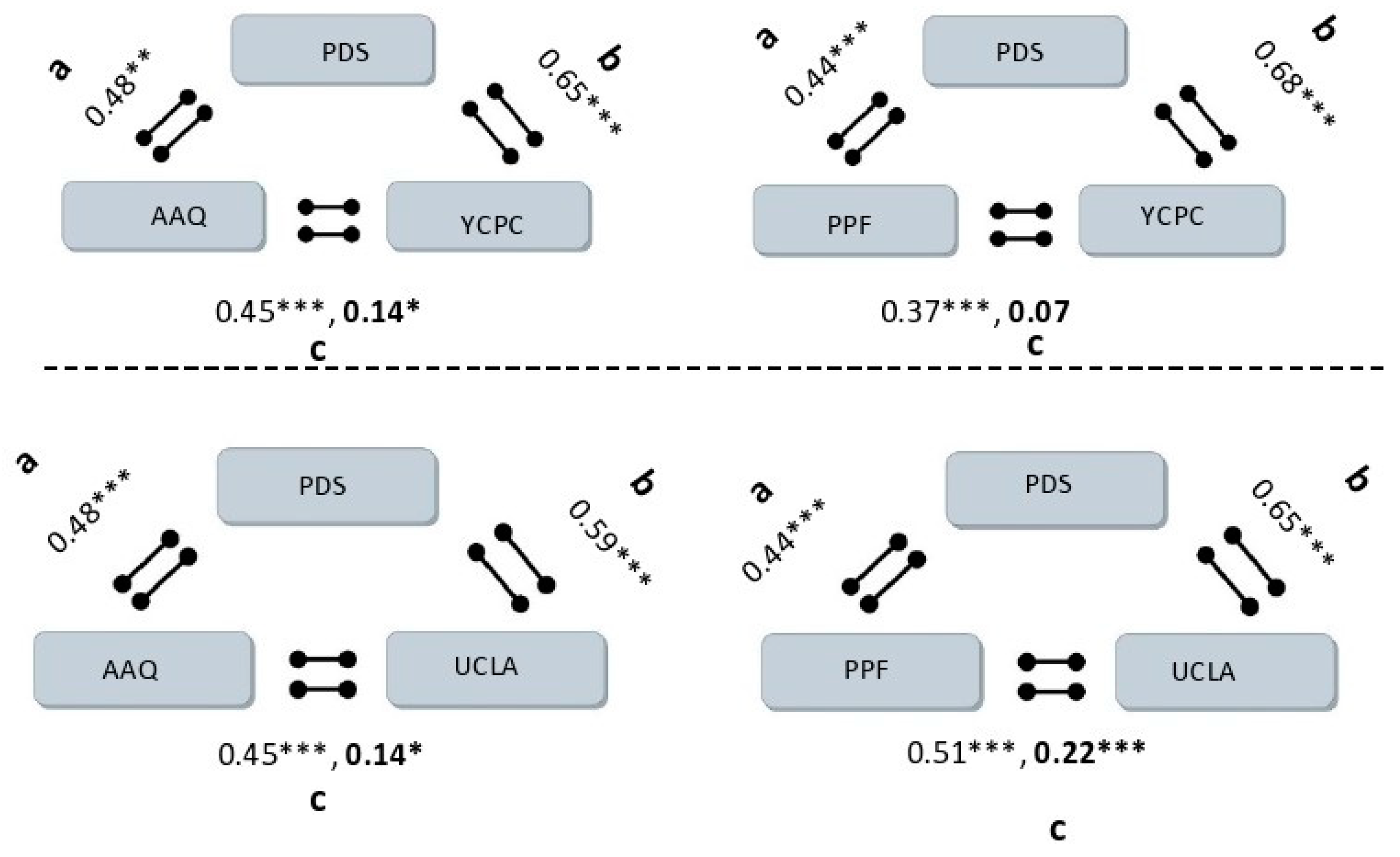
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Terr, L.C. Children of Chowchilla: A study of psychic trauma. Psychoanal. Study Child 1979, 34, 547–623. [Google Scholar] [CrossRef]
- Terr, L.C. Time sense following psychic trauma: A clinical study of ten adults and twenty children. Am. J. Orthopsychiatry 1983, 53, 244. [Google Scholar] [CrossRef]
- Dyregrov, A.; Yule, W. A review of PTSD in children. Child Adolesc. Ment. Health 2006, 11, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Thabet, A.A.M.; Abed, Y.; Vostanis, P. Comorbidity of PTSD and depression among refugee children during war conflict. J. Child Psychol. Psychiatry 2004, 45, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Scheeringa, M.S.; Myers, L.; Putnam, F.W.; Zeanah, C.H. Diagnosing PTSD in early childhood: An empirical assessment of four approaches. J. Trauma. Stress 2012, 25, 359–367. [Google Scholar] [CrossRef]
- Ari, A.B.; Peri, T.; Margalit, D.; Galili-Weisstub, E.; Udassin, R.; Benarroch, F. Surgical procedures and pediatric medical traumatic stress (PMTS) syndrome: Assessment and future directions. J. Pediatr. Surg. 2018, 53, 1526–1531. [Google Scholar] [CrossRef] [PubMed]
- Ari, A.B.; Margalit, D.; Udassin, R.; Benarroch, F. Traumatic stress among school-aged pediatric surgery patients and their parents. Eur. J. Pediatr. Surg. 2019, 29, 437–442. [Google Scholar] [PubMed]
- Forgey, M.; Bursch, B. Assessment and management of pediatric iatrogenic medical trauma. Curr. Psychiatry Rep. 2013, 15, 340. [Google Scholar] [CrossRef]
- Landolt, M.A.; Vollrath, M.; Timm, K.; Gnehm, H.E.; Sennhauser, F.H. Predicting posttraumatic stress symptoms in children after road traffic accidents. J. Am. Acad. Child Adolesc. Psychiatry 2005, 44, 1276–1283. [Google Scholar] [CrossRef]
- Judge, D.; Nadel, S.; Vergnaud, S.; Garralda, E.M. Psychiatric adjustment following meningococcal disease treated on a PICU. Intensive Care Med. 2002, 28, 648–650. [Google Scholar] [CrossRef]
- Rennick, J.E.; Rashotte, J. Psychological outcomes in children following pediatric intensive care unit hospitalization: A systematic review of the research. J. Child Health Care 2009, 13, 128–149. [Google Scholar] [CrossRef] [PubMed]
- Kazak, A.E.; Alderfer, M.; Rourke, M.T.; Simms, S.; Streisand, R.; Grossman, J.R. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J. Pediatr. Psychol. 2004, 29, 211–219. [Google Scholar] [CrossRef]
- Connolly, D.; McClowry, S.; Hayman, L.; Mahony, L.; Artman, M. Posttraumatic stress disorder in children after cardiac surgery. J. Pediatr. 2004, 144, 480–484. [Google Scholar] [CrossRef]
- McGarry, S. Pediatric Medical Traumatic Stress: The Impact on Children, Parents and Staff. Ph.D. Thesis, Edith Cowen University, Joondalup, Australia, 2013. [Google Scholar]
- Nelson, L.P.; Gold, J.I. Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: A review. Pediatr. Crit. Care Med. 2012, 13, 338–347. [Google Scholar] [CrossRef]
- Balluffi, A.; Kassam-Adams, N.; Kazak, A.; Tucker, M.; Dominguez, T.; Helfaer, M. Traumatic stress in parents of children admitted to the pediatric intensive care unit. Pediatr. Crit. Care Med. 2004, 5, 547–553. [Google Scholar] [CrossRef]
- Colville, G.A.; Tighe, H.; Pierce, C. Children’s factual and delusional memories of pediatrics intensive care. Crit. Care Med. 2006, 34, 20–23. [Google Scholar] [CrossRef]
- Brosbe, M.S.; Hoefling, K.; Faust, J. Predicting posttraumatic stress following pediatric injury: A systematic review. J. Pediatr. Psychol. 2011, 36, 718–729. [Google Scholar] [CrossRef] [Green Version]
- Daviss, W.B.; Mooney, D.; Racusin, R.; Ford, J.D.; Fleischer, A.; McHugo, G.J. Predicting posttraumatic stress after hospitalization for pediatric injury. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Brassell, A.A.; Rosenberg, E.; Parent, J.; Rough, J.N.; Fondacaro, K.; Seehuus, M. Parent’s psychological flexibility: Associations with parenting and child psychosocial well-being. J. Contextual Behav. Sci. 2016, 5, 111–120. [Google Scholar] [CrossRef]
- Fischer, T.D.; Smout, M.F.; Delfabbro, P.H. The relationship between psychological flexibility, early maladaptive schemas, perceived parenting and psychopathology. J. Contextual Behav. Sci. 2016, 5, 169–177. [Google Scholar] [CrossRef]
- Wallace, D.P.; McCracken, L.M.; Weiss, K.E.; Harbeck-Weber, C. The role of parent psychological flexibility in relation to adolescent chronic pain: Further instrument development. J. Pain 2015, 16, 235–246. [Google Scholar] [CrossRef]
- Gloster, A.T.; Meyer, A.H.; Lieb, R. Psychological flexibility as a malleable public health target: Evidence from a representative sample. J. Contextual Behav. Sci. 2017, 6, 166–171. [Google Scholar] [CrossRef] [Green Version]
- Flujas-Contreras, J.M.; Gómez, I. Improving flexible parenting with Acceptance and Commitment Therapy: A case study. J. Contextual Behav. Sci. 2018, 8, 29–35. [Google Scholar] [CrossRef]
- Gaudiano, B.A.; Schofield, C.A.; Davis, C.; Rifkin, L.S. Psychological inflexibility as a mediator of the relationship between depressive symptom severity and public stigma in depression. J. Contextual Behav. Sci. 2017, 6, 159–165. [Google Scholar] [CrossRef]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Masuda, A.; Anderson, P.L.; Wendell, J.W.; Chou, Y.Y.; Price, M.; Feinstein, A.B. Psychological flexibility mediates the relations between self-concealment and negative psychological outcomes. Personal. Individ. Differ. 2011, 50, 243–247. [Google Scholar] [CrossRef]
- Mendoza, H.; Tully, E.C.; Goodnight, B.; Gray, J.; Masuda, A. The indirect effect of self-concealment on distress through psychological inflexibility in Asian American, Black American, and White American college students. Personal. Individ. Differ. 2018, 126, 93–98. [Google Scholar] [CrossRef]
- Sairanen, E.; Lappalainen, P.; Hiltunen, A. Psychological inflexibility explains distress in parents whose children have chronic conditions. PLoS ONE 2018, 13, e0201155. [Google Scholar] [CrossRef] [PubMed]
- Kashdan, T.B.; Rottenberg, J. Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 2010, 30, 865–878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moyer, D.N.; Sandoz, E.K. The role of psychological flexibility in the relationship between parent and adolescent distress. J. Child Fam. Stud. 2015, 24, 1406–1418. [Google Scholar] [CrossRef]
- Williams, K.E.; Ciarrochi, J.; Heaven, P.C. Inflexible parents, inflexible kids: A 6-year longitudinal study of parenting style and the development of psychological flexibility in adolescents. J. Youth Adolesc. 2012, 41, 1053–1066. [Google Scholar] [CrossRef] [PubMed]
- Cheron, D.M.; Ehrenreich, J.T.; Pincus, D.B. Assessment of parental experiential avoidance in a clinical sample of children with anxiety disorders. Child Psychiatry Hum. Dev. 2009, 40, 383–403. [Google Scholar] [CrossRef]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef] [Green Version]
- Burke, K.; Moore, S. Development of the parental psychological flexibility questionnaire. Child Psychiatry Hum. Dev. 2015, 46, 548–557. [Google Scholar] [CrossRef]
- Steinberg, A.M.; Brymer, M.J.; Kim, S.; Briggs, E.C.; Ippen, C.G.; Ostrowski, S.A.; Pynoos, R.S. Psychometric properties of the UCLA PTSD reaction index: Part I. J. Trauma. Stress 2013, 26, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kaplow, J.B.; Rolon-Arroyo, B.; Layne, C.M.; Rooney, E.; Oosterhoff, B.; Hill, R.; Steinberg, A.M.; Lotterman, J.; Gallagher, K.A.; Pynoos, R.S. Validation of the UCLA PTSD reaction index for DSM-5: A developmentally informed assessment tool for youth. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 186–194. [Google Scholar] [CrossRef]
- Scheeringa, M.S. Young Child PTSD Checklist (YCPC); Tulane University: New Orleans, LA, USA, 2013; Available online: https://medicine.tulane.edu/departments/psychiatry/dr-scheeringas-lab/manuals-measures-trainings (accessed on 6 August 2021).
- Foa, E.B. The Posttraumatic Diagnostic Scale (PDS) Manual; National Computer Systems: Minneapolis, MN, USA, 1995. [Google Scholar]
- Foa, E.B.; McLean, C.P.; Zang, Y.; Zhong, J.; Powers, M.B.; Kauffman, B.Y.; Rauch, S.; Porter, K.; Knowles, K. Psychometric properties of the Posttraumatic Diagnostic Scale for DSM–5 (PDS–5). Psychol. Assess. 2016, 28, 1166. [Google Scholar] [CrossRef] [PubMed]
- Tuchner, M.; Meiner, Z.; Parush, S.; Hartman-Maeir, A. Health-related quality of life two years after injury due to terrorism. Isr. J. Psychiatry Relat. Sci. 2010, 47, 269–275. [Google Scholar] [PubMed]
- Arbuckle, J. AMOS 22 Users Guide; SmallWaters Corporation: Chicago, IL, USA, 2013. [Google Scholar]
- Cox, C.M.; Kenardy, J.A.; Hendrikz, J.K. A meta-analysis of risk factors that predict psychopathology following accidental trauma. J. Spec. Pediatr. Nurs. 2008, 13, 98–110. [Google Scholar] [CrossRef]
- Dindo, L.; Brandt, C.P.; Fiedorowicz, J. Cross-sectional relations between psychological inflexibility and symptoms of depression and anxiety among adults reporting migraines or risk factors for cardiovascular disease. J. Contextual Behav. Sci. 2019, 13, 1–6. [Google Scholar] [CrossRef]
- Wang, S.M.; Gaal, D.; Maranets, I.; Caldwell-Andrews, A.; Kain, Z.N. Acupressure and preoperative parental anxiety: A pilot study. Anesth. Analg. 2005, 101, 666–669. [Google Scholar] [CrossRef] [PubMed]
- Caldwell-Andrews, A.A.; Kain, Z.N.; Mayes, L.C.; Kerns, R.D.; Ng, D. Motivation and maternal presence during induction of anesthesia. Anesthesiology 2005, 103, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Kain, Z.N.; Mayes, L.C.; Caldwell-Andrews, A.A.; Karas, D.E.; McClain, B.C. Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics 2006, 118, 651–658. [Google Scholar] [CrossRef] [Green Version]
- Tabrizi, J.S.; Seyedhejazi, M.; Fakhari, A.; Ghadimi, F.; Hamidi, M.; Taghizadieh, N. Preoperative education and decreasing preoperative anxiety among children aged 8–10 years old and their mothers. Anesth. Pain Med. 2015, 5, e25036. [Google Scholar] [CrossRef] [Green Version]
- Perez-Gramaje, A.F.; Garcia, O.F.; Reyes, M.; Serra, E.; Garcia, F. Parenting styles and aggressive adolescents: Relationships with self-esteem and personal maladjustment. Eur. J. Psychol. Appl. Leg. Context 2020, 12, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Fuentes, M.C.; García, F.; Gracia, E.; Alarcón, A. Parental Socialization Styles and Psychological Adjustment. A Study in Spanish Adolescents//Los estilos parentales de socialización y el ajuste psicológico. Un estudio con adolescentes españoles. Rev. Psicodidáct. 2015, 20, 117–138. [Google Scholar] [CrossRef]
- Long, D.M.; Hayes, S.C. Development of an ACT prototype for therapeutic skill assessment. J. Contextual Behav. Sci. 2018, 9, 63–71. [Google Scholar] [CrossRef]
- Levin, M.E.; MacLane, C.; Daflos, S.; Seeley, J.R.; Hayes, S.C.; Biglan, A.; Pistorello, J. Examining psychological inflexibility as a transdiagnostic process across psychological disorders. J. Contextual Behav. Sci. 2014, 3, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Hayes, S.C.; Barnes-Holmes, D.; Wilson, K.G. Contextual behavioral science: Creating a science more adequate to the challenge of the human condition. J. Contextual Behav. Sci. 2012, 1, 1–16. [Google Scholar] [CrossRef]
| Variable | Mean | * SD | N | % |
|---|---|---|---|---|
| Gender (Males) | 94 | 61.8 | ||
| Age | 2.89 | 1.52 | ||
| Surgery complexity | ||||
| Low | 91 | 64.1 | ||
| Moderate | 46 | 32.4 | ||
| High | 5 | 3.5 | ||
| Hospitalization duration | 2.60 | 2.00 | ||
| Socio-Economic status | ||||
| Low | 34 | 22.2 | ||
| Moderate | 93 | 61.5 | ||
| High | 25 | 16.3 | ||
| Child’s mental difficulties | 1.21 | 0.25 | ||
| Parent’s mental difficulties | 0.47 | 0.58 |
| M | SD | YCPC | UCLA | AAQ | PPF | |
|---|---|---|---|---|---|---|
| YCPC (child PTSD measure) | 0.34 | 0.42 | - | |||
| UCLA (child PTSD measure) | 3.31 | 3.76 | 0.85 * | - | ||
| AAQ (parental flexibility measure) | 36.75 | 12.25 | −0.45 * | −0.61 * | - | |
| PPF (parental flexibility measure) | 105.60 | 30.78 | −0.37 * | −0.51 * | 0.75 * | - |
| PDS (parental PTSD measure) | 2.51 | 2.57 | 0.72 * | 0.75 * | −0.48 * | −0.44 * |
| Parent Flexibility Measure | Child PTSD Measure | B (SE) | 95% CI |
|---|---|---|---|
| AAQ | YCPC | 0.01 (0.00) | 0.01; 0.01 |
| AAQ | UCLA | 0.09 (0.02) | 0.05; 0.12 |
| PPF | YCPC | 0.00 (0.00) | 0.00; 0.01 |
| PPF | UCLA | 0.03 (0.01) | 0.02; 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ben-Ari, A.; Aloni, R.; Ben-David, S.; Benarroch, F.; Margalit, D. Parental Psychological Flexibility as a Mediating Factor of Post-Traumatic Stress Disorder in Children after Hospitalization or Surgery. Int. J. Environ. Res. Public Health 2021, 18, 11699. https://doi.org/10.3390/ijerph182111699
Ben-Ari A, Aloni R, Ben-David S, Benarroch F, Margalit D. Parental Psychological Flexibility as a Mediating Factor of Post-Traumatic Stress Disorder in Children after Hospitalization or Surgery. International Journal of Environmental Research and Public Health. 2021; 18(21):11699. https://doi.org/10.3390/ijerph182111699
Chicago/Turabian StyleBen-Ari, Amichai, Roy Aloni, Shiri Ben-David, Fortu Benarroch, and Daniella Margalit. 2021. "Parental Psychological Flexibility as a Mediating Factor of Post-Traumatic Stress Disorder in Children after Hospitalization or Surgery" International Journal of Environmental Research and Public Health 18, no. 21: 11699. https://doi.org/10.3390/ijerph182111699
APA StyleBen-Ari, A., Aloni, R., Ben-David, S., Benarroch, F., & Margalit, D. (2021). Parental Psychological Flexibility as a Mediating Factor of Post-Traumatic Stress Disorder in Children after Hospitalization or Surgery. International Journal of Environmental Research and Public Health, 18(21), 11699. https://doi.org/10.3390/ijerph182111699





