Effects of Oral Function Training and Oral Health Status on Physical Performance in Potentially Dependent Older Adults
Abstract
1. Introduction
2. Methods
2.1. Study Participants
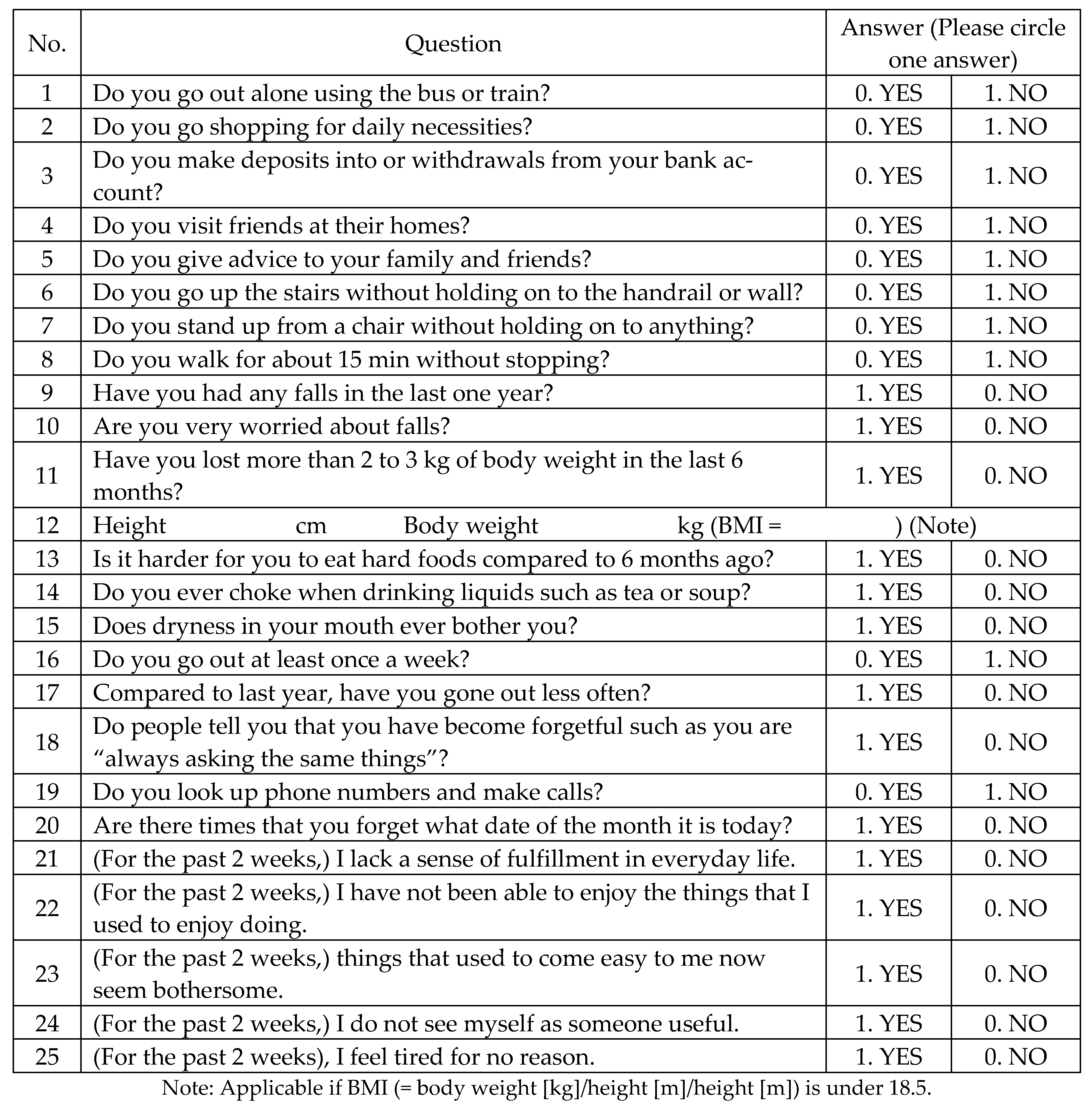
2.2. Survey Methods
2.3. Evaluation of Physical Function
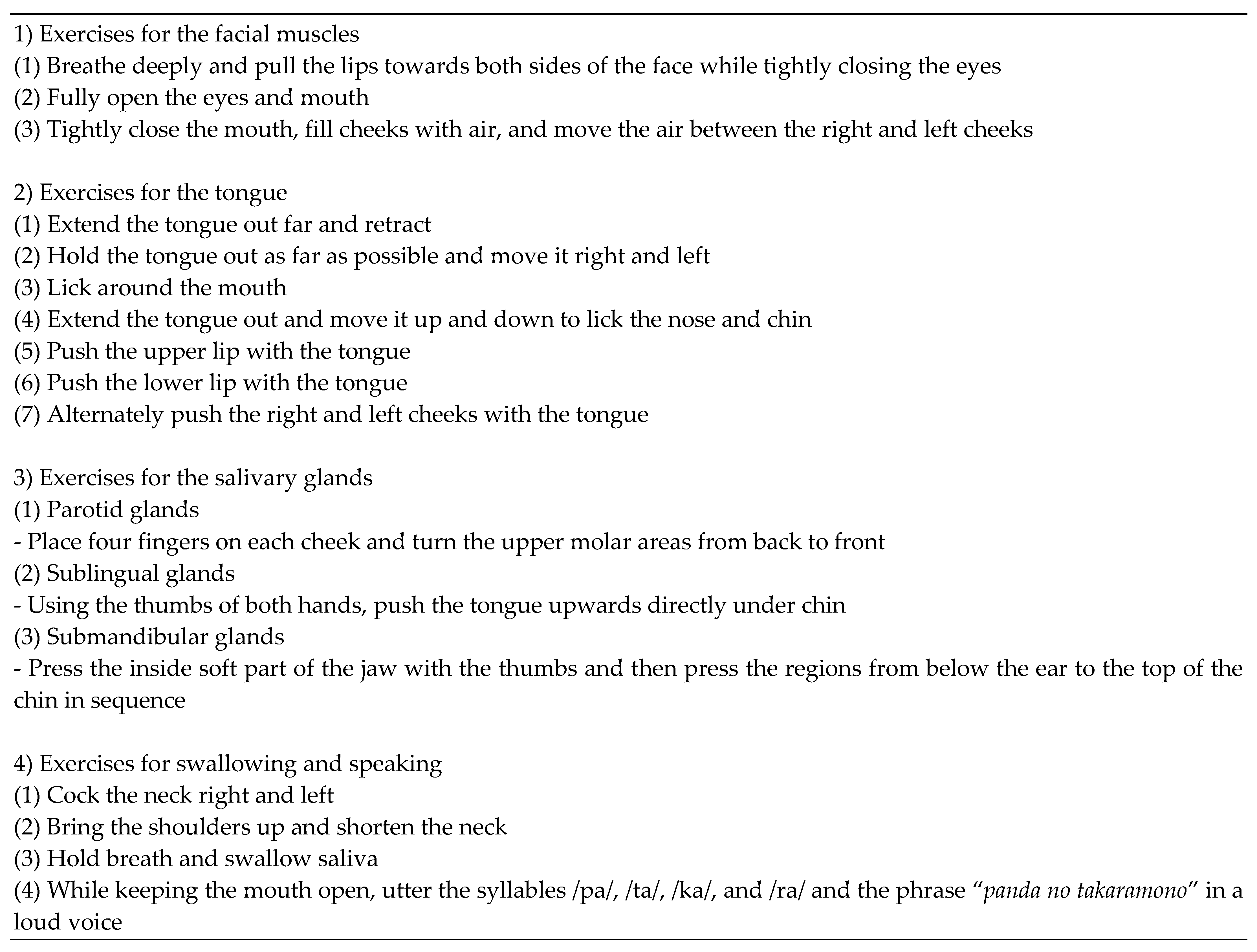
2.4. Oral Function Improvement Program
2.5. Evaluation of Oral Health Status
2.6. Characteristics of the Study Participants at Baseline
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Statistical Bureau of the Ministry of Internal Affairs and Communications. The Estimation of Japanese Population. 2014. Available online: http://www.stat.go.jp/data/jinsui/2014np/index.htm (accessed on 9 February 2016).
- Vermeulen, J.; Neyens, J.C.; van Rossum, E.; Spreeuwenberg, M.D.; de Witte, L.P. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: A systematic review. BMC Geriatr. 2011, 11, 33. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Labor and Welfare. Long-Term Care Prevention Manual for Japan. 2012. Available online: http://www.mhlw.go.jp/topics/2009/05/tp050-1.html (accessed on 9 February 2016).
- Wang, D.X.M.; Yao, J.; Zirek, Y.; Reijnierse, E.M.; Maier, A.B. Muscle mass, strength, and physical performance predicting activities of daily living: A meta-analysis. J. Cachexia Sarcopenia Muscle 2020, 11, 3–25. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, N.; Yamaga, T.; Yoshihara, A.; Nohno, K.; Yoshitake, Y.; Kimura, Y.; Shimada, M.; Nakagawa, N.; Nishimuta, M.; Ohashi, M.; et al. Influence of dental occlusion on physical fitness decline in a healthy Japanese elderly population. Arch. Gerontol. Geriatr. 2011, 52, 172–176. [Google Scholar] [CrossRef]
- Yamaga, T.; Yoshihara, A.; Ando, Y.; Yoshitake, Y.; Kimura, Y.; Shimada, M.; Nishimuta, M.; Miyazaki, H. Relationship between dental occlusion and physical fitness in an elderly population. J. Gerontol. Ser. A Biol. Sci. Med Sci. 2002, 57, M616–M620. [Google Scholar] [CrossRef] [PubMed]
- Izuno, H.; Hori, K.; Sawada, M.; Fukuda, M.; Hatayama, C.; Ito, K.; Nomura, Y.; Inoue, M. Physical fitness and oral function in community-dwelling older people: A pilot study. Gerodontology 2016, 33, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Sakayori, T.; Maki, Y.; Hirata, S.; Okada, M.; Ishii, T. Evaluation of a Japanese “Prevention of long-term care” project for the improvement in oral function in the high-risk elderly. Geriatr. Gerontol. Int. 2013, 13, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Ibayashi, H.; Fujino, Y.; Pham, T.M.; Matsuda, S. Intervention study of exercise program for oral function in healthy elderly people. Tohoku J. Exp. Med. 2008, 215, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Cohen, S.A.; Lofgren, I.E.; Greene, G.W.; Delmonico, M.J.; Greaney, M.L. Relationship between Diet Quality, Physical Activity and Health-Related Quality of Life in Older Adults: Findings from 2007–2014 National Health and Nutrition Examination Survey. J. Nutr. Health Aging 2018, 22, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Obuchi, S.; Arai, T.; Satake, K.; Takahira, N. The long-term effects of progressive resistance training on health-related quality in older adults. J. Physiol. Anthropol. 2008, 27, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Michikawa, T.; Nishiwaki, Y.; Takebayashi, T.; Toyama, Y. One-leg standing test for elderly populations. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2009, 14, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Mathias, S.; Nayak, U.S.; Isaacs, B. Balance in elderly patients: The “get-up and go” test. Arch. Phys. Med. Rehabil. 1986, 67, 387–389. [Google Scholar]
- Ito, K.; Yoshihara, A.; Tanano, N.; Ishigami., K.; Seida, Y.; Miyazaki, H. A comparison of methods for the measurement of oral diadochokinesis. Ronen Shika Igaku 2009, 24, 48–54. [Google Scholar]
- Hara, S.; Miura, H.; Yamazaki, K.; Sumi, Y. Association between activities of daily living and oral diadochokinesis among Japanese elderly individuals in a nursing home. Jpn. J. Gerodont. 2012, 49, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Hartelius, L.; Lillvik, M. Lip and tongue function differently affected in individuals with multiple sclerosis. Folia Phoniatr. Logop. Off. Organ Int. Assoc. Logop. Phoniatr. (IALP) 2003, 55, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Hamamoto, K.; Nakaue, K.; Ono, M.; Hanatani, S.; Hatakeda, A.; Kanzaki, W. A report on oral function assessment results in dental hygiene students—The relationship between oral diadochokinesis and repetitive saliva swallowing test-. Nihon Shikairyo Fukushi Gakkai Zassi 2018, 23, 14–20. [Google Scholar]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef] [PubMed]
- Haga, H.; Shibata, H.; Shichita, K.; Matsuzaki, T.; Hatano, S. Falls in the institutionalized elderly in Japan. Arch. Gerontol. Geriatr. 1986, 5, 1–9. [Google Scholar] [CrossRef]
- Miyahara, T.; Hagiya, N.; Ohyama, T.; Nakamura, Y. Modulation of human soleus H reflex in association with voluntary clenching of the teeth. J. Neurophysiol. 1996, 76, 2033–2041. [Google Scholar] [CrossRef]
- Taylor, A.; Appenteng, K.; Morimoto, T. Proprioceptive input from the jaw muscles and its influence on lapping, chewing, and posture. Can. J. Physiol. Pharmacol. 1981, 59, 636–644. [Google Scholar] [CrossRef]
- Bracco, P.; Deregibus, A.; Piscetta, R. Effects of different jaw relations on postural stability in human subjects. Neurosci. Lett. 2004, 356, 228–230. [Google Scholar] [CrossRef]
- Yamada, A.; Kanazawa, M.; Komagamine, Y.; Minakuchi, S. Association between tongue and lip functions and masticatory performance in young dentate adults. J. Oral Rehabil. 2015, 42, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Ballini, A.; Capodiferro, S.; Toia, M.; Cantore, S.; Favia, G.; De Frenza, G.; Grassi, F.R. Evidence-based dentistry: What’s new? Int. J. Med. Sci. 2007, 4, 174–178. [Google Scholar] [CrossRef] [PubMed][Green Version]

| Number of Participants (%), mean ± SD | |||
|---|---|---|---|
| Group | p-Value | ||
| Intervention Group | Control Group | ||
| n = 60 | n = 46 | ||
| Age (years) | |||
| ≥80 | 21 (35.0) | 14 (30.4) | 0.620 * |
| <80 | 39 (65.0) | 32 (69.6) | |
| Gender | |||
| Male | 12 (20.0) | 10 (21.7) | 0.827 * |
| Female | 48 (80.0) | 36 (78.3) | |
| Residential area | |||
| Yahiko village | 22 (36.7) | 24 (52.2) | 0.110 * |
| Sado city | 38 (63.3) | 22 (47.8) | |
| Dry mouth | 27 (45.0) | 30 (65.2) | 0.313 * |
| Choking | 26 (43.3) | 26 (56.5) | 0.661 * |
| Difficulty eating | 26 (43.3) | 21 (45.7) | 0.657 * |
| Remaining teeth | |||
| ≥20 | 29 (48.3) | 26 (56.5) | 0.403 * |
| <20 | 31 (51.7) | 20 (43.5) | |
| BMI | 23.9 ± 4.0 | 24.6 ± 3.6 | 0.353 ** |
| Measurements | Intervention Group | Control Group | ||
|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | |
| Physical fitness (s) | ||||
| OLST * | 16.5 (2.8/27.6) | 24.1 (9.1/36.2) a | 19.6 (4.0/22.0) | 20.6 (5.1/29.6) |
| TUG ** | 9.1 ± 1.7 | 8.0 ± 1.3 a | 9.5 ± 2.8 | 8.5 ± 2.6 a |
| Oral functional status (counts/s) | ||||
| OD (/pa/) ** | 6.1 ± 1.1 | 6.3 ± 0.8 a | 6.2 ± 0.7 | 6.2 ± 0.9 |
| OD (/ta/) ** | 6.0 ± 0.8 | 6.2 ± 0.6 a | 6.2 ± 0.6 | 6.2 ± 0.5 |
| OD (/ka/) ** | 5.7 ± 0.9 | 5.9 ± 0.7 a | 5.8 ± 0.9 | 6.0 ± 0.6 |
| Measurements | Rank 0 | Rank 1 | Rank 2 | Rank 3 |
|---|---|---|---|---|
| Physical fitness (s) | ||||
| OLST | 5.5–7.6 N = 27 | 7.7–8.7 N = 26 | 8.8–10.5 N = 28 | 10.5–17.4 N = 25 |
| TUG | 0–3.2 N = 27 | 3.3–8.2 N = 26 | 9.3–24.0 N = 27 | 27.0–105.2 N = 26 |
| Measurements | Group | OLST | p-Value | TUG | p-Value | ||
|---|---|---|---|---|---|---|---|
| Improvement (+) | Improvement (–) | Improvement (+) | Improvement (–) | ||||
| Oral health status (at the baseline) | |||||||
| Remaining teeth | High score | 14 (58.3) | 10 (41.7) | 0.046 | 14 (56.0) | 11 (44.0) | 0.103 |
| Low score | 9 (31.0) | 20 (69.0) | 11 (35.5) | 20 (64.5) | |||
| OD (/pa/) | High score | 9 (52.9) | 8 (47.1) | 0.252 | 7 (43.8) | 9 (56.3) | 0.586 |
| Low score | 14 (38.9) | 22 (61.1) | 18 (45.0) | 22 (55.0) | |||
| OD (/ta/) | High score | 7 (36.8) | 12 (63.2) | 0.569 | 6 (35.3) | 11 (64.7) | 0.263 |
| Low score | 16 (47.1) | 18 (52.9) | 19 (48.7) | 20 (51.3) | |||
| OD (/ka/) | High score | 9 (42.9) | 12 (57.1) | 0.588 | 10 (50.0) | 10 (50.0) | 0.374 |
| Low score | 14 (43.8) | 18 (56.3) | 15 (41.7) | 21 (58.3) | |||
| Oral function program | Intervention | 17 (54.8) | 14 (45.2) | 0.042 | 19 (59.4) | 13 (40.6) | 0.010 |
| Control | 6 (27.3) | 16 (72.7) | 6 (25.0) | 18 (75.0) | |||
| Independent Variables | Dependent Variables: OLST [1: Improvement (+)] | |||||
|---|---|---|---|---|---|---|
| Model 1: Intervention | Model 2: Remaining Teeth and OD | |||||
| OR | p-Value | 95% CI | OR | p-Value | 95% CI | |
| Gender | ||||||
| 1: Female | 1.12 | 0.881 | 0.26–4.80 | 1.49 | 0.656 | 0.26–8.52 |
| Age | ||||||
| 0.89 | 0.051 | 0.79–1.00 | 0.82 | 0.009 | 0.71–0.95 | |
| Model 1: | ||||||
| Intervention | ||||||
| Oral function training intervention | 4.31 | 0.027 | 1.18–15.69 | 6.48 | 0.023 | 1.29–32.47 |
| 1: Intervention (+) | ||||||
| Model 2: | ||||||
| Remaining teeth and OD | ||||||
| Remaining teeth | ||||||
| 1: ≥20 | 7.44 | 0.012 | 1.55–35.63 | |||
| Oral diadochokinesis (/pa/) | ||||||
| 1: High score | 8.75 | 0.028 | 1.27–60.24 | |||
| Oral diadochokinesis (/ta/) | ||||||
| 1: High score | 0.20 | 0.138 | 0.03–1.67 | |||
| Oral diadochokinesis (/ka/) | ||||||
| 1: High score | 0.89 | 0.90 | 0.15–5.43 | |||
| Number of participants | 53 | 53 | ||||
| Coefficient of determination (R2) | 0.114 | 0.277 | ||||
| Independent Variables | Dependent Variables: TUG [1: Improvement (+)] | |||||
| Model 1: Intervention | Model 2: Remaining Teeth and OD | |||||
| OR | p-Value | 95% CI | OR | p-Value | 95% CI | |
| Gender | ||||||
| 1: Female | 1.34 | 0.723 | 0.27–6.76 | 1.80 | 0.548 | 0.26–12.21 |
| Age | ||||||
| 0.79 | 0.001 | 0.68–0.91 | 0.70 | <0.001 | 0.58–0.86 | |
| Model 1: | ||||||
| Oral function training intervention | ||||||
| 1: Intervention (+) | 9.66 | 0.004 | 2.07–45.02 | 13.90 | 0.011 | 1.81–106.90 |
| Model 2: | ||||||
| Remaining teeth and OD | ||||||
| Remaining teeth | ||||||
| 1: ≥20 | 4.53 | 0.073 | 0.87–23.64 | |||
| Oral diadochokinesis (/pa/) | ||||||
| 1: High score | 8.13 | 0.044 | 1.06–62.37 | |||
| Oral diadochokinesis (/ta/) | ||||||
| 1: High score | 0.17 | 0.138 | 0.02–1.77 | |||
| Oral diadochokinesis (/ka/) | ||||||
| 1: High score | 2.55 | 0.404 | 0.28–22.91 | |||
| Number of participants | 53 | 53 | ||||
| Coefficient of determination (R2) | 0.300 | 0.415 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sasajima, M.; Yoshihara, A.; Odajima, A. Effects of Oral Function Training and Oral Health Status on Physical Performance in Potentially Dependent Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 11348. https://doi.org/10.3390/ijerph182111348
Sasajima M, Yoshihara A, Odajima A. Effects of Oral Function Training and Oral Health Status on Physical Performance in Potentially Dependent Older Adults. International Journal of Environmental Research and Public Health. 2021; 18(21):11348. https://doi.org/10.3390/ijerph182111348
Chicago/Turabian StyleSasajima, Masataka, Akihiro Yoshihara, and Ayuko Odajima. 2021. "Effects of Oral Function Training and Oral Health Status on Physical Performance in Potentially Dependent Older Adults" International Journal of Environmental Research and Public Health 18, no. 21: 11348. https://doi.org/10.3390/ijerph182111348
APA StyleSasajima, M., Yoshihara, A., & Odajima, A. (2021). Effects of Oral Function Training and Oral Health Status on Physical Performance in Potentially Dependent Older Adults. International Journal of Environmental Research and Public Health, 18(21), 11348. https://doi.org/10.3390/ijerph182111348





