Influence of Chronic Exposure to Exercise on Heart Rate Variability in Children and Adolescents Affected by Obesity: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
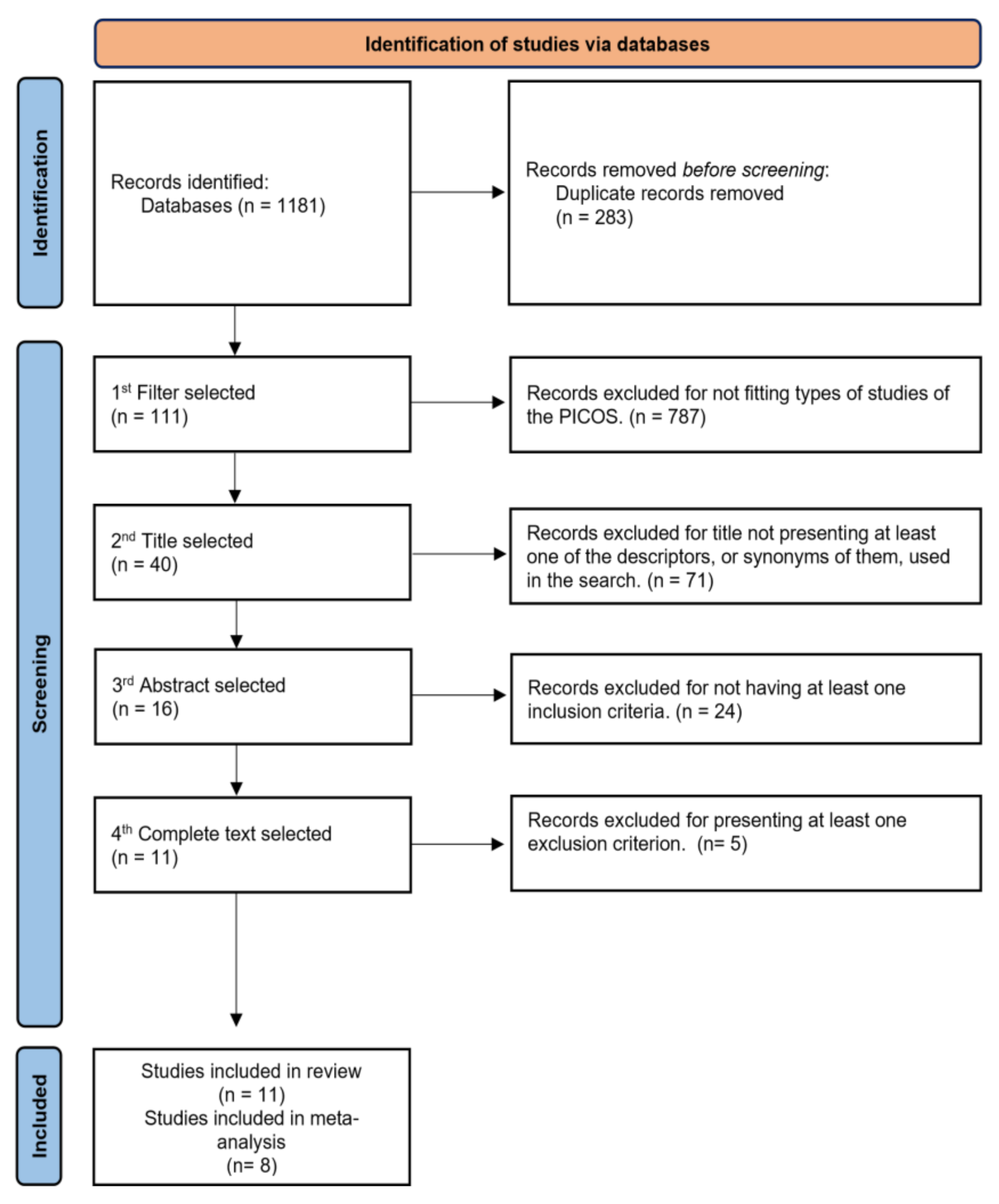
2. Materials and Methods
2.1. Research Strategy
2.2. Inclusion and Exclusion Criteria for Selection of Studies
2.3. Data Extraction
2.4. Parameters of Interest
2.5. Evaluation of Risk of Bias
2.6. Statistical Analyses
3. Results
3.1. Study Methods
3.2. Main Study Outcomes
3.3. Risk of Bias
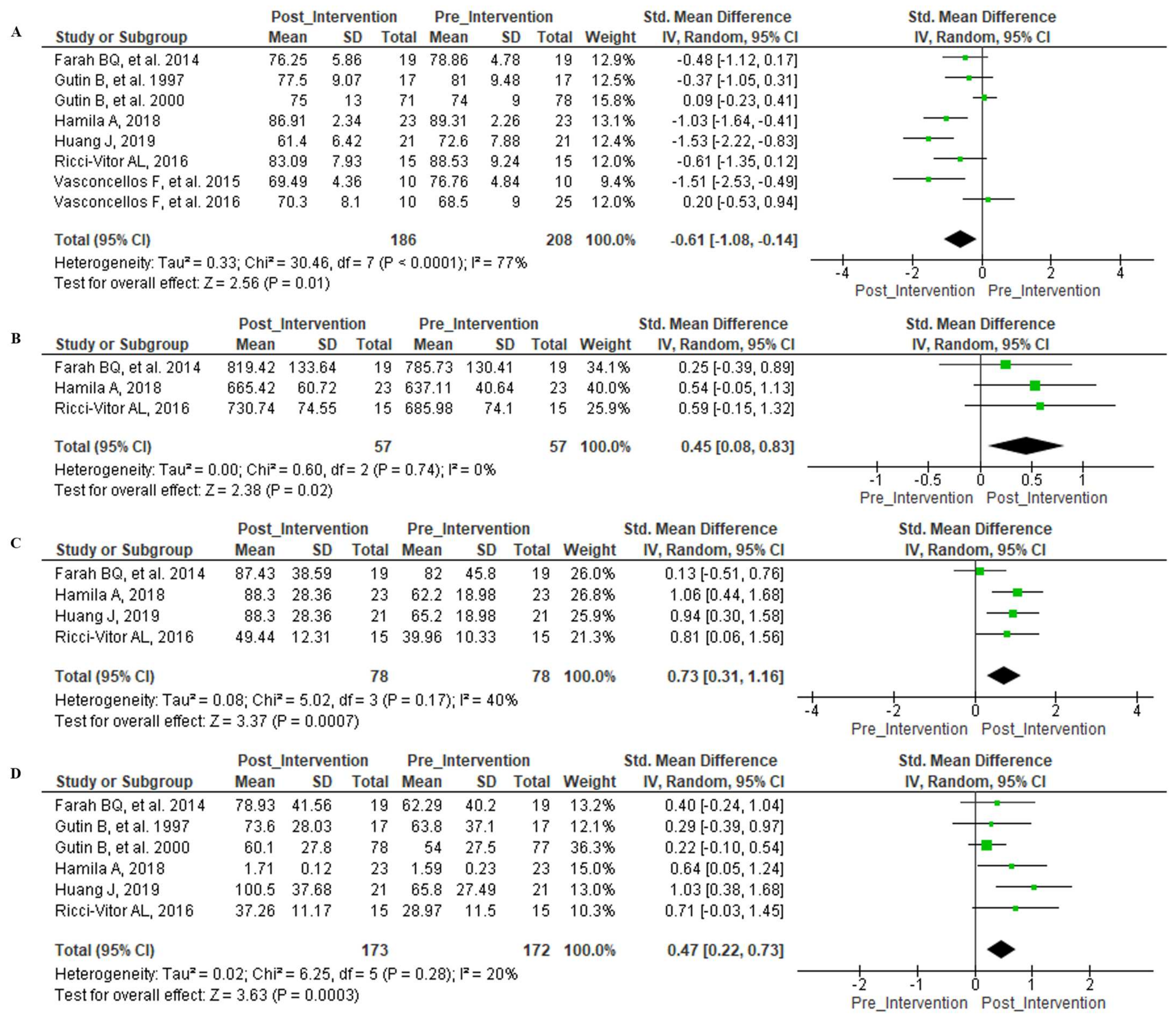
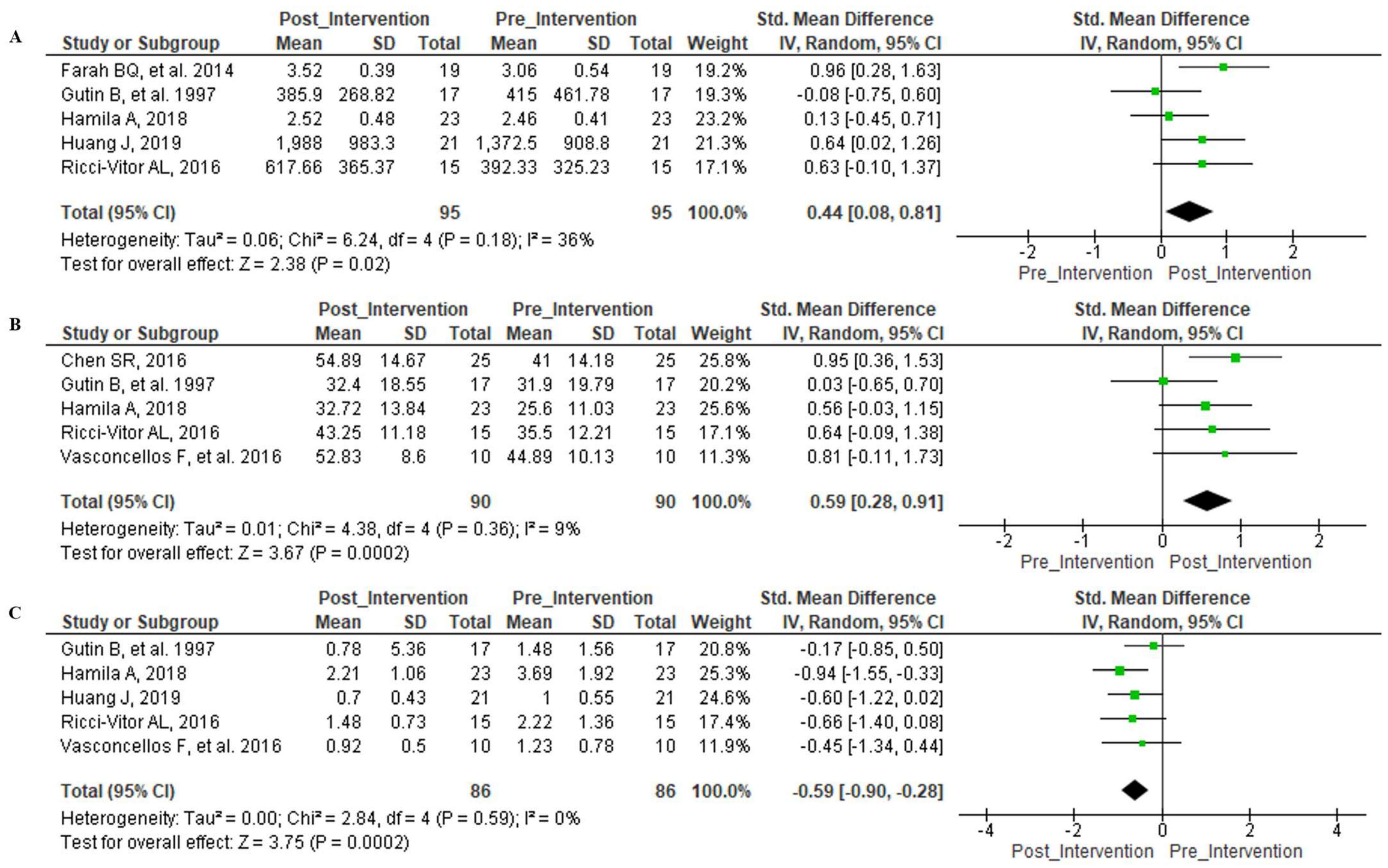
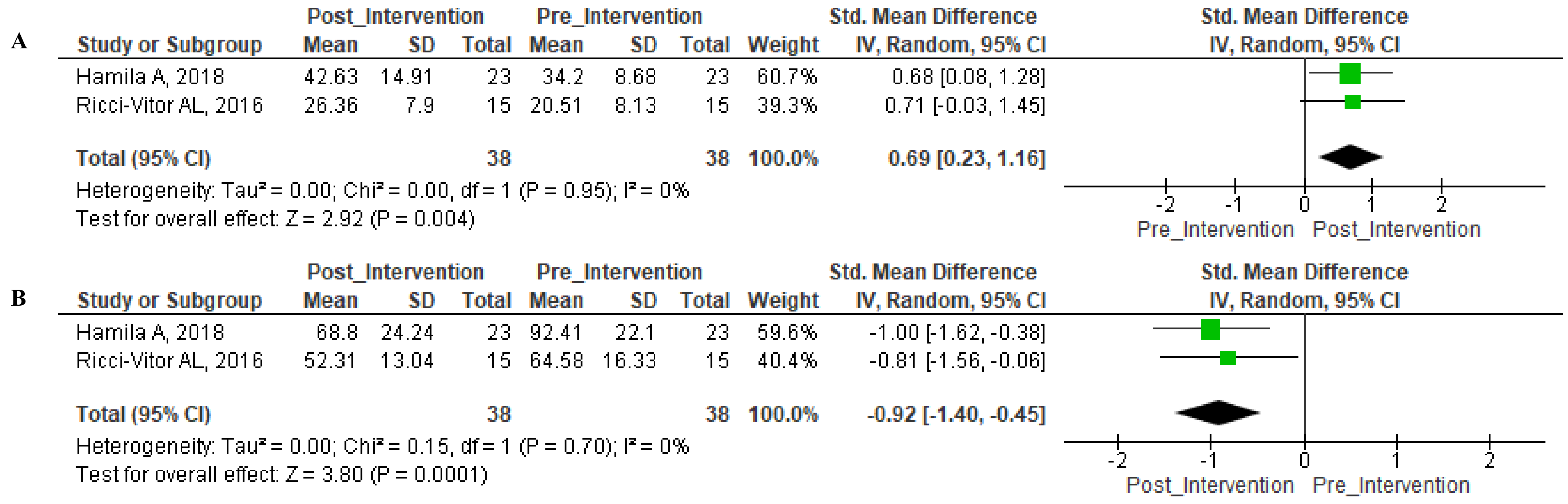
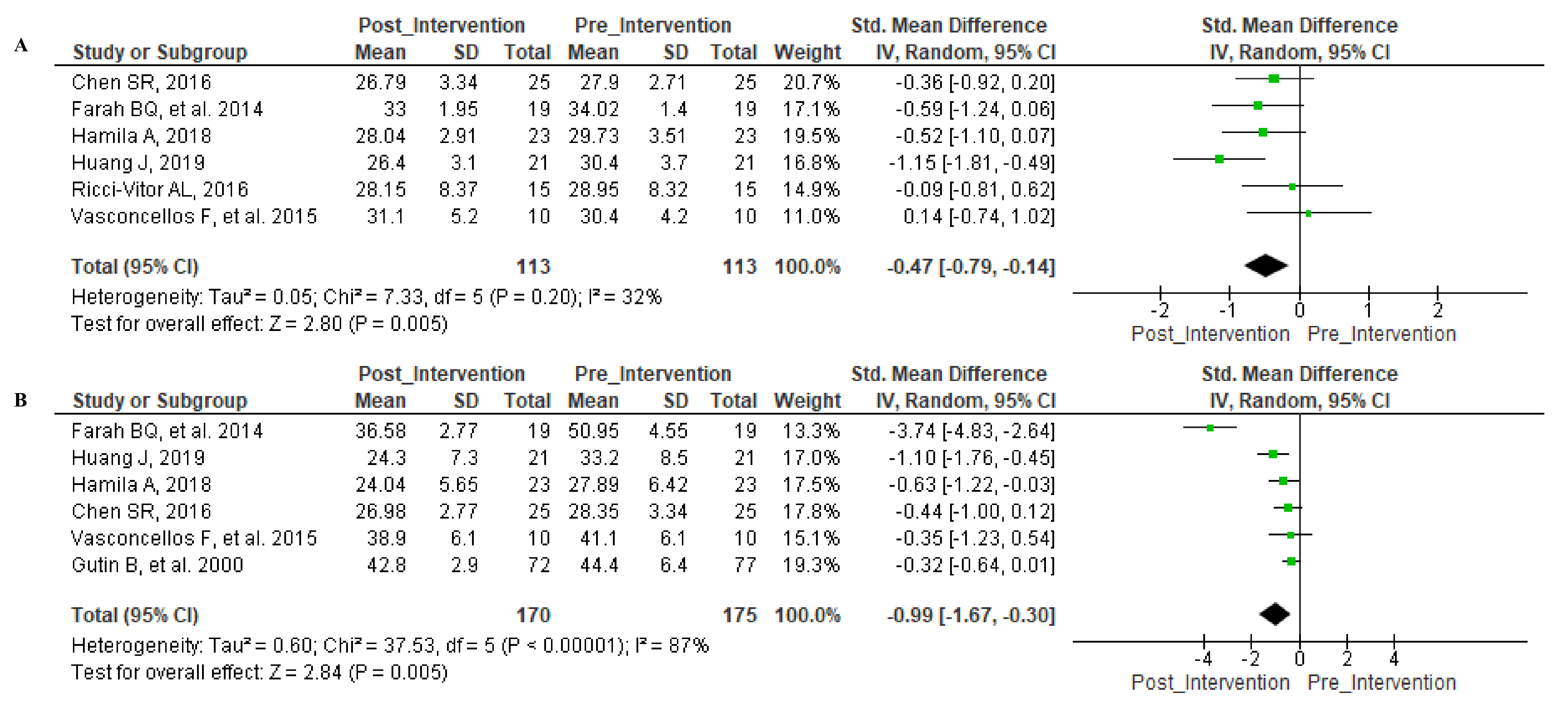
3.4. Meta-Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 14 July 2020).
- OPAS/OMS Brasil Obesidade Entre Crianças e Adolescentes Aumentou dez Vezes em Quatro Décadas, Revela Novo Estudo do Imperial College London e da OMS. Available online: https://www.paho.org/bra/index.php?option=com_content&view=article&id=5527:obesidade-entre-criancas-e-adolescentes-aumentou-dez-vezes-em-quatro-decadas-revela-novo-estudo-do-imperial-college-london-e-da-oms&Itemid=820 (accessed on 18 December 2019).
- Farah, B.Q.; Ritti-Dias, R.M.; Balagopal, P.; Hill, J.O.; Prado, W.L. Does Exercise Intensity Affect Blood Pressure and Heart Rate in Obese Adolescents? A 6-Month Multidisciplinary Randomized Intervention Study. Pediatr. Obes. 2014, 9, 111–120. [Google Scholar] [CrossRef]
- Calcaterra, V.; Palombo, C.; Malacarne, M.; Pagani, M.; Federico, G.; Kozakova, M.; Zuccotti, G.; Lucini, D. Interaction between Autonomic Regulation, Adiposity Indexes and Metabolic Profile in Children and Adolescents with Overweight and Obesity. Children 2021, 8, 686. [Google Scholar] [CrossRef]
- Chen, S.R.; Tseng, C.L.; Kuo, S.Y.; Chang, Y.K. Effects of a Physical Activity Intervention on Autonomic and Executive Functions in Obese Young Adolescents: A Randomized Controlled Trial. Health Psychol. 2016, 35, 1120–1125. [Google Scholar] [CrossRef]
- Hamila, A.; Younes, M.; Cottin, F.; Ben Amor, Y.; Shephard, R.; Tabka, Z.; Bouhlel, E. Effects of Walking Exercises on Body Composition, Heart Rate Variability, and Perceptual Responses in Overweight and Obese Adolescents. Sci. Sports 2018, 33, e191–e202. [Google Scholar] [CrossRef]
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric Obesity-Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef]
- Tran, B.X.; Nghiem, S.; Afoakwah, C.; Latkin, C.A.; Ha, G.H.; Nguyen, T.P.; Doan, L.P.; Pham, H.Q.; Ho, C.S.H.; Ho, R.C.M. Characterizing Obesity Interventions and Treatment for Children and Youths during 1991–2018. Int. J. Environ. Res. Public Health 2019, 16, 4227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Katzmarzyk, P.T.; Denstel, K.D.; Beals, K.; Bolling, C.; Wright, C.; Crouter, S.E.; McKenzie, T.L.; Pate, R.R.; Saelens, B.E.; Staiano, A.E.; et al. Results from the United States of America’s 2016 Report Card on Physical Activity for Children and Youth. J. Phys. Act. Health 2016, 13, S307–S313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Alkandari, J.R.; Andersen, L.B.; Bauman, A.E.; Brownson, R.C.; et al. Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- González-Ruiz, K.; Ramírez-Vélez, R.; Correa-Bautista, J.E.; Peterson, M.D.; García-Hermoso, A. The Effects of Exercise on Abdominal Fat and Liver Enzymes in Pediatric Obesity: A Systematic Review and Meta-Analysis. Child. Obes. 2017, 13, 272–282. [Google Scholar] [CrossRef]
- Kingsley, J.D.; Figueroa, A. Acute and Training Effects of Resistance Exercise on Heart Rate Variability. Clin. Physiol. Funct. Imaging 2016, 36, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Moraes, Í.A.P.; Silva, T.; Massetti, T.; Menezes, L.; Ribeiro, V.; Tropiano, L.; Barnabé, V.; Hoshi, R.; Monteiro, C.; Fernandes, M. Fractal Correlations and Linear Analyses of Heart Rate Variability in Healthy Young People with Different Levels of Physical Activity. Cardiol. Young 2019, 29, 1236–1242. [Google Scholar] [CrossRef] [PubMed]
- Marasingha-Arachchige, S.; Rubio-Arias, J.; Alcaraz, P.; Chung, L. Factors That Affect Heart Rate Variability Following Acute Resistance Exercise: A Systematic Review and Meta-Analysis. J. Sport Health Sci. 2020. [Google Scholar] [CrossRef] [PubMed]
- Turri-Silva, N.; Ricci-Vitor, A.L.; Cipriano, G.; Garner, D.; Netto, J.; Giacon, T.; Destro Christofaro, D.G.; Marques Vanderlei, L.C. Functional Resistance Training Superiority over Conventional Training in Metabolic Syndrome: A Randomized Clinical Trial. Res. Q. Exerc. Sport 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Farah, B.; Andrade-Lima, A.; Germano-Soares, A.; Christofaro, D.; de Barros, M.; do Prado, W.; Ritti-Dias, R. Physical Activity and Heart Rate Variability in Adolescents with Abdominal Obesity. Pediatr. Cardiol. 2018, 39, 466–472. [Google Scholar] [CrossRef] [Green Version]
- Farinatti, P.; Neto, S.R.M.; Dias, I.; Cunha, F.A.; Bouskela, E.; Kraemer-Aguiar, L.G. Short-Term Resistance Training Attenuates Cardiac Autonomic Dysfunction in Obese Adolescents. Pediatr. Exerc. Sci. 2016, 28, 374–380. [Google Scholar] [CrossRef]
- Vanderlei, L.; Pastre, C.; Hoshi, R.; Carvalho, T.; Godoy, M. Noções Básicas de Variabilidade Da Frequência Cardíaca e Sua Aplicabilidade Clínica. Rev. Bras. Cir. Cardiovasc. 2009, 24, 205–217. [Google Scholar] [CrossRef] [Green Version]
- Ernst, G. Heart-Rate Variability—More than Heart Beats? Front. Public Health 2017, 5, 240. [Google Scholar] [CrossRef]
- Akselrod, S.; Gordon, D.; Ubel, F.A.; Shannon, D.C.; Barger, A.C.; Cohen, R.J. Power Spectrum Analysis of Heart Rate Fluctuation: A Quantitative Probe of Beat-to-Beat Cardiovascular Control. Science 1981, 213, 220–222. [Google Scholar] [CrossRef]
- Huang, J.; Lai, Q.; Wang, D.; Yin, H.; Liao, J.; Wang, S.; Xu, F.; Hou, X.; Hu, M. Effects of Exercise Training with Dietary Restriction on Arterial Stiffness, Central Hemodynamic Parameters and Cardiac Autonomic Function in Obese Adolescents. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 2157–2163. [Google Scholar] [CrossRef] [Green Version]
- Van Biljon, A.; McKune, A.J.; Dubose, K.D.; Kolanisi, U.; Semple, S.J. Short-Term High-Intensity Interval Training Is Superior to Moderate-Intensity Continuous Training in Improving Cardiac Autonomic Function in Children. Cardiology 2018, 141, 1–8. [Google Scholar] [CrossRef]
- Oliveira, R.S.; Barker, A.R.; Wilkinson, K.M.; Abbott, R.A.; Williams, C.A. Is Cardiac Autonomic Function Associated with Cardiorespiratory Fitness and Physical Activity in Children and Adolescents? A Systematic Review of Cross-Sectional Studies. Int. J. Cardiol. 2017, 236, 113–122. [Google Scholar] [CrossRef] [Green Version]
- Farrell, C.; Turgeon, D.R. Normal versus Chronic Adaptations to Aerobic Exercise; StatPearls: Treasure Island, FL, USA, 2021. [Google Scholar]
- Beller, E.M.; Glasziou, P.P.; Altman, D.G.; Hopewell, S.; Bastian, H.; Chalmers, I.; Gøtzsche, P.C.; Lasserson, T.; Tovey, D. PRISMA for Abstracts: Reporting Systematic Reviews in Journal and Conference Abstracts. PLoS Med. 2013, 10, e1001419. [Google Scholar] [CrossRef] [Green Version]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Altman, D.G.; Booth, A.; et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (Prisma-p) 2015: Elaboration and Explanation. BMJ 2015, 349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Estarli, M.; Barrera, E.S.A.; et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Rev. Esp. Nutr. Hum. Diet. 2016, 20, 148–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Welch, V.; Petticrew, M.; Tugwell, P.; Moher, D.; O’Neill, J.; Waters, E.; White, H.; Atun, R.; Awasthi, S.; Barbour, V.; et al. PRISMA-Equity 2012 Extension: Reporting Guidelines for Systematic Reviews with a Focus on Health Equity. PLoS Med. 2012, 9, e1001333. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Stewart, L.A.; Clarke, M.; Rovers, M.; Riley, R.D.; Simmonds, M.; Stewart, G.; Tierney, J.F. Preferred Reporting Items for a Systematic Review and Meta-Analysis of Individual Participant Data: The PRISMA-IPD Statement. JAMA 2015, 313, 1657–1665. [Google Scholar] [CrossRef]
- Zorzela, L.; Loke, Y.K.; Ioannidis, J.P.; Golder, S.; Santaguida, P.; Altman, D.G.; Moher, D.; Vohra, S.; Boon, H.; Clark, J.; et al. PRISMA Harms Checklist: Improving Harms Reporting in Systematic Reviews. BMJ 2016, 352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saaiq, M.; Ashraf, B. Modifying “Pico” Question into “Picos” Model for More Robust and Reproducible Presentation of the Methodology Employed in A Scientific Study. World J. Plast. Surg. 2017, 6, 390–392. [Google Scholar] [PubMed]
- BMI-for-Age (5–19 Years). Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (accessed on 9 September 2021).
- Must, A.; Dallal, G.; Dietz, W. Reference Data for Obesity: 85th and 95th Percentiles of Body Mass Index (Wt/Ht2) and Triceps Skinfold Thickness. Am. J. Clin. Nutr. 1991, 53, 839–846. [Google Scholar] [CrossRef]
- WebPlotDigitizer—Copyright 2010–2020 Ankit Rohatgi. Available online: https://apps.automeris.io/wpd/ (accessed on 22 July 2021).
- Physiotherapy Evidence Database. Available online: https://www.pedro.org.au/ (accessed on 12 December 2019).
- PEDro Scale. Available online: https://www.pedro.org.au/english/downloads/pedro-scale/ (accessed on 12 December 2019). (In English).
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2021. [Google Scholar]
- McGrath, S.; Zhao, X.F.; Steele, R.; Thombs, B.D.; Benedetti, A.; Levis, B.; Riehm, K.E.; Saadat, N.; Levis, A.W.; Azar, M.; et al. Estimating the Sample Mean and Standard Deviation from Commonly Reported Quantiles in Meta-Analysis. Stat. Methods Med. Res. 2020, 29, 2520–2537. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Li, T.; Deeks, J.J. Choosing effect measures and computing estimates of effect. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019; pp. 143–176. [Google Scholar]
- Gutin, B.; Owens, S.; Slavens, G.; Riggs, S.; Treiber, F. Effect of Physical Training on Heart-Period Variability in Obese Children. J. Pediatr. 1997, 130, 938–943. [Google Scholar] [CrossRef]
- Gutin, B.; Barbeau, P.; Litaker, M.S.; Ferguson, M.; Owens, S. Heart Rate Variability in Obese Children: Relations to Total Body and Visceral Adiposity, and Changes with Physical Training and Detraining. Obes. Res. 2000, 8, 12–19. [Google Scholar] [CrossRef] [Green Version]
- Paschoal, M.; Neves, F.; Donato, B. Heart Rate and Cardiac Autonomic Modulation of Obese Pre-Adolescent before, Durin and Short Aerobic Training Program. Rev. Ciênc. Méd 2018, 27, 125–133. [Google Scholar] [CrossRef]
- Ricci-Vitor, A.L.; Rossi, F.E.; Hirai, P.M.; Da Silva, N.T.; Vanderlei, F.M.; Haddad, M.I.; Gonzaga, L.A.; Pastre, C.M.; Valenti, V.E.; Freitas, I.F.; et al. Effects of a Multidisciplinary Program on Autonomic Modulation in Overweight or Obese Children and Adolescents. J. Hum. Growth Dev. 2016, 26, 154–161. [Google Scholar] [CrossRef] [Green Version]
- Vasconcellos, F.; Seabra, A.; Cunha, F.; Montenegro, R.; Penha, J.; Bouskela, E.; Nogueira Neto, J.F.; Collett-Solberg, P.; Farinatti, P. Health Markers in Obese Adolescents Improved by a 12-Week Recreational Soccer Program: A Randomised Controlled Trial. J. Sports Sci. 2016, 34, 564–575. [Google Scholar] [CrossRef]
- Vasconcellos, F.; Seabra, A.; Montenegro, R.; Cunha, F.; Bouskela, E.; Farinatti, P. Can Heart Rate Variability Be Used to Estimate Gas Exchange Threshold in Obese Adolescents? Int. J. Sports Med. 2015, 36, 654–660. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- García Bermejo, P.; de la Cruz Torres, B.; Naranjo Orellana, J.; Albornoz Cabello, M. Autonomic Activity in Women during Percutaneous Needle Electrolysis. Eur. J. Integr. Med. 2017, 11, 53–58. [Google Scholar] [CrossRef]
- Windham, B.G.; Fumagalli, S.; Ble, A.; Sollers, J.J.; Thayer, J.F.; Najjar, S.S.; Griswold, M.E.; Ferrucci, L. The Relationship between Heart Rate Variability and Adiposity Differs for Central and Overall Adiposity. J. Obes. 2012, 2012. [Google Scholar] [CrossRef]
- Plaza-Florido, A.; Migueles, J.H.; Mora-Gonzalez, J.; Molina-Garcia, P.; Rodriguez-Ayllon, M.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Navarrete, S.; Lozano, R.M.; Michels, N.; et al. The Role of Heart Rate on the Associations between Body Composition and Heart Rate Variability in Children with Overweight/Obesity: The Active Brains Project. Front. Physiol. 2019, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.A.; Park, Y.G.; Cho, K.H.; Hong, M.H.; Han, H.C.; Choi, Y.S.; Yoon, D. Heart Rate Variability and Obesity Indices: Emphasis on the Response to Noise and Standing. J. Am. Board Fam. Pract. 2005, 18, 97–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mouridsen, M.R.; Bendsen, N.T.; Astrup, A.; Haugaard, S.B.; Binici, Z.; Sajadieh, A. Modest Weight Loss in Moderately Overweight Postmenopausal Women Improves Heart Rate Variability. Eur. J. Prev. Cardiol. 2013, 20, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Adachi, T.; Sert-Kuniyoshi, F.H.; Calvin, A.D.; Singh, P.; Romero-Corral, A.; Van Der Walt, C.; Davison, D.E.; Bukartyk, J.; Konecny, T.; Pusalavidyasagar, S.; et al. Effect of Weight Gain on Cardiac Autonomic Control during Wakefulness and Sleep. Hypertension 2011, 57, 723–730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veijalainen, A.; Haapala, E.A.; Väistö, J.; Leppänen, M.H.; Lintu, N.; Tompuri, T.; Seppälä, S.; Ekelund, U.; Tarvainen, M.P.; Westgate, K.; et al. Associations of Physical Activity, Sedentary Time, and Cardiorespiratory Fitness with Heart Rate Variability in 6- to 9-Year-Old Children: The PANIC Study. Eur. J. Appl. Physiol. 2019, 119, 2487–2498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristics of the Samples | ||||||
| Author | N | Age (Years) | Sex (Males) | BMI (kg/m2) | SD | PEDro Score |
| Chen S. R. et al., 2016 [5] | 50 | ±12 | 28 | Control: 27.9 ± 2.71 | RCT | 05/10 |
| Experimental: 26.79 ± 3.34 | ||||||
| Farah B. Q. et al., 2014 [3] | 43 | 13–18 | 14 | Controls: HIT = 33.5 ± 1.4; LIT = 34.5 ± 1.3 | RCT | 05/10 |
| Experimental: HIT = 32 ± 1.8; LIT = 33.9 ± 1.7 | ||||||
| Farinatti P. et al., 2016 [17] | 44 | 13–17 | 20 | Control: 20.6 ± 2.4 | CT | 04/10 |
| Experimental: 32.1 ± 3.6 | ||||||
| Gutin B. et al., 1997 [41] | 35 | 7–11 | 12 | Control: 28.8 ± 1.6 | RCT | 05/10 |
| Experimental: 31.4 ± 1.8 | ||||||
| Gutin B. et al., 2000 [42] | 79 | ±10 | 26 | - | RCT | 03/10 |
| Hamila A. et al., 2018 [6] | 31 | ±14 | 12 | - | RCT | 04/10 |
| Huang J. et al., 2019 [21] | 21 | 5–16 | 11 | Control: 30.4 ± 3.7 | CT | 04/10 |
| Experimental: 26.4 ± 3.1 | ||||||
| Paschoal M. A. et al., 2018 [43] | 15 | 9–12 | - | Baseline: 23.20 ± 1.3 | CT | 03/10 |
| Ricci-Vitor A. L. et al., 2016 [44] | 15 | 10.93 ± 2.28 | 7 | Control: 28.95 ± 8.32 | CT | 04/10 |
| Experimental: 28.15 ± 8.37 | ||||||
| Vasconcellos F. et al., 2015 [46] | 35 | ±14 | 26 | - | RCT | 05/10 |
| Vasconcellos F. et al., 2016 [45] | 30 | 12–2017 | 20 | Control: 32.2 ± 4.9 | RCT | 05/10 |
| Experimental: 31.1 ± 5.2 | ||||||
| Methods of Included Studies | ||||||
| Author | Intervention Time | Exercise Type | Control Group | Graduation Method of Exercise Intensity | Main Instrument of HRV | |
| Chen S. R. et al., 2016 [5] | 12 wk | Aerobic | No exercise | % HR max | CheckMyHeart 3.0, DailyCareBioMedical, Inc., Taoyuan, Taiwan | |
| Farah B. Q. et al., 2014 [3] | 24 wk | Aerobic | - | Metabolic equivalent of task (MET) and VO2Max | Polar model RS800CX, Polar Electro Inc., Lake Success, New York, NY, USA | |
| Farinatti P. et al., 2016 [17] | 30–40 min/3 d/12 wk | Resistance training | Normal weight | % Maximum Repetition | Finometer, Finapres Medical Systems, Amsterdam, The Netherlands | |
| Gutin B. et al., 1997 [41] | 40 min/5 d/16 wk | Aerobic | No exercise | % HR Submax | Polar Vantage, Port Washington, New York, NY, USA | |
| Gutin B. et al., 2000 [42] | 40 min/5 d/16 wk | Aerobic | - | HR | Polar Vantage, Port Washington, New York, NY, USA | |
| Hamila A. et al., 2018 [8] | 60 min/3 d/8 wk | Aerobic | No exercise | Maximal aerobic speed | Polar RS810, Kempele, Finland | |
| Huang J. et al., 2019 [21] | 5 h/6 d/6 wk | Aerobic | - | % HR max | Sphygmo Corsystem, AtCor Medical, Sydney, Australia | |
| Paschoal M. A. et al., 2018 [40] | 12 sessions/40 min | Aerobic | - | % HR Submax | Polar S810®, Kempele, Finland | |
| Ricci-Vitor A. L. et al., 2016 [44] | 60 min/3 d/12 wk | Aerobic | - | Not graduated | Polar Electro, model S810i, Kempele, Finland | |
| Vasconcellos F. et al., 2015 [46] | 60 min/3 d/12 wk | Sport | No exercise/Normal weight | HRV | Polar RS800cx, PolarTM, Kempele, Finland | |
| Vasconcellos F. et al., 2016 [45] | 60 min/3 d/12 wk | Sport | No exercise/Normal weight | Not graduated | Polar RS800cx, PolarTM, Kempele, Finland | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dias, R.M.; Moraes, Í.A.P.; Dantas, M.T.A.P.; Fernani, D.C.G.L.; Fontes, A.M.G.G.; Silveira, A.C.; Barnabé, V.; Fernandes, M.; Martinelli, P.M.; Monteiro, C.B.M.; et al. Influence of Chronic Exposure to Exercise on Heart Rate Variability in Children and Adolescents Affected by Obesity: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 11065. https://doi.org/10.3390/ijerph182111065
Dias RM, Moraes ÍAP, Dantas MTAP, Fernani DCGL, Fontes AMGG, Silveira AC, Barnabé V, Fernandes M, Martinelli PM, Monteiro CBM, et al. Influence of Chronic Exposure to Exercise on Heart Rate Variability in Children and Adolescents Affected by Obesity: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(21):11065. https://doi.org/10.3390/ijerph182111065
Chicago/Turabian StyleDias, Rodrigo M., Íbis A. P. Moraes, Maria T. A. P. Dantas, Deborah C. G. L. Fernani, Anne M. G. G. Fontes, Ana C. Silveira, Viviani Barnabé, Marcelo Fernandes, Patrícia M. Martinelli, Carlos B. M. Monteiro, and et al. 2021. "Influence of Chronic Exposure to Exercise on Heart Rate Variability in Children and Adolescents Affected by Obesity: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 21: 11065. https://doi.org/10.3390/ijerph182111065
APA StyleDias, R. M., Moraes, Í. A. P., Dantas, M. T. A. P., Fernani, D. C. G. L., Fontes, A. M. G. G., Silveira, A. C., Barnabé, V., Fernandes, M., Martinelli, P. M., Monteiro, C. B. M., Garner, D. M., Abreu, L. C., & Silva, T. D. (2021). Influence of Chronic Exposure to Exercise on Heart Rate Variability in Children and Adolescents Affected by Obesity: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(21), 11065. https://doi.org/10.3390/ijerph182111065







