Prevalence of Locomotive Organ Impairment and Associated Factors among Middle-Aged and Older People in Nan Province, Thailand
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Study Site, Target Population
2.2. Data Collection
2.3. Sampling Method
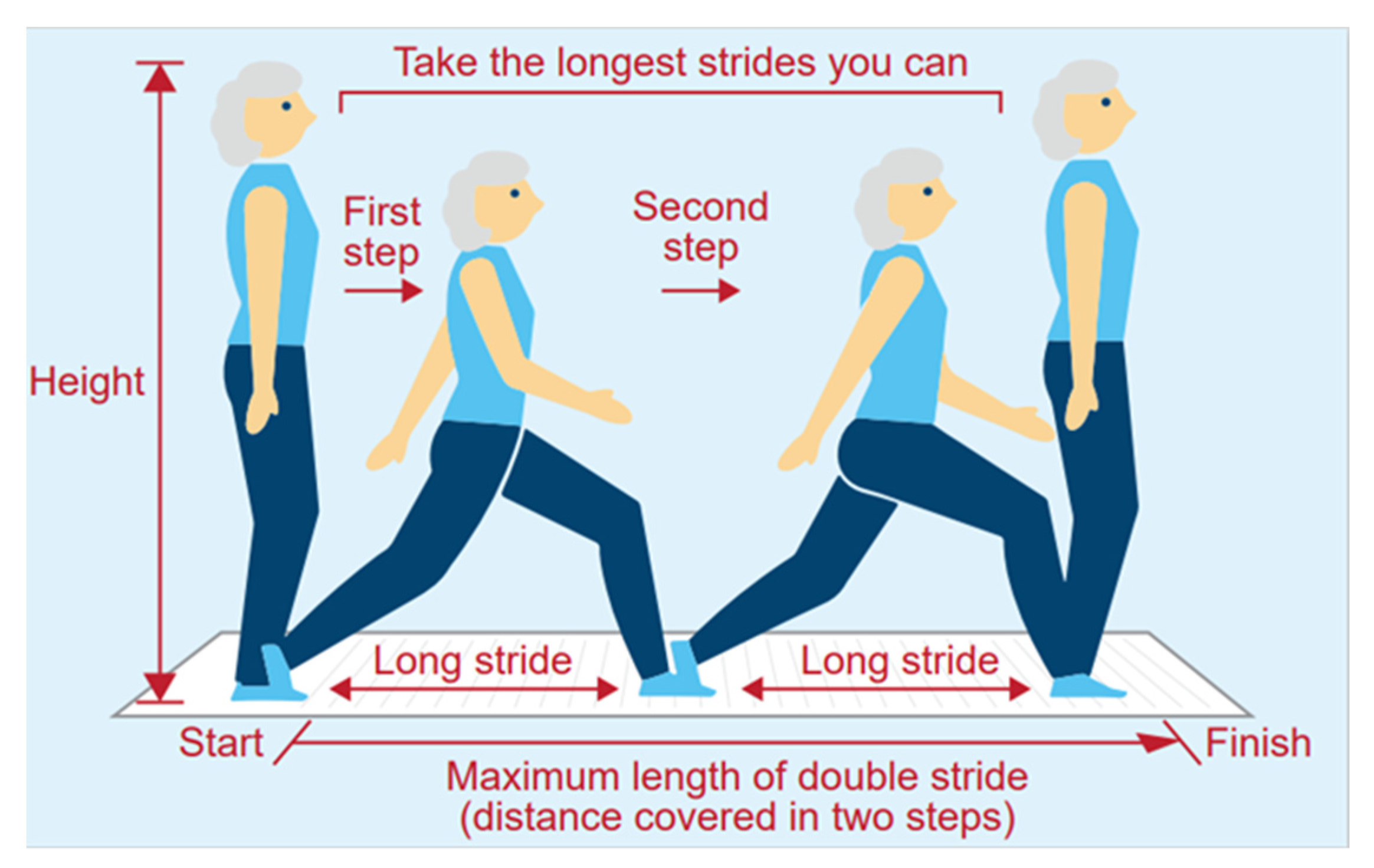
2.4. The Two-Step Test
2.5. Questionnaire Survey
2.6. Statistical Analyses
3. Results
3.1. Characteristics of the Participants
3.2. Factors Associated with a Low Two-Step Score
3.3. Determinants That Exacerbate the Low Two-Step Score
4. Discussion
4.1. Prevalence of Locomotive Organ Impairment
4.2. Locomotive Organ Impairment and Associated Factors
4.3. Physical Activities and Locomotive Organ Impairment
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. World Population Prospects 2019. Demographic Profiles, Volume II. Available online: https://population.un.org/wpp/Publications/Files/WPP2019_Volume-II-Demographic-Profiles.pdf (accessed on 23 December 2019).
- World Health Organization. Aging Health. Available online: https://www.who.int/en/news-room/fact-sheets/detail/ageing-and-health (accessed on 25 February 2021).
- Nakamura, K. A ‘Super-aged’ society and the “locomotive syndrome”. J. Orthop. Sci. 2008, 13, 1–2; [Google Scholar] [CrossRef]
- Williamson, S.; Landeiro, F.; McConnell, T.; Fulford-Smith, L.; Javaid, M.; Judge, A.; Leal, J. Costs of fragility hip fractures globally: A systematic review and meta-regression analysis. Osteoporos. Int. 2017, 28, 2791–2800. [Google Scholar] [CrossRef]
- United Nations. World Population Ageing. 2017. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf (accessed on 12 September 2021).
- Nakamura, K. The concept and treatment of locomotive syndrome: Its acceptance and spread in Japan. J. Orthop. Sci. 2011, 16, 489–491; [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Niu, K.; Fujita, K.; Hozawa, A.; Ohmori-Matsuda, K.; Kuriyama, S.; Nakaya, N.; Ebihara, S.; Okazaki, T.; Guo, H.; et al. Impact of physical activity and performance on medical care costs among the Japanese elderly. Geriatr. Gerontol. Int. 2010, 11, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Ishibashi, H. Locomotive syndrome in Japan. Osteoporos. Sarcopenia 2018, 4, 86–94; [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, N.; Muraki, S.; Oka, H.; Tanaka, S.; Ogata, T.; Kawaguchi, H.; Akune, T.; Nakamura, K. Association between new indices in the locomotive syndrome risk test and decline in mobility: Third survey of the ROAD study. J. Orthop. Sci. 2015, 20, 896–905. [Google Scholar] [CrossRef]
- Locomotive Challenge! Council, Locomotive Syndrome Pamphlet 2015. Available online: https://locomo-joa.jp/assets/pdf/index_english.pdf (accessed on 23 November 2020).
- Nakamura, K.; Ogata, T. Locomotive syndrome: Definition and management. Clin. Rev. Bone Miner. Metab. 2016, 14, 56–67. [Google Scholar] [CrossRef]
- World Bank Open Data. Available online: https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=TH (accessed on 16 November 2020).
- World Bank April 8, 2016. Aging in Thailand–Addressing Unmet Health Needs of the Elderly Poor. Available online: https://www.worldbank.org/en/news/press-release/2016/04/08/aging-in-thailand---addressing-unmet-health-needs-of-the-elderly-poor (accessed on 23 December 2019).
- Jitapunkul, S.; Wivatvanit, S. National policies and programs for the aging population in Thailand. Ageing Int. 2008, 33, 62–74. [Google Scholar] [CrossRef]
- จังหวัดน่าน [Official Website of Nan Province]. Available online: http://www.nan.go.th/index.php. Thailand. (accessed on 1 March 2021).
- ข้อมูลด้านสาธารณสุขของจังหวัดน่าน [Public Health Information of Nan Province]. Available online: https://wwwnno.moph.go.th/NHDL/inspector/2559_1/2559-1_general-info.pdf. Thailand. (accessed on 1 March 2021).
- World Health Organization. Primary Health Care Systems (PRIMASYS)-Case Study from Thailand. Available online: https://www.who.int/alliance-hpsr/projects/alliancehpsr_thailandprimasys.pdf?ua=1 (accessed on 8 February 2021).
- Furukawa, T.; Tango, T. Statistics to Medicine; Asakura Publishing Co., Ltd.: Tokyo, Japan, 1983; pp. 172–174. (In Japanese) [Google Scholar]
- Seichi, A.; Hoshino, Y.; Doi, T.; Akai, M.; Tobimatsu, Y.; Iwaya, T. Development of a screening tool for risk of locomotive syndrome in the elderly: The 25-question Geriatric Locomotive Function Scale. J. Orthop. Sci. 2012, 17, 163–172. [Google Scholar] [CrossRef]
- Iwaya, T.; Doi, T.; Seichi, A.; Hoshino, Y.; Ogata, T.; Akai, M. Characteristics of disability in activity of daily living in elderly people associated with locomotive disorders. BMC Geriatr. 2017, 17, 1–13. [Google Scholar] [CrossRef]
- Sasaki, E.; Ishibashi, Y.; Tsuda, E.; Ono, A.; Yamamoto, Y.; Inoue, R.; Takahashi, I.; Umeda, T.; Nakaji, S. Evaluation of locomotive disability using loco-check: A cross-sectional study in the Japanese general population. J. Orthop. Sci. 2013, 18, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Yoshinaga, S.; Shiomitsu, T.; Kamohara, M.; Fujii, Y.; Chosa, E.; Tsuruta, K. Lifestyle-related signs of locomotive syndrome in the general Japanese population: A cross-sectional study. J. Orthop. Sci. 2019, 24, 1105–1109. [Google Scholar] [CrossRef]
- Yoshimura, Y.; Ishijima, M.; Ishibashi, M.; Liu, L.; Arikawa-Hirasawa, E.; Machida, S.; Naito, H.; Hamada, C.; Kominami, E. A nationwide observational study of locomotive syndrome in Japan using the ResearchKit: The Locomonitor study. J. Orthop. Sci. 2019, 24, 1094–1104. [Google Scholar] [CrossRef]
- Seichi, A.; Kimura, A.; Konno, S.; Yabuki, S. Epidemiologic survey of locomotive syndrome in Japan. J. Orthop. Sci. 2016, 21, 222–225. [Google Scholar] [CrossRef] [PubMed]
- Shiratani, K.; Tadaka, E.; Ito, E.; Arimoto, A.; Okochi, A. Population-based study to explore the risk factors to locomotive syndrome among community-dwelling middle-aged people in an urban area. Jpn. Acad. Community Health Nurs. 2017, 20, 4–12. (In Japanese) [Google Scholar]
- Yoshimura, N.; Muraki, S.; Nakamura, K.; Tanaka, S. Epidemiology of the locomotive syndrome: The research on osteoarthritis/osteoporosis against disability study 2005–2015. Mod. Rheumatol. 2017, 27, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, H.; Hagino, H.; Osaki, M.; Tanishima, S.; Tanimura, C.; Matsuura, A.; Makabe, T. Gait variability analysed using an accelerometer is associated with locomotive syndrome among the general elderly population: The GAINA study. J. Orthop. Sci. 2016, 21, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Arbex, M.C.F.B.; Okazaki, J.E.F.; Tavares, D.R.B.; Bersani, A.L.F.; Santos, F.C. Locomotive Syndrome is associated with chronic pain and poor quality of life in Brazilian oldest old: LOCOMOV Project. J. Orthop. Sci. 2021, 26, 162–166. [Google Scholar] [CrossRef]
- Yamada, K.; Ito, Y.M.; Akagi, M.; Chosa, E.; Fuji, T.; Hirano, K.; Ikeda, S.; Ishibashi, H.; Ishibashi, Y.; Ishijima, M.; et al. Reference values for the locomotive syndrome risk test quantifying mobility of 8681 adults aged 20–89 years: A cross-sectional nationwide study in Japan. J. Orthop. Sci. 2020, 25, 1084–1092. [Google Scholar] [CrossRef]
- Kimura, K.; Ninomiya, H.; Endo, Y.; Kambayashi, Y. The effect of diabetes mellitus on the Two-Step value for gait ability. Aging Med. 2018, 1, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Minoura, Y.; Notsu, T. Kayaioka schools and the expansion of secondary education in rural Northeastern Thailand: With special reference to the mechanism for the rapid rise in attendance. Jpn. J. Southeast. Asian Stud. 1998, 36, 131–148. (In Japanese) [Google Scholar]
- Suzuki, K.; Morishita, M.; Kampeeraparb, S. A study on the principles and development of basic education reform in Thailand. Comp. Educ. 2004, 30, 148–167. (In Japanese) [Google Scholar] [CrossRef][Green Version]
- Nakamura, S.; Inayama, T.; Hata, K. Association between health literacy and eating vegetables and socioeconomic status in adults. Jpn. J. Health Promot. 2016, 18, 27–35. (In Japanese) [Google Scholar]
- Lee, S.Y.; Tsai, T.I.; Tsai, Y.W.; Kuo, K.N. Health literacy, health status, and healthcare utilization of Taiwanese adults: Results from a national survey. BMC Public Health. 2010, 10, 614. [Google Scholar] [CrossRef]
- Prevalence of Overweight Among Adults, BMI ≥25 (Age-Standardized Estimate). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/prevalence-of-overweight-among-adults-bmi-=-25-)(age-standardized-estimate)-(-) (accessed on 23 November 2020).
- Cetthakrikul, N.; Phulkerd, S.; Jaichuen, N.; Sacks, G.; Tangcharoensathien, V. Assessment of the stated policies of prominent food companies related to obesity and non-communicable disease (NCD) prevention in Thailand. Glob. Health 2019, 15, 12; [Google Scholar] [CrossRef]
- Tanaka, S.; Ando, K.; Kobayashi, K.; Seki, T.; Ishizuka, S.; Machino, M.; Morozumi, M.; Kanbara, S.; Ito, S.; Inoue, T.; et al. Waist Circumference Measured by Bioelectrical Impedance Analysis Is Interchangeable with Manual Measurement: Increased Waist Circumference Is Associated with Locomotive Syndrome Risk. BioMed Res. Int. 2019, 2019, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Aoki, K.; Sakuma, M.; Ogisho, N.; Nakamura, K.; Chosa, E.; Endo, N. The effects of self-directed home exercise with serial telephone contacts on physical functions and quality of life in elderly people at high risk of locomotor dysfunction. Acta Med. Okayama 2015, 69, 245–253. [Google Scholar] [PubMed]
- Hashimoto, M.; Yasumura, S.; Nakano, K.; Kimura, M.; Nakamura, K.; Fujino, K.; Ito, H. Feasibility study of locomotion training in a home-visit preventive care program. Nippon. Ronen Igakkai Zasshi. Jpn. J. Geriatr. 2012, 49, 476–482. [Google Scholar] [CrossRef] [PubMed]
| Two-Step Score <1.3 (n = 118) | Two-Step Score ≥1.3 (n = 47) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Mean ± SD | n | % | Mean ± SD | p-Value | |||
| Age | 66.9 ± 7.8 | 61.0 ± 7.1 | <0.001 (a) | *** | |||||
| Sex | Male | 37 | 31.4 | 14 | 29.8 | 0.992 (b) | |||
| Female | 81 | 68.6 | 33 | 70.2 | |||||
| Years of schooling (year) | Median (25th,75th) | 4.0 (4.0,6.5) | 9.0 (4.0,13.0) | <0.001 (d) | *** | ||||
| BMI (kg/m2) | 24.3 ± 3.7 | 23.3 ± 2.4 | 0.057 (c) | ||||||
| <25.0 | 69 | 58.5 | 37 | 78.7 | 0.023 (b) | * | |||
| ≥25.0 | 49 | 41.5 | 10 | 21.3 | |||||
| The two-step score | 1.1 ± 0.1 | 1.4 ± 0.1 | <0.001 (d) | *** | |||||
| Difficulty with simple tasks (n = 164) | Extremely difficult | 0 | 0.0 | 0 | 0.0 | 0.300 (d) | |||
| Considerably difficult | 1 | 0.9 | 0 | 0.0 | |||||
| Moderately difficult | 6 | 5.1 | 0 | 0.0 | |||||
| Mildly difficult | 15 | 12.8 | 6 | 12.8 | |||||
| Not difficult | 95 | 81.2 | 41 | 87.2 | |||||
| Difficulty with load-bring tasks | Extremely difficult | 11 | 9.3 | 2 | 4.3 | 0.031 (d) | * | ||
| Considerably difficult | 15 | 12.7 | 4 | 8.5 | |||||
| Moderately difficult | 29 | 24.6 | 9 | 19.2 | |||||
| Mildly difficult | 34 | 28.8 | 13 | 27.7 | |||||
| Not difficult | 29 | 24.6 | 19 | 40.4 | |||||
| Difficulty walking briskly | Extremely difficult | 5 | 4.2 | 0 | 0.0 | 0.005 (d) | ** | ||
| Considerably difficult | 1 | 0.9 | 0 | 0.0 | |||||
| Moderately difficult | 15 | 12.7 | 0 | 0.0 | |||||
| Mildly difficult | 33 | 28.0 | 12 | 25.5 | |||||
| Not difficult | 64 | 54.2 | 35 | 74.5 | |||||
| Continuous walking time (n = 163) | Less than 10 s | 4 | 3.5 | 0 | 0.0 | <0.001 (d) | *** | ||
| About 1 min | 5 | 4.3 | 0 | 0.0 | |||||
| About 5 min | 20 | 17.2 | 2 | 4.3 | |||||
| About 10 min | 41 | 35.3 | 14 | 29.8 | |||||
| 15 min or more | 46 | 39.7 | 31 | 66.0 | |||||
| COR | 95% CI | p-Value | AOR | 95%CI | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | 50–59 | 1.00 | ||||||||||
| 60–69 | 2.09 | 0.94 | 4.66 | 0.071 | ||||||||
| ≥70 | 10.40 | 3.44 | 31.48 | <0.001 | *** | |||||||
| Sex | Male | 1.00 | 1.00 | |||||||||
| Female | 0.93 | 0.45 | 1.94 | 0.844 | 1.57 | 0.68 | 3.65 | 0.291 | ||||
| Years of schooling | ≥12 years | 1.00 | 1.00 | |||||||||
| 7–11 years | 2.33 | 0.78 | 6.92 | 0.129 | 2.61 | 0.81 | 8.43 | 0.109 | ||||
| 0–6 years | 5.69 | 2.38 | 13.58 | <0.001 | *** | 4.46 | 1.77 | 11.28 | 0.002 | ** | ||
| Comorbidities | Hypertension | - | 1.00 | 1.00 | ||||||||
| + | 1.87 | 0.94 | 3.72 | 0.076 | 1.62 | 0.76 | 3.44 | 0.210 | ||||
| Hyperlipidemia | - | 1.00 | 1.00 | |||||||||
| + | 2.69 | 1.22 | 5.92 | 0.014 | * | 2.14 | 0.93 | 4.94 | 0.074 | |||
| Diabetes | - | 1.00 | 1.00 | |||||||||
| + | 2.70 | 0.98 | 7.49 | 0.056 | 2.31 | 0.79 | 6.70 | 0.125 | ||||
| No underlying diseases | 1.00 | 1.00 | ||||||||||
| Underlying diseases | 3.18 | 1.55 | 6.51 | 0.002 | ** | 2.55 | 1.19 | 5.48 | 0.017 | * | ||
| BMI (kg/m2) | 18.5–24.9 | 1.00 | 1.00 | |||||||||
| <18.5 | 2.81 | 0.32 | 25.02 | 0.354 | 0.96 | 0.09 | 10.27 | 0.974 | ||||
| ≥25.0 | 2.76 | 1.25 | 6.09 | 0.012 | * | 3.06 | 1.32 | 7.09 | 0.009 | ** | ||
| Low back pain | - | 1.00 | 1.00 | |||||||||
| + | 1.20 | 0.60 | 2.40 | 0.602 | 1.19 | 0.57 | 2.48 | 0.653 | ||||
| Knee pain | - | 1.00 | 1.00 | |||||||||
| + | 1.95 | 0.97 | 3.92 | 0.059 | 1.91 | 0.91 | 4.02 | 0.087 | ||||
| Anxious about fall in daily life | No | 1.00 | 1.00 | |||||||||
| Yes | 1.63 | 0.82 | 3.21 | 0.161 | 1.41 | 0.68 | 2.92 | 0.362 | ||||
| Anxious about difficulty with walking in the future | No | 1.00 | 1.00 | |||||||||
| Yes | 0.81 | 0.41 | 1.59 | 0.538 | 0.75 | 0.36 | 1.57 | 0.444 | ||||
| Difficulty in putting on trousers | Not difficult | 1.00 | 1.00 | |||||||||
| Difficult | 1.33 | 0.61 | 2.90 | 0.482 | 0.96 | 0.41 | 2.25 | 0.924 | ||||
| Difficulty walking briskly | Not difficult | 1.00 | 1.00 | |||||||||
| Difficult | 2.46 | 1.16 | 5.21 | 0.019 | * | 1.72 | 0.77 | 3.82 | 0.187 | |||
| Difficulty with simple tasks | Not difficult | 1.00 | 1.00 | |||||||||
| Difficult | 1.58 | 0.60 | 4.19 | 0.356 | 1.49 | 0.51 | 4.38 | 0.473 | ||||
| Difficulty with load-bearing tasks | Not difficult | 1.00 | 1.00 | |||||||||
| Difficult | 2.08 | 1.02 | 4.27 | 0.045 | * | 1.83 | 0.85 | 3.95 | 0.122 | |||
| Weekday sitting time | <360 min | 1.00 | 1.00 | |||||||||
| ≥360 min | 1.69 | 0.53 | 5.34 | 0.374 | 1.69 | 0.50 | 5.73 | 0.402 | ||||
| Weekend sitting time | <360 min | 1.00 | 1.00 | |||||||||
| ≥360 min | 1.32 | 0.45 | 3.83 | 0.612 | 1.13 | 0.36 | 3.55 | 0.829 | ||||
| Exercising time in a day | ≥30 min | 1.00 | 1.00 | |||||||||
| <30 min | 1.85 | 0.81 | 4.23 | 0.143 | 1.40 | 0.58 | 3.40 | 0.452 | ||||
| Continuous walking time | ≥15 min | 1.00 | 1.00 | |||||||||
| <15 min | 2.95 | 1.45 | 5.99 | 0.003 | ** | 2.51 | 1.18 | 5.31 | 0.017 | * | ||
| Partial Regression Coefficient | 95% CI | p-Value | |||
|---|---|---|---|---|---|
| Age (years) | −0.01 | −0.01 | 0.00 | <0.001 | *** |
| Knee pain | −0.03 | −0.06 | 0.00 | 0.048 | * |
| Anxiety about falling in daily life | −0.02 | −0.04 | 0.00 | 0.026 | * |
| Difficulty with simple tasks | −0.06 | −0.10 | −0.02 | 0.007 | ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niwayama, M.; Sakisaka, K.; Wongwatcharapaiboon, P.; Rattanachun, V.; Miyata, S.; Takahashi, K. Prevalence of Locomotive Organ Impairment and Associated Factors among Middle-Aged and Older People in Nan Province, Thailand. Int. J. Environ. Res. Public Health 2021, 18, 10871. https://doi.org/10.3390/ijerph182010871
Niwayama M, Sakisaka K, Wongwatcharapaiboon P, Rattanachun V, Miyata S, Takahashi K. Prevalence of Locomotive Organ Impairment and Associated Factors among Middle-Aged and Older People in Nan Province, Thailand. International Journal of Environmental Research and Public Health. 2021; 18(20):10871. https://doi.org/10.3390/ijerph182010871
Chicago/Turabian StyleNiwayama, Marie, Kayako Sakisaka, Pongthep Wongwatcharapaiboon, Valika Rattanachun, Satoshi Miyata, and Kenzo Takahashi. 2021. "Prevalence of Locomotive Organ Impairment and Associated Factors among Middle-Aged and Older People in Nan Province, Thailand" International Journal of Environmental Research and Public Health 18, no. 20: 10871. https://doi.org/10.3390/ijerph182010871
APA StyleNiwayama, M., Sakisaka, K., Wongwatcharapaiboon, P., Rattanachun, V., Miyata, S., & Takahashi, K. (2021). Prevalence of Locomotive Organ Impairment and Associated Factors among Middle-Aged and Older People in Nan Province, Thailand. International Journal of Environmental Research and Public Health, 18(20), 10871. https://doi.org/10.3390/ijerph182010871






