Association between Fruit and Vegetable Consumption and Depression Symptoms in Young People and Adults Aged 15–45: A Systematic Review of Cohort Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Study Selection
2.5. Data Extraction
2.6. Quality Assessment
3. Results
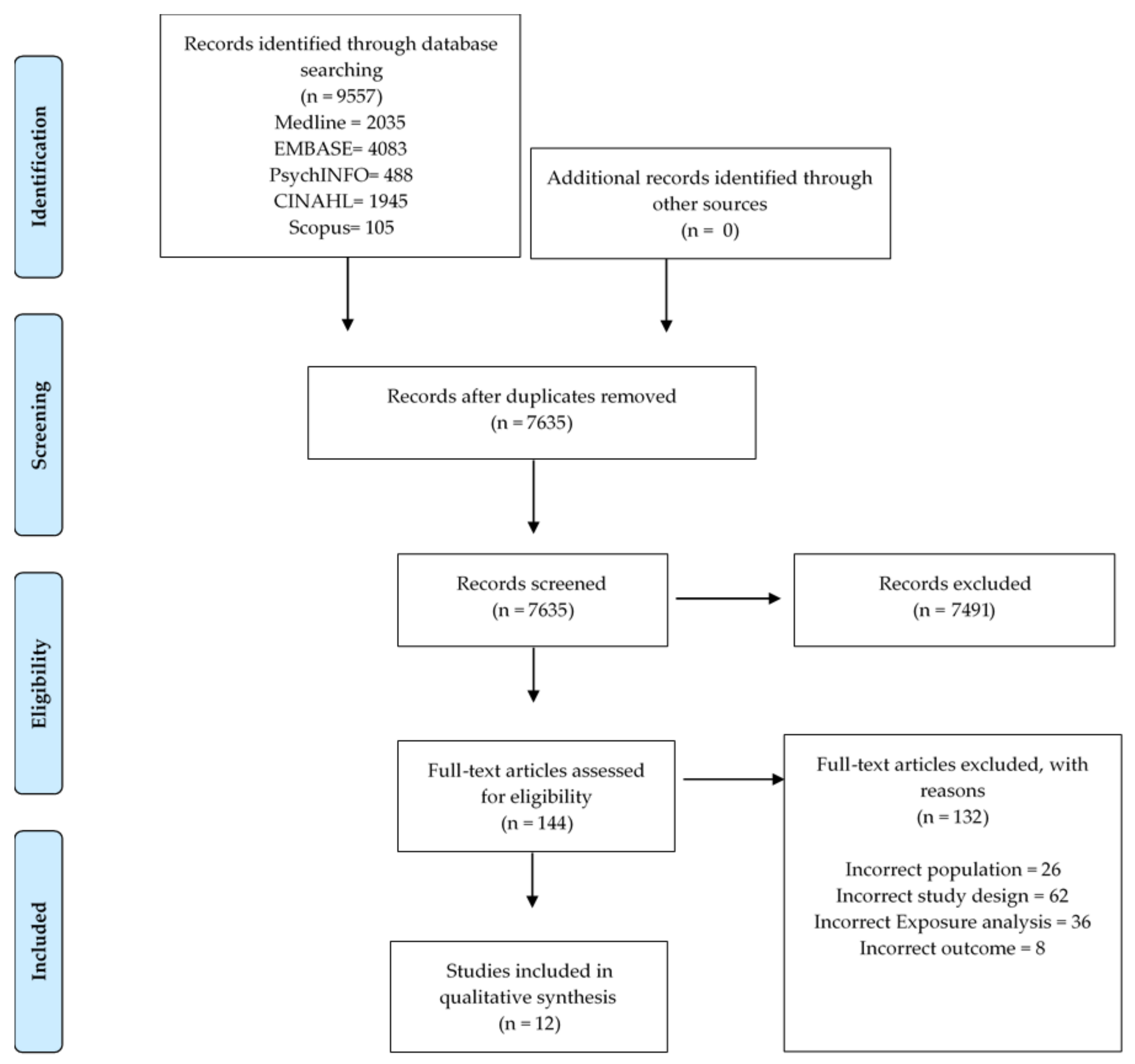
3.1. Search Results
3.2. Study Characteristics
3.3. Dietary Measures
3.4. Depression Measures
3.5. Quality Assessment
3.6. Outcomes
3.6.1. Impact of Fruit and Vegetable Intake on Depressive Symptoms
3.6.2. Impact of Fruit and Vegetable Intake on Depression
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Diet Types Explained
References
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Available online: http://apps.who.int/iris/bitstream/10665/254610/1/WHO-MSD-MER-2017.2-eng.pdf?ua=1 (accessed on 28 July 2020).
- Ferrari, A.J.; Charlson, F.J.; Norman, R.E.; Patten, S.B.; Freedman, G.D.; Murray, C.J.; Vos, T.; Whiteford, H.A. Burden of Depressive Disorders by Country, Sex, Age, and Year: Findings from the Global Burden of Disease Study. PLoS Med. 2013, 10, e1001547. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; He, H.; Yang, J.; Feng, X.; Zhao, F.; Lyu, J. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. J. Psychiatr. Res. 2020, 126, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Saghafian, F.; Malmir, H.; Saneei, P.; Milajerdi, A.; Larijani, B.; Esmaillzadeh, A. Fruit and vegetable consumption and risk of depression: Accumulative evidence from an updated systematic review and meta-analysis of epidemiological studies. Br. J. Nutr. 2018, 119, 1087–1101. [Google Scholar] [CrossRef]
- Bilsen, J. Suicide and Youth: Risk Factors. Front. Psychiatry 2018, 9, 540. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.M.; Ross, D.; Hardy, R.; Kuh, D.; Power, C.; Johnson, A.; Wellings, K.; McCambridge, J.; Cole, T.J.; Kelly, Y.; et al. Life course epidemiology: Recognising the importance of adolescence. J. Epidemiol. Community Health 2015, 69, 719–720. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- World Health Organizanization. Mental Health and Substance Use. Available online: https://www.who.int/teams/mental-health-and-substance-use/suicide-data (accessed on 2 January 2021).
- Lopresti, A.L.; Hood, S.D.; Drummond, P.D. A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. J. Affect. Disord. 2013, 148, 12–27. [Google Scholar] [CrossRef]
- Lassale, C.; Batty, G.D.; Baghdadli, A.; Jacka, F.N.; Sánchez-Villegas, A.; Kivimäki, M.; Akbaraly, T.N. Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol. Psychiatry 2019, 24, 965–986. [Google Scholar] [CrossRef]
- Altun, A.; Brown, H.; Szoeke, C.; Goodwill, A.M. The Mediterranean dietary pattern and depression risk: A systematic review. Neurol. Psychiatry Brain Res. 2019, 33, 1–10. [Google Scholar] [CrossRef]
- Lai, J.S.; Hiles, S.; Bisquera, A.; Hure, A.J.; McEvoy, M.; Attia, J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am. J. Clin. Nutr. 2013, 99, 181–197. [Google Scholar] [CrossRef]
- Tarelho, A.; Duarte, M.; Melim, J.; Batista, A.; Almeida, S. Dietary Pattern and Mental Health: Review of Literature. Eur. Psychiatry 2016, 33, S517. [Google Scholar] [CrossRef]
- Mason-D’Croz, D.; Bogard, J.R.; Sulser, T.B.; Cenacchi, N.; Dunston, S.; Herrero, M.; Wiebe, K. Gaps between fruit and vegetable production, demand, and recommended consumption at global and national levels: An integrated modelling study. Lancet Planet. Health 2019, 3, e318–e329. [Google Scholar] [CrossRef]
- Slavin, J.L.; Lloyd, B. Health Benefits of Fruits and Vegetables. Adv. Nutr. 2012, 3, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Conner, T.S.; Brookie, K.L.; Carr, A.C.; Mainvil, L.A.; Vissers, M.C.M. Let them eat fruit! The effect of fruit and vegetable consumption on psychological well-being in young adults: A randomized controlled trial. PLoS ONE 2017, 12, e0171206. [Google Scholar] [CrossRef]
- Saghafian, F.; Malmir, H.; Saneei, P.; Keshteli, A.H.; Hosseinzadeh-Attar, M.J.; Afshar, H.; Siassi, F.; Esmaillzadeh, A.; Adibi, P. Consumption of fruit and vegetables in relation with psychological disorders in Iranian adults. Eur. J. Nutr. 2018, 57, 2295–2306. [Google Scholar] [CrossRef]
- Ju, S.-Y.; Park, Y.-K. Low fruit and vegetable intake is associated with depression among Korean adults in data from the 2014 Korea National Health and Nutrition Examination Survey. J. Health Popul. Nutr. 2019, 38, 1–10. [Google Scholar] [CrossRef]
- Peltzer, K.; Pengpid, S. Dietary consumption and happiness and depression among university students: A cross-national survey. J. Psychol. Afr. 2017, 27, 372–377. [Google Scholar] [CrossRef]
- Wu, S.; Fisher-Hoch, S.P.; Reininger, B.M.; McCormick, J.B. Association between fruit and vegetable intake and symptoms of mental health conditions in Mexican Americans. Health Psychol. 2018, 37, 1059–1066. [Google Scholar] [CrossRef]
- Bhattacharyya, M.; Marston, L.; Walters, K.; D’Costa, G.; King, M.; Nazareth, I. Psychological distress, gender and dietary factors in South Asians: A cross-sectional survey. Public Health Nutr. 2013, 17, 1538–1546. [Google Scholar] [CrossRef]
- Kim, T.-H.; Choi, J.-Y.; Lee, H.-H.; Park, Y. Associations between Dietary Pattern and Depression in Korean Adolescent Girls. J. Pediatr. Adolesc. Gynecol. 2015, 28, 533–537. [Google Scholar] [CrossRef]
- Angelino, D.; Godos, J.; Ghelfi, F.; Tieri, M.; Titta, L.; Lafranconi, A.; Marventano, S.; Alonzo, E.; Gambera, A.; Sciacca, S.; et al. Fruit and vegetable consumption and health outcomes: An umbrella review of observational studies. Int. J. Food Sci. Nutr. 2019, 70, 652–667. [Google Scholar] [CrossRef] [PubMed]
- Głąbska, D.; Guzek, D.; Groele, B.; Gutkowska, K. Fruit and Vegetable Intake and Mental Health in Adults: A Systematic Review. Nutrition 2020, 12, 115. [Google Scholar] [CrossRef] [PubMed]
- Goh, C.M.J.; Abdin, E.; Jeyagurunathan, A.; Shafie, S.; Sambasivam, R.; Zhang, Y.; Vaingankar, J.A.; Chong, S.A.; Subramaniam, M. Exploring Singapore’s consumption of local fish, vegetables and fruits, meat and problematic alcohol use as risk factors of depression and subsyndromal depression in older adults. BMC Geriatr. 2019, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tsai, A.C.; Chang, T.-L.; Chi, S.-H. Frequent consumption of vegetables predicts lower risk of depression in older Taiwanese-results of a prospective population-based study. Public Health Nutr. 2011, 15, 1087–1092. [Google Scholar] [CrossRef] [PubMed]
- Payne, M.E.; Steck, S.E.; George, R.R.; Steffens, D.C. Fruit, Vegetable, and Antioxidant Intakes Are Lower in Older Adults with Depression. J. Acad. Nutr. Diet. 2012, 112, 2022–2027. [Google Scholar] [CrossRef]
- Głąbska, D.; Guzek, D.; Groele, B.; Gutkowska, K. Fruit and vegetables intake in adolescents and mental health: A systematic review. Rocz. Państwowego Zakładu Hig. 2020, 71, 15–25. [Google Scholar] [CrossRef]
- Khalid, S.; Williams, C.M.; Reynolds, S. Is there an association between diet and depression in children and adolescents? A systematic review. Br. J. Nutr. 2016, 116, 2097–2108. [Google Scholar] [CrossRef]
- McMartin, S.E.; Jacka, F.N.; Colman, I. The association between fruit and vegetable consumption and mental health disorders: Evidence from five waves of a national survey of Canadians. Prev. Med. 2013, 56, 225–230. [Google Scholar] [CrossRef]
- Palta, P.; Samuel, L.J.; Miller, E.R., 3rd; Szanton, S.L. Depression and Oxidative Stress: Results from a meta-analysis of observational studies. Psychosom. Med. 2014, 76, 12–19. [Google Scholar] [CrossRef]
- Maes, M.; De Vos, N.; Pioli, R.; Demedts, P.; Wauters, A.; Neels, H.; Christophe, A. Lower serum vitamin E concentrations in major depression–Another marker of lowered antioxidant defenses in that illness. J. Affect. Disord. 2000, 58, 241–246. [Google Scholar] [CrossRef]
- Miller, A.L. The methylation, neurotransmitter, and antioxidant connections between folate and depression. Altern. Med. Rev. 2008, 13, 216–226. [Google Scholar] [PubMed]
- Jiménez-Fernández, S.; Gurpegui, M.; Díaz-Atienza, F.; Pérez-Costillas, L.; Gerstenberg, M.; Correll, C.U. Oxidative Stress and Antioxidant Parameters in Patients with Major Depressive Disorder Compared to Healthy Controls Before and After Antidepressant Treatment: Results from a Meta-Analysis. J. Clin. Psychiatry 2015, 76, 1658–1667. [Google Scholar] [CrossRef] [PubMed]
- Nowak, G. Zinc, future mono/adjunctive therapy for depression: Mechanisms of antidepressant action. Pharmacol. Rep. 2015, 67, 659–662. [Google Scholar] [CrossRef]
- Fava, M.; Borus, J.S.; Alpert, J.E.; Nierenberg, A.A.; Rosenbaum, J.F.; Bottiglieri, T. Folate, vitamin B12, and homocysteine in major depressive disorder. Am. J. Psychiatry 1997, 154, 426–428. [Google Scholar] [CrossRef] [PubMed]
- Ghadirian, A.M.; Ananth, J.; Engelsmann, F. Folic acid deficiency and depression. J. Psychosom. Res. 1980, 21, 926–929. [Google Scholar] [CrossRef]
- Reynolds, E.H. Folic acid, ageing, depression, and dementia. BMJ 2002, 324, 1512–1515. [Google Scholar] [CrossRef]
- Rooney, C.; McKinley, M.; Woodside, J. A systematic review of the potential role of fruit and vegetables in depression. Proc. Nutr. Soc. 2016, 75, E162. [Google Scholar] [CrossRef]
- Rahe, C.; Unrath, M.; Berger, K. Dietary patterns and the risk of depression in adults: A systematic review of observational studies. Eur. J. Nutr. 2014, 53, 997–1013. [Google Scholar] [CrossRef]
- Murakami, K.; Sasaki, S. Dietary intake and depressive symptoms: A systematic review of observational studies. Mol. Nutr. Food Res. 2009, 54, 471–488. [Google Scholar] [CrossRef]
- Sanhueza, C.; Ryan, L.; Foxcroft, D. Diet and the risk of unipolar depression in adults: Systematic review of cohort studies. J. Hum. Nutr. Diet. 2012, 26, 56–70. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Mental Health. Available online: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/mental-health/latest-release (accessed on 15 October 2020).
- National Intitute of Mental Health. Major Depression. Available online: https://www.nimh.nih.gov/health/statistics/major-depression.shtml (accessed on 15 October 2020).
- Frech, A. Healthy behavior trajectories between adolescence and young adulthood. Adv. Life Course Res. 2012, 17, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.; Dash, S.; Allender, S.; Jacka, F.; Hoare, E. Diet and Mental Health During Emerging Adulthood: A Systematic Review. Emerg. Adulthood. 2020, 1–15. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. National Survey of Mental Health and Wellbeing: Summary of Results. Available online: https://www.abs.gov.au/statistics/health/mental-health/national-survey-mental-health-and-wellbeing-summary-results/latest-release#articles (accessed on 2 January 2020).
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Murlow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 20 September 2020).
- Lo, C.K.-L.; Mertz, D.; Loeb, M. Newcastle-Ottawa Scale: Comparing reviewers’ to authors’ assessments. BMC Med. Res. Methodol. 2014, 14, 45. [Google Scholar] [CrossRef]
- Choda, N.; Wakai, K.; Naito, M.; Imaeda, N.; Goto, C.; Maruyama, K.; Kadomatsu, Y.; Tsukamoto, M.; Sasakabe, T.; Kubo, Y.; et al. Associations between diet and mental health using the 12-item General Health Questionnaire: Cross-sectional and prospective analyses from the Japan Multi-Institutional Collaborative Cohort Study. Nutr. J. 2020, 19, 1–14. [Google Scholar] [CrossRef]
- Mujcic, R.; Oswald, A.J. Does eating fruit and vegetables also reduce the longitudinal risk of depression and anxiety? A commentary on ’Lettuce be happy’. Soc. Sci. Med. 2019, 222, 346–348. [Google Scholar] [CrossRef]
- Ocean, N.; Howley, P.; Ensor, J. Lettuce be happy: A longitudinal UK study on the relationship between fruit and vegetable consumption and well-being. Soc. Sci. Med. 2019, 222, 335–345. [Google Scholar] [CrossRef]
- Winzer, R.; Sorjonen, K.; Lindberg, L. What Predicts Stable Mental Health in the 18–29 Age Group Compared to Older Age Groups? Results from the Stockholm Public Health Cohort 2002–2014. Int. J. Environ. Res. Public Health 2018, 15, 2859. [Google Scholar] [CrossRef]
- Winpenny, E.M.; Van Harmelen, A.-L.; White, M.; Van Sluijs, E.M.; Goodyer, I.M. Diet quality and depressive symptoms in adolescence: No cross-sectional or prospective associations following adjustment for covariates. Public Health Nutr. 2018, 21, 2376–2384. [Google Scholar] [CrossRef]
- Hoare, E.; Hockey, M.; Ruusunen, A.; Jacka, F.N. Does Fruit and Vegetable Consumption During Adolescence Predict Adult Depression? A Longitudinal Study of US Adolescents. Front. Psychiatry 2018, 9, 581. [Google Scholar] [CrossRef]
- Collin, C.; Assmann, K.E.; Andreeva, V.A.; Lemogne, C.; Hercberg, S.; Galan, P.; Kesse-Guyot, E. Adherence to dietary guidelines as a protective factor against chronic or recurrent depressive symptoms in the French SU.VI.MAX cohort. Prev. Med. 2016, 91, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Kingsbury, M.; Dupuis, G.; Jacka, F.; Roy-Gagnon, M.-H.; McMartin, S.E.; Colman, I. Associations between fruit and vegetable consumption and depressive symptoms: Evidence from a national Canadian longitudinal survey. J. Epidemiol. Community Health 2015, 70, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.-C.; Cassidy, A.; Willett, W.C.; Rimm, E.B.; O’Reilly, E.J.; Okereke, O.I. Dietary flavonoid intake and risk of incident depression in midlife and older women. Am. J. Clin. Nutr. 2016, 104, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Akbaraly, T.N.; Sabia, S.; Shipley, M.J.; Batty, G.D.; Kivimäki, M. Adherence to healthy dietary guidelines and future depressive symptoms: Evidence for sex differentials in the Whitehall II study. Am. J. Clin. Nutr. 2013, 97, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Chai, W.; Nigg, C.R.; Pagano, I.; Motl, R.W.; Horwath, C.C.; Dishman, R.K. Associations of quality of life with physical activity, fruit and vegetable consumption, and physical inactivity in a free living, multiethnic population in Hawaii: A longitudinal study. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 83. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A.; Delgado-Rodríguez, M.; Alonso, A.; Schlatter, J.; Lahortiga, F.; Majem, L.S.; Martínez-González, M.A. Association of the Mediterranean Dietary Pattern With the Incidence of Depression: The Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Arch. Gen. Psychiatry 2009, 66, 1090–1098. [Google Scholar] [CrossRef]
- Mujcic, R.; Oswald, A.J. Evolution of Well-Being and Happiness After Increases in Consumption of Fruit and Vegetables. Am. J. Public Health 2016, 106, 1504–1510. [Google Scholar] [CrossRef]
- Seguí-Gómez, M.; De La Fuente, C.; Vázquez, Z.; De Irala, J.; A Martínez-González, M. Cohort profile: The ‘Seguimiento Universidad de Navarra’ (SUN) study. Int. J. Epidemiol. 2006, 35, 1417–1422. [Google Scholar] [CrossRef]
- Mihrshahi, S.; Dobson, A.J.; Mishra, G.D. Fruit and vegetable consumption and prevalence and incidence of depressive symptoms in mid-age women: Results from the Australian longitudinal study on women’s health. Eur. J. Clin. Nutr. 2015, 69, 585–591. [Google Scholar] [CrossRef]
- Emanuel, A.S.; McCully, S.N.; Gallagher, K.M.; Updegraff, J.A. Theory of Planned Behavior explains gender difference in fruit and vegetable consumption. Appetite 2012, 59, 693–697. [Google Scholar] [CrossRef]
- De Wit, L.; Van Straten, A.; Van Herten, M.; Penninx, B.; Cuijpers, P. Depression and body mass index, a u-shaped association. BMC Public Health 2009, 9, 14. [Google Scholar] [CrossRef] [PubMed]
- Révah-Levy, A.; Speranza, M.; Barry, C.; Hassler, C.; Gasquet, I.; Moro, M.-R.; Falissard, B. Association between Body Mass Index and depression: The “fat and jolly” hypothesis for adolescents girls. BMC Public Health 2011, 11, 649. [Google Scholar] [CrossRef] [PubMed]
- Bountziouka, V.; Polychronopoulos, E.; Zeimbekis, A.; Papavenetiou, E.; Ladoukaki, E.; Papairakleous, N.; Gotsis, E.; Metal-linos, G.; Lionis, C.; Panagiotakos, D. Long-term fish intake is associated with less severe depressive symptoms among elderly men and women: The MEDIS (MEDiterranean ISlands Elderly) epidemiological study. J. Aging Health 2009, 21, 864–880. [Google Scholar] [CrossRef] [PubMed]
- Timonen, M.; Horrobin, D.; Jokelainen, J.; Laitinen, J.; Herva, A.; Räsänen, P. Fish consumption and depression: The Northern Finland 1966 birth cohort study. J. Affect. Disord. 2004, 82, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Liu, X.; Zhang, D. Fish consumption and risk of depression: A meta-analysis. J. Epidemiol. Community Health 2015, 70, 299–304. [Google Scholar] [CrossRef]
- Offringa, L.C.; Stanton, M.V.; Hauser, M.E.; Gardner, C.D. Fruits and Vegetables Versus Vegetables and Fruits: Rhyme and Reason for Word Order in Health Messages. Am. J. Lifestyle Med. 2018, 13, 224–234. [Google Scholar] [CrossRef]
- Hebert, J.R.; Clemow, L.; Pbert, L.; Ockene, I.S.; Ockene, J.K. Social Desirability Bias in Dietary Self-Report May Compromise the Validity of Dietary Intake Measures. Int. J. Epidemiol. 1995, 24, 389–398. [Google Scholar] [CrossRef]
- Fried, E.I. The 52 symptoms of major depression: Lack of content overlap among seven common depression scales. J. Affect. Disord. 2017, 208, 191–197. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale. A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Blackwell, B. Psychiatric Illness in General Practice: A Detailed Study Using a New Method of Case Identification. BMJ 1970, 2, 439–443. [Google Scholar] [CrossRef]
- Eaton, W.W.; Neufeld, K.; Chen, L.-S.; Cai, G. A Comparison of Self-report and Clinical Diagnostic Interviews for Depression: Diagnostic interview schedule and schedules for clinical assessment in neuropsychiatry in the Baltimore epidemiologic catchment area follow-up. Arch. Gen. Psychiatry 2000, 57, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Polaino, A.; Senra, C. Measurement of depression: Comparison between self-reports and clinical assessments of depressed outpatients. J. Psychopathol. Behav. Assess. 1991, 13, 313–324. [Google Scholar] [CrossRef]
- Uher, R.; Perlis, R.H.; Placentino, A.; Dernovšek, M.Z.; Henigsberg, N.; Mors, O.; Maier, W.; McGuffin, P.; Farmer, A. Self-Report And Clinician-Rated Measures Of Depression Severity: Can One Replace The Other? Depress. Anxiety 2012, 29, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Quirk, S.E.; Williams, L.J.; O’Neil, A.; Pasco, J.A.; Jacka, F.N.; Housden, S.; Berk, M.; Brennan, S.L. The association between diet quality, dietary patterns and depression in adults: A systematic review. BMC Psychiatry 2013, 13, 175. [Google Scholar] [CrossRef] [PubMed]
- Francis, H.; Stevenson, R.J.; Chambers, J.R.; Gupta, D.; Newey, B.; Lim, C.K. A brief diet intervention can reduce symptoms of depression in young adults–A randomised controlled trial. PLoS ONE 2019, 14, e0222768. [Google Scholar] [CrossRef]
- Jacka, F.N.; O’Neil, A.; Opie, R.; Itsiopoulos, C.; Cotton, S.; Mohebbi, M.; Castle, D.; Dash, S.; Mihalopoulos, C.; Chatterton, M.L.; et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017, 15, 1–13. [Google Scholar] [CrossRef]
- Estaquio, C.; Kesse-Guyot, E.; Deschamps, V.; Bertrais, S.; Dauchet, L.; Galan, P.; Hercberg, S.; Castetbon, K. Adherence to the French Programme National Nutrition Santé Guideline Score Is Associated with Better Nutrient Intake and Nutritional Status. J. Am. Diet. Assoc. 2009, 109, 1031–1041. [Google Scholar] [CrossRef]
| Reference/Country/Year | Participant Characteristics (Age Range, Mean Age at Baseline (SD), Gender) | Study Characteristics (Number of Participants, Follow-Up Period) | Cohort | Dietary Assessment Method (Recall Period) | Depression Assessment Method (Analysis Assessment) |
|---|---|---|---|---|---|
| Choda et al. [51] Japan, 2020 | Age range at baseline: 35–69 y Age mean: Participants with a GHQ score ≥ 4 is 50.1 (9.1); participants with a GHQ score < 4 is 52.9 (9.5) Gender (female): ~50% | 4701 ~5 y (Daiko) ~6 y (Shizuoka) | The Japan Multi-Institutional Collaborative Cohort (J-MICC), the Daiko Study and the Shizuoka area | A validated short FFQ (46 food items) (over the past years) | The 12-item General Health Questionnaire (the GHQ-12) (psychological distress and social dysfunction factors) |
| Mujcic and Oswald [52] Australia, 2019 | Age range: ≥15 y Age mean:-a Gender (female):-a | 7108 2 y | The Household, Income, and Labour Dynamics in Australia (HILDA) Survey | Short questions on usual intake and frequency intake: “how many days in a usual week do you eat fruit?” and “how many days in a usual week do you eat vegetables?” “On a day when you eat fruit, how many serves of fruit do you usually eat?” and “On a day when you eat vegetables, how many serves of vegetables do you usually eat?” [63] | “Have you ever been told by a doctor or nurse that you have any of long-term health conditions listed below? Please only include those conditions that have lasted or are likely to last for six months or more: Depression/Anxiety” |
| Ocean et al. [53] UK, 2019 | Age range at baseline: 15–104 y Age mean: 47.1 Gender (female):-a | Over 45,000 6 y | The UK Household Longitudinal Study (UKHLS) | Short questions on portion intake: “on a day when you eat fruit or vegetables, how many portions of fruit and vegetables in total do you usually eat?” | The 12-item General Health Questionnaire (the GHQ-12) (psychological distress and social dysfunction factors) |
| Winzer et al. [54] Sweden, 2018 | Age range: 18–29 y Age mean:-a Gender (female): 61.8% | 1704 ~12 y | The Stockholm Public Health Cohort (SPHC) | Short questions on frequency intake: How often do you eat Fruit and berries (an apple, an orange, a banana, a glass of juice, grapes, strawberries)? | The 12-item General Health Questionnaire (the GHQ-12) (psychological distress and social dysfunction factors) |
| Winpenny et al. [55] UK, 2018 | Age range at baseline: 14 y Age mean: 14.5 (0.3) Gender (female): 60% | 603 3 y | The ROOTS study | A 4d diet diary (two weekdays and two weekend days) | The Moods and Feelings Questionnaire (MFQ) (depressive symptoms) |
| Hoare et al. [56] USA, 2018 | Age range at baseline: 12–18 y Age mean at baseline: 15.9 (1.7) Age mean at follow up: 28.9 (1.7) Gender (female):-a | 3696 ~14 y | Add Health | Short questions on frequency intake: “How often did you eat fruit or drink fruit juice yesterday?” The same item with response options was asked for vegetable consumption (previous day) | The Centre for Epidemiologic Studies Depression Scale CES-D 20 (Wave 1) CES-D 10 (Wave 4) (depressive symptoms) |
| Collin et al. [57] France, 2016 | Age range: 35–60 y Age mean: 49.5 (6.2) Gender (female): 56.2% | 3328 11 y * | Supplementation en Vitamines et Mineraux AntioXydants (SU.VI.MAX) | Multiple (3–6) 24-h recalls (Usual intake) | CES-D 20 (Chronic or recurrent depressive symptoms) |
| Kingsbury et al. [58] Canada, 2016 | Age range: 18–104 y Age mean: 44.16 (18.41) Gender (female): 52.8% | 8353 Continuous every 2 y (1994/1995–2010/2011) | Canadian Longitudinal Survey | Food frequency questions: From the fruit and vegetable module in the behavioural risk factor surveillance system of the USA Centres for Disease Control and prevention (Usual intake) | CIDI-SF (Major depression) K6 (Distress) |
| Chang et al. [59] USA, 2016 | Age ** range: 36–55 y Age mean: ~46.3 (4.6) Gender (female): 100% | 36,658 10 y | Nurses’ Health Study II ** (NHSII) | Semi-quantitative FFQ (130 food items) (Previous years usual intake) | MHI-5 (1993, 1997) Antidepressant use (1997) Doctor diagnosis (2001) (Depression) |
| Akbaraly et al. [60] UK, 2013 | Age range at baseline: 35–55 y Age at initial measurement for this analysis: 39–64 y Gender (female): 25.1% | 4215 (5 y) 4053 (10 y) | Whitehall II study, UK civil servants | Semi-quantitative FFQ (127 food items) (Previous years usual intake) | CES-D 20 or/and use of antidepressant medication (Depressive symptoms) |
| Chai et al. [61] USA, 2010 | Age range: >18 y Age mean: 55.3 (15.5) Gender (female): 74.1% | 139 2 y | Multiethnic sample of adults living in Hawaii | Food Frequency questions: National Cancer Institute fruit and vegetable questionnaire. (Previous months intake) | SF-12 Health Survey (SF-12) |
| Sanchez-Villegas et al. [62] Spain, 2009 | Age range at baseline: 18–104 y Age mean male: 42.7 (13.3)[64] Age mean female: 35.1 (10.7) [64] Gender (female): ~58.4% | 10,094 4.4 y | The Seguimiento Universidad de Navarra’ Study cohort, alumni of the University in Spain (SUN cohort) | Semi-quantitative FFQ (136 food items) (Usual intake) | Positive response to “Have you ever been diagnosed as having depression by a medical doctor” or/and who reported the habitual use of antidepressant drugs. (Clinical depression) |
| Ref | Exposure | Outcome | Key Results | ||
|---|---|---|---|---|---|
| Fruit and Vegetable | Fruit | Vegetable | |||
| [51] | Vegetable intake (frequency) | Mental Health (GHQ-12) | N/A | N/A | Model 2 p-trend = 0.291 Ref: Lowest quartile of exposure (Q1) OR: Q2 = 1.20 (0.95–1.50) OR: Q3 = 0.98 (0.77–1.25) OR: Q4 = 1.21 (0.95–1.55) |
| [52] | Fruit and vegetable (portions/day) | Depression/Anxiety (Doctor diagnosis) | β = −0.0041 (−0.008, −0.001) p = 0.017 ** | N/A | N/A |
| Reverse causality Diagnosed with depression/anxiety | Fruit and vegetable | β = −0.0718 (−0.174, 0.031) p = 0.170 | N/A | N/A | |
| [53] | Fruit and vegetable (portions/day) Days each week eat fruit (frequency) Days each week eat vegetables (frequency) | Well-being (GHQ-12) | Specification (3) = 0.133 *** (0.0245) | Specification (4) Ref: Never 1–3 days = 0.259 *** (0.0896) 4–6 days = 0.423 *** (0.0989) Every day = 0.613 *** (0.0982) | Specification (4) Ref: Never 1–3 days = 0.518 *** (0.171) 4–6 days = 0.803 *** (0.175) Every day = 0.925 *** (0.177) |
| [54] | Consumption of fruit and berries (frequency) | Mental Health (GHQ-12) | N/A | N/A | p-trend = 0.071 Ref: Rare consumption of fruit and berries OR: Daily consumption = 1.39 (1.05–1.84) ** OR: Weekly consumption = 1.25 (0.94–1.67) |
| [55] | Fruit and vegetables (servings/day) | Depressive symptoms (MFQ) | Model 3: β = 0.14 (−0.15, 0.43) Model 3 (male): β = 0.06 (−0.32, 0.44) Model 3 (female): β = 0.21 (−0.22, 0.64) | N/A | N/A |
| [56] | Fruit consumption (quantity/day) Vegetable consumption (quantity/day) | Depression (CES-D 10 and CES-D 20) | N/A | Model 3 (pro) In males results Ref: No fruit consumption OR: Once = 0.72 (0.46, 1.11) OR: Twice + = 0.71 (0.47, 1.07) In females results Ref: No fruit consumption OR: Once = 0.92 (0.63, 1.33) OR: Twice + = 0.73 (0.62, 1.26) | Model 3 (pro) In males results Ref: No vegetable consumption OR: Once = 1.07 (0.72, 1.57) OR: Twice + = 1.02 (0.66, 1.56) In females results Ref: No vegetable consumption OR: Once = 0.74 (0.54, 1.02) OR: Twice + = 0.80 (0.57, 1.12) |
| [57] | PNNS-GS a without Fruits and vegetables | Depressive symptoms (CES-D 20) | Excluding fruits and vegetables OR: 0.84 (0.77, 0.91) *** p = <0.0001 When adjusted for fruit and vegetable intake the PNNS-GS score remained statistically significant | N/A | N/A |
| [58] | Fruit and vegetable intake (daily frequency) Fruit and vegetable intake (daily frequency) | Depression (CIDI-SF) Distress (K6) | Model 2 (dep): β = −0.03 (−0.05 to −0.01) Model 3 (dep): β = 0.001 (−0.03 to 0.04) Model 2 (dis): β = −0.03 (−0.05 to −0.01) Model 3 (dis): β = 0.02 (−0.01 to 0.04) | N/A | N/A |
| [58] | Inverse association Depression Distress | Fruit and vegetable intake Fruit and vegetable intake | Model 2: β = −0.27 (−0.42 to −0.11) Model 3: β = −0.10 (−0.22 to 0.02) Model 2: β = −0.02 (−0.03 to −0.01) Model 3: β = 0.01 (−0.01 to 0.02) | N/A | N/A |
| [59] | Citrus fruit and Juice combined (servings/day) Citrus fruit (servings/day) Onions (servings/day) | Depression (MHI−5, antidepressant use, doctor diagnosis) | N/A | Citrus fruit and Juice combined p = <0.0001 *** Ref: Lowest quintile of exposure (Q1) HR: Q2 = 0.94 (0.85, 1.05) HR: Q3 = 0.89 (0.78, 1.02) HR: Q4 = 0.85 (0.75, 0.97) HR: Q5 = 0.82 (0.74, 0.91) Citrus fruit p = 0.001 *** Ref: Lowest quintile of exposure (Q1) HR: Q2 = 0.93 (0.88, 0.99) HR: Q3 = 0.91 (0.86, 0.96) HR: Q4 = 0.97 (0.83, 1.13) HR: Q5 = 0.87 (0.75, 1.01) | Onions p = 0.25 Ref: Lowest quintile of exposure (Q1) HR: Q2 = 1.00 (0.94, 1.06) HR: Q3 = 0.98 (0.92, 1.05) HR: Q4 = 0.96 (0.89, 1.02) HR: Q5 = 0.99 (0.89, 1.09) |
| [60] | 5−year analysis (Phase 7) Vegetable intake (servings/day) Fruit intake (servings/day) | Depressive symptoms (CES−D 20 or/and use of antidepressant medication) | N/A | OR: ~0.68 b (0.58, 0.97) (Model 3) | OR: ~0.65 b (0.51, 0.88) (Model 3) |
| [60] | 10-year analysis (Phase 9) Vegetable intake (servings/day) Fruit intake (servings/day) | Depressive symptoms (CES-D 20 or/and use of antidepressant medication) | N/A | Women’s results Ref: Those who maintained low OR: Maintaining = ~0.60 b (0.40, 1.01) OR: improving = ~0.30 b (0.25, 0.60) Ref: Those who maintained high OR: Decreasing = ~1.55 b (0.90, 3.01) (NS) | Women’s results Ref: Those who maintained low OR: Maintaining = ~0.50 b (0.30, 0.90) OR: Improving2 = ~0.45 b (0.27, 0.91) Ref: Those who maintained high OR: Decreasing = ~2.6 b (1.35, 5.35) |
| [61] | Fruit and vegetable intake (servings/day) | Quality of Life (SF-12) | MCS scores p > 0.05 at all-time points (T1–T7) Correlation co-efficient ranged from: −0.06 to 0.13 | N/A | N/A |
| [62] | Fruits and nuts (grams/day) Vegetables (grams/day) | Depression (doctor diagnosis or antidepressant use) | N/A | p trend = 0.007 *** Ref: Lowest quintile of exposure (Q1) HR: Q2 = 0.69 (0.53–0.91) HR: Q3 = 0.67 (0.51–0.88) HR: Q4 = 0.69 (0.52–0.91) HR: Q5 = 0.61 (0.45–0.82) Merged Q3–Q5: 0.67 (0.54–0.84) | P trend = 0.81 Ref: Lowest quintile of exposure (Q1)HR: Q2 = 0.88 (0.67–1.17) HR: Q3 = 0.87 (0.66–1.16) HR: Q4 = 0.94 (0.71–1.25) HR: Q5 = 0.93 (0.69–1.24) |
| Ref | Summary | Quality |
|---|---|---|
| [51] | Vegetable consumption was not associated with GHQ score before or after adjustment of confounders using prospective logistic regression. Adequate consumption of certain nutrients and foods may lead to better mental health in Japanese adults. | Good |
| [52] | Individuals who increased fruit and vegetable intake from 0 to 8 portions/day were on average 3.2% points less likely to experience depression or anxiety within the next 24 months. Fruit and vegetable consumption may help to protect against future risk of clinical depression and anxiety. There is no decisive evidence on whether the current rate of depression or anxiety predicts higher or lower fruit and vegetable consumption in the future. | Good |
| [53] | Mental well-being responds in a dose-response fashion to increases in both the quantity and the frequency of fruits and vegetables consumed. Increasing one’s consumption of fruit and vegetables by one portion (on a day where at least one portion is consumed) leads to a 0.133-unit increase in mental well-being (p < 0.01). The more often fruit and vegetables are consumed in a week, the more likely individuals have a higher mental well-being. | Good |
| [54] | Consuming fruit and berries on a daily basis were considered as a determinant for stable mental health. Having healthy food intake, demonstrated by consuming fruit and berries, was one of six determinants to predict stability in mental health. | Good |
| [55] | Fruit and vegetable consumption at age 14 years were not significantly associated with depressive symptoms at age 17 years based on based on prospective logistic regression. Diet quality was not significantly associated with depressive symptoms. | Moderate |
| [56] | Fruit and vegetable consumption could be a protective factor against adult depression. Fruit consumption among males and vegetable consumption among females were prospectively associated with a reduced risk of adult depression in unadjusted models (Model 1). The association between vegetable consumption and reduced risk of adult depression among females remained significant after adjusted for adolescent depression, but not in fully adjusted model (Model 3). | Good |
| [57] | Higher adherence to the French nutritional guideline assessed by PNNS-GS a was associated with a lower likelihood of chronic or recurrent depressive symptoms. This association was not driven by any specific component of the PNNS-GS (including Fruit and vegetables) but was a result of an overall healthy diet. | Moderate |
| [58] | A greater fruit and vegetable consumption at the initial measurement was associated with a lower risk of depression at the next. This association was evident in Model 2 adjustments however disappeared once obesity was included in the adjustment (Model 3). Similarly, a greater fruit and vegetable consumption at the initial measurement was associated with lower distress scores at the next; however, disappeared once social support smoking and physical activity were added to the model (Model 3). Inverse association showed that depression and distress at initial measurements predicted lower consumption of fruits and vegetables at the next measurement. These associations were no longer evident once social support, smoking and physical activity were added to the model. | Very Good |
| [59] | Citrus intake (fruit and juice) ≥2 servings/d was associated with an 18% reduction in depression risk. b Independently both citrus fruit and juice showed significant associations to a reduction in depression. This was true for moderate to high intakes of citrus fruit but only high intakes of juice. Onion intake was not associated with depression risk. Diet higher in flavonoids results in a moderate reduction in risk of depression- especially in older women. | Good |
| [60] | High consumption of fruits and vegetables was associated with lower odds of recurrent depression. Improvement in fruit and vegetable score led to lower odds of subsequent depressive symptoms compared to those who maintained low scores. Decrease in AHEI a score led to higher odds of depression in vegetables but not fruit. Improvement in fruit and vegetable score led to lower odds of subsequent depressive symptoms compared to those who maintained low scores. Decrease in AHEI score led to higher odds of depression in vegetables but not fruit. | Good |
| [61] | There was no significant association between MCS score and daily fruit and vegetable consumption. Increasing weekly physical activity levels was significantly associated with increasing MCS at all time points. Physical activity predictive of positive mental health irrespective of other behaviours such as fruit and vegetable intake and TV/video watching | Moderate |
| [62] | Greater adherence to the Mediterranean dietary pattern a resulted in more than a 30% reduction in depression development. Compared to participants with the lowest consumption fruit and nut those with the highest intake had a 39% decreased risk of developing depression. There was no significant association between vegetable intake and depression. Compared to participants with lowest consumption of legumes those with highest intake had a 27% decreased risk of developing depression. | Good |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dharmayani, P.N.A.; Juergens, M.; Allman-Farinelli, M.; Mihrshahi, S. Association between Fruit and Vegetable Consumption and Depression Symptoms in Young People and Adults Aged 15–45: A Systematic Review of Cohort Studies. Int. J. Environ. Res. Public Health 2021, 18, 780. https://doi.org/10.3390/ijerph18020780
Dharmayani PNA, Juergens M, Allman-Farinelli M, Mihrshahi S. Association between Fruit and Vegetable Consumption and Depression Symptoms in Young People and Adults Aged 15–45: A Systematic Review of Cohort Studies. International Journal of Environmental Research and Public Health. 2021; 18(2):780. https://doi.org/10.3390/ijerph18020780
Chicago/Turabian StyleDharmayani, Putu Novi Arfirsta, Melissa Juergens, Margaret Allman-Farinelli, and Seema Mihrshahi. 2021. "Association between Fruit and Vegetable Consumption and Depression Symptoms in Young People and Adults Aged 15–45: A Systematic Review of Cohort Studies" International Journal of Environmental Research and Public Health 18, no. 2: 780. https://doi.org/10.3390/ijerph18020780
APA StyleDharmayani, P. N. A., Juergens, M., Allman-Farinelli, M., & Mihrshahi, S. (2021). Association between Fruit and Vegetable Consumption and Depression Symptoms in Young People and Adults Aged 15–45: A Systematic Review of Cohort Studies. International Journal of Environmental Research and Public Health, 18(2), 780. https://doi.org/10.3390/ijerph18020780








