Swallowing Function Evaluation in a Patient with Gerstmann-Sträussler-Scheinker Disease with Pro105Leu: A Case Report
Abstract
:1. Introduction
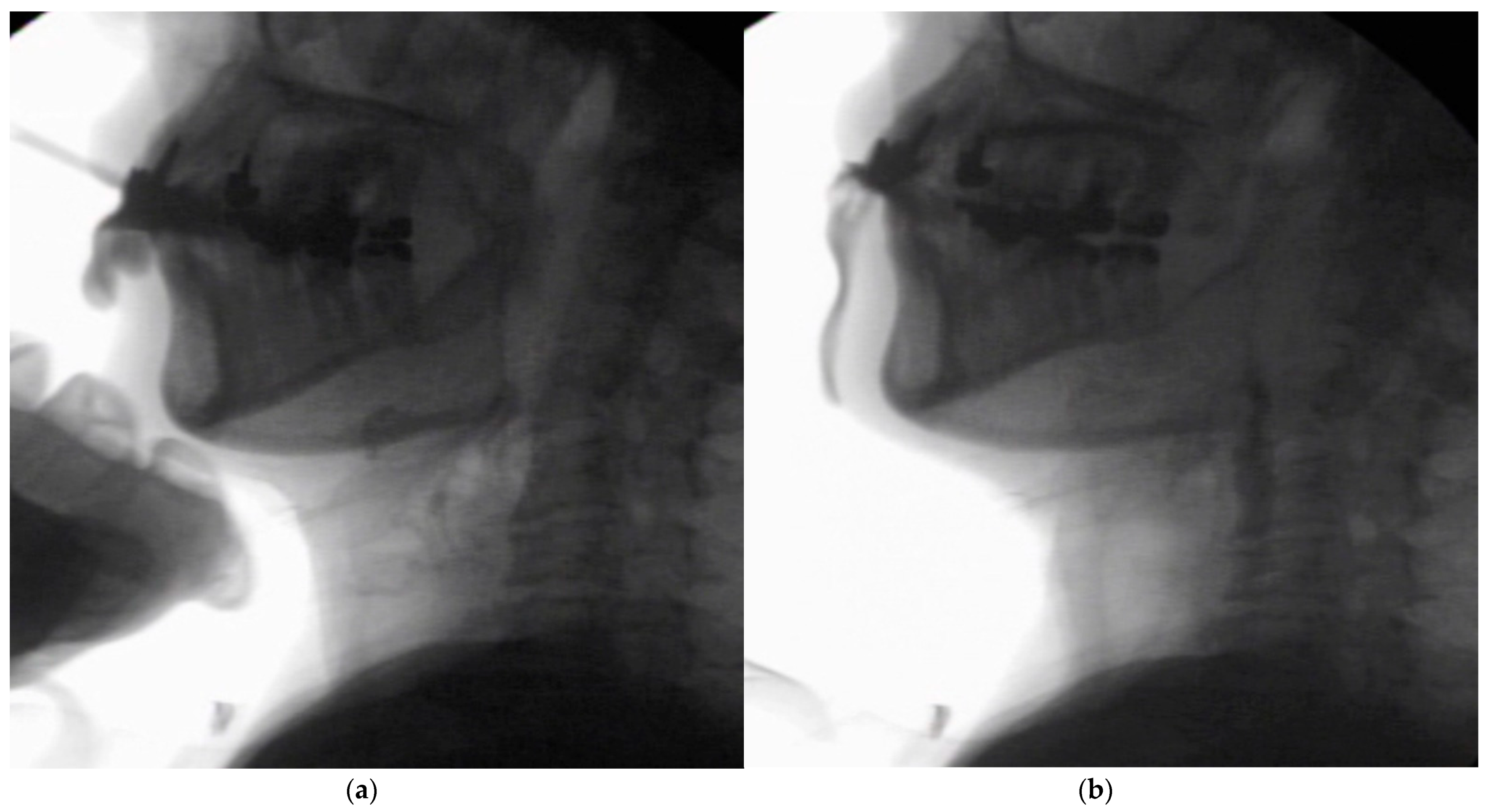
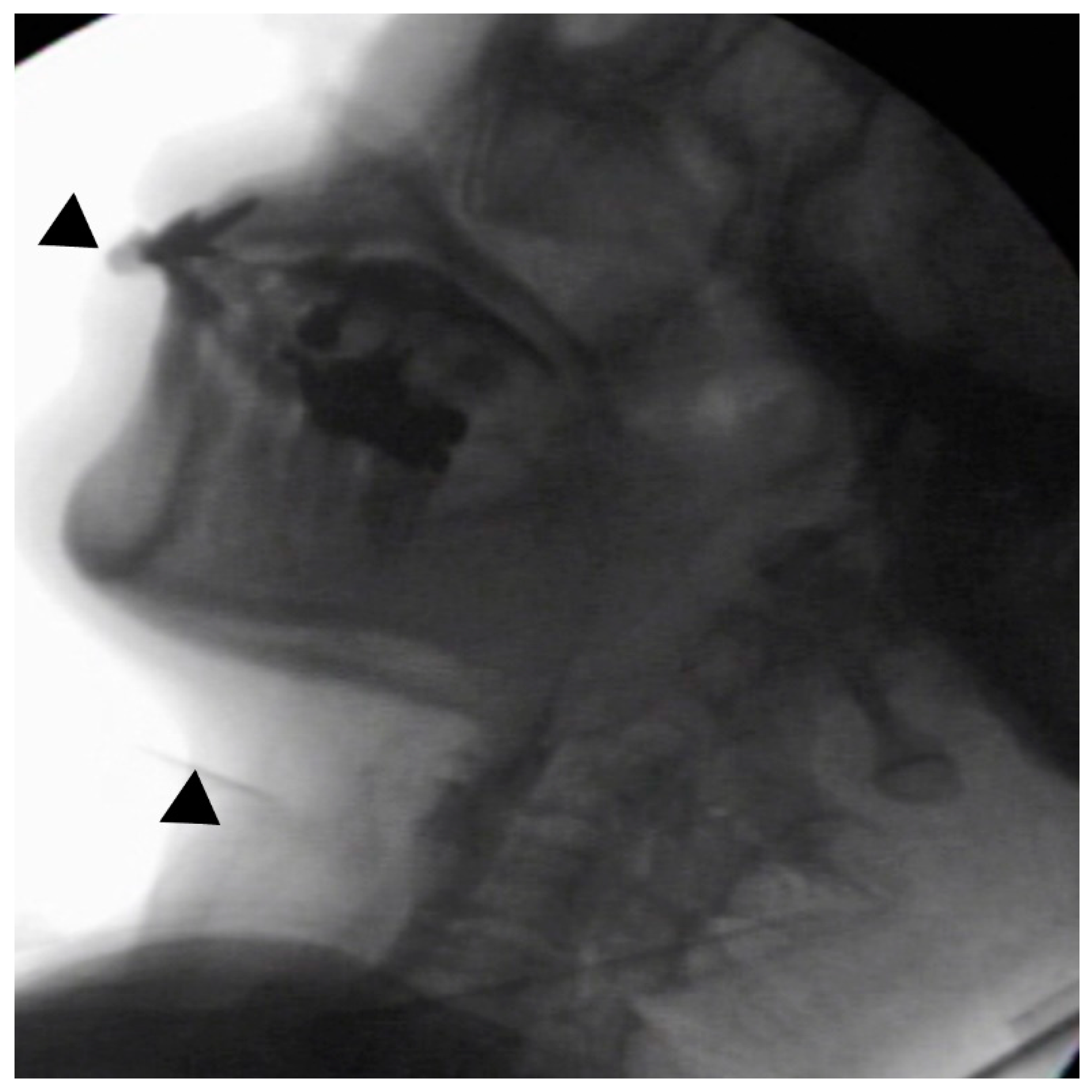
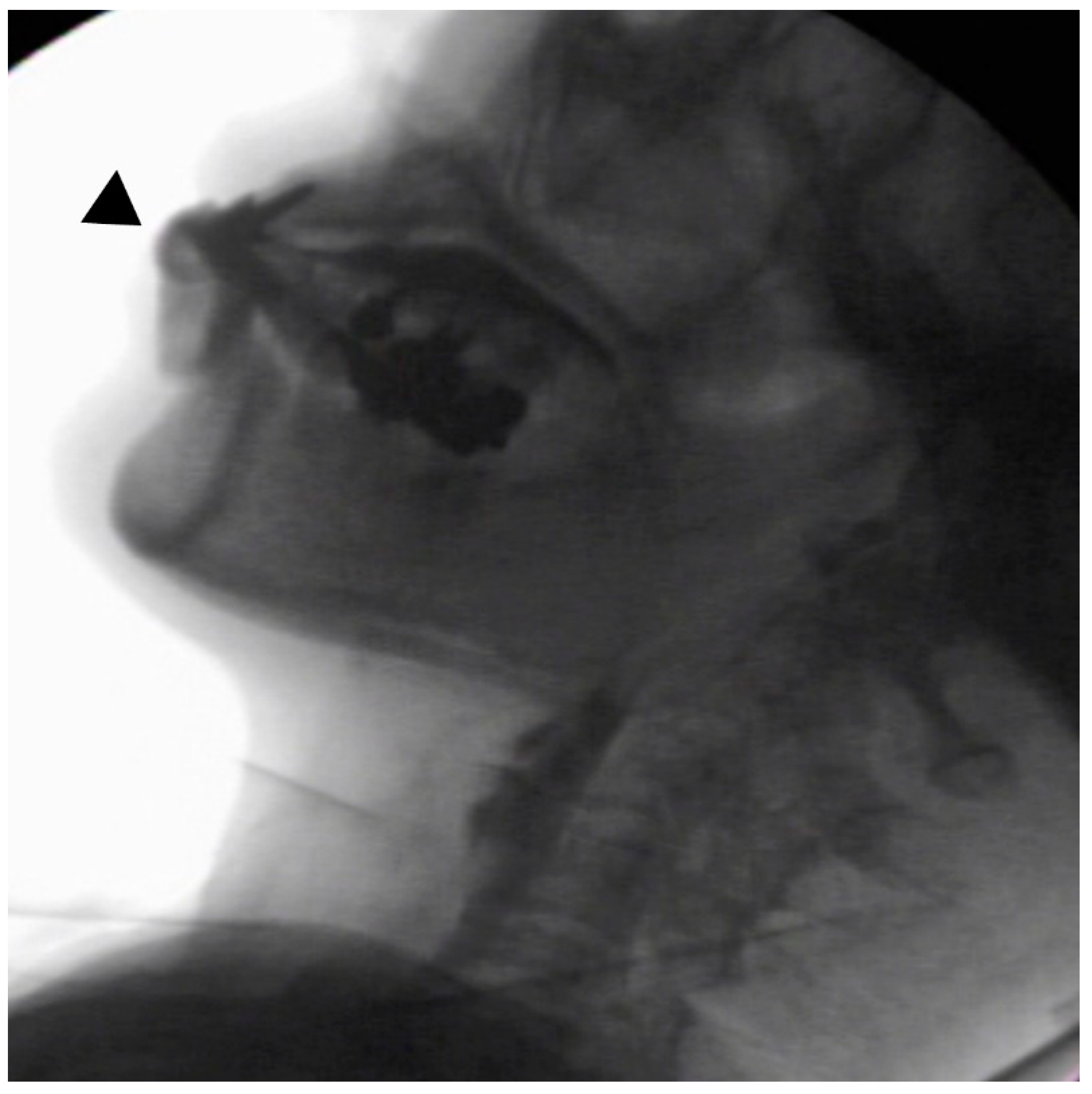
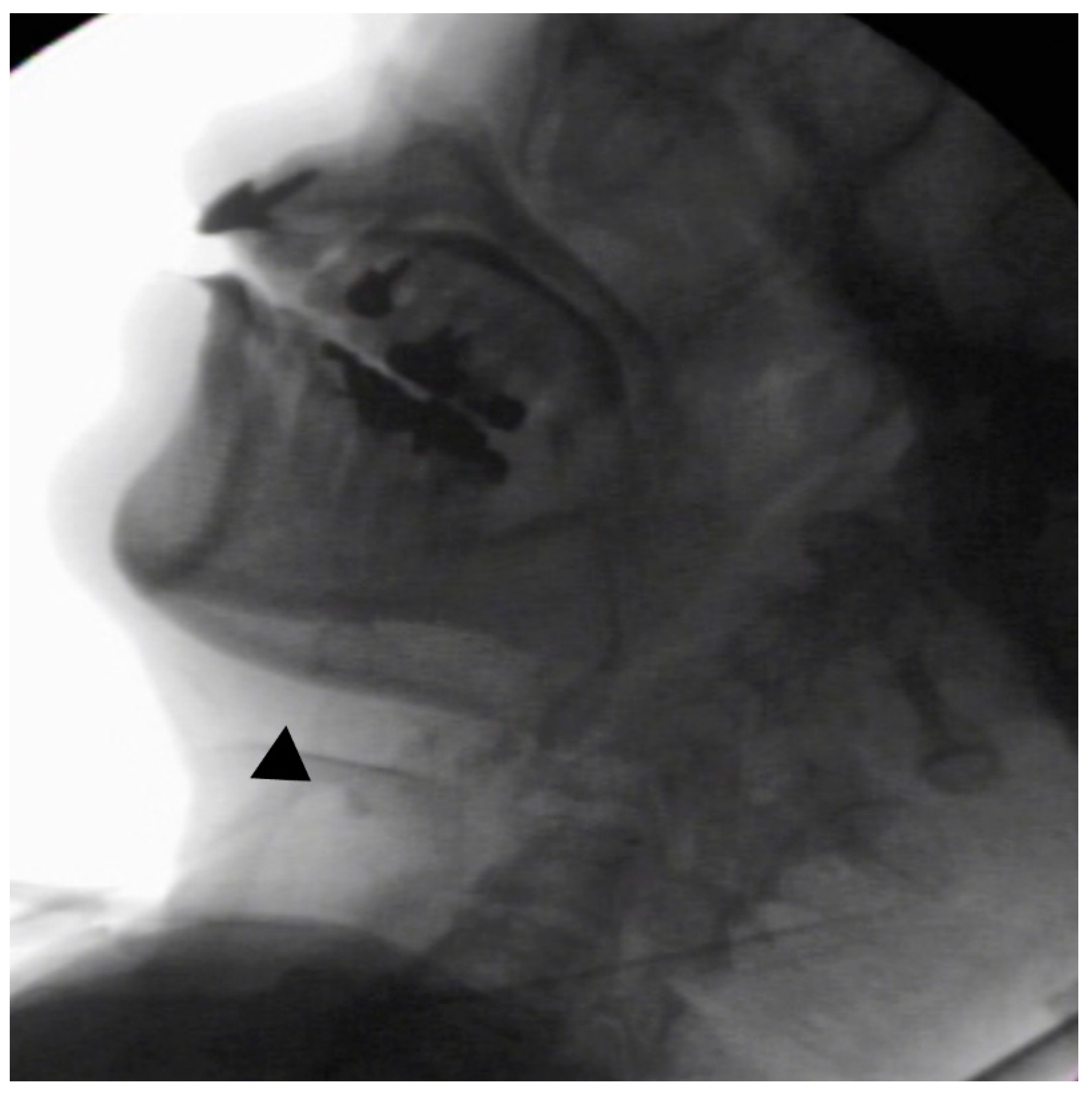
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Mano, K.K.; Matsukawa, T.; Mitsui, J.; Ishiura, H.; Tokushige, S.I.; Takahashi, Y.; Sato, N.S.; Nakamoto, F.K.; Ichikawa, Y.; Nagashima, Y.; et al. Atypical parkinsonism caused by Pro105Leu mutation of prion protein. Neurol. Genet. 2016, 2, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iwasaki, Y.; Kizawa, M.; Hori, N.; Kitamoto, T.; Sobue, G. A case of Gerstmann-Sträussler-Scheinker syndrome with the P105L prion protein gene mutation presenting with ataxia and extrapyramidal signs without spastic paraparesis. Clin. Neurol. Neurosurg. 2009, 111, 606–609. [Google Scholar] [CrossRef] [PubMed]
- 2020 Ministry of Health, Labour and Welfare, Japan. Health, Labour, and Welfare Policy Research Grants. Research Program on Rare and Intractable Diseases. Research Group on Surveillance and Infection Control of Prion Disease/Japanese Society of Neurology. Available online: http://prion.umin.jp/guideline/cjd_2020.pdf (accessed on 15 September 2021). (In Japanese).
- Beck, J.A.; Poulter, M.; Campbell, T.A.; Adamson, G.; Uphill, J.B.; Guerreiro, R.; Jackson, G.S.; Stevens, J.C.; Manji, H.; Collinge, J.; et al. PRNP allelic series from 19 years of prion protein gene sequencing at the MRC prion unit. Hum. Mutat. 2010, 31, E1551–E1563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Logemann, J.A. Manual for the Videofluorographic Study of Swallowing, 2nd ed.; Pro-ed: Austin, TX, USA, 1993. [Google Scholar]
- Kunieda, K.; Ohno, T.; Fujishima, I.; Hojo, K.; Morita, T. Reliability and validity of a tool to measure the severity of dysphagia: The food intake LEVEL scale. J. Pain Sympt. Manag. 2013, 46, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Wakasugi, Y.; Yamamoto, T.; Oda, C.; Murata, M.; Tohara, H.; Minakuchi, S. Effect of an impaired oral stage on swallowing in patients with Parkinson’s disease. J. Oral Rehabil. 2017, 44, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, M.; Yoshida, M.; Nagasaki, T.; Tanimoto, K.; Tsuga, K.; Akagawa, Y.; Komatsu, T. Aspects of swallowing in healthy dentate elderly persons older than 80 years. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 506–509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dos Santos, C.M.; Cassiani, R.A.; Dantas, R.O. Videofluoroscopic evaluation of swallowing in Chagas’ disease. Dysphagia 2011, 26, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Cassiani, R.A.; Santos, C.M.; Parreria, L.C.; Dantas, R.O. The relationship between the oral and pharyngeal phases of swallowing. Clinics 2011, 66, 1385–1388. [Google Scholar] [CrossRef] [PubMed]
- Dantas, R.O.; de Aguiar Cassiani, R.; Dos Santos, C.M.; Gonzaga, G.C.; Alves, L.M.; Mazin, S.C. Effect of gender on swallow event duration assessed by videofluoroscopy. Dysphagia 2009, 24, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, Y.; Kunieda, K.; Kudo, T.; Kimura, A.; Fujishima, I.; Shimohata, T. Long-term preservation of pharyngeal swallowing function in MM2-cortical-type sporadic Creutzfeldt-Jakob disease. Prion 2021, 15, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Kunieda, K.; Hayashi, Y.; Yamada, M.; Waza, M.; Yaguchi, T.; Fujishima, I.; Shimohata, T. Serial evaluation of swallowing function in a long-term survivor of V180I genetic Creutzfeldt-Jakob disease. Prion 2020, 14, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Oba, N.; Fujimoto, Y.; Hirata, K.; Ando, N.; Saida, K. A case of Gerstmann-Sträussler-Scheinker disease with severe muscular atrophy and vertical gaze palsy. Rinsho Shinkeigaku 2000, 40, 726–731. (In Japanese) [Google Scholar] [PubMed]
- Kubo, M.; Nishimura, T.; Shikata, E.; Kokubun, Y.; Takasu, T. A case of variant Gerstmann-Sträussler-Scheinker disease with the mutation of codon P105L. Rinsho Shinkeigaku 1995, 35, 873–877. (In Japanese) [Google Scholar]
- Yamazaki, M.; Oyanagi, K.; Mori, O.; Kitamura, S.; Ohyama, M.; Terashi, A.; Kitamoto, T.; Katayama, Y. Variant Gerstmann-Straussler syndrome with the P105L prion gene mutation: An unusual case with nigral degeneration and widespread neurofibrillary tangles. Acta Neuropathol. 1999, 98, 506–511. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, F.; Sanjo, N.; Kobayashi, A.; Hamaguchi, T.; Yamada, M.; Kitamoto, T.; Mizusawa, H.; Yokota, T. Specific amyloid-β42 deposition in the brain of a Gerstmann-Sträussler-Scheinker disease patient with a P105L mutation on the prion protein gene. Prion 2018, 12, 315–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leopold, N.A.; Kagel, M.C. Swallowing, Ingestion and Dysphagia: A Reappraisal. Arch. Phys. Med. Rehabil. 1938, 64, 371–373. [Google Scholar]
- Japanese Dysphagia Diet 2013 by the JSDR Dysphagia Diet Committee (JDD2013). Available online: https://www.jsdr.or.jp/wp-content/uploads/file/doc/classification2013-manual.pdf (accessed on 15 September 2021).
| Case | Author | Participants | Age | Sex | Test Food | Volumes (mL) | OTT(s) | PDT(s) | PTT(s) | PC(s) | UOD(s) | OT(s) | STD(s) | DHM(s) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Current patient | 67 | female | paste | 5 | 20.25 | 0.1 | 0.43 | 6.91 | 0.27 | 20.42 | 6.67 | 0.47 | |
| 2 | Wakasugi [7] | Healthy elderly | 70.3 ± 7.8 | 13 males, 7 females | liquids | 10 | 0.89 ± 0.46 | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. |
| 3 | Santos [9] | Healthy volunteer | 55.2 (35–69) | 8 males, 7 females | paste | 5 | 0.72 ± 0.73 | N.D. | 0.38 ± 0.08 | 0.64 ± 0.22 | 0.35 ± 0.09 | 0.94 ± 0.49 | 0.07 ± 0.21 | 0.69 ± 0.26 |
| 4 | Cassani [10] | Healthy volunteer | 58 (29–77) | 18 males, 12 females | paste | 5 | 0.41 ± 0.28 | N.D. | 0.23 ± 0.07 | 0.48 ± 0.27 | N.D. | N.D. | N.D. | N.D. |
| 5 | Dantas [11] | Volunteers | 61 (33–77) | 8 males | paste | 5 | 0.39 ± 0.28 | N.D. | 0.22 ± 0.07 | 0.42 ± 0.25 | 0.2 ± 0.04 | 0.64 ± 0.35 | N.D. | N.D. |
| 53 (29–72) | 7 females | paste | 5 | 0.59 ± 0.42 | N.D. | 0.25 ± 0.07 | 0.56 ± 0.27 | 0.22 ± 0.07 | 0.94 ± 0.58 | N.D. | N.D. | |||
| 6 | Yoshiakawa [8] | Dantate elderly | 81.2 (80–87) | 12 males, 7 females | liquids | 10 | 1.05 ± 0.31 | 0.16 ± 0.14 | 0.7 ± 0.15 | N.D. | N.D. | N.D. | N.D. | N.D. |
| Case | Author | Participants | Onset of Age | Sex | Duration of Onset | FILS Level | Nutrition Intake | Meal | Position | Test Food | Bolus Transport | PC(s) | OT(s) | STD(s) | Pharyngeal Swallow | Aspiration |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Current patient | GSS p105L | 54 | F | 156 M | 7 | oral | assistance | sitting | 5 mL of extremely thick paste | poor | 6.91 | 20.42 | 6.67 | delayed | non |
| assistance | reclining | 〃 | poor | 2.47 | 5.67 | 2.3 | not delay | non | ||||||||
| assistance | reclining | 5 mL of moderately thick paste | poor | 7.68 | 9.74 | 8.48 | delayed | Aspiration | ||||||||
| 2 | Hayashi [12] | MM2C-type sCJD | 52 | F | 58 | 8 | oral | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. |
| 68 | 3 | oral | N.D. | N.D. | N.D. | poor | N.D. | N.D. | N.D. | preserved | non | |||||
| N.D. | 4 | oral, gastrostomy | assistance | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |||||
| 3 | Kunieda [13] | gCJD v1801 | 69 | F | 12 M | 8 | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. |
| 27 M | N.D. | oral | N.D. | sitting | Jelly, liquid, chopped food | slightly poor | N.D. | N.D. | N.D. | not delay | N.D. | |||||
| 31 M–39 M | N.D. | N.D. | 〃 | N.D. | slightly worse | N.D. | N.D. | N.D. | delayed | N.D. | ||||||
| 42 M | 5 | oral, gastrostomy | assistance | N.D. | easy to swallow food | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |||||
| 79 M | N.D. | oral, gastrostomy | assistance | reclining | N.D. | poor | N.D. | N.D. | N.D. | more delayed | non |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakane, A.; Hasegawa, S.; Ishii, M.; Tamai, T.; Moritoyo, R.; Saito, M.; Ando, M.; Tohara, H. Swallowing Function Evaluation in a Patient with Gerstmann-Sträussler-Scheinker Disease with Pro105Leu: A Case Report. Int. J. Environ. Res. Public Health 2021, 18, 9734. https://doi.org/10.3390/ijerph18189734
Nakane A, Hasegawa S, Ishii M, Tamai T, Moritoyo R, Saito M, Ando M, Tohara H. Swallowing Function Evaluation in a Patient with Gerstmann-Sträussler-Scheinker Disease with Pro105Leu: A Case Report. International Journal of Environmental Research and Public Health. 2021; 18(18):9734. https://doi.org/10.3390/ijerph18189734
Chicago/Turabian StyleNakane, Ayako, Shohei Hasegawa, Miki Ishii, Tomoe Tamai, Rieko Moritoyo, Mitsuko Saito, Mariko Ando, and Haruka Tohara. 2021. "Swallowing Function Evaluation in a Patient with Gerstmann-Sträussler-Scheinker Disease with Pro105Leu: A Case Report" International Journal of Environmental Research and Public Health 18, no. 18: 9734. https://doi.org/10.3390/ijerph18189734






