Assessing the Quality of Life of Oral Submucous Fibrosis Patients: A Cross-Sectional Study Using the WHOQOL-BREF Tool
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Inclusion and Exclusion Criteria
2.2. Data Collection Procedure
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| QoL | Quality of Life |
| OSMF | Oral Submucous Fibrosis |
| WHOQOL-BREF | World Health Organization Quality of Life-BREF |
| LUMHS | Liaquat University of Medical and Health Sciences |
| HPV | Human Papilloma Virus |
| WHO | World Health Organization |
| OIDP | Oral Impacts on Daily Performances |
| OHIP | Oral Health Impact Profile |
| UWQOL | University of Washington Quality of Life Questionnaire |
| COMDQ | Chronic Oral Mucosal Disease Questionnaire |
| OHQoL-UK | Oral Health Related Quality of Life-UK |
| OHRQoL | Oral Health Related Quality of Life |
| SPSS | Statistical Package for Social Sciences |
| SD | Standard Deviation |
| DOM | Domain |
| LMO | Limited Mouth Opening |
References
- Bari, S.; Metgud, R.; Vyas, Z.; Tak, A. An update on studies on etiological factors, disease progression, and malignant transformation in oral submucous fibrosis. J. Cancer Res. Ther. 2017, 13, 399–405. [Google Scholar]
- Gadbail, A.; Dande, R.; Sarode, S.C.; Gondivkar, S.; Belekar, L.; Mankar-Gadbail, M.; Sarode, G.S.; Patil, S.; Yuwanati, M. Patients with oral submucous fibrosis who visit dental hospitals have nonspecific chief complaints. Transl. Res. Oral Oncol. 2019, 24. [Google Scholar] [CrossRef]
- Kumar, L.B.; Mathew, P.; Madhavan, N.; Siddique, S.; Kshetrimayum, N.; Iyer, K. Evaluation of mast cells and burning sensation in various stages of Oral Submucous Fibrosis. J. Oral Biol. Craniofacial Res. 2020, 10, 430–434. [Google Scholar] [CrossRef]
- Shen, Y.-W.; Shih, Y.-H.; Fuh, L.-J.; Shieh, T.-M. Oral Submucous Fibrosis: A Review on Biomarkers, Pathogenic Mechanisms, and Treatments. Int. J. Mol. Sci. 2020, 21, 7231. [Google Scholar] [CrossRef] [PubMed]
- Gondivkar, S.M.; Bhowate, R.R.; Gadbail, A.R.; Gaikwad, R.N.; Gondivkar, R.S.; Sarode, S.C.; Sarode, G.S. Development and validation of oral health-related quality of life measure in oral submucous fibrosis. Oral Dis. 2018, 24, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Aswath, N.; Balakrishnan, C. Estimation of serum, salivary immunoglobulin G, immunoglobulin A levels and total protein, hemoglobin in smokeless tobacco chewers and oral submucous fibrosis patients. Contemp. Clin. Dent. 2015, 6, S157–S162. [Google Scholar] [CrossRef] [PubMed]
- Arakeri, G.; Rai, K.K.; Hunasgi, S.; Merkx, M.A.W.; Gao, S.; Brennan, P.A. Oral submucous fibrosis: An update on current theories of pathogenesis. J. Oral Pathol. Med. 2017, 46, 406–412. [Google Scholar] [CrossRef]
- Guruprasad, R.; Nair, P.P.; Singh, M.; Singh, M.; Singh, M.; Jain, A. Serum vitamin c and iron levels in oral submucous fibrosis. Indian J. Dent. 2014, 5, 81–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.-P.; Wu, Y.-C.; Cheng, S.-J.; Chen, H.-M.; Sun, A.; Chang, J.Y.-F. High frequencies of vitamin B12 and folic acid deficiencies and gastric parietal cell antibody positivity in oral submucous fibrosis patients. J. Formos. Med. Assoc. 2015, 114, 813–819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teh, M.T.; Tilakaratne, W.M.; Chaplin, T.; Young, B.D.; Ariyawardana, A.; Pitiyage, G.; Lalli, A.; Stewart, J.E.; Hagi-Pavli, E.; Cruchley, A.; et al. Fingerprinting genomic instability in oral submucous fibrosis. J. Oral Pathol. Med. 2008, 37, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Tilakaratne, W.M.; Klinikowski, M.F.; Saku, T.; Peters, T.J.; Warnakulasuriya, S. Oral submucous fibrosis: Review on aetiology and pathogenesis. Oral Oncol. 2006, 42, 561–568. [Google Scholar] [CrossRef]
- Chang, M.C.; Chiang, C.P.; Lin, C.L.; Lee, J.-J.; Hahn, L.J.; Jeng, J.H. Cell-mediated immunity and head and neck cancer: With special emphasis on betel quid chewing habit. Oral Oncol. 2005, 41, 757–775. [Google Scholar] [CrossRef]
- Cox, S.C.; Walker, D.M. Oral submucous fibrosis. A review. Aust. Dent. J. 1996, 41, 294–299. [Google Scholar] [CrossRef]
- Ilić, I.; Šipetić, S.; Grujičić, J.; Mačužić, I.Ž.; Kocić, S.; Ilić, M. Psychometric Properties of the World Health Organization’s Quality of Life (WHOQOL-BREF) Questionnaire in Medical Students. Medicina 2019, 55, 772. [Google Scholar] [CrossRef] [Green Version]
- Chiu, C.-J.; Chang, M.-L.; Chiang, C.-P.; Hahn, L.-J.; Hsieh, L.-L.; Chen, C.-J. Interaction of collagen-related genes and susceptibility to betel quid-induced oral submucous fibrosis. Cancer Epidemiol. Biomark. Prev. 2002, 11, 646–653. [Google Scholar]
- Shih, Y.-H.; Wang, T.-H.; Shieh, T.-M.; Tseng, Y.-H. Oral Submucous Fibrosis: A Review on Etiopathogenesis, Diagnosis, and Therapy. Int. J. Mol. Sci. 2019, 20, 2940. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tadakamadla, J.; Kumar, S.; Johnson, N.W. Quality of life in patients with oral potentially malignant disorders: A systematic review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 644–655. [Google Scholar] [CrossRef]
- Szabo, S. The world health organisation quality of life (WHOQOL) assessment instrument. In Quality of Life and Pharmaeconomics in Clinical Trials, 2nd ed.; Spilker, B., Ed.; Lippincott-Raven Publishers: Philadelphia, PA, USA, 1996. [Google Scholar]
- Eriksson, M.; Lindström, B. Antonovsky’s sense of coherence scale and its relation with quality of life: A systematic review. J. Epidemiol. Community Heath 2007, 61, 938–944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fayers, P.M.; Machin, D. 5 Multi-item scales. In Quality of Life: The Assessment, Analysis and Interpretation of Patient-Reported Outcomes, 2nd ed.; John Wiley & Sons, Ltd: Hoboken, NJ, USA, 2007; pp. 109–130. [Google Scholar]
- The Whoqol Group Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol. Med. 1998, 28, 551–558. [CrossRef] [PubMed] [Green Version]
- Tesch, F.C.; Oliveira, B.H.; Leao, A. Measuring the impact of oral health problems on hildren’s quality of life: Conceptual and methodological issues. Cad. Saude Publica 2007, 23, 2555–2564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomes, A.S.; Abegg, C. The impact of oral health on daily performance of municipal waste disposal workers in Porto Alegre, Rio Grande do, Sul State, Brazil. Cad. Saude Publica 2007, 23, 1707–1714. [Google Scholar] [CrossRef] [Green Version]
- Benyamini, Y.; Leventhal, H.; Leventhal, E.A. Self-rated oral health as an independent predictor of self-rated general health, self-esteem and life satisfaction. Soc. Sci. Med. 2004, 59, 1109–1116. [Google Scholar] [CrossRef] [PubMed]
- Cruz, L.N.; Polanczyk, C.A.; Camey, S.A.; Hoffmann, J.F.; Fleck, M.P. Quality of life in Brazil: Normative values for the WHOQOL-bref in a southern general population sample. Qual. Life Res. 2011, 20, 1123–1129. [Google Scholar] [CrossRef] [PubMed]
- Nedjat, S.; Holakouie Naieni, K.; Mohammad, K.; Majdzadeh, R.; Montazeri, A. Quality of life among an Iranian general population sample using the World Health Organization’s quality of life instrument (WHOQOL-BREF). Int. J. Public Health 2010, 56, 55–61. [Google Scholar] [CrossRef]
- McNeil, D.W.; Rainwater, A.J. Development of the Fear of Pain Questionnaire-III. J. Behav. Med. 1998, 21, 389–410. [Google Scholar] [CrossRef]
- Saxena, S.; Carlson, D.; Billington, R.; Orley, J. The WHO quality of life assessment instrument (WHOQOL-Bref): The importance of its items for cross-cultural research. Qual. Life Res. 2001, 10, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Hawthorne, G.; Herrman, H.; Murphy, B. Interpreting the WHOQOL-Brèf: Preliminary Population Norms and Effect Sizes. Soc. Indic. Res. 2006, 77, 37–59. [Google Scholar] [CrossRef]
- World Health Organization. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment: Field Trial Version, December 1996; World Health Organization: Geneva, Switzerland, 1996. [Google Scholar]
- Saqib Lodhi, F.; Raza, O.; Montazeri, A.; Nedjat, S.; Yaseri, M.; Holakouie-Naieni, K. Psychometric properties of the Urdu version of the World Health Organization’s quality of life questionnaire (WHOQOL-BREF). Med. J. Islam. Repub. Iran 2017, 31, 129. [Google Scholar] [CrossRef] [Green Version]
- Pagnin, D.; Queiroz, V. Influence of burnout and sleep difficulties on the quality of life among medical students. SpringerPlus 2015, 4, 676. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Qu, B.; Lun, S.; Wang, D.; Guo, Y.; Liu, J. Quality of Life of Medical Students in China: A Study Using the WHOQOL-BREF. PLoS ONE 2012, 7, e49714. [Google Scholar] [CrossRef]
- Suliman, N.M.; Johannessen, A.C.; Ali, R.W.; Salman, H.; Åstrøm, A.N. Influence of oral mucosal lesions and oral symptoms on oral health related quality of life in dermatological patients: A cross sectional study in Sudan. BMC Oral Health 2012, 12, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaudhry, K.; Bali, R.; Patnana, A.K.; Bindra, S.; Jain, G.; Sharma, P.P. Impact of Oral Submucous Fibrosis on Quality of Life: A Cross-Sectional Study. J. Maxillofac. Oral Surg. 2019, 18, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, K.; Bali, R.; Patnana, A.K.; Chattopadhyay, C.; Sharma, P.P.; Khatana, S. Impact of Oral Submucous Fibrosis on Quality of Life: A Multifactorial Assessment. J. Maxillofac. Oral Surg. 2020, 19, 251–256. [Google Scholar] [CrossRef] [PubMed]
- The World Health Organization Quality of Life Group. The World Health Organization Quality of Life Assessment (WHOQOL-BREF): Introduction, Administration, Scoring and Generic Version of the Assessment; Programme on Mental Health: Geneva, Switzerland, 1996. [Google Scholar]
- Dijkstra, P.U.; Bont, L.G.M.; Stegnenga, B.; Boering, G. Angle of mouth opening measurement: Reliability of a technique for temporomandibular joint mobility assessment. J. Oral Rehabil. 1995, 22, 263. [Google Scholar] [CrossRef]
- More, C.B.; Das, S.; Patel, H.; Adalja, C.; Kamatchi, V.; Venkatesh, R. Proposed clinical classification for oral submucous fibrosis. Oral Oncol. 2012, 48, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, S.; Faulk, J.; Blakey, G.H.; Phillips, C.; Phero, J.A.; White, R.P. Quality of Life Outcomes After Third Molar Removal in Subjects with Minor Symptoms of Pericoronitis. J. Oral Maxillofac. Surg. 2012, 70, 2494–2500. [Google Scholar] [CrossRef] [PubMed]
- Kieffer, J.M.; van Wijk, A.J.; Ho, J.P.; Lindeboom, J.A.H. The internal responsiveness of the Oral Health Impact Profile-14 to detect differences in clinical parameters related to surgical third molar removal. Qual. Life Res. 2012, 21, 1241–1247. [Google Scholar] [CrossRef] [Green Version]
- Jaroń, A.; Preuss, O.; Konkol, B.; Trybek, G. Quality of Life of Patients after Kinesio Tape Applications Following Impacted Mandibular Third Molar Surgeries. J. Clin. Med. 2021, 10, 2197. [Google Scholar] [CrossRef] [PubMed]
- Skevington, S.; Lotfy, M.; O’Connell, K. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A Report from the WHOQOL Group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef]
- Akpa, O.; Fowobaje, K. The Factor Structure of the Adapted WHO Quality of Life BREF questionnaire in a sample of adolescents in Nigeria. Arch. Basic Appl. Med. 2018, 6, 35–44. [Google Scholar]
- Baiano, M.; Salvo, P.; Righetti, P.; Cereser, L.; Baldissera, E.; Camponogara, I.; Balestrieri, M. Exploring health-related quality of life in eating disorders by a cross-sectional study and a comprehensive review. BMC Psychiatry 2014, 14, 165. [Google Scholar] [CrossRef] [Green Version]
- Berlim, M.T.; Pavanello, D.P.; Caldieraro, M.A.; Fleck, M.P.A. Reliability and validity of the WHOQOL BREF in a sample of Brazilian outpatients with major depression. Qual. Life Res. 2005, 14, 561–564. [Google Scholar] [CrossRef]
- Bennadi, D.; Reddy, C.V. Oral health related quality of life. J. Int Soc. Prev. Community Dent. 2013, 3, 1–6. [Google Scholar] [CrossRef]
- Kularatna, S.; Whitty, J.A.; Johnson, N.W.; Jayasinghe, R.; Scuffham, P.A. A comparison of health state utility values associated with oral potentially malignant disorders and oral cancer in Sri Lanka assessed using the EQ-5D-3 L and the EORTC-8D. Health Qual. Life Outcomes 2016, 14, 101. [Google Scholar] [CrossRef] [Green Version]
- Tadakamadla, J.; Kumar, S.; Lalloo, R.; Gandhi Babu, D.B.; Johnson, N. Impact of oral potentially malignant disorders on quality of life. J. Oral Pathol. Med. 2017, 47, 60–65. [Google Scholar] [CrossRef] [Green Version]
- Rimal, J.; Shrestha, A. Validation of Nepalese Oral Health Impact Profile14 and Assessment of Its Impact in Patients with Oral Submucous Fibrosis in Nepal. J. Nepal Health Res. Counc. 2015, 13, 43–49. [Google Scholar]
- Chitguppi, C.; Brar, T. Paediatric oral submucous fibrosis—The neglected pre-malignancy of childhood. Int. J. Pediatr. Otorhinolaryngol. 2017, 97, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Sinor, P.N.; Gupta, P.C.; Murti, P.R.; Bhonsle, R.B.; Daftary, D.K.; Mehta, F.S.; Pindborg, J.J. A case-control study of oral submucous fibrosis with special reference to the etiologic role of areca nut. J. Oral Pathol. Med. 1990, 19, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S. Oral submucous fibrosis: A demographic study. J. Indian Acad. Oral Med. Radiol. 2016, 28, 124. [Google Scholar] [CrossRef]
- Hazarey, V.K.; Erlewad, D.M.; Mundhe, K.A.; Ughade, S.N. Oral submucous fibrosis: Study of 1000 cases from central India. J. Oral Pathol. Med. 2006, 36, 12–17. [Google Scholar] [CrossRef]
- Sahmadhavi, N.; Raju, M.A.; Reddy, R.; Ramesh, T.; Tabassum, D.; Ramya, K. Impact of oral diseases on quality of life insubjects attending out-patient department of a dental hospital, India. J. Orofac. Sci. 2013, 5, 27–31. [Google Scholar] [CrossRef]
- Caglayan, F.; Altun, O.; Miloglu, O.; Kaya, M.-D.; Yilmaz, A.-B. Correlation between oral health-related quality of life (OHQoL) and oral disorders in a Turkish patient population. Medicina Oral Patología Oral Cirugia Bucal 2009, 14, e573–e578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rao, T.S.; Nagaraj, A.K.M. Female sexuality. Indian J. Psychiatry 2015, 57, S296–S302. [Google Scholar] [PubMed]
- Koenig, A.M. Comparing Prescriptive and Descriptive Gender Stereotypes About Children, Adults, and the Elderly. Front. Psychol. 2018, 9, 1086. [Google Scholar] [CrossRef]
- Rajendran, R. Oral submucous fibrosis: Etiology, pathogenesis, and future research. Bull. World Health Organ. 1994, 72, 985–996. [Google Scholar] [PubMed]
- Murti, P.R.; Bhonsle, R.B.; Gupta, P.C.; Daftary, D.K.; Pindborg, J.J.; Mehta, F.S. Etiology of oral submucous fibrosis with special reference to the role of areca nut chewing. J. Oral Pathol. Med. 1995, 24, 145–152. [Google Scholar] [CrossRef]
- Babu, S.; Venkataramana Bhat, R.; Uday Kumar, P.; Sesikaran, B.; Visweswara Rao, K.; Aruna, P.; Ramachandra Reddy, P.R. A comparative clinicopathological study of oral submucous fibrosis in habitualchewers of pan masala and betel quid. Clin. Toxicol. 1996, 34, 317–322. [Google Scholar]
- Tadakamadla, J.; Kumar, S.; Lalloo, R.; Johnson, N.W. Qualitative analysis of the impact of Oral Potentially Malignant Disorders on daily life activities. PLoS ONE 2017, 12, e0175531. [Google Scholar] [CrossRef] [Green Version]
- Lodhi, F.S.; Montazeri, A.; Nedjat, S.; Mahmoodi, M.; Farooq, U.; Yaseri, M.; Kasaeian, A.; Holakouie-Naieni, K. Assessing the quality of life among Pakistani general population and their associated factors by using the World Health Organization’s quality of life instrument (WHOQOL-BREF): A population based cross-sectional study. Health Qual. Life Outcomes 2019, 17, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ginieri-Coccossis, M.; Triantafillou, E.; Tomaras, V.; Soldatos, C.; Mavreas, V.; Christodoulou, G. Psychometric properties of WHOQOL-BREF in clinical and health Greek populations: Incorporating new culture-relevant items. Psychiatriki. 2012, 23, 130–142. [Google Scholar]
- Lucas-Carrasco, R. The WHO quality of life (WHOQOL) questionnaire: Spanish development and validation studies. Qual. Life Res. 2012, 21, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.-K.; Kim, D.; Jun, J.-B.; Bae, S.-C.; Sung, Y.-K. Factors influencing quality of life (QOL) for Korean patients with rheumatoid arthritis (RA). Rheumatol. Int. 2012, 33, 93–102. [Google Scholar] [CrossRef]
- Sijtsma, K. On the Use, the Misuse, and the Very Limited Usefulness of Cronbach’s Alpha. Psychometrika 2008, 74, 107–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paul, K. The Handbook of Psychological Testing; Routledge: London, UK; New York, NY, USA, 2000; 165p. [Google Scholar]

| Physical Health | Psychological Health | Social Relationships | Environmental Health | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| AGE GROUPS | ||||
| Less than <40 Years (n = 61) | 26.78± 4.46 | 21.24 ± 2.63 | 10.81 ± 1.62 | 28.00 ± 4.39 |
| More than >40 Years (n = 51) | 24.89 ± 4.31 | 19.88 ± 2.87 | 10.66 ± 1.32 | 26.01 ± 4.01 |
| p-value | 0.032 | 0.010 | 0.591 | 0.015 |
| GENDER | ||||
| Male (n = 74) | 25.56 ± 4.72 | 20.37 ± 2.92 | 11.09 ± 1.50 | 26.54 ± 4.31 |
| Female (n = 38) | 26.73 ± 3.86 | 21.10 ± 2.57 | 10.07 ± 1.23 | 28.18 ± 4.17 |
| p-value | 0.191 | 0.198 | 0.001 | 0.056 |
| HABIT DURATION | ||||
| <Less than 5 years (n = 41) | 25.70 ± 4.49 | 20.87 ± 2.67 | 10.60 ± 1.49 | 27.25 ± 4.61 |
| >More than 5 Years (n = 71) | 26.00 ± 4.41 | 20.42 ± 2.87 | 10.80 ± 1.47 | 26.94 ± 4.16 |
| p-value | 0.733 | 0.416 | 0.492 | 0.721 |
| FUNCTIONAL STAGES | ||||
| M-2 Mild (n = 32) | 25.34 ± 4.94 | 20.59 ± 2.55 | 10.53 ± 1.75 | 26.65 ± 5.02 |
| M-3 Moderate (n = 80) | 26.21 ± 4.27 | 20.63 ± 2.93 | 10.83 ± 1.37 | 27.27 ± 4.02 |
| p-value | 0.355 | 0.941 | 0.329 | 0.496 |
| Domains of Life | Minimum | Maximum | Mean | Std. Deviation |
|---|---|---|---|---|
| DOM-1 | 16.00 | 34.00 | 25.96 | 4.46 |
| DOM-2 | 16.00 | 25.00 | 20.62 | 2.81 |
| DOM-3 | 7.00 | 14.00 | 10.75 | 1.49 |
| DOM-4 | 18.00 | 35.00 | 27.09 | 4.32 |
| Rate of Quality of Life | 1 | 5 | 3.21 | 0.85 |
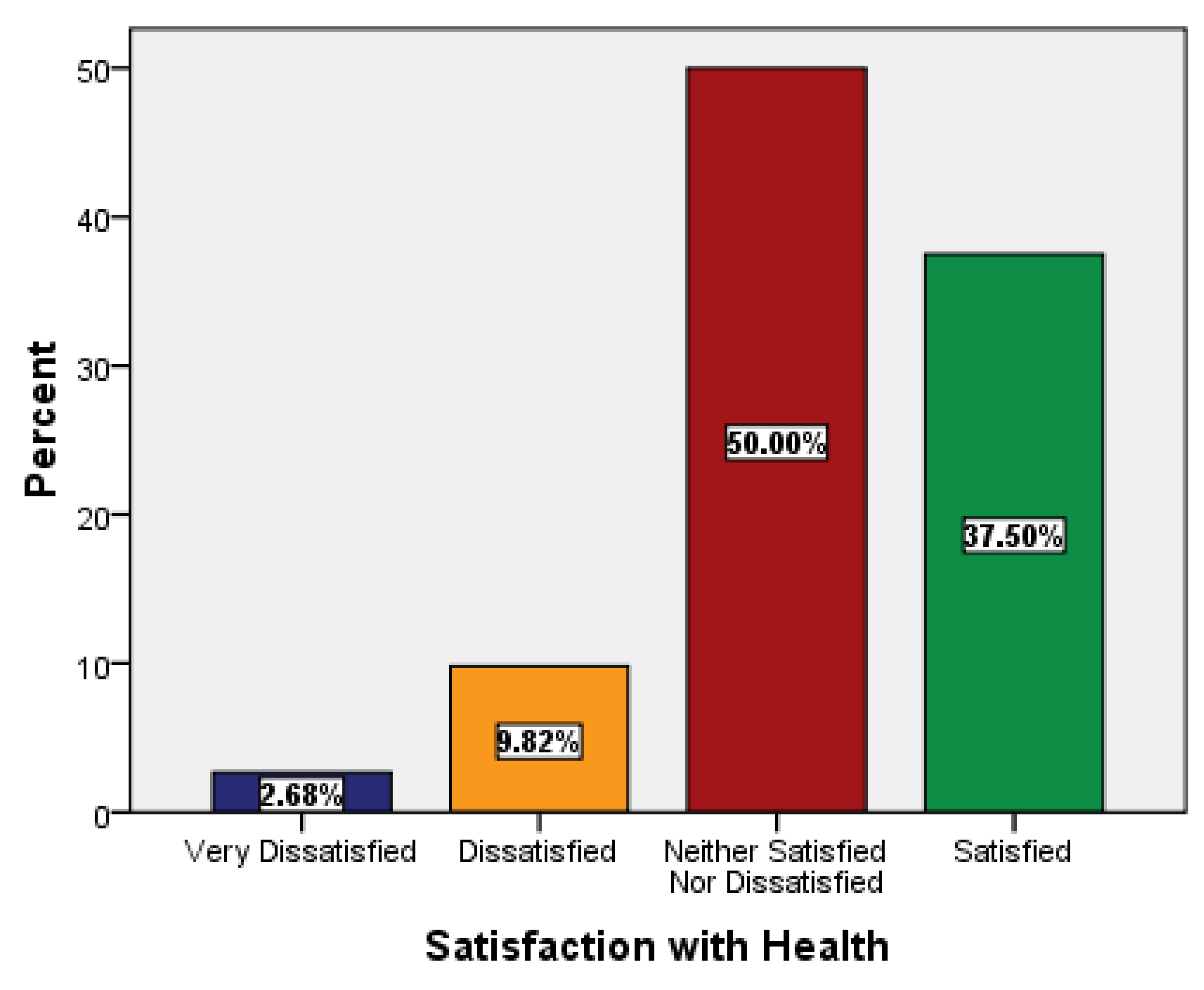
| Satisfaction with Health | 1 | 4 | 3.22 | 0.73 |
| Cronbach’s α coefficient | 0.880 | |||
| WHOQOL BREF | Mean | Standard Deviation | Corrected Item Total Correlation | Cronbach’s Coefficient | Cronbach‘s Alpha if Item Deleted |
|---|---|---|---|---|---|
| Domain 1 | 0.805 | ||||
| Physical pain | 2.60 | 1.16 | 0.487 | 0.806 | |
| Medical treatment | 2.66 | 1.03 | 0.423 | 0.810 | |
| Enough energy | 3.40 | 0.67 | 0.702 | 0.756 | |
| Get around | 3.38 | 0.78 | 0.566 | 0.774 | |
| Sleep satisfaction | 3.68 | 0.50 | 0.393 | 0.803 | |
| Daily living activities | 3.39 | 0.67 | 0.767 | 0.746 | |
| Capacity of work | 3.48 | 0.68 | 0.681 | 0.759 | |
| Domain 2 | 0.776 | ||||
| Life enjoyment | 3.53 | 0.69 | 0.662 | 0.706 | |
| Meaningful life | 3.65 | 0.65 | 0.665 | 0.708 | |
| Able to concentrate | 3.50 | 0.63 | 0.703 | 0.700 | |
| Bodily appearance | 3.49 | 0.50 | 0.531 | 0.747 | |
| Satisfaction with him/herself | 3.35 | 0.59 | 0.765 | 0.689 | |
| Negative feelings | 3.11 | 0.94 | 0.119 | 0.881 | |
| Domain 3 | 0.628 | ||||
| Personal relationship | 3.40 | 0.52 | 0.623 | 0.335 | |
| Sex life | 4.02 | 0.52 | 0.362 | 0.630 | |
| Support from friends | 3.33 | 0.86 | 0.436 | 0.636 | |
| Domain 4 | 0.952 | ||||
| Feeling of safety | 3.46 | 0.68 | 0.917 | 0.939 | |
| Physical environment | 3.35 | 0.56 | 0.719 | 0.952 | |
| Money for needs | 3.47 | 0.78 | 0.901 | 0.942 | |
| Information in daily life | 3.42 | 0.61 | 0.868 | 0.943 | |
| Leisure activities | 3.23 | 0.50 | 0.499 | 0.963 | |
| Satisfaction with living place | 3.44 | 0.61 | 0.828 | 0.945 | |
| Satisfaction health services | 3.35 | 0.59 | 0.955 | 0.937 | |
| Satisfaction with transport | 3.38 | 0.60 | 0.899 | 0.941 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Memon, A.B.; Rahman, A.A.U.; Channar, K.A.; Zafar, M.S.; Kumar, N. Assessing the Quality of Life of Oral Submucous Fibrosis Patients: A Cross-Sectional Study Using the WHOQOL-BREF Tool. Int. J. Environ. Res. Public Health 2021, 18, 9498. https://doi.org/10.3390/ijerph18189498
Memon AB, Rahman AAU, Channar KA, Zafar MS, Kumar N. Assessing the Quality of Life of Oral Submucous Fibrosis Patients: A Cross-Sectional Study Using the WHOQOL-BREF Tool. International Journal of Environmental Research and Public Health. 2021; 18(18):9498. https://doi.org/10.3390/ijerph18189498
Chicago/Turabian StyleMemon, Abdul Bari, Aneela Atta Ur Rahman, Kashif Ali Channar, Muhammad Sohail Zafar, and Naresh Kumar. 2021. "Assessing the Quality of Life of Oral Submucous Fibrosis Patients: A Cross-Sectional Study Using the WHOQOL-BREF Tool" International Journal of Environmental Research and Public Health 18, no. 18: 9498. https://doi.org/10.3390/ijerph18189498








