Racial and Gender Discrimination Predict Mental Health Outcomes among Healthcare Workers Beyond Pandemic-Related Stressors: Findings from a Cross-Sectional Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Recruitment
2.3. Data Collection Tool
2.4. Data Analysis
3. Results
3.1. Study Sample
3.2. Predictors of Mental Health Outcomes
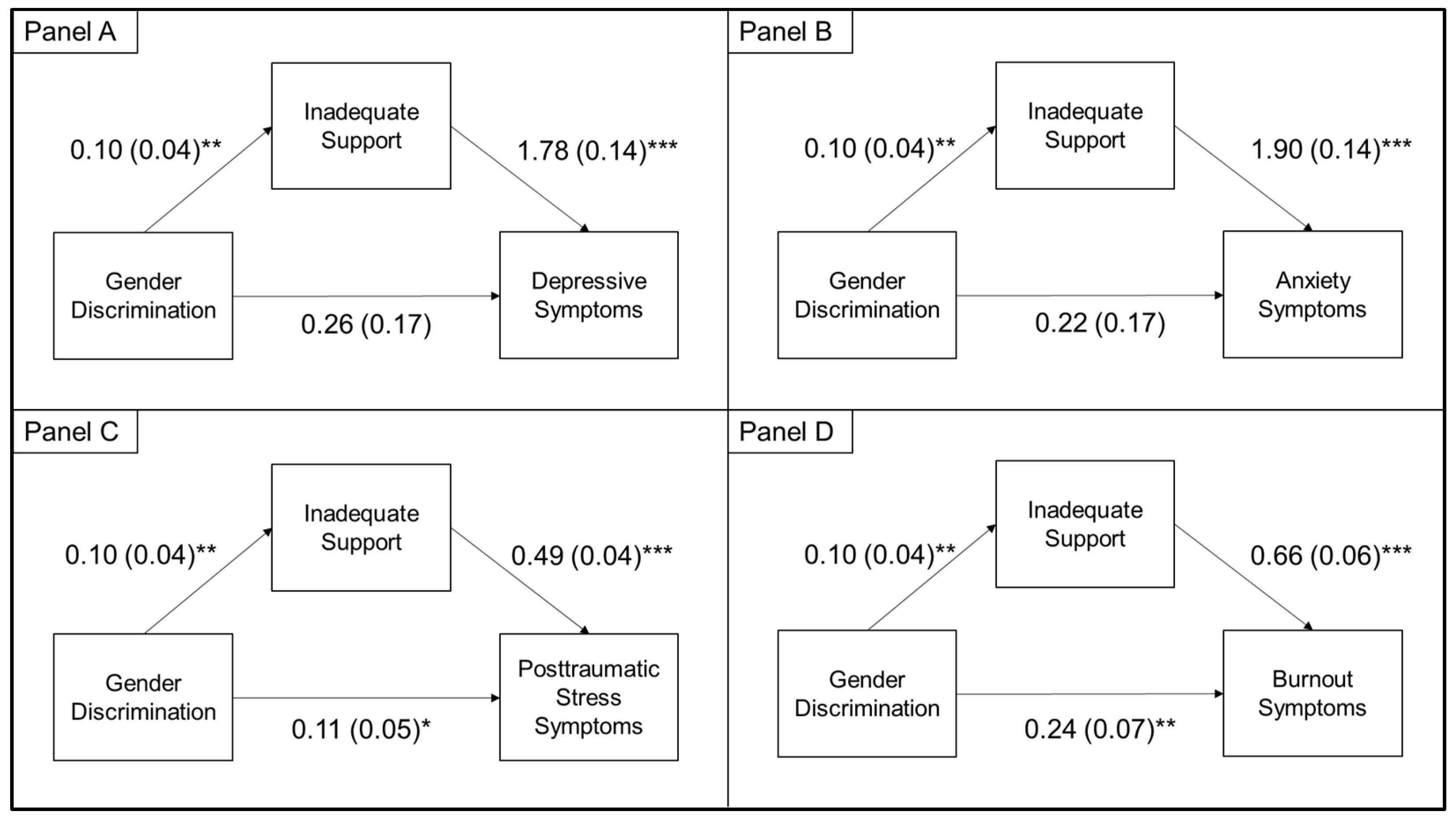
3.3. Indirect Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Y.; Scherer, N.; Felix, L.; Kuper, H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0246454. [Google Scholar] [CrossRef]
- Evanoff, B.A.; Strickland, J.R.; Dale, A.M. Work-Related and Personal Factors Associated With Mental Well-Being During the COVID-19 Response: Survey of Health Care and Other Workers. J. Med. Internet Res. 2020, 22, e21366. [Google Scholar] [CrossRef]
- Nguemeni Tiako, M.J.; South, E.C.; Ray, V. Medical Schools as Racialized Organizations: A Primer. Ann. Intern. Med. 2021, 174, 1143–1144. [Google Scholar] [CrossRef]
- Kaye, E.C. Misogyny in Medicine. N. Engl. J. Med. 2021, 384, 2267–2269. [Google Scholar] [CrossRef] [PubMed]
- Paradies, Y.; Ben, J.; Denson, N.; Elias, A.; Priest, N.; Pieterse, A.; Gupta, A.; Kelaher, M.; Gee, G. Racism as a Determinant of Health: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0138511. [Google Scholar] [CrossRef] [Green Version]
- Filut, A.; Alvarez, M.; Carnes, M. Discrimination Toward Physicians of Color: A Systematic Review. J. Natl. Med. Assoc. 2020, 112, 117–140. [Google Scholar] [CrossRef]
- Sudol, N.T.; Guaderrama, N.M.; Honsberger, P.; Weiss, J.; Li, Q.; Whitcomb, E.L. Prevalence and Nature of Sexist and Racial/Ethnic Microaggressions Against Surgeons and Anesthesiologists. JAMA Surg. 2021, 156, e210265. [Google Scholar] [CrossRef]
- Williams, D.R.; Lawrence, J.A.; Davis, B.A. Racism and Health: Evidence and Needed Research. Annu. Rev. Public Health 2019, 40, 105–125. [Google Scholar] [CrossRef] [Green Version]
- Cohen, L.H. Life Events and Psychological Functioning: Theoretical and Methodological Issues; SAGE Publications: London, UK, 1988; pp. 211–236. [Google Scholar]
- Prelow, H.M.; Mosher, C.E.; Bowman, M.A. Perceived Racial Discrimination, Social Support, and Psychological Adjustment Among African American College Students. J. Black Psychol. 2006, 32, 442–454. [Google Scholar] [CrossRef]
- Centers for Diseases Control and Prevention. Trends in Number of COVID-19 Cases and Deaths in the US Reported to CDC, by State/Territory. 2021. Available online: https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases (accessed on 1 February 2021).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard: Situation by Country, Territory, & Area. Available online: https://covid19.who.int/table (accessed on 1 February 2021).
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. Available online: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2763229 (accessed on 8 July 2021). [CrossRef] [PubMed]
- American Association of Public Opinion Research. Survey Disclosure Checklist. Available online: https://www.aapor.org/Standards-Ethics/Standard-Definitions-(1).aspx (accessed on 1 March 2021).
- Landrine, H.; Klonoff, E.A.; Corral, I.; Fernandez, S.; Roesch, S. Conceptualizing and Measuring Ethnic Discrimination in Health Research. J. Behav. Med. 2006, 29, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Vu, M.; Li, J.; Haardörfer, R.; Windle, M.; Berg, C.J. Mental health and substance use among women and men at the intersections of identities and experiences of discrimination: Insights from the intersectionality framework. BMC Public Health 2019, 19, 108. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [Green Version]
- Cameron, R.P.; Gusman, D. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Prim. Care Psychiatry 2003, 9, 9–14. [Google Scholar]
- West, C.P.; Dyrbye, L.N.; Sloan, J.A.; Shanafelt, T.D. Single Item Measures of Emotional Exhaustion and Depersonalization Are Useful for Assessing Burnout in Medical Professionals. J. Gen. Intern. Med. 2009, 24, 1318–1321. [Google Scholar] [CrossRef] [Green Version]
- Mata, D.A.; Ramos, M.A.; Bansal, N.; Khan, R.; Guille, C.; Di Angelantonio, E.; Sen, S. Prevalence of Depression and Depressive Symptoms Among Resident Physicians: A Systematic Review and Meta-analysis. JAMA 2018, 314, 2373–2383. [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.; Provencio, A.; Bentley-Kumar, K.; Pearcy, C.; Cook, T.; McLean, K.; Morgan, J.; Haque, Y.; Agrawal, V.; Bankhead-Kendall, B.; et al. PTSD and surgical residents: Everybody hurts… sometimes. Am. J. Surg. 2017, 214, 1118–1124. [Google Scholar] [CrossRef]
- Buselli, R.; Corsi, M.; Baldanzi, S.; Chiumiento, M.; Del Lupo, E.; Dell’Oste, V.; Bertelloni, C.A.; Massimetti, G.; Dell’Osso, L.; Cristaudo, A.; et al. Professional Quality of Life and Mental Health Outcomes among Health Care Workers Exposed to Sars-Cov-2 (Covid-19). Int. J. Environ. Res. Public Health 2020, 17, 6180. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available online: https://wwwn.cdc.gov/nchs/nhanes/Search/variablelist.aspx?Component=Questionnaire (accessed on 17 October 2020).
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain. Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Pacitti, F.; Di Lorenzo, G.; Di Marco, A.; Siracusano, A.; Rossi, A. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw. Open 2020, 3, e2010185. [Google Scholar] [CrossRef]
- Nunez-Smith, M.; Curry, L.A.; Berg, D.; Krumholz, H.M.; Bradley, E.H. Healthcare Workplace Conversations on Race and the Perspectives of Physicians of African Descent. J. Gen. Intern. Med. 2008, 23, 1471–1476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nunez-Smith, M.; Curry, L.A.; Bigby, J.; Berg, D.; Krumholz, H.M.; Bradley, E.H. Impact of race on the professional lives of physicians of African descent. Ann. Intern. Med. 2007, 146, 45–51. [Google Scholar] [CrossRef]
- Dahlke, A.R.; Johnson, J.K.; Greenberg, C.C.; Love, R.; Kreutzer, L.; Hewitt, D.B.; Quinn, C.M.; Engelhardt, K.E.; Bilimoria, K.Y. Gender Differences in Utilization of Duty-hour Regulations, Aspects of Burnout, and Psychological Well-being Among General Surgery Residents in the United States. Ann. Surg. 2018, 268, 204–211. [Google Scholar] [CrossRef] [PubMed]
- Harandi, T.F.; Taghinasab, M.M.; Nayeri, T.D. The correlation of social support with mental health: A meta-analysis. Electron. Physician 2017, 9, 5212–5222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017; pp. 120–141. [Google Scholar]
- Hu, Y.-Y.; Ellis, R.J.; Hewitt, D.B.; Yang, A.D.; Cheung, E.O.; Moskowitz, J.T.; Potts, J.R.; Buyske, J.; Hoyt, D.B.; Nasca, T.J.; et al. Discrimination, Abuse, Harassment, and Burnout in Surgical Residency Training. N. Engl. J. Med. 2019, 381, 1741–1752. [Google Scholar] [CrossRef]
- Anderson, N.; Lett, E.; Asabor, E.N.; Hernandez, A.L.; Tiako, M.J.N.; Johnson, C.; Montenegro, R.E.; Rizzo, T.M.; Latimore, D.; Nunez-Smith, M.; et al. The Association of Microaggressions with Depressive Symptoms and Institutional Satisfaction Among a National Cohort of Medical Students. J. Gen. Intern. Med. 2021. [Google Scholar] [CrossRef]
- Rhead, R.D.; Chui, Z.; Bakolis, I.; Gazard, B.; Harwood, H.; MacCrimmon, S.; Woodhead, C.; Hatch, S.L. Impact of workplace discrimination and harassment among National Health Service staff working in London trusts: Results from the TIDES study. BJPsych Open 2021, 7, e10. [Google Scholar] [CrossRef] [PubMed]
- Garcia, L.C.; Shanafelt, T.D.; West, C.P.; Sinsky, C.A.; Trockel, M.T.; Nedelec, L.; Maldonado, Y.A.; Tutty, M.; Dyrbye, L.N.; Fassiotto, M. Burnout, Depression, Career Satisfaction, and Work-Life Integration by Physician Race/Ethnicity. JAMA Netw. Open 2020, 3, e2012762. [Google Scholar] [CrossRef]
- Hennein, R.; Mew, E.J.; Lowe, S.R. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS ONE 2021, 16, e0246602. [Google Scholar] [CrossRef]
- Prasad, K.; McLoughlin, C.; Stillman, M.; Poplau, S.; Goelz, E.; Taylor, S.; Nankivil, N.; Brown, R.; Linzer, M.; Cappelucci, K.; et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine 2021, 35, 100879. [Google Scholar] [CrossRef]
- Erving, C.L.; Thomas, C.S.; Frazier, C. Is the Black-White Mental Health Paradox Consistent Across Gender and Psychiatric Disorders? Am. J. Epidemiol. 2019, 188, 314–322. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Druss, B.G.; Perlick, D.A. The Impact of Mental Illness Stigma on Seeking and Participating in Mental Health Care. Psychol. Sci. Public Interest 2014, 15, 37–70. [Google Scholar] [CrossRef] [Green Version]
- Gibbons, F.X.; Stock, M.L. Perceived Racial Discrimination and Health Behavior: Mediation and Moderation. In The Oxford Handbook of Stigma, Discrimination, and Health; Oxford University Press: New York, NY, USA, 2018; pp. 355–377. [Google Scholar]
- Kiecolt, K.J.; Hughes, M.; Keith, V.M. Can A High Sense of Control and John Henryism be Bad for Mental Health? Sociol. Q. 2009, 50, 693–714. [Google Scholar] [CrossRef]
- Robinson, M.N.; Tobin, C.S.T. Is John Henryism a Health Risk or Resource?: Exploring the Role of Culturally Relevant Coping for Physical and Mental Health among Black Americans. J. Health Soc. Behav. 2021, 62, 136–151. [Google Scholar] [CrossRef]
- Bronder, E.C.; Speight, S.L.; Witherspoon, K.M.; Thomas, A.J. John Henryism, Depression, and Perceived Social Support in Black Women. J. Black Psychol. 2013, 40, 115–137. [Google Scholar] [CrossRef]
- Hudson, D.L.; Neighbors, H.W.; Geronimus, A.T.; Jackson, J.S. Racial Discrimination, John Henryism, and Depression Among African Americans. J. Black Psychol. 2016, 42, 221–243. [Google Scholar] [CrossRef] [PubMed]
- Goreis, A.; Asbrock, F.; Nater, U.M.; Mewes, R. What Mediates the Relationship Between Ethnic Discrimination and Stress? Coping Strategies and Perceived Social Support of Russian Immigrants in Germany. Front. Psychiatry 2020, 11, 557148. [Google Scholar] [CrossRef]
- Kondrat, D.C.; Sullivan, W.P.; Wilkins, B.; Barrett, B.J.; Beerbower, E. The mediating effect of social support on the relationship between the impact of experienced stigma and mental health. Stigma Health 2018, 3, 305–314. [Google Scholar] [CrossRef]
- Miu, A.S.; Moore, J.R. Behind the Masks: Experiences of Mental Health Practitioners of Color During the COVID-19 Pandemic. Acad. Psychiatry 2021, 1–6. [Google Scholar] [CrossRef]
- USA Census Bureau. 2000 Census and 2017 American Community Survey 1-Year Estimates. 2017. Available online: https://www.census.gov/programs-surveys/acs/ (accessed on 1 March 2021).
- Bureau of Labor Statistics. State Occupational Employment Statistics Survey. 2018. Available online: http://www.bls.gov/oes/tables.htm (accessed on 1 March 2021).
- Jin, Y.; Zhu, D.; He, P. Social causation or social selection? The longitudinal interrelationship between poverty and depressive symptoms in China. Soc. Sci. Med. 2020, 249, 112848. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | n (%) or Mean (SD) |
|---|---|
| Demographic characteristics | |
| Age | 38.22 (11.77) |
| Pre-pandemic mental health diagnosis | 269 (26.98%) |
| Gender | |
| Male | 285 (28.59%) |
| Female | 712 (71.41%) |
| Race/ethnicity | |
| White | 688 (69.01%) |
| Asian | 148 (14.84%) |
| Black | 86 (8.63%) |
| Latinx | 73 (7.32%) |
| Other * | 21 (2.11%) |
| Marital status | |
| Married | 552 (55.37%) |
| Single | 392 (39.32%) |
| Divorced/widowed | 53 (5.32%) |
| Household income | |
| <$10,000 | 61 (6.12%) |
| $10,000 to $24,999 | 21 (2.11%) |
| $25,000 to $49,999 | 62 (6.22%) |
| $50,000 to $74,999 | 173 (17.35%) |
| $75,000 to $99,999 | 114 (11.43%) |
| $100,000 to $149,999 | 137 (13.74%) |
| $150,000 to $199,999 | 110 (11.03%) |
| $200,000 to 299,999 | 130 (13.04%) |
| >$300,000 | 189 (18.96%) |
| Profession | |
| Physician | 318 (31.90%) |
| Trainee | 280 (28.08%) |
| Nurse | 125 (12.54%) |
| Health technician | 76 (7.62%) |
| Physician, nursing, medical assistant | 47 (4.71%) |
| Other clinical | 86 (8.63%) |
| Other non-clinical | 65 (6.52%) |
| Pandemic-related social factors | |
| Family/friend contracted COVID-19 | 580 (58.17%) |
| Any housing change | 94 (9.43%) |
| Childcare needs among those with a child (n = 258) | |
| Does not need more childcare support | 75 (29.07%) |
| Needs a little more childcare support | 90 (34.88%) |
| Needs a lot more childcare support | 93 (36.05%) |
| Support needs | |
| None | 296 (29.69%) |
| A little | 262 (26.28%) |
| Some | 284 (28.49%) |
| A lot | 155 (15.55%) |
| Pandemic-related work factors | |
| Frontline status | |
| None | 330 (33.10%) |
| Indirect | 123 (12.34%) |
| Direct | 544 (54.56%) |
| Change in hours | |
| Same | 636 (63.79%) |
| Less | 82 (8.22%) |
| More | 279 (27.98%) |
| Roles changed | 452 (45.34%) |
| Racial Discrimination | |
| Overall | 23.65 (8.25) |
| Race/ethnicity | |
| White | 21.21 (4.77) b |
| Asian | 27.26 (9.91) a,b |
| Black | 33.96 (12.79) a |
| Latinx | 27.20 (10.18) a,b |
| Other * | 26.52 (10.96) |
| Gender Discrimination | |
| Overall | 1.65 (0.92) |
| Gender | |
| Female | 1.85 (0.03) c |
| Male | 1.16 (0.05) |
| Characteristics | Depressive Symptoms | Anxiety Symptoms | Posttraumatic Stress Symptoms | Burnout Symptoms |
|---|---|---|---|---|
| B (SE) | B (SE) | B (SE) | B (SE) | |
| Discrimination | ||||
| Racial/ethnic discrimination | 0.07 (0.02) *** | 0.07 (0.02) *** | 0.03 (0.01) *** | 0.02 (0.01) ** |
| Gender discrimination | 0.91 (0.16) *** | 0.90 (0.16) *** | 0.31 (0.04) *** | 0.50 (0.07) *** |
| Demographic characteristics | ||||
| Age | −0.01 (0.01) | −0.04 (0.01) ** | −0.02 (0.01) *** | −0.02 (0.01) *** |
| Gender | ||||
| Male (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 1.55 (0.33) *** | 1.79 (0.33) *** | 0.45 (0.09) *** | 0.62 (0.14) *** |
| Pre−pandemic mental health diagnosis | 2.84 (0.33) *** | 2.65 (0.33) *** | 0.53 (0.09) *** | 0.59 (0.14) *** |
| Race/ethnicity | ||||
| White (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Asian | −0.46 (0.43) | −0.61 (0.43) | −0.10 (0.12) | −0.15 (0.18) |
| Black | −0.85 (0.54) | −0.88 (0.55) | 0.04 (0.15) | −0.58 (0.23) * |
| Latinx | 0.70 (0.58) | 0.62 (0.59) | 0.23 (0.16) | 0.29 (0.29) |
| Other | −1.25 (1.05) | −0.74 (1.06) | −0.41 (0.29) | −0.58 (0.44) |
| Marital status | ||||
| Married (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Single | 1.09 (0.31) ** | 1.02 (0.32) ** | 0.32 (0.09) *** | 0.32 (0.13) * |
| Divorced/widowed | 1.89 (0.68) ** | 0.16 (0.69) | 0.24 (0.19) | −0.17 (0.29) |
| Household income | −0.17 (0.06) ** | −0.11 (0.06) | −0.04 (0.02) * | 0.01 (0.03) |
| Profession | ||||
| Physician (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Trainee | 0.45 (0.39) | 0.21 (0.39) | 0.13 (0.11) | 0.20 (0.16) |
| Nurse | 1.76 (0.50) *** | 2.31 (0.50) *** | 0.66 (0.14) *** | 0.73 (0.21) ** |
| Health technician | 1.67 (0.60) ** | 2.06 (0.60) ** | 0.33 (0.17) * | 0.23 (0.25) |
| Physician, nursing, medical assistant | 2.17 (0.74) ** | 2.67 (0.74) *** | 0.65 (0.20) ** | 0.69 (0.31) * |
| Other clinical | 1.03 (0.57) | 0.43 (0.57) | 0.19 (0.16) | −0.39 (0.24) |
| Other non-clinical | 1.69 (0.64) ** | 2.08 (0.64) ** | 0.60 (0.18) ** | 0.16 (0.27) |
| Pandemic-related social factors | ||||
| Family/friend contracted COVID-19 | 0.86 (0.31) ** | 1.19 (0.31) *** | 0.41 (0.08) *** | 0.18 (0.13) |
| Any housing change | 2.02 (0.51) *** | 1.38 (0.52) ** | 0.53 (0.14) *** | 0.59 (0.22) ** |
| Childcare needs | 0.51 (0.24) * | 0.84 (0.24) ** | 0.18 (0.07) ** | 0.37 (0.10) *** |
| Support needs | 2.06 (0.21) *** | 2.21 (0.13) *** | 0.61 (0.04) | 0.86 (0.05) *** |
| Pandemic-related work factors | ||||
| Frontline status | ||||
| None (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Indirect | 0.16 (0.50) | −0.09 (0.51) | 0.15 (0.14) | 0.26 (0.21) |
| Direct | 0.13 (0.33) | 0.16 (0.34) | 0.23 (0.09) * | 0.64 (0.14) *** |
| Change in hours | ||||
| Same (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Less | 0.13 (0.55) | −0.43 (0.56) | −0.09 (0.15) | −0.20 (0.23) |
| More | 1.45 (0.34) *** | 1.07 (0.34) ** | 0.47 (0.47) *** | 1.15 (0.14) *** |
| Roles changed | 0.91 (0.30) ** | 0.81 (0.30) ** | 0.41 (0.08) *** | 0.57 (0.13) *** |
| Characteristics | Depressive Symptoms | Anxiety Symptoms | Posttraumatic Stress Symptoms | Burnout Symptoms |
|---|---|---|---|---|
| B (SE) | B (SE) | B (SE) | B (SE) | |
| Discrimination | ||||
| Racial/ethnic discrimination | 0.04 (0.02) * | 0.05 (0.02) ** | 0.01 (0.01) ** | 0.01 (0.01) |
| Gender discrimination | 0.25 (0.17) | 0.20 (0.17) | 0.11 (0.05) * | 0.24 (0.07) ** |
| Demographic characteristics | ||||
| Age | 0.03 (0.02) * | −0.02 (0.02) | −0.01 (0) ** | −0.01 (0.01) * |
| Gender | ||||
| Male (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | −0.02 (0.34) | 0.03 (0.33) | −0.07 (0.09) | 0.04 (0.14) |
| Pre-pandemic mental health diagnosis | 2.01 (0.31) *** | 1.69 (0.30) *** | 0.23 (0.08) ** | 0.21 (0.13) |
| Race/ethnicity | ||||
| White (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Asian | −0.15 (0.41) | −0.35 (0.40) | −0.11 (0.11) | −0.28 (0.17) |
| Black | −1.52 (0.53) ** | −1.42 (0.53) ** | −0.13 (0.15) | −0.62 (0.22) ** |
| Latinx | 0.07 (0.52) | 0.03 (0.51) | 0.04 (0.14) | 0.12 (0.22) |
| Other | −1.45 (0.91) | −0.55 (0.90) | −0.40 (0.25) | −0.55 (0.38) |
| Marital status | ||||
| Married (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Single | 0.67 (0.36) | 0.66 (0.36) | 0.12 (0.10) | 0.22 (0.15) |
| Divorced/widowed | 1.11 (0.62) | −0.14 (0.61) | 0.18 (0.17) | 0.03 (0.26) |
| Household income | 0.01 (0.09) | 0.16 (0.09) | 0.03 (0.02) | 0.13 (0.04) ** |
| Profession | ||||
| Physician (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Trainee | −0.04 (0.47) | −0.48 (0.47) | −0.09 (0.13) | 0.39 (0.25) |
| Nurse | 0.77 (0.49) | 1.42 (0.48) * | 0.47 (0.13) *** | 0.70 (0.20) ** |
| Health technician | 1.12 (0.59) | 1.77 (0.58) ** | 0.29 (0.16) | 0.47 (0.25) |
| Physician, nursing, medical assistant | 0.89 (0.70) | 1.49 (0.69) * | 0.40 (0.19) * | 0.77 (0.29) * |
| Other clinical | 0.70 (0.58) | 0.20 (0.58) | 0.21 (0.16) | 0.05 (0.24) |
| Other non-clinical | 0.83 (0.63) | 1.33 (0.62) * | 0.43 (0.17) * | 0.33 (0.26) |
| Pandemic-related social factors | ||||
| Family/friend contracted COVID-19 | 0.36 (0.27) | 0.65 (0.27) * | 0.23 (0.07) ** | 0.01 (0.11) |
| Any housing change | 0.60 (0.47) | −0.11 (0.46) | 0.02 (0.13) | −0.04 (0.20) |
| Childcare needs | 0.05 (0.23) | 0.22 (0.23) | 0.01 (0.06) | 0.07 (0.10) |
| Support needs | 1.77 (0.14) *** | 1.89 (0.14) *** | 0.49 (0.04) *** | 0.65 (0.06) *** |
| Pandemic-related work factors | ||||
| Frontline status | ||||
| None (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Indirect | −0.09 (0.44) | −0.31 (0.44) | 0.08 (0.12) | 0.02 (0.19) |
| Direct | −0.20 (0.33) | −0.43 (0.32) | 0.07 (0.09) | 0.18 (0.14) |
| Change in hours | ||||
| Same (Reference) | 1.00 | 1.00 | 1.00 | 1.00 |
| Less | 0.18 (0.51) | −0.26 (0.50) | −0.11 (0.14) | −0.26 (0.21) |
| More | 0.70 (0.32) * | 0.32 (0.32) | 0.23 (0.09) ** | 0.75 (0.14) *** |
| Roles changed | −0.24 (0.29) | −0.21 (0.29) | 0.11 (0.08) | 0.15 (0.12) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hennein, R.; Bonumwezi, J.; Nguemeni Tiako, M.J.; Tineo, P.; Lowe, S.R. Racial and Gender Discrimination Predict Mental Health Outcomes among Healthcare Workers Beyond Pandemic-Related Stressors: Findings from a Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 9235. https://doi.org/10.3390/ijerph18179235
Hennein R, Bonumwezi J, Nguemeni Tiako MJ, Tineo P, Lowe SR. Racial and Gender Discrimination Predict Mental Health Outcomes among Healthcare Workers Beyond Pandemic-Related Stressors: Findings from a Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2021; 18(17):9235. https://doi.org/10.3390/ijerph18179235
Chicago/Turabian StyleHennein, Rachel, Jessica Bonumwezi, Max Jordan Nguemeni Tiako, Petty Tineo, and Sarah R. Lowe. 2021. "Racial and Gender Discrimination Predict Mental Health Outcomes among Healthcare Workers Beyond Pandemic-Related Stressors: Findings from a Cross-Sectional Survey" International Journal of Environmental Research and Public Health 18, no. 17: 9235. https://doi.org/10.3390/ijerph18179235
APA StyleHennein, R., Bonumwezi, J., Nguemeni Tiako, M. J., Tineo, P., & Lowe, S. R. (2021). Racial and Gender Discrimination Predict Mental Health Outcomes among Healthcare Workers Beyond Pandemic-Related Stressors: Findings from a Cross-Sectional Survey. International Journal of Environmental Research and Public Health, 18(17), 9235. https://doi.org/10.3390/ijerph18179235






