Evidence of Better Psychological Profile in Working Population Meeting Current Physical Activity Recommendations
Abstract
1. Introduction
2. Materials and Methods
2.1. Lifestyle Assessment
2.2. Statistics
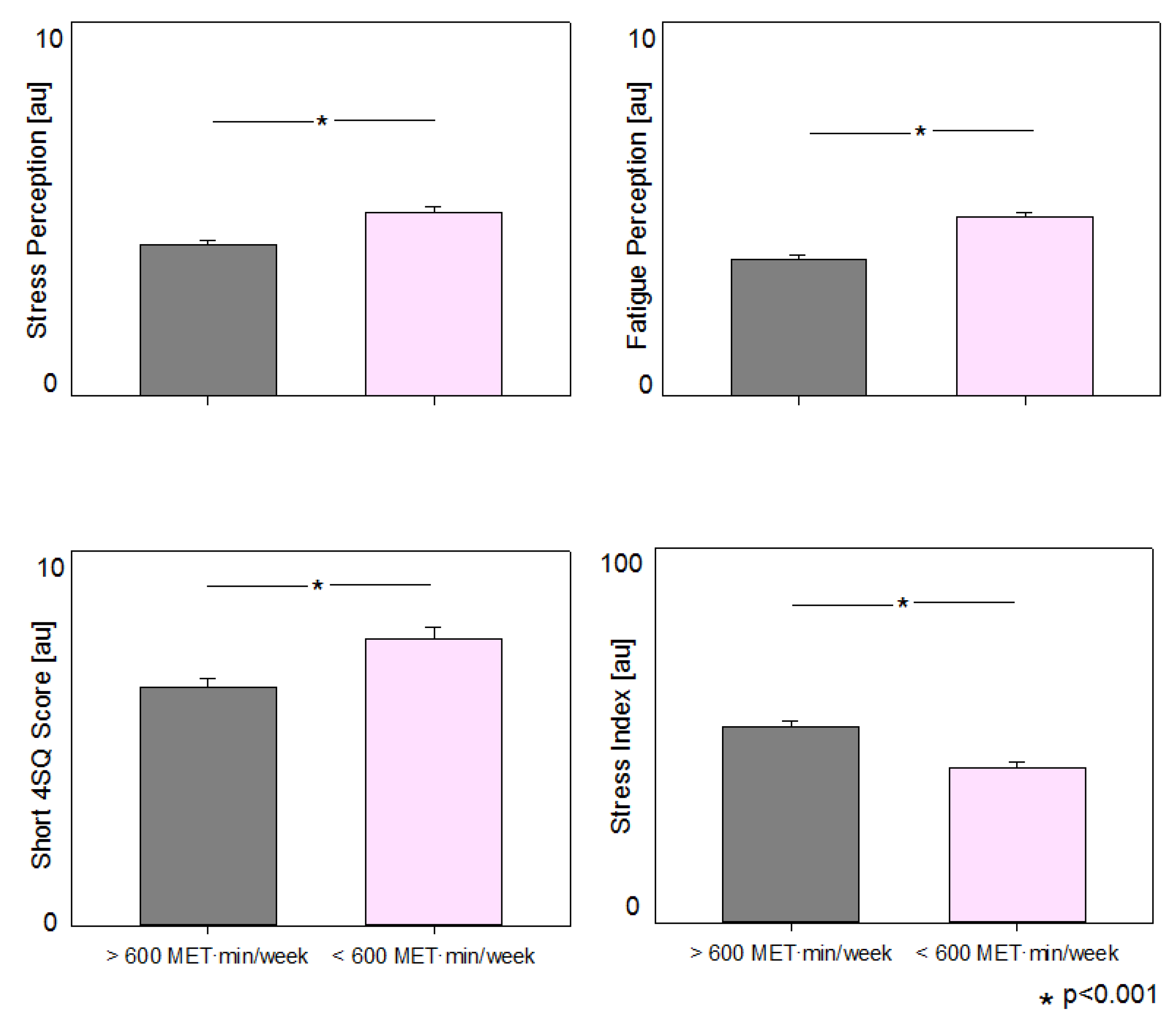
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lucini, D.; Malacarne, M.; Gatzemeier, W.; Pagani, M. A Simple Home-Based Lifestyle Intervention Program to Improve Cardiac Autonomic Regulation in Patients with Increased Cardiometabolic Risk. Sustainability 2020, 12, 7671. [Google Scholar] [CrossRef]
- Sallis, R.; Young, D.R.; Tartof, S.Y.; Sallis, J.F.; Sall, J.; Li, Q.; Smith, G.N.; Cohen, D.A. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48440 adult patients. Br. J. Sports Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.J.; Ozminkowski, R.J.; Serxner, S. Improving employee productivity through improved health. J. Occup. Environ. Med. 2013, 55, 1142–1148. [Google Scholar] [CrossRef]
- Baicker, K.; Cutler, D.; Song, Z. Workplace wellness programs can generate savings. Health Aff. 2010, 29, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Cadilhac, D.A.; Cumming, T.B.; Sheppard, L.; Pearce, D.C.; Carter, R.; Magnus, A. The economic benefits of reducing physical inactivity: An Australian example. Int. J. Behav. Nutr. Phys. Act 2011, 8, 99. [Google Scholar] [CrossRef]
- Wolf, A.M.; Siadaty, M.S.; Crowther, J.Q.; Nadler, J.L.; Wagner, D.L.; Cavalieri, S.L.; Elward, K.S.; Bovbjerg, V.E. Impact of lifestyle intervention on lost productivity and disability: Improving control with activity and nutrition. J. Occup. Environ. Med. 2009, 51, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Verra, S.E.; Benzerga, A.; Jiao, B.; Ruggeri, K. Health Promotion at Work: A Comparison of Policy and Practice across Europe. Saf. Health Work 2019, 10, 21–29. [Google Scholar] [CrossRef]
- Fonarow, G.C.; Calitz, C.; Arena, R.; Baase, C.; Isaac, F.W.; Lloyd-Jones, D.; Peterson, E.D.; Pronk, N.; Sanchez, E.; Terry, P.E.; et al. Workplace wellness recognition for optimizing workplace health: A presidential advisory from the American Heart Association. Circulation 2015, 131, e480–e497. [Google Scholar] [CrossRef]
- Song, Z.; Baicker, K. Effect of a Workplace Wellness Program on Employee Health and Economic Outcomes: A Randomized Clinical Trial. JAMA 2019, 321, 1491–1501. [Google Scholar] [CrossRef]
- Rongen, A.; Robroek, S.J.; van Lenthe, F.J.; Burdorf, A. Workplace health promotion: A meta-analysis of effectiveness. Am. J. Prev. Med. 2013, 44, 406–415. [Google Scholar] [CrossRef]
- Goetzel, R.Z.; Henke, R.M.; Tabrizi, M.; Pelletier, K.R.; Loeppke, R.; Ballard, D.W.; Grossmeier, J.; Anderson, D.R.; Yach, D.; Kelly, R.; et al. Do workplace health promotion (wellness) programs work? J. Occup. Environ. Med. 2014, 56, 927–934. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.P. What Is the ROI for Workplace Health Promotion? It Really Does Depend, and That’s the Point; SAGE Publications Sage CA: Los Angeles, CA, USA, 2015. [Google Scholar]
- European Commission. Communication from the Commission to the European Parliament, the Council, the European Economic and Social Committee and the Committee of the Regions on an EU Strategic Framework on Health and Safety at Work 2014–2020; European Commission: Brussels, Belgium, 2014; Available online: http://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:52014DC0332&from=EN (accessed on 26 June 2021).
- ENWHP. Luxembourg Declaration on Workplace Health Promotion in the European Union; ENWHP: Leuven, Belgium, 2007; Available online: http://www.enwhp.org/fileadmin/rs-dokumente/dateien/Luxembourg_Declaration.pdf (accessed on 26 June 2021).
- World Health Organization. The Ottawa Charter for Health Promotion; The Ottawa Charter; WHO: Ottawa, ON, USA, 1986; Available online: http://www.euro.who.int/en/publications/policy-documents/ottawa-charter-for-health-promotion (accessed on 26 June 2021).
- Milani, R.V.; Lavie, C.J. Health Care 2020: Reengineering Health Care Delivery to Combat Chronic Disease. Am. J. Med. 2015, 128, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Rao, G.; Burke, L.E.; Spring, B.J.; Ewing, L.J.; Turk, M.; Lichtenstein, A.H.; Cornier, M.-A.; Spence, J.D.; Coons, M. New and emerging weight management strategies for busy ambulatory settings: A scientific statement from the American Heart Association endorsed by the Society of Behavioral Medicine. Circulation 2011, 124, 1182–1203. [Google Scholar] [CrossRef]
- Hassard, J.; Muylaert, K.; Namysl, A.; Kazenas, A.; Flaspoler, E. Motivation for Employers to Carry Out Workplace Health Promotion: Literature Review; Office of the European Union: Luxembourg, 2012. [Google Scholar]
- O’Donnel, M.P. Health Promotion in the Workplace, 5th ed.; Art & Science of Health Promotion Institute CEO: Troy, MI, USA, 2017; pp. 1–721. [Google Scholar]
- Lucini, D.; Pagani, M. Exercise Prescription to Foster Health and Well-Being: A Behavioral Approach to Transform Barriers into Opportunities. Int. J. Environ. Res. Public Health 2021, 18, 968. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart disease and stroke statistics 2020 update: A report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- Artinian, N.T.; Fletcher, G.F.; Mozaffarian, D.; Kris-Etherton, P.; Van, H.L.; Lichtenstein, A.H.; Kumanyika, S.; Kraus, W.E.; Fleg, J.L.; Redeker, N.S.; et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: A scientific statement from the American Heart Association. Circulation 2010, 122, 406–441. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van, H.L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613. [Google Scholar] [CrossRef]
- Yang, Q.; Cogswell, M.E.; Flanders, W.D.; Hong, Y.; Zhang, Z.; Loustalot, F.; Gillespie, C.; Merritt, R.; Hu, F.B. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA 2012, 307, 1273–1283. [Google Scholar] [CrossRef]
- Lucini, D.; Zanuso, S.; Blair, S.; Pagani, M. A simple healthy lifestyle index as a proxy of wellness: A proof of concept. Acta Diabetol. 2015, 52, 81–89. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Patient Empowerment and Healt Care. In WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care; 20 Avenue Appia CH-1211; WHO: Geneva, Switzerland, 2009; p. 190. ISBN 978 92 4 159790 6. [Google Scholar]
- Carnethon, M.; Whitsel, L.P.; Franklin, B.A.; Kris-Etherton, P.; Milani, R.; Pratt, C.A.; Wagner, G.R. Worksite wellness programs for cardiovascular disease prevention: A policy statement from the American Heart Association. Circulation 2009, 120, 1725–1741. [Google Scholar] [CrossRef]
- Lucini, D.; Pagani, M. From stress to functional syndromes: An internist’s point of view. Eur. J. Intern. Med. 2012, 23, 295–301. [Google Scholar] [CrossRef]
- Stults-Kolehmainen, M.A.; Sinha, R. The effects of stress on physical activity and exercise. Sports Med. 2014, 44, 81–121. [Google Scholar] [CrossRef]
- Sharon-David, H.; Tenenbaum, G. The effectiveness of exercise interventions on coping with stress: Research synthesis. Stud. Sport Humanit. 2017, 21, 19–29. [Google Scholar] [CrossRef]
- Mental Health in the Workplaces. 2021. Available online: https://www.iso.org/obp/ui/#iso:std:iso:45003:ed-l:vl:en (accessed on 26 June 2021).
- Stress Management. Available online: https://www.heart.org/en/healthy-living/healthy-lifestyle/stress-management (accessed on 26 June 2021).
- Kivimäki, M.; Pentti, J.; Ferrie, J.E.; Batty, G.D.; Nyberg, S.T.; Jokela, M.; Virtanen, M.; Alfredsson, L.; Dragano, N.; Fransson, E.I.; et al. Work stress and risk of death in men and women with and without cardiometabolic disease: A multicohort study. Lancet Diabetes Endocrinol. 2018, 6, 705–713. [Google Scholar] [CrossRef]
- Kivimäki, M.; Jokela, M.; Nyberg, S.T.; Singh-Manoux, A.; Fransson, E.I.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Casini, A.; et al. Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015, 386, 1739–1746. [Google Scholar] [CrossRef]
- Lucini, D.; Riva, S.; Pizzinelli, P.; Pagani, M. Stress management at the worksite: Reversal of symptoms profile and cardiovascular dysregulation. Hypertension 2007, 49, 291–297. [Google Scholar] [CrossRef]
- Pischon, T.; Boeing, H.; Hoffmann, K.; Bergmann, M.; Schulze, M.B.; Overvad, K.; Van Der Schouw, Y.; Spencer, E.; Moons, K.; Tjønneland, A.; et al. General and abdominal adiposity and risk of death in Europe. N. Engl. J. Med. 2008, 359, 2105–2120. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Minetto, M.A.; Motta, G.; Gorji, N.E.; Lucini, D.; Biolo, G.; Pigozzi, F.; Portincasa, P.; Maffiuletti, N.A. Reproducibility and validity of the Italian version of the International Physical Activity Questionnaire in obese and diabetic patients. J. Endocrinol. Investig. 2018, 41, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 74, e177–e232. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Lucini, D.; Solaro, N.; Lesma, A.; Gillet, V.B.; Pagani, M. Health promotion in the workplace: Assessing stress and lifestyle with an intranet tool. J. Med. Internet Res. 2011, 13, e88. [Google Scholar] [CrossRef]
- Lucini, D.; Di Fede, G.; Parati, G.; Pagani, M. Impact of chronic psychosocial stress on autonomic cardiovascular regulation in otherwise healthy subjects. Hypertension 2005, 46, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Lucini, D.; Zanuso, S.; Solaro, N.; Vigo, C.; Malacarne, M.; Pagani, M. Reducing the risk of metabolic syndrome at the worksite: Preliminary experience with an ecological approach. Acta Diabetol. 2016, 53, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.L.; Makarem, N.; Shimbo, D.; Aggarwal, B. Gender Differences in Associations between Stress and Cardiovascular Risk Factors and Outcomes. Gend Genome 2018, 2, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Balhara, Y.P.; Gupta, C.S. Gender differences in stress response: Role of developmental and biological determinants. Ind. Psychiatry J. 2011, 20, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Rosengren, A.; Hawken, S.; Ounpuu, S.; Sliwa, K.; Zubaid, M.; Almahmeed, W.A.; Blackett, K.N.; Sitthi-Amorn, C.; Sato, H.; Yusuf, S. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 953–962. [Google Scholar] [CrossRef]
- Lucini, D.; Pagani, M. Autonomic Nervous System Assessment: A Novel Window on Clinical Stress. EC Psychol. Psychiatry 2017, 4, 172–180. [Google Scholar]
- Sjøgaard, G.; Christensen, J.R.; Justesen, J.B.; Murray, M.; Dalager, T.; Fredslund, G.H.; Søgaard, K. Exercise is more than medicine: The working age population’s well-being and productivity. J. Sport Health Sci. 2016, 5, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Fohr, T.; Pietila, J.; Helander, E.; Myllymaki, T.; Lindholm, H.; Rusko, H.; Kujala, U.M. Physical activity, body mass index and heart rate variability-based stress and recovery in 16 275 Finnish employees: A cross-sectional study. BMC Public Health 2016, 16, 701. [Google Scholar] [CrossRef]
- Phillips, A.C.; Burns, V.E.; Lord, J.M. Stress and exercise: Getting the balance right for aging immunity. Exerc. Sport Sci. Rev. 2007, 35, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Marques, I.; Balle, A.R.; Curado, C. The contribution of physical exercise to organisational performance. Eur. J. Manag. Stud. 2018, 23, 101–121. [Google Scholar] [CrossRef]
- Herring, M.P.; O’Connor, P.J.; Dishman, R.K. The effect of exercise training on anxiety symptoms among patients: A systematic review. Arch. Intern. Med. 2010, 170, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Rozanski, A. Exercise as medical treatment for depression. J. Am. Coll. Cardiol. 2012, 60, 1064–1066. [Google Scholar] [CrossRef][Green Version]
- Gordon, B.R.; McDowell, C.P.; Lyons, M.; Herring, M.P. Resistance exercise training for anxiety and worry symptoms among young adults: A randomized controlled trial. Sci. Rep. 2020, 10, 17548. [Google Scholar] [CrossRef]
- Robbins, R.; Jackson, C.L.; Underwood, P.; Vieira, D.; Jean-Louis, G.; Buxton, O.M. Employee Sleep and Workplace Health Promotion: A Systematic Review. Am. J. Health Promot. 2019, 33, 1009–1019. [Google Scholar] [CrossRef]
- Ramar, K.; Malhotra, R.K.; Carden, K.A.; Martin, J.L.; Abbasi-Feinberg, F.; Aurora, R.N.; Kapur, V.K.; Olson, E.J.; Rosen, C.L.; Rowley, J.A.; et al. Sleep is essential to health: An American Academy of Sleep Medicine position statement. J. Clin. Sleep Med. 2021. [Google Scholar] [CrossRef]
- Workplace Health Model. Available online: https://www.cdc.gov/workplacehealthpromotion/model/index.html (accessed on 26 June 2021).
- Hunt, M.K.; Lederman, R.; Stoddard, A.M.; LaMontagne, A.D.; McLellan, D.; Combe, C.; Barbeau, E.; Sorensen, G. Process evaluation of an integrated health promotion/occupational health model in WellWorks-2. Health Educ. Behav. 2005, 32, 10–26. [Google Scholar] [CrossRef]
- Grossmeier, J.; Johnson, S.S. Factors Driving Exemplary Workplace Health and Well-Being Initiatives; SAGE Publications Sage CA: Los Angeles, CA, USA, 2020. [Google Scholar] [CrossRef]
- Linnan, L.; Bowling, M.; Childress, J.; Lindsay, G.; Blakey, C.; Pronk, S.; Wieker, S.; Royall, P. Results of the 2004 national worksite health promotion survey. Am. J. Public Health 2008, 98, 1503–1509. [Google Scholar] [CrossRef]
- Bondi, M.A.; Harris, J.R.; Atkins, D.; French, M.E.; Umland, B. Employer coverage of clinical preventive services in the United States. Am. J. Health Promot. 2006, 20, 214–222. [Google Scholar] [CrossRef] [PubMed]
- McCoy, M.K.; Stinson, M.K.; Scott, M.K.; Tenney, M.L.; Newman, L.S. Health promotion in small business: A systematic review of factors influencing adoption and effectiveness of worksite wellness programs. J. Occup. Environ. Med./Am. Coll. Occup. Environ. Med. 2014, 56, 579. [Google Scholar] [CrossRef] [PubMed]
- Ryan, M.; Erck, L.; McGovern, L.; McCabe, K.; Myers, K.; Nobrega, S.; Li, W.; Lin, W.-C.; Punnett, L. “Working on Wellness:” protocol for a worksite health promotion capacity-building program for employers. BMC Public Health 2019, 19, 111. [Google Scholar] [CrossRef] [PubMed]
- Crane, M.; Bohn-Goldbaum, E.; Lloyd, B.; Rissel, C.; Bauman, A.; Indig, D.; Khanal, S.; Grunseit, A. Evaluation of Get Healthy at Work, a state-wide workplace health promotion program in Australia. BMC Public Health 2019, 19, 183. [Google Scholar] [CrossRef]
- Mazur, B.; Mazur-Małek, M. Towards corporate wellness: Health culture and wellness programs. J. Intercult. Manag. 2017, 9, 45–61. [Google Scholar] [CrossRef][Green Version]
- Schwatka, N.V.; Smith, D.; Weitzenkamp, D.; Atherly, A.; Dally, M.J.; Brockbank, C.V.; Tenney, L.; Goetzel, R.Z.; Jinnett, K.; McMillen, J. The impact of worksite wellness programs by size of business: A 3-year longitudinal study of participation, health benefits, absenteeism, and presenteeism. Ann. Work. Expo. Health 2018, 62 (Suppl. 1), S42–S54. [Google Scholar] [CrossRef]
- Taylor, A.W.; Pilkington, R.; Montgomerie, A.; Feist, H. The role of business size in assessing the uptake of health promoting workplace initiatives in Australia. BMC Public Health 2016, 16, 353. [Google Scholar] [CrossRef]
- Sun, H.; Edziah, B.K.; Sun, C.; Kporsu, A.K. Institutional quality, green innovation and energy efficiency. Energy Policy 2019, 135, 111002. [Google Scholar] [CrossRef]
- Aldana, S.G. Financial impact of health promotion programs: A comprehensive review of the literature. Am. J. Health Promot. 2001, 15, 296–320. [Google Scholar] [CrossRef]
- Chapman, L.S. Meta-evaluation of worksite health promotion economic return studies: 2005 update. Am. J. Health Promot. 2005, 19, 1–11. [Google Scholar] [CrossRef]
| Variables | Total | Female | Male | Significance p |
|---|---|---|---|---|
| N | 1305 | 620 | 685 | |
| Age [yrs] | 48.70 ± 11.21 | 45.63 ± 10.19 | 51.48 ± 11.37 | <0.001 |
| Weight [Kg] | 71.64 ± 14.88 | 61.84 ± 11.51 | 80.48 ± 11.68 | <0.001 |
| BMI [Kg/m2] | 24.12 ± 3.87 | 22.69 ± 4.02 | 25.41 ± 3.23 | <0.001 |
| Height [cm] | 171.80 ± 9.10 | 165.06 ± 6.28 | 177.88 ± 6.59 | <0.001 |
| Waist circumference [cm] | 86.89 ± 13.79 | 80.08 ± 12.59 | 94.07 ± 11.12 | <0.001 |
| Activity volume (moderate brisk walking) [MET·min/week] | 394.71 ± 470.76 | 384.65 ± 470.49 | 404.87 ± 471.43 | ns |
| Activity volume (other moderate activities) [MET·min/week] | 265.32 ± 396.36 | 265.50 ± 401.98 | 265.59 ± 391.95 | ns |
| Activity volume (vigorous) [MET·min/week] | 401.30 ± 788.72 | 295.10 ± 692.71 | 498.49 ± 856.42 | <0.001 |
| Total Activity volume [MET·min/week] | 1061.34 ± 1255 | 945.25 ± 1233 | 1168.94 ± 1268 | 0.01 |
| AHA Diet Score [au] | 2.22 ± 1.03 | 2.34 ± 1.06 | 2.12 ± 0.99 | ns |
| short 4SQ score [au] | 6.95 ± 7.30 | 8.57 ± 7.71 | 5.49 ± 6.59 | <0.001 |
| Smoke [n (%)] | 186 (14.25) | 92 (14.8) | 94 (13.7) | ns |
| STRESS perception [au] | 4.45 ± 3.00 | 5.15 ± 2.99 | 3.81 ± 2.87 | <0.001 |
| FATIGUE perception [au] | 4.17 ± 2.96 | 4.93 ± 2.99 | 3.47 ± 2.74 | <0.001 |
| SLEEP [hours per night] | 6.75 ± 1.09 | 6.82 ± 1.13 | 6.69 ± 1.06 | ns |
| Perception of sleep quality [au] | 6.26 ± 2.14 | 6.22 ± 2.18 | 6.29 ± 2.09 | ns |
| Perception of HEALTH quality [au] | 6.94 ± 1.57 | 6.90 ± 1.63 | 6.97 ± 1.52 | ns |
| Perception of JOB PERFORMANCE [au] | 4.26 ± 0.78 | 4.26 ± 0.74 | 4.25 ± 0.81 | ns |
| NUTRITION index [au] | 50.51 ± 11.52 | 51.25 ± 12.17 | 49.74 ± 10.77 | ns |
| EXERCISE index [au] | 67.71 ± 41.24 | 64.35 ± 42.10 | 70.87 ± 40.20 | 0.029 |
| STRESS index [au] | 47.42 ± 34.88 | 38.55 ± 22.89 | 55.56 ± 33.79 | <0.001 |
| LIFESTYLE INDEX [au] | 54.87 ± 20.69 | 51.63 ± 20.32 | 58.31 ± 20.50 | <0.001 |
| Variables | Above | Below | Significance p |
|---|---|---|---|
| N | 711 | 594 | |
| Age [yrs] | 49.38 ± 11.33 | 48.89 ± 11.00 | 0.017 |
| Weight [Kg] | 71.06 ± 13.95 | 72.30 ± 15.87 | <0.001 |
| BMI [Kg/m2] | 23.73 ± 3.53 | 24.58 ± 4.20 | <0.001 |
| Height [cm] | 172.51 ± 8.95 | 170.92 ± 9.18 | 0.338 |
| Waist circumference [cm] | 85.52 ± 12.87 | 88.74 ± 14.64 | <0.001 |
| Activity volume (moderate brisk walking) [MET·min/week] | 186.57 ± 159.38 | 39.83 ± 51.10 | <0.001 |
| Activity volume (other moderate activities) [MET·min/week] | 615.68 ± 525.96 | 131.43 ± 107.61 | <0.001 |
| Activity volume (vigorous) [MET·min/week] | 726.23 ± 953.72 | 13.59 ± 58.20 | <0.001 |
| Total Activity volume [MET·min/week] | 1787.52 ± 1307.45 | 195.04 ± 197.34 | <0.001 |
| AHA Score [au] | 2.58 ± 0.04 | 2.22 ± 0.04 | <0.001 |
| short 4SQ score [au] | 6.36 ± 9.94 | 7.67 ± 7.67 | 0.018 |
| Smoke [n (%)] | 91 (12.8) | 95 (16.0) | ns |
| STRESS perception [au] | 4.04 ± 2.79 | 4.92 ± 3.16 | <0.001 |
| FATIGUE perception [au] | 3.66 ± 2.79 | 4.77 ± 3.03 | <0.001 |
| SLEEP [hours per night] | 6.78 ± 1.08 | 6.71 ± 1.1 | ns |
| Perception of sleep quality [au] | 6.44 ± 2.00 | 6.05 ± 2.26 | 0.001 |
| Perception of HEALTH quality [au] | 7.30 ± 1.30 | 6.50 ± 1.74 | <0.001 |
| Perception of JOB PERFORMANCE [au] | 4.31 ± 0.73 | 4.19 ± 0.81 | 0.002 |
| NUTRITION index [au] | 52.94 ± 10.66 | 47.59 ± 11.84 | <0.001 |
| EXERCISE index [au] | 97.80 ± 3.17 | 31.83 ± 36.73 | <0.001 |
| STRESS index [au] | 52.47 ± 33.82 | 41.50 ± 35.20 | <0.001 |
| LIFESTYLE INDEX [au] | 67.51 ± 12.46 | 39.84 ± 18.34 | <0.001 |
| AHA Diet Score | WC | Short 4SQ Score | STRESS Perception | FATIGUE Perception | Sleep Hours | Total Activity Volume [MET·min/week] | |
|---|---|---|---|---|---|---|---|
| AHA Diet Score | 1.000 | ||||||
| WC | −0.170 ** | 1.000 | |||||
| 0.000 | |||||||
| Short 4SQ score | −0.091 ** | −0.082 ** | 1.000 | ||||
| 0.001 | 0.006 | ||||||
| STRESS perception | −0.126 ** | −0.079 ** | 0.528 ** | 1.000 | |||
| 0.000 | 0.008 | 0.000 | |||||
| FATIGUE perception | −0.136 ** | −0.087 ** | 0.553 ** | 0.742 ** | 1.000 | ||
| 0.000 | 0.003 | 0.000 | 0.000 | ||||
| Sleep hours | 0.023 | −0.099 ** | −0.071 * | −0.125 ** | −0.104 ** | 1.000 | |
| 0.406 | 0.001 | 0.01 | 0.000 | 0.000 | |||
| Total Activity volume [MET·min/week] | 0.186 ** | −0.150 ** | −0.115 ** | −0.190 ** | −0.221 ** | 0.057 * | 1.000 |
| 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.038 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucini, D.; Pagani, E.; Capria, F.; Galliano, M.; Marchese, M.; Cribellati, S. Evidence of Better Psychological Profile in Working Population Meeting Current Physical Activity Recommendations. Int. J. Environ. Res. Public Health 2021, 18, 8991. https://doi.org/10.3390/ijerph18178991
Lucini D, Pagani E, Capria F, Galliano M, Marchese M, Cribellati S. Evidence of Better Psychological Profile in Working Population Meeting Current Physical Activity Recommendations. International Journal of Environmental Research and Public Health. 2021; 18(17):8991. https://doi.org/10.3390/ijerph18178991
Chicago/Turabian StyleLucini, Daniela, Eleonora Pagani, Francesco Capria, Michele Galliano, Marcello Marchese, and Stefano Cribellati. 2021. "Evidence of Better Psychological Profile in Working Population Meeting Current Physical Activity Recommendations" International Journal of Environmental Research and Public Health 18, no. 17: 8991. https://doi.org/10.3390/ijerph18178991
APA StyleLucini, D., Pagani, E., Capria, F., Galliano, M., Marchese, M., & Cribellati, S. (2021). Evidence of Better Psychological Profile in Working Population Meeting Current Physical Activity Recommendations. International Journal of Environmental Research and Public Health, 18(17), 8991. https://doi.org/10.3390/ijerph18178991





