Socioecological Factors Associated with an Urban Exercise Prescription Program for Under-Resourced Women: A Mixed Methods Community-Engaged Research Project
Abstract
:1. Introduction
2. Materials and Methods
2.1. Quantitative Methods
Quantitative Data and Statistical Analysis
2.2. Qualitative Methods
3. Results
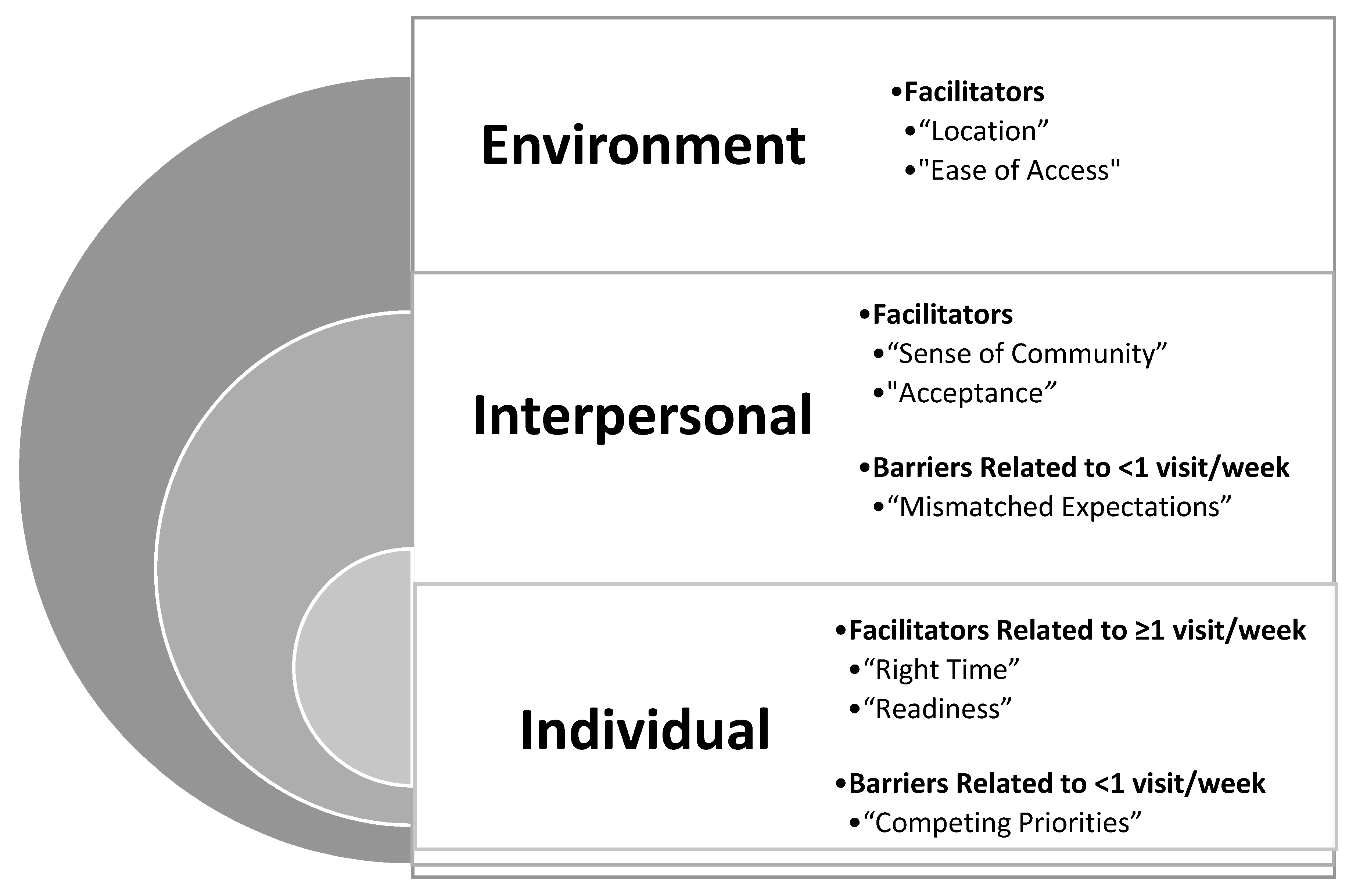
3.1. Individual Level
3.1.1. Quantitative Results
3.1.2. Qualitative Results
3.2. Interpersonal Level
3.2.1. Quantitative Results
3.2.2. Qualitative Results
3.3. Environmental Level
3.3.1. Quantitative Results
3.3.2. Qualitative Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Finkelstein, E.A.; Khavjou, O.A.; Thompson, H.; Trogdon, J.G.; Pan, L.; Sherry, B.; Dietz, W. Obesity and severe obesity forecasts through 2030. Am. J. Prev. Med. 2012, 42, 563–570. [Google Scholar] [CrossRef]
- Park, Y.W.; Zhu, S.; Palaniappan, L.; Heshka, S.; Carnethon, M.R.; Heymsfield, S.B. The metabolic syndrome: Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988-1994. Arch. Intern. Med. 2003, 163, 427–436. [Google Scholar] [CrossRef] [Green Version]
- Bastien, M.; Poirier, P.; Lemieux, I.; Despres, J.P. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog. Cardiovasc. Dis. 2014, 56, 369–381. [Google Scholar] [CrossRef]
- USDHHS. Physical Activity Guidelines for Americans. Available online: http://www.health.gov/paguidelines/ (accessed on 18 June 2018).
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U.; Lancet Physical Activity Series Working Gruop. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Shi, L. The impact of primary care: A focused review. Scientifica 2012, 2012, 432892. [Google Scholar] [CrossRef]
- Elley, C.R.; Kerse, N.; Arroll, B.; Robinson, E. Effectiveness of counselling patients on physical activity in general practice: Cluster randomised controlled trial. BMJ 2003, 326, 793. [Google Scholar] [CrossRef] [Green Version]
- Sallis, R.E. Exercise is medicine and physicians need to prescribe it! Br. J. Sports Med. 2009, 43, 3–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American College of Sports Medicine, Exercise Is Medicine Website. Available online: http://www.exerciseismedicine.org/support_page.php/community-resources/ (accessed on 25 October 2017).
- Lobelo, F.; Stoutenberg, M.; Hutber, A. The Exercise is Medicine Global Health Initiative: A 2014 update. Br. J. Sports Med. 2014, 48, 1627–1633. [Google Scholar] [CrossRef] [PubMed]
- Force, U.S.P.S.T.; Krist, A.H.; Davidson, K.W.; Mangione, C.M.; Barry, M.J.; Cabana, M.; Caughey, A.B.; Donahue, K.; Doubeni, C.A.; Epling, J.W., Jr.; et al. Behavioral Counseling Interventions to Promote a Healthy Diet and Physical Activity for Cardiovascular Disease Prevention in Adults with Cardiovascular Risk Factors: US Preventive Services Task Force Recommendation Statement. JAMA 2020, 324, 2069–2075. [Google Scholar] [CrossRef]
- Omura, J.D.; Carlson, S.A.; Paul, P.; Watson, K.B.; Loustalot, F.; Foltz, J.L.; Fulton, J.E. Adults Eligible for Cardiovascular Disease Prevention Counseling and Participation in Aerobic Physical Activity—United States, 2013. Morb. Mortal. Wkly. Rep. 2015, 64, 1047–1051. [Google Scholar] [CrossRef] [PubMed]
- Williams, N.H.; Hendry, M.; France, B.; Lewis, R.; Wilkinson, C. Effectiveness of exercise-referral schemes to promote physical activity in adults: Systematic review. Br. J. Gen. Pract. 2007, 57, 979–986. [Google Scholar] [CrossRef]
- Lord, J.C.A.G.F. Exercise on prescription: Does it work? Health Educ. J. 1995, 54, 453–464. [Google Scholar] [CrossRef]
- Pavey, T.; Taylor, A.; Hillsdon, M.; Fox, K.; Campbell, J.; Foster, C.; Moxham, T.; Mutrie, N.; Searle, J.; Taylor, R. Levels and predictors of exercise referral scheme uptake and adherence: A systematic review. J. Epidemiol. Community Health 2012, 66, 737–744. [Google Scholar] [CrossRef]
- Waterman, M.R.; Wiecha, J.M.; Manne, J.; Tringale, S.M.; Costa, E.; Wiecha, J.L. Utilization of a free fitness center-based exercise referral program among women with chronic disease risk factors. J. Community Health 2014, 39, 1179–1185. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Absalah, S.; Nierkens, V.; Stronks, K. Which factors engage women in deprived neighbourhoods to participate in exercise referral schemes? BMC Public Health 2008, 8, 371. [Google Scholar] [CrossRef] [Green Version]
- Arsenijevic, J.; Groot, W. Physical activity on prescription schemes (PARS): Do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses. BMJ Open 2017, 7, e012156. [Google Scholar] [CrossRef]
- Lin, J.S.; O’Connor, E.; Evans, C.V.; Senger, C.A.; Rowland, M.G.; Groom, H.C. Behavioral counseling to promote a healthy lifestyle in persons with cardiovascular risk factors: A systematic review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2014, 161, 568–578. [Google Scholar] [CrossRef]
- Gallegos-Carrillo, K.; Garcia-Pena, C.; Salmeron, J.; Salgado-de-Snyder, V.N.; Vazquez-Cabrer, G.; Lobelo, F. Exercise-referral scheme to promote physical activity among hypertensive patients: Design of a cluster randomized trial in the Primary Health Care Units of Mexico’s Social Security System. BMC Public Health 2014, 14, 706. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Morgan, F.; Battersby, A.; Weightman, A.L.; Searchfield, L.; Turley, R.; Morgan, H.; Jagroo, J.; Ellis, S. Adherence to exercise referral schemes by participants—What do providers and commissioners need to know? A systematic review of barriers and facilitators. BMC Public Health 2016, 16, 227. [Google Scholar] [CrossRef]
- Choitz, P.; Johnson, M.P.; Berhane, Z.; Lefever, G.; Anderson, J.K.; Eiser, A.R. Urban fitness centers: Removing barriers to promote exercise in underserved communities. J. Health Care Poor Underserved 2010, 21, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Nierkens, V.; Hartman, M.A.; Nicolaou, M.; Vissenberg, C.; Beune, E.J.; Hosper, K.; van Valkengoed, I.G.; Stronks, K. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. a systematic review. PLoS ONE 2013, 8, e73373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boston Chronic Disease and Health Statistics. Available online: http://wellnesstrail.tuftsctsi.org/neighborhoods/disease_rates/north_dorchester (accessed on 18 October 2017).
- Shore, C.B.; Hubbard, G.; Gorely, T.; Polson, R.; Hunter, A.; Galloway, S.D. Insufficient Reporting of Factors Associated With Exercise Referral Scheme Uptake, Attendance, and Adherence: A Systematic Review of Reviews. J. Phys. Act. Health 2019, 16, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Davidson, E.; Bhopal, R.; White, M.; Johnson, M.; Netto, G.; Deverill, M.; Sheikh, A. Adapting health promotion interventions to meet the needs of ethnic minority groups: Mixed-methods evidence synthesis. Health Technol. Assess. 2012, 16, 1–469. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [Green Version]
- Hallal, P.C.; Victora, C.G. Reliability and validity of the International Physical Activity Questionnaire (IPAQ). Med. Sci. Sports Exerc. 2004, 36, 556. [Google Scholar] [CrossRef]
- Marcus, B.H.; Selby, V.C.; Niaura, R.S.; Rossi, J.S. Self-efficacy and the stages of exercise behavior change. Res. Q. Exerc. Sport 1992, 63, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Marcus, B.H.; Rossi, J.S.; Selby, V.C.; Niaura, R.S.; Abrams, D.B. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992, 11, 386–395. [Google Scholar] [CrossRef]
- Barriers to Being Physically Active Quiz. Available online: https://www.cdc.gov/diabetes/ndep/pdfs/8-road-to-health-barriers-quiz-508.pdf (accessed on 15 March 2017).
- Sallis, J.F.; Grossman, R.M.; Pinski, R.B.; Patterson, T.L.; Nader, P.R. The development of scales to measure social support for diet and exercise behaviors. Prev. Med. 1987, 16, 825–836. [Google Scholar] [CrossRef]
- Matheny, A.P., Jr.; Wachs, T.D.; Ludwig, J.L.; Phillips, K. Bringing Order Out of Chaos: Psychometric Characteristics of the Confusion, Hubbub, and Order Scale. J. Appl. Dev. Psychol. 1995, 16, 429–444. [Google Scholar] [CrossRef]
- Duncan, D.T. What’s your Walk Score(R)?: Web-based neighborhood walkability assessment for health promotion and disease prevention. Am. J. Prev. Med. 2013, 45, 244–245. [Google Scholar] [CrossRef] [PubMed]
- Duncan, D.T.; Aldstadt, J.; Whalen, J.; Melly, S.J.; Gortmaker, S.L. Validation of walk score for estimating neighborhood walkability: An analysis of four US metropolitan areas. Int. J. Environ. Res. Public Health 2011, 8, 4160–4179. [Google Scholar] [CrossRef] [PubMed]
- Davidson, E.M.; Liu, J.J.; Bhopal, R.; White, M.; Johnson, M.R.; Netto, G.; Wabnitz, C.; Sheikh, A. Behavior change interventions to improve the health of racial and ethnic minority populations: A tool kit of adaptation approaches. Milbank Q. 2013, 91, 811–851. [Google Scholar] [CrossRef] [Green Version]
- Saldaña, J. The Coding Manual for Qualitative Researchers, 3rd ed.; SAGE: Los Angeles, CA, USA; London, UK, , 2016; 339p. [Google Scholar]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry & Research Design: Choosing among Five Approaches, 4th ed.; SAGE: Los Angeles, CA, USA, 2018; 459p. [Google Scholar]
- Ware, J.E., Jr.; Kosinski, M.; Gandek, B.; Sundaram, M.; Bjorner, J.B.; Turner-Bowker, D.M.; Maruish, M.E. User’s Manual for the SF-12v2 Health Survey, 3rd ed.; QualityMetric Incorporated: Lincoln, RI, USA, 2012. [Google Scholar]
- WalkScore. Walkscore Methodology. Available online: https://www.walkscore.com/methodology.shtml (accessed on 10 February 2019).
- Riva, M.; Gauvin, L.; Richard, L. Use of local area facilities for involvement in physical activity in Canada: Insights for developing environmental and policy interventions. Health Promot. Int. 2007, 22, 227–235. [Google Scholar] [CrossRef] [Green Version]
- Damush, T.M.; Stump, T.E.; Saporito, A.; Clark, D.O. Predictors of older primary care patients’ participation in a submaximal exercise test and a supervised, low-impact exercise class. Prev. Med. 2001, 33, 485–494. [Google Scholar] [CrossRef]
- Hanson, C.L.; Neubeck, L.; Kyle, R.G.; Brown, N.; Gallagher, R.; Clark, R.A.; McHale, S.; Dawkes, S. Gender Differences in Uptake, Adherence and Experiences: A Longitudinal, Mixed-Methods Study of a Physical Activity Referral Scheme in Scotland, UK. Int. J. Environ. Res. Public Health 2021, 18, 1700. [Google Scholar] [CrossRef]
- Hanson, C.L.; Oliver, E.J.; Dodd-Reynolds, C.J.; Allin, L.J. How do participant experiences and characteristics influence engagement in exercise referral? A qualitative longitudinal study of a scheme in Northumberland, UK. BMJ Open 2019, 9, e024370. [Google Scholar] [CrossRef] [Green Version]
- Claire, M.; Woolf-May, K. The retrospective evaluation of a general practioner exercise prescription programme. J. Hum. Nutr. Diet. 1999, 12, 32–42. [Google Scholar]
- Tobi, P.; Estacio, E.V.; Yu, G.; Renton, A.; Foster, N. Who stays, who drops out? Biosocial predictors of longer-term adherence in participants attending an exercise referral scheme in the UK. BMC Public Health 2012, 12, 347. [Google Scholar] [CrossRef] [Green Version]
- Taylor, A.H.; Doust, J.; Webborn, N. Randomised controlled trial to examine the effects of a GP exercise referral programme in Hailsham, East Sussex, on modifiable coronary heart disease risk factors. J. Epidemiol. Community Health 1998, 52, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Picorelli, A.M.; Pereira, L.S.; Pereira, D.S.; Felicio, D.; Sherrington, C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: A systematic review. J. Physiother. 2014, 60, 151–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Helen, W.; Ingle, L. GP exercise referral schemes: Improving the patient’s exerperience. Health Educ. J. 2018, 63, 362–373. [Google Scholar] [CrossRef]
- Martin-Borras, C.; Gine-Garriga, N.; Puig-Ribera, A.; Martin, C.; Sola, M.; Cuesta-Vargas, A.I.; Group, P. A new model of exercise referral scheme in primary care: Is the effect on adherence to physical activity sustainable in the long term? A 15-month randomised controlled trial. BMJ Open 2018, 8, e017211. [Google Scholar] [CrossRef]
- Carroll, R.; Ali, N.; Azam, N. Promoting physical activity in South Asian Muslim women through “exercise on prescription”. Health Technol. Assess. 2002, 6, 1–101. [Google Scholar] [CrossRef] [Green Version]
- Andersen, P.; Lendahls, L.; Holmberg, S.; Nilsen, P. Patients’ experiences of physical activity on prescription with access to counsellors in routine care: A qualitative study in Sweden. BMC Public Health 2019, 19, 210. [Google Scholar] [CrossRef] [Green Version]
- Leijon, M.E.; Faskunger, J.; Bendtsen, P.; Festin, K.; Nilsen, P. Who is not adhering to physical activity referrals, and why? Scand. J. Prim. Health Care 2011, 29, 234–240. [Google Scholar] [CrossRef]
- Kumanyika, S.K. Special issues regarding obesity in minority populations. Ann. Intern. Med. 1993, 119, 650–654. [Google Scholar] [CrossRef]
- Kumanyika, S.K. Obesity in minority populations: An epidemiologic assessment. Obes. Res. 1994, 2, 166–182. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Hickey, M.E.; Mason, S.E. Age and gender differences in particpation rates, motivators for, and barriers to exercise. Mod. Pyschol. Stud. 2017, 22, 3. [Google Scholar]
- Reddeman, L.; Bourgeois, N.; Angl, E.N.; Heinrich, M.; Hillier, L.; Finn, H.; Bosiak, B.; Agarwal, P.; Mawson, R.; Propp, R.; et al. How should family physicians provide physical activity advice? Qualitative study to inform the design of an e-health intervention. Can. Fam. Physician 2019, 65, e411–e419. [Google Scholar] [PubMed]
| Total (n = 30) | |
|---|---|
| Age (years) | 42.5 ± 13.4 |
| Range (years) | 21–78 |
| Race/Ethnicity n (%) | |
| Black (Hispanic/Non-Hispanic) | 22 (74) |
| Hispanic | 4 (13) |
| Mixed/Other | 4 (12) |
| Education n (%) | |
| High school diploma or less | 15 (50) |
| Some college | 6 (20) |
| Associate degree/2 year college | 3 (10) |
| College degree | 6 (20) |
| Employment n (%) | |
| Full-time | 10 (34) |
| Part time | 7 (23) |
| Unemployed | 12 (40) |
| Retired/other | 1 (3) |
| Marital Status n (%) | |
| Single | 18 (60) |
| Divorced | 5 (17) |
| Married | 5 (17) |
| Other | 2 (6) |
| Children n (%) | |
| 0 | 6 (20) |
| 1–2 | 11 (37) |
| 3–4 | 13 (43) |
| Number of Dependents | 1.3 ± 1.4 |
| Household Income n (%) | |
| <45,000/year | 18 (69) |
| ≥45,000/year | 8 (31) |
| People in Household | 3.5 ± 2.2 |
| Utilization | p-Value | ||
|---|---|---|---|
| Definition | <1 Visit/Week | ≥1 Visit/Week | |
| Individual Factors: Demographics and Health Status | |||
| n (% of total) | 20 (67) | 10 (33) | |
| Age (years) | 42.2 ± 13.2 | 42.9 ± 14.3 | 0.9 |
| Race: Black (Hispanic/Non-Hispanic) n (%) | 15 (75) | 7 (70) | 0.72 |
| Hispanic | 3(15) | 1 (10) | |
| Other (mixed race and other) | 2 (10) | 2 (20) | |
| BMI (kg/m2) | 35.4 ± 7.9 | 35.7 ± 6.0 | 0.92 |
| Employment (full or part time) n (%) | 12 (60) | 5(50) | 0.6 |
| Education: < high school n (%) | 7 (35) | 10 (80) | 0.02 + |
| Household Income: <45,000/year | 14 (73) | 4 (57) | 0.42 |
| Health: Self-perceived Mental Health (SF-12) | 45.3 ± 13.5 | 41.9 ± 13.2 * | 0.54 |
| Self-perceived Physical Health (SF-12) | 48.2 ± 7.5 | 53.3 ± 6.2 | 0.09 |
| CVD Risk factors (#) | 1.0 ± 1.0 | 0.6 ± 1.0 | 0.37 |
| Diabetes n (%) | 3 (15) | 0 (0) | 0.2 |
| Hypertension n (%) | 8 (40) | 3 (30) | 0.59 |
| Musculoskeletal Disorder n (%) | 6 (30) | 2 (20) | 0.56 |
| Dyslipidemia n (%) | 2 (10) | 1 (10) | 0.99 |
| Cardiovascular Disease n (%) | 0 | 0 | - |
| Medication n (%) | 15 (75) | 6 (60) | 0.40 |
| Individual Factors: Health Behaviors | |||
| Sedentary Behavior: TV (≤2 h/day) | 13 (65) | 7 (70) | 0.78 |
| Computer (≤2 h/day) | 8 (40) | 6 (60) | 0.3 |
| Sitting (mins/day) | 268 ± 211 | 307 ± 193 | 0.65 |
| Usual Daily Activity: Sits | 5 (25) | 1 (10) | |
| Stand/walks | 9 (45) | 1 (10) | 0.03 + |
| Lift loads | 6 (30) | 8 (80) | |
| Physical Activity: Walking (MET * mins) | 766 ± 1041 | 1210 ± 1034 | 0.31 |
| Moderate (MET * mins) | 1036 ± 2180 | 2333 ± 3943 | 0.38 |
| Vigorous (MET * mins) | 1338 ± 2302 | 1809 ± 1936 | 0.60 |
| Total (MET * mins) | 3184 ± 3402 | 5352 ± 5609 | 0.22 |
| Smoking: Current n (%) | 2 (10) | 1(10) | 0.96 |
| Former n (%) | 9(45) | 4(40) | |
| Alcohol: (drinks/week) | 1.1 ± 2.9 | 0.6 ± 1.1 | 0.48 |
| Physical Activity Self-efficacy (Range 1–5) | 2.5 ± 0.8 | 3.1 ± 0.9 | 0.08 |
| Stage of Change: Pre-action | 10 (50) | 3 (33) | 0.40 |
| Action n (%) | 10 (50) | 6 (67) | |
| Barriers: Lack of Time (Range 0–9) # | 3.0 ± 2.6 | 1.6 ± 2.3 | 0.18 |
| Social Influence | 3.9 ± 2.3 | 2.2 ± 2.4 | 0.09 |
| Lack of Energy | 4.3 ± 2.9 | 2.0 ± 2.9 | 0.07 |
| Lack of Willpower/Motivation | 6.0 ± 2.5 # | 2.8 ±2.8 | 0.007 + |
| Fear of Injury | 2.0 ± 2.4 | 1.2 ± 1.8 | 0.40 |
| Lack of Skill | 1.2 ± 1.3 | 0.9 ± 1.5 | 0.55 |
| Lack of Resources | 4.0 ± 2.9 | 2.2 ± 2.3 | 0.12 |
| Interpersonal and Social Factors | |||
| Marital Status: Married n% | 4 (20) | 1 (10) | 0.48 |
| Children | 2.1 ± 1.1 | 2.2 ± 1.7 | 0.78 |
| Number of Dependents | 1.6 ± 1.5 | 0.8 ± 0.9 | 0.15 |
| People in Household | 3.2 ± 1.6 | 4.1 ± 3.0 | 0.39 |
| CHAOS: Range 15–60 | 28.5 ± 11.1 | 27.3 ± 7.5 | 0.78 |
| Social Support for Physical Activity Family Participation (Range 10–80) | 20.4 ± 10.0 | 20.4 ± 8.9 | 0.99 |
| Friend Participation | 21.4 ± 9.4 | 16.6 ± 5.9 | 0.15 |
| Family Health History CVD risk factors (#) | 1.1 ± 1.1 | 2.0 ± 1.2 | 0.04 + |
| Diabetes n (%) | 7 (35) | 4 (40) | 0.79 |
| Hypertension n (%) | 9 (45) | 8 (80) | 0.07 |
| Dyslipidemia n (%) | 3 (15) | 5 (50) | 0.04 + |
| CVD n (%) | 2 (10) | 3 (30) | 0.17 |
| Environmental Factors | |||
| WalkScore (Range 0–100) | 79.9 ± 13.2 | 78.6 ± 11.0 | 0.79 |
| TransitScore (Range 0–100) | 71.7 ± 6.4 | 70.2 ± 5.7 | 0.55 |
| BikeScore (Range 0–100) | 59.8 ± 9.0 | 63.3 ± 7.2 | 0.31 |
| Walking distance to health center (miles) | 1.5 ± 2.1 | 2.1 ± 1.7 | 0.58 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camhi, S.M.; Debordes-Jackson, G.; Andrews, J.; Wright, J.; Lindsay, A.C.; Troped, P.J.; Hayman, L.L. Socioecological Factors Associated with an Urban Exercise Prescription Program for Under-Resourced Women: A Mixed Methods Community-Engaged Research Project. Int. J. Environ. Res. Public Health 2021, 18, 8726. https://doi.org/10.3390/ijerph18168726
Camhi SM, Debordes-Jackson G, Andrews J, Wright J, Lindsay AC, Troped PJ, Hayman LL. Socioecological Factors Associated with an Urban Exercise Prescription Program for Under-Resourced Women: A Mixed Methods Community-Engaged Research Project. International Journal of Environmental Research and Public Health. 2021; 18(16):8726. https://doi.org/10.3390/ijerph18168726
Chicago/Turabian StyleCamhi, Sarah M., Gifty Debordes-Jackson, Julianna Andrews, Julie Wright, Ana Cristina Lindsay, Philip J. Troped, and Laura L. Hayman. 2021. "Socioecological Factors Associated with an Urban Exercise Prescription Program for Under-Resourced Women: A Mixed Methods Community-Engaged Research Project" International Journal of Environmental Research and Public Health 18, no. 16: 8726. https://doi.org/10.3390/ijerph18168726
APA StyleCamhi, S. M., Debordes-Jackson, G., Andrews, J., Wright, J., Lindsay, A. C., Troped, P. J., & Hayman, L. L. (2021). Socioecological Factors Associated with an Urban Exercise Prescription Program for Under-Resourced Women: A Mixed Methods Community-Engaged Research Project. International Journal of Environmental Research and Public Health, 18(16), 8726. https://doi.org/10.3390/ijerph18168726








