Identifying the Impact of Intimate Partner Violence in Humanitarian Settings: Using an Ecological Framework to Review 15 Years of Evidence
Abstract
:1. Introduction
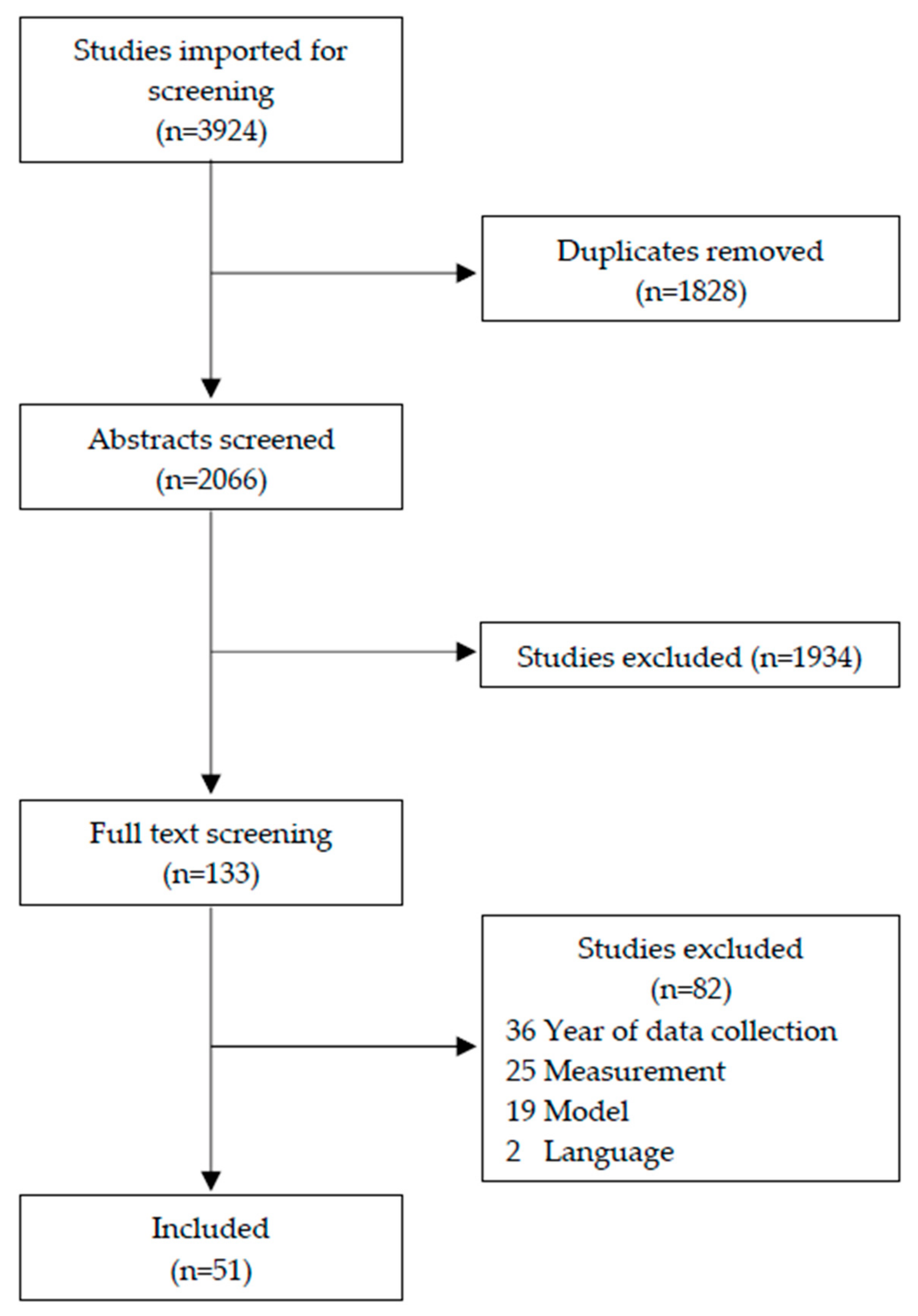
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
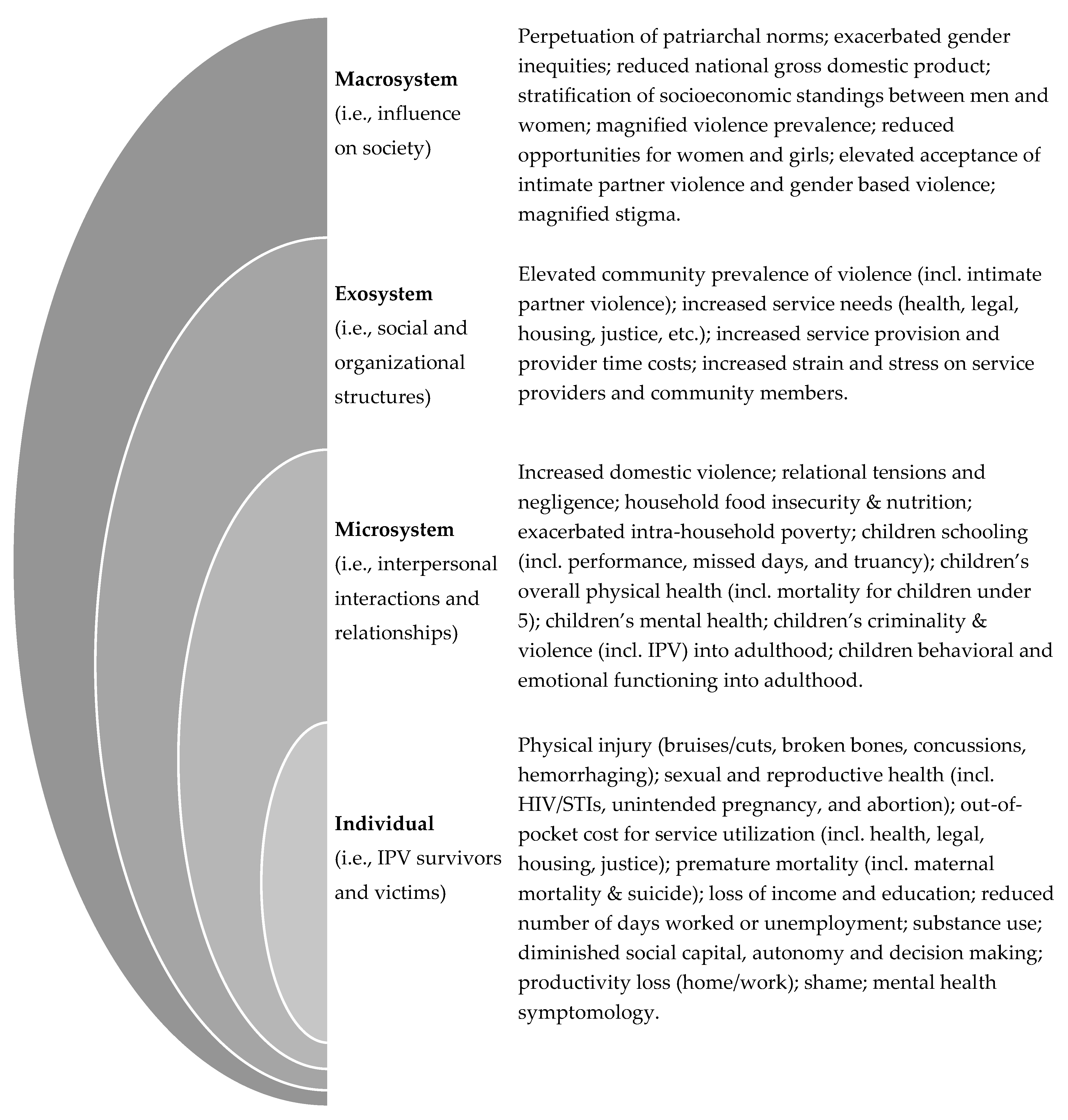
3. Findings
3.1. Overview of Included Articles
3.2. Impacts of IPV
3.3. IPV Variables
3.4. Quality Assessment
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- IASC. Guidelines for Integrating Gender-Based Violence Interventions in Humanitarian Action; IASC: Geneva, Switzerland, 2015. [Google Scholar]
- UNFPA. Managing Gender-based Violence Programmes in Emergencies. Available online: https://extranet.unfpa.org/Apps/GBVinEmergencies/index.html (accessed on 17 December 2020).
- Catani, C. War in the Home- an Overview of the Connection between War Traumatization and Domestic Violence. Behav. Ther. 2010, 20, 19–27. [Google Scholar] [CrossRef]
- Kelly, J.T.D.; Colantuoni, E.; Robinson, C.; Decker, M.R. From the Battlefield to the Bedroom: A Multilevel Analysis of the Links between Political Conflict and Intimate Partner Violence in Liberia. BMJ Glob. Health 2018, 3, 668. [Google Scholar] [CrossRef]
- Parcesepe, A.; Stark, L.; Roberts, L.; Boothby, N. Measuring Physical Violence and Rape against Somali Women Using the Neighborhood Method. Violence Women 2016, 22, 798–816. [Google Scholar] [CrossRef]
- Stark, L.; Ager, A. A Systematic Review of Prevalence Studies of Gender-Based Violence in Complex Emergencies. Trauma Violence Abus. 2011, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Stark, L.; Warner, A.; Lehmann, H.; Boothby, N.; Ager, A. Measuring the Incidence and Reporting of Violence against Women and Girls in Liberia Using the “Neighborhood Method”. Confl. Health 2013, 7, 20. [Google Scholar] [CrossRef] [Green Version]
- Rubenstein, B.L.; Lu, L.Z.N.; MacFarlane, M.; Stark, L. Predictors of Interpersonal Violence in the Household in Humanitarian Settings: A Systematic Review. Trauma Violence Abus. 2020, 31–44. [Google Scholar] [CrossRef]
- Stark, L.; Seff, I.; Reis, C. Gender-Based Violence against Adolescent Girls in Humanitarian Settings: A Review of the Evidence. Lancet Child Adolesc. Health 2020, 5, 210–222. [Google Scholar] [CrossRef]
- Coker, A.L.; Davis, K.E.; Arias, I.; Desai, S.; Sanderson, M.; Brandt, H.M.; Smith, P.H. Physical and Mental Health Effects of Intimate Partner Violence for Men and Women. Am. J. Prev. Med. 2002, 23, 260–268. [Google Scholar] [CrossRef]
- Campbell, J.C. Health Consequences of Intimate Partner Violence. Lancet 2002, 359, 1331–1336. [Google Scholar] [CrossRef]
- Grose, R.G.; Roof, K.A.; Semenza, D.C.; Leroux, X.; Yount, K.M. Mental Health, Empowerment, and Violence against Young Women in Lower-Income Countries: A Review of Reviews. Aggress. Violent Behav. 2019, 46, 25–36. [Google Scholar] [CrossRef]
- Grose, R.G.; Chen, J.S.; Roof, K.A.; Rachel, S.; Yount, K.M. Sexual and Reproductive Health Outcomes of Violence Against Women and Girls in Lower-Income Countries: A Review of Reviews. J. Sex Res. 2020, 1–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Classen, C.C.; Palesh, O.G.; Aggarwal, R. Sexual Revictimization. Trauma Violence Abus. 2005, 6, 103–129. [Google Scholar] [CrossRef]
- Logie, C.H.; Okumu, M.; Mwima, S.; Hakiza, R.; Irungi, K.P.; Kyambadde, P.; Kironde, E.; Narasimhan, M. Social Ecological Factors Associated with Experiencing Violence among Urban Refugee and Displaced Adolescent Girls and Young Women in Informal Settlements in Kampala, Uganda: A Cross-Sectional Study. Confl. Health 2019, 13, 60. [Google Scholar] [CrossRef]
- Kohli, A.; Perrin, N.; Mpanano, R.M.; Banywesize, L.; Mirindi, A.B.; Banywesize, J.H.; Mitima, C.M.; Binkurhorhwa, A.K.; Bufole, N.M.; Glass, N. Family and Community Driven Response to Intimate Partner Violence in Post-Conflict Settings. Soc. Sci. Med. 2015, 146, 276–284. [Google Scholar] [CrossRef] [Green Version]
- Panter-Brick, C. Conflict, Violence, and Health: Setting a New Interdisciplinary Agenda. Soc. Sci. Med. 2010, 1–6. [Google Scholar] [CrossRef]
- Rios-Avila, F.; Canavire-Bacarreza, G.J. The Effect of Intimate Partner Violence on Labor Market Decisions: Evidence from a Multi-Ethnic Country. Int. J. Soc. Econ. 2017, 44, 75–92. [Google Scholar] [CrossRef]
- Swanberg, J.E.; Logan, T.K.; Macke, C. Intimate Partner Violence, Employment, and The Workplace: Consequences and Future Directions. Trauma Violence Abus. 2005, 6, 286–312. [Google Scholar] [CrossRef]
- Dalal, K.; Dawad, S. Economic Costs of Domestic Violence: A Community Study in South Africa. HealthMED 2011, 5, 1931–1940. [Google Scholar]
- Lince-Deroche, N.; Berry, K.M.; Hendrickson, C.; Sineke, T.; Kgowedi, S.; Mulongo, M. Women’s Costs for Accessing Comprehensive Sexual and Reproductive Health Services: Findings from an Observational Study in Johannesburg, South Africa. Reprod. Health 2019, 16, 179. [Google Scholar] [CrossRef]
- Abramsky, T.; Watts, C.H.; Garcia-Moreno, C.; Devries, K.; Kiss, L.; Ellsberg, M.; Jansen, H.A.; Heise, L. What Factors Are Associated with Recent Intimate Partner Violence? Findings from the WHO Multi-Country Study on Women’s Health and Domestic Violence. BMC Public Health 2011, 11, 109. [Google Scholar] [CrossRef] [Green Version]
- Fulu, E.; Miedema, S.; Roselli, T.; McCook, S.; Chan, K.L.; Haardörfer, R.; Jewkes, R.; Fulu, E.; Jewkes, R.; Warner, X.; et al. Pathways between Childhood Trauma, Intimate Partner Violence, and Harsh Parenting: Findings from the UN Multi-Country Study on Men and Violence in Asia and the Pacific. Lancet Glob. Health 2017, 5, e512–e522. [Google Scholar] [CrossRef] [Green Version]
- Jewkes, R. Intimate Partner Violence: Causes and Prevention. Lancet Lond. Engl. 2002, 359, 1423–1429. [Google Scholar] [CrossRef]
- Krug, E.G.; Mercy, J.A.; Dahlberg, L.L.; Zwi, A.B. The World Report on Violence and Health. Lancet 2002, 360, 1083–1088. [Google Scholar] [CrossRef] [Green Version]
- United Nations. United Nations Security Council Resolution 1325 on Women, Peace and Security Understanding the Implications, Fulfilling the Obligations; United Nations: New York, NY, USA, 2000. [Google Scholar]
- Pinheiro, P.S. World Report on Violence against Children; UN: Geneva, Switzerland, 2009. [Google Scholar]
- Bundhamcharoen, K.; Odton, P.; Mugem, S.; Phulkerd, S.; Dhisayathikom, K.; Brown, D.W.; Tangcharoensathien, V. Costs of Injuries Due to Interpersonal and Self-Directed Violence in Thailand. J. Med. Assoc. Thai. 2005, 91, S110–S118. [Google Scholar]
- Raghavendra, S.; Duvvury, N.; Ashe, S. The Macroeconomic Loss Due to Violence against Women: The Case of Vietnam. Fem. Econ. 2017, 23, 62–89. [Google Scholar] [CrossRef]
- Roldós, M.I.; Corso, P. The Economic Burden of Intimate Partner Violence in Ecuador: Setting the Agenda for Future Research and Violence Prevention Policies. West. J. Emerg. Med. 2013, 14, 347–353. [Google Scholar] [CrossRef]
- Heise, L.L. Violence against Women: An Integrated, Ecological Framework. Violence Woman 1998, 4, 262–290. [Google Scholar] [CrossRef]
- Cislaghi, B.; Heise, L. Using Social Norms Theory for Health Promotion in Low-Income Countries. Health Promot. Int. 2019, 34, 616–623. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ 2009, 332–336. [Google Scholar] [CrossRef] [Green Version]
- WHO. WHO Multi-Country Study on Women’s Health and Domestic Violence against Women; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- United Nations Office for the Coordination of Humanitarian Affairs. Financial Tracking System. Available online: https://fts.unocha.org/ (accessed on 17 December 2020).
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a Critical Appraisal Tool to Assess the Quality of Cross-Sectional Studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef] [Green Version]
- Goessmann, K.; Ibrahim, H.; Neuner, F. Association of War-Related and Gender-Based Violence With Mental Health States of Yazidi Women. JAMA Netw. Open 2020, 3, e2013418. [Google Scholar] [CrossRef] [PubMed]
- Al-Atrushi, H.H.; Al-Tawil, N.G.; Shabila, N.P.; Al-Hadithi, T.S. Intimate Partner Violence against Women in the Erbil City of the Kurdistan Region, Iraq. BMC Womens Health 2013, 13, 37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zakar, R.; Zakar, M.Z.; Mikolajczyk, R.; Krämer, A. Intimate Partner Violence and Its Association with Women’s Reproductive Health in Pakistan. Int. J. Gynaecol. Obstet. 2012, 117, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Zakar, R.; Zakar, M.Z.; Mikolajczyk, R.; Kraemer, A. Spousal Violence against Women and Its Association with Women’s Mental Health in Pakistan. Health Care Women Int. 2013, 34, 795–813. [Google Scholar] [CrossRef]
- Sousa, C.; Yacoubian, K.; Flaherty Fischette, P.; Haj-Yahia, M.M. The Co-Occurrence and Unique Mental Health Effects of Political Violence and Intimate Partner Violence. J. Interpers. Violence 2018, 33, 268–292. [Google Scholar] [CrossRef]
- Falb, K.L.; Blackwell, A.; Stennes, J.; Hussein, M.; Annan, J. Depressive Symptoms among Women in Raqqa Governorate, Syria: Associations with Intimate Partner Violence, Food Insecurity, and Perceived Needs. Glob. Ment. Health Camb. Engl. 2019, 6, e22. [Google Scholar] [CrossRef] [Green Version]
- Fiorentino, M.; Sagaon-Teyssier, L.; Ndiaye, K.; Suzan-Monti, M.; Mengue, M.-T.; Vidal, L.; Kuaban, C.; March, L.; Laurent, C.; Spire, B.; et al. Intimate Partner Violence against HIV-Positive Cameroonian Women: Prevalence, Associated Factors and Relationship with Antiretroviral Therapy Discontinuity—Results from the ANRS-12288 EVOLCam Survey. Womens Health 2019, 15, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Peltzer, K.; Pengpid, S. Female Genital Mutilation and Intimate Partner Violence in the Ivory Coast. BMC Womens Health 2014, 14, 13. [Google Scholar] [CrossRef] [Green Version]
- Alenko, A.; Girma, S.; Abera, M.; Workicho, A. Children Emotional and Behavioural Problems and Its Association with Maternal Depression in Jimma Town, Southwest Ethiopia. Gen. Psychiatry 2020, 33. [Google Scholar] [CrossRef]
- Gebreslasie, K.Z.; Weldemariam, S.; Gebre, G.; Mehari, M.-A. Intimate Partner Violence during Pregnancy and Risk of Still Birth in Hospitals of Tigray Region Ethiopia. Ital. J. Pediatr. 2020, 46, 107. [Google Scholar] [CrossRef]
- Sipsma, H.; Callands, T.A.; Bradley, E.; Harris, B.; Johnson, B.; Hansen, N.B. Healthcare Utilisation and Empowerment among Women in Liberia. J. Epidemiol. Community Health 2013, 67, 953–959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sobkoviak, R.M.; Yount, K.M.; Halim, N. Domestic Violence and Child Nutrition in Liberia. Soc. Sci. Med. 2012, 74, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Hayes, B.; van Baak, C. Risk Factors of Physical and Sexual Abuse for Women in Mali: Findings from a Nationally Representative Sample. Violence Women 2017, 23, 1361–1381. [Google Scholar] [CrossRef] [PubMed]
- DeLong, S.M.; Brooks, M.I.; Aliou, S.; Lundgren, R.; Corneliess, C.; Johns, N.E.; Challa, S.; Carter, N.; Lauro, G.; Silverman, J.G. Married Very Young Adolescent Girls in Niger at Greatest Risk of Lifetime Male Partner Reproductive Coercion and Sexual Violence. PLoS ONE 2020, 15, 30231392. [Google Scholar] [CrossRef]
- Silverman, J.G.; Challa, S.; Boyce, S.C.; Averbach, S.; Raj, A. Associations of Reproductive Coercion and Intimate Partner Violence with Overt and Covert Family Planning Use among Married Adolescent Girls in Niger. EClinicalMedicine 2020, 22, 100393. [Google Scholar] [CrossRef] [PubMed]
- Kana, M.A.; Safiyan, H.; Yusuf, H.E.; Musa, A.S.M.; Richards-Barber, M.; Harmon, Q.E.; London, S.J. Association of Intimate Partner Violence during Pregnancy and Birth Weight among Term Births: A Cross-Sectional Study in Kaduna, Northwestern Nigeria. BMJ Open 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Abiodun, O.; Sodeinde, K.; Bamidele, F.; Ojinni, Y.; Adekeye, J.; Ohiaogu, F.; Mbonu, F. Intimate Partner Violence among Women Accessing HIV-Care Services at Tertiary Hospitals in Ogun State, Nigeria: Implications for Policy and Practice. J. Interpers. Violence 2020, 1–21. [Google Scholar] [CrossRef]
- Kidman, R.; Palermo, T.; Bertrand, J. Intimate Partner Violence, Modern Contraceptive Use and Conflict in the Democratic Republic of the Congo. Soc. Sci. Med. 2015, 133, 2–10. [Google Scholar] [CrossRef]
- Fleming, P.J.; McCleary-Sills, J.; Morton, M.; Levtov, R.; Heilman, B.; Barker, G. Risk Factors for Men’s Lifetime Perpetration of Physical Violence against Intimate Partners: Results from the International Men and Gender Equality Survey (IMAGES) in Eight Countries. PLoS ONE 2015, 10, e0118639. [Google Scholar] [CrossRef]
- Johnson, K.; Scott, J.; Rughita, B.; Kisielewski, M.; Asher, J.; Ong, R.; Lawry, L. Association of Sexual Violence and Human Rights Violations with Physical and Mental Health in Territories of the Eastern Democratic Republic of the Congo. JAMA J. Am. Med. Assoc. 2010, 304, 553–562. [Google Scholar] [CrossRef] [Green Version]
- Gichane, M.W.; Moracco, K.E.; Thirumurthy, H.; Okitolonda, E.W.; Behets, F.; Yotebieng, M. Intimate Partner Violence and Prevention of Mother to Child Transmission of HIV: Evidence from Kinshasa, Democratic Republic of Congo. PLoS ONE 2018, 13, e0203471. [Google Scholar] [CrossRef]
- Tiruneh, F.N.; Chuang, K.Y.; Ntenda, P.A.M.; Chuang, Y.C. Unwanted Pregnancy, Pregnancy Loss, and Other Risk Factors for Intimate Partner Violence in the Democratic Republic of the Congo. Women Health 2018, 58, 983–1000. [Google Scholar] [CrossRef]
- Mpody, C.; Thompson, P.; Tabala, M.; Ravelomanana, N.L.R.; Malongo, F.; Kawende, B.; Behets, F.; Okitolonda, E.; Yotebieng, M. Hepatitis B Infection among Pregnant and Post-Partum Women Living with HIV and on Antiretroviral Therapy in Kinshasa, DR Congo: A Cross-Sectional Study. PLoS ONE 2019, 14, e0216293. [Google Scholar] [CrossRef] [Green Version]
- Onsomu, E.O.; Abuya, B.A.; Okech, I.N.; Rosen, D.L.; Duren-Winfield, V.; Simmons, A.C. Association between Domestic Violence and HIV Serostatus among Married and Formerly Married Women in Kenya. Health Care Women Int. 2015, 36, 205–228. [Google Scholar] [CrossRef] [Green Version]
- Shi, C.; Kouyoumdjian, F.G.; Dushoff, J. Intimate Partner Violence Is Associated with HIV Infection in Women in Kenya: A Cross-Sectional Analysis. BMC Public Health 2013, 13, 512. [Google Scholar] [CrossRef] [Green Version]
- Seff, I.; Stark, L. A Sex-Disaggregated Analysis of How Emotional Violence Relates to Suicide Ideation in Low- and Middle-Income Countries. Child Abus. Negl. 2019, 93, 222–227. [Google Scholar] [CrossRef]
- Phillips-Howard, P.A.; Otieno, G.; Burmen, B.; Otieno, F.; Odongo, F.; Odour, C.; Nyothach, E.; Amek, N.; Zielinski-Gutierrez, E.; Odhiambo, F.; et al. Menstrual Needs and Associations with Sexual and Reproductive Risks in Rural Kenyan Females: A Cross-Sectional Sehavioral Survey Linked with HIV Prevalence. J. Womens Health 2015, 24, 801–811. [Google Scholar] [CrossRef]
- Kinuthia, J.; Singa, B.; McGrath, C.J.; Odeny, B.; Langat, A.; Katana, A.; Ng’ang’a, L.; Pintye, J.; John-Stewart, G. Prevalence and Correlates of Non-Disclosure of Maternal HIV Status to Male Partners: A National Survey in Kenya. BMC Public Health 2018, 18, 671. [Google Scholar] [CrossRef] [PubMed]
- Goyette, M.; Mutiti, P.; Bukusi, D.; Wamuti, B.M.; Otieno, F.A.; Cherutich, P.; Golden, M.R.; Spiegel, H.; Richardson, B.A.; Ng’ang’a, A.; et al. HIV Assisted Partner Services among Those with and without a History of Intimate Partner Violence in Kenya. J. Acquir. Immune Defic. Syndr. 2018, 78, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Wagman, J.A.; Charvat, B.; Thoma, M.E.; Ndyanabo, A.; Nalugoda, F.; Ssekasanvu, J.; Kigozi, G.; Serwadda, D.; Kagaayi, J.; Wawer, M.J.; et al. Intimate Partner Violence as a Predictor of Marital Disruption in Rural Rakai, Uganda: A Longitudinal Study. Int. J. Public Health 2016, 61, 961–970. [Google Scholar] [CrossRef] [PubMed]
- Kouyoumdjian, F.G.; Calzavara, L.M.; Bondy, S.J.; O’Campo, P.; Serwadda, D.; Nalugoda, F.; Kagaayi, J.; Kigozi, G.; Wawer, M.; Gray, R. Intimate Partner Violence Is Associated with Incident HIV Infection in Women in Uganda. AIDS Lond. Engl. 2013, 27, 1331–1338. [Google Scholar] [CrossRef] [PubMed]
- Speizer, I.S. Intimate Partner Violence Attitudes and Experience among Women and Men in Uganda. J. Interpers. Violence 2010, 25, 1224–1241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Macucha, C.M.; Taunde, S.A. Domestic Homicide in Maputo Province, Mozambique. Forensic Sci. Int. Online 2020, 2, 157–161. [Google Scholar] [CrossRef]
- Adjiwanou, V.; N’Bouke, A. Exploring the Paradox of Intimate Partner Violence and Increased Contraceptive Use in Sub-Saharan Africa. Stud. Fam. Plann. 2015, 46, 127–142. [Google Scholar] [CrossRef]
- Shamu, S.; Zarowsky, C.; Roelens, K.; Temmerman, M.; Abrahams, N. High-Frequency Intimate Partner Violence during Pregnancy, Postnatal Depression and Suicidal Tendencies in Harare, Zimbabwe. Gen. Hosp. Psychiatry 2016, 38, 109–114. [Google Scholar] [CrossRef] [Green Version]
- Shamu, S.; Munjanja, S.; Zarowsky, C.; Shamu, P.; Temmerman, M.; Abrahams, N. Intimate Partner Violence, Forced First Sex and Adverse Pregnancy Outcomes in a Sample of Zimbabwean Women Accessing Maternal and Child Health Care. BMC Public Health 2018, 18, 595. [Google Scholar] [CrossRef] [PubMed]
- Nyamukoho, E.; Mangezi, W.; Marimbe, B.; Verhey, R.; Chibanda, D. Depression among HIV Positive Pregnant Women in Zimbabwe: A Primary Health Care Based Cross-Sectional Study. BMC Pregnancy Childbirth 2019, 19, 53. [Google Scholar] [CrossRef]
- Kayibanda, J.F.; Alary, M. Trends and Risk Factors Associated with the Perpetration of Physical Intimate Partner Violence by Women in Haiti, 2000–2012. Women Health 2020, 60, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Gage, A.J. Exposure to Spousal Violence in the Family, Attitudes and Dating Violence Perpetration among High School Students in Port-Au-Prince. J. Interpers. Violence 2016, 31, 2445–2474. [Google Scholar] [CrossRef]
- Saxena, A.; Deschamps, M.; Dorvil, N.; Christophe, I.; Rosenberg, R.; Jean-Gilles, M.; Koenig, S.; Pape, J.W.; Dévieux, J.G. Association between Intimate Partner Violence and HIV Status among Haitian Women. Glob. Public Health 2019, 14, 1557–1568. [Google Scholar] [CrossRef] [PubMed]
- Occean, J.R.; Thomas, N.; Lim, A.C.; Lovett, S.M.; Michael-Asalu, A.; Salinas-Miranda, A.A. Prevalence and Factors Associated with Intimate Partner Violence among Women in Haiti: Understanding Household, Individual, Partner, and Relationship Characteristics. J. Interpers. Violence 2020, 1–29. [Google Scholar] [CrossRef]
- Zalla, L.C.; Herce, M.E.; Edwards, J.K.; Michel, J.; Weir, S.S. The Burden of HIV among Female Sex Workers, Men Who Have Sex with Men and Transgender Women in Haiti: Results from the 2016 Priorities for Local AIDS Control Efforts (PLACE) Study. J. Int. AIDS Soc. 2019, 22, e25281. [Google Scholar] [CrossRef]
- Bellizzi, S.; Nivoli, A.; Salaris, P.; Ronzoni, A.R.; Pichierri, G.; Palestra, F.; Wazway, O.; Luque-Fernandez, M.A. Sexual Violence and Eclampsia: Analysis of Data from Demographic and Health Surveys from Seven Low-and Middle-Income Countries. J. Glob. Health 2019, 9, 020434. [Google Scholar] [CrossRef]
- Gibbs, A.; Corboz, J.; Jewkes, R. Factors Associated with Recent Intimate Partner Violence Experience amongst Currently Married Women in Afghanistan and Health Impacts of IPV: A Cross Sectional Study. BMC Public Health 2018, 18, 593. [Google Scholar] [CrossRef] [Green Version]
- Aye, W.T.; Lien, L.; Stigum, H.; Schei, B.; Sundby, J.; Bjertness, E. Domestic Violence Victimisation and Its Association with Mental Distress: A Cross-Sectional Study of the Yangon Region, Myanmar. BMJ Open 2020, 10, e037936. [Google Scholar] [CrossRef]
- Tsai, L.C.; Cappa, C.; Petrowski, N. The Relationship between Intimate Partner Violence and Family Planning among Girls and Young Women in the Philippines. Glob. J. Health Sci. 2016, 8, 121–131. [Google Scholar] [CrossRef]
- Falb, K.L.; McCormick, M.C.; Hemenway, D.; Anfinson, K.; Silverman, J.G. Symptoms Associated with Pregnancy Complications along the Thai-Burma Border: The Role of Conflict Violence and Intimate Partner Violence. Matern. Child Health J. 2014, 18, 29–37. [Google Scholar] [CrossRef]
- Fellmeth, G.; Plugge, E.; Fazel, M.; Oo, M.M.; Pimanpanarak, M.; Phichitpadungtham, Y.; Wai, K.; Charunwatthana, P.; Simpson, J.A.; Nosten, F.; et al. Prevalence and Determinants of Perinatal Depression among Labour Migrant and Refugee Women on the Thai-Myanmar Border: A Cohort Study. BMC Psychiatry 2020, 20, 168. [Google Scholar] [CrossRef] [Green Version]
- Gibbs, A.; Said, N.; Corboz, J.; Jewkes, R. Factors Associated with ‘Honour Killing’ in Afghanistan and the Occupied Palestinian Territories: Two Cross-Sectional Studies. PLoS ONE 2019, 14, e0219125. [Google Scholar] [CrossRef] [Green Version]
- Misch, E.S.; Yount, K.M. Intimate Partner Violence and Breastfeeding in Africa. Matern. Child Health J. 2014, 18, 688–697. [Google Scholar] [CrossRef]
- Gámez, A.M.; Speizer, I.S. Community-Level Intimate Partner Violence and the Circumstances of First Sex among Young Women from Five African Countries. Reprod. Health 2010, 7, 11. [Google Scholar] [CrossRef] [Green Version]
- Bermudez, L.G.; Stark, L.; Bennouna, C.; Jensen, C.; Potts, A.; Kaloga, I.F.; Tilus, R.; Buteau, J.E.; Marsh, M.; Hoover, A.; et al. Converging Drivers of Interpersonal Violence: Findings from a Qualitative Study in Post-Hurricane Haiti. Child Abuse Negl. 2019, 89, 178–191. [Google Scholar] [CrossRef]
- Marsh, M.; Blake, M. Where Is the Money? How the Humanitarian System Is Failing in Its Commitments to End Violence against Women and Girls; IRC. 2019. Available online: https://www.rescue.org/report/wheres-money-how-humanitarian-system-failing-fund-end-violence-against-women-and-girls (accessed on 10 June 2019).
- Schölmerich, V.L.N.; Kawachi, I. Translating the Socio-Ecological Perspective into Multilevel Interventions: Gaps between Theory and Practice. Health Educ. Behav. 2016, 43, 17–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Golden, S.D.; McLeroy, K.R.; Green, L.W.; Earp, J.A.L.; Lieberman, L.D. Upending the Social Ecological Model to Guide Health Promotion Efforts toward Policy and Environmental Change. Health Educ. Behav. 2015, 42 (Suppl. 1), 8S–14S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- IASC. IASC System-Wide Response Activations and Deactivations. Available online: https://interagencystandingcommittee.org/iasc-transformative-agenda/iasc-system-wide-response-activations-and-deactivations (accessed on 21 December 2020).
- ACAPS. INFORM Global Crisis Severity Index: Guidance Note; ACAPS: Geneva, Switzerland, 2020. [Google Scholar]
- UNGA. Transforming Our World: The 2030 Agenda for Sustainable Development; UNGA: New York, NY, USA, 2015. [Google Scholar]
| # | Citation | Year(s) of Data Collection | Country of Data Collection | Study Type | Study Name | Temporality | Primary Analysis Model | Outcome Variable(s) ++++ | Quality Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Middle East | |||||||||
| 1 | Goessmann, Ibrahim, and Neuner, 2020 [37] | 2018–2019 | Iraqi Kurdistan | Other non-population based design | Not stated | Cross-sectional | Multi-variable hierarchical regression |
| Top category |
| 2 | Al-Atrushi et al., 2013 [38] | 2009–2011 | Iraqi Kurdistan | Other non-population based design | Not stated | Cross-sectional | Descriptive analysis of women who reported lifetime IPV |
| Lower-middle category |
| 3 | Zakar et al., 2012 [39] | 2008–2009 | Pakistan | Other non-population based design | Not stated | Cross-sectional | Multi-variable logistic regression (forms of violence included within separate models) |
| Top category |
| 4 | Zakar et al., 2013 [40] | 2008–2009 | Pakistan | Other non-population based design | Not stated | Cross-sectional | Multi-variable logistic regression (different forms of violence in separate models) |
| Top category |
| 5 | Sousa et al., 2018 [41] | 2007–2008 | Palestine | Other non-population based design | Not stated | Cross-sectional | Multi-variable regression (all forms of violence included within same model) |
| Lower-middle category |
| 6 | Falb et al., 2019 [42] | 2018 | Syria | Intervention study | Not stated (cash transfer program) | Cross-sectional (baseline) | Multi-variable linear regression (all forms of violence included within same model) |
| Top category |
| West Africa and the Sahel Region | |||||||||
| 7 | Fiorentino et al., 2019 [43] | 2014 | Cameroon | Other non-population based design | ANRS-12288 EVOLCam | Cross-sectional | Multi-variable logistic regression |
| Top category |
| 8 | Peltzer and Pengpid, 2014 [44] | 2011–2012 | Ivory Coast | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression |
| Upper-middle category |
| 9 | Alenko, et al., 2020 [45] | 2019 | Ethiopia | Other non-population based design | Not stated | Cross-sectional | Multi-variable logistic regression |
| Top category |
| 10 | Gebreslasie et al., 2020 [46] | 2017–2018 | Ethiopia | Other non-population based design | Not stated | Cross-sectional | Multi-variable logistic regression |
| Top category |
| 11 | Sipsma et al., 2013 [47] | 2007 | Liberia | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression (all forms of violence included within same model) |
| Upper-middle category |
| 12 | Sobkoviak, Yount, and Halim, 2012 [48] | 2007 | Liberia | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable linear or logistic regression (all forms of violence included within same model) |
| Upper-middle category |
| 13 | Hayes and van Baak, 2017 [49] | 2012–2013 | Mali | Population-based design | Demographic Health Survey | Cross-sectional | Logistic regression |
| Upper-middle category |
| 14 | DeLong et al., 2020 [50] | 2016 | Niger | Other non-population-based design | RMA study | Cross-sectional (baseline) | Multi-variable logistic regression (violence typologies included within same model & separate models for girls 15–16 & 17–19 years old) |
| Upper-middle category |
| 15 | Silverman et al., 2020 [51] | 2016 | Niger | Intervention study | RMA study | Cross-sectional (baseline) | Multi-variable logistic regression (violence typologies included within same model) |
| Upper-middle category |
| 16 | Kana, et al., 2020 [52] | 2017–2019 | Nigeria | Other non-population based design | Not stated | Cross-sectional | Multi-variable logistic regression |
| Top category |
| 17 | Abiodun et al., 2020 [53] | 2019 | Nigeria | Other non-population based design | not stated | Cross-sectional | Multi-variable logistic regression |
| Top category |
| Southern and Eastern Africa | |||||||||
| 18 | Kidman, Palermo and Bertrand, 2015 [54] | 2007 | Democratic Republic of Congo | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression (separate models for each form of IPV) |
| Upper-middle category |
| 19 | Fleming et al., 2015 [55] | 2009–2012 | Democratic Republic of Congo + | Intervention study | IMAGES | Cross-sectional (baseline) | Multi-variable logistic regression |
| Top category |
| 20 | Johnson et al., 2010 [56] | 2010 | Democratic Republic of Congo | Population-based design ++ | Not stated | Cross-sectional | Bivariate comparisons of prevalence calculated using the adjusted Wald test of association (modeled for males and females) |
| Upper-middle category |
| 21 | Gichane et al., 2018 [57] | 2013–2014 | Democratic Republic of Congo | Intervention study | Unnamed—Conditional Cash Transfer study | Longitudinal | Adjusted prevalence ratios (forms of violence included within separate models) |
| Top category |
| 22 | Tiruneh et al., 2018 [58] | 2013–2014 | Democratic Republic of the Congo | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression (two models: one with physical, sexual, and emotional IPV as separate variables, and the second with any IPV) +++ |
| Upper-middle category |
| 23 | Mpody et al., 2019 [59] | 2016–2018 | Democratic Republic of Congo | Intervention study | CQI-PMTCT study | Cross-sectional (baseline) | Multi-variable logistic regression (separate models based on pregnancy status during enrollment) |
| Upper-middle category |
| 24 | Onsomu et al., 2015 [60] | 2008–2009 | Kenya | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression (separate models for each form of IPV) |
| Top category |
| 25 | Shi, Kouyoumdjian and Dushoff, 2013 [61] | 2008–2009 | Kenya | Population-based design | Demographic Health Survey | Cross-sectional | Generalized linear mixed models |
| Top category |
| 26 | Seff and Stark, 2019 [62] | 2010 | Kenya + | Population-based design ++ | Violence Against Children Surveys | Cross-sectional | Multi-variable logistic regression (separate models for males and females) |
| Upper-middle category |
| 27 | Phillips-Howard et al., 2015 [63] | 2011–2012 | Kenya | Other non-population based design | Not stated | Cross-sectional | Multi-variable logistic regression (separate models for married and never-married women) |
| Upper-middle category |
| 28 | Kinuthia et al., 2018 [64] | 2013 | Kenya | Other non-population based design | Not stated | Cross-sectional | Multi-variable logistic regression |
| Top category |
| 29 | Goyette et al., 2018 [65] | 2013–2015 | Kenya | Intervention study | not stated | Longitudinal | Log-binomial generalized estimated equation |
| Upper-middle category |
| 30 | Wagman et al., 2016 [66] | 1999–2006 | Uganda | Intervention study | RCCS in Rakai | Longitudinal | Multi-variable linear regressions (all forms of violence included within same model and model includes an aggregate of each wave of data collection) |
| Upper-middle category |
| 31 | Kouyoumdjian et al., 2013 [67] | 2000–2009 | Uganda | Intervention study | RCCS in Rakai | Longitudinal | Multi-variable population attributable fraction (separate models for forms of IPV) |
| Top category |
| 32 | Speizer, 2010 [68] | 2006 | Uganda | Population-based design ++ | Demographic Health Survey | Cross-sectional | Multi-variable multinomial logistic regression (separate models for married or unionized men and women) |
| Upper-middle category |
| 33 | Macucha and Taunde, 2020 [69] | 2016–2017 | Mozambique | Retrospective case review | Not stated | Cross-sectional | Descriptive analysis of autopsy reports |
| Upper-middle category |
| 34 | Adjiwan and N’Bouke, 2015 [70] | 2010 | Zimbabwe + | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable probit model |
| Upper-middle category |
| 35 | Shamu et al., 2016 [71] | 2011 | Zimbabwe | Other non-population based design | not stated | Cross-sectional | Multi-variable logistic regression (all forms of violence included within same model) |
| Upper-middle category |
| 36 | Shamu et al., 2018 [72] | 2011 | Zimbabwe | Other non-population based design | Not stated | Cross-sectional | Multi-variable logistic regression (all forms of violence included within same model) |
| Upper-middle category |
| 37 | Nyamukoho et al., 2019 [73] | 2016 | Zimbabwe | Other non-population based design | Not stated | Cross sectional | Logistic regression |
| Lower-middle category |
| Caribbean | |||||||||
| 38 | Kayibanda and Alary, 2020 [74] | 2000, 2005, 2012 | Haiti | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable analysis adjusted prevalence ratios (all forms of violence included within same model) |
| Upper-middle category |
| 39 | Gage, 2016 [75] | 2013 | Haiti | Intervention study ++ | SAFE Dates | Cross-sectional (baseline) | Multi-variable logistic regression (both forms of violence included in model and separate models for males and females) |
| Upper-middle category |
| 40 | Saxena et al., 2019 [76] | 2013 | Haiti | Intervention study | GHESKIO | Cross-sectional (baseline) | Multi-variable logistic regression (all violence forms included within same model) |
| Upper-middle category |
| 41 | Occean et al., 2020 [77] | 2016–2017 | Haiti | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression |
| Upper-middle category |
| 42 | Zalla et al., 2019 [78] | 2016–2017 | Haiti | Other non-population based design | Local AIDS Control Efforts (PLACE) study | Cross-sectional | Bivariate log-binomial regression (separate models for each group—MSM, FSW, TWG) |
| Upper-middle category |
| Central and Southeast Asia | |||||||||
| 43 | Bellizzi et al., 2019 [79] | 2015 | Afghanistan + | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression |
| Upper-middle category |
| 44 | Gibbs, Corboz, and Jewkes, 2018 [80] | 2016–2017 | Afghanistan | Intervention study | WfWI trial | Cross-sectional (baseline) | Multi-variable linear regressions (separate models for forms and rates of IPV) |
| Upper-middle category |
| 45 | Aye, et al., 2020 [81] | 2016 | Myanmar | Population-based design ++ | Demographic Health Survey | Cross-sectional | Multi-variablelinear regression |
| Top category |
| 46 | Tsai, Cappa and Petrowski, 2016 [82] | 2013 | Philippines | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression (separate models for each form of IPV) |
| Upper-middle category |
| 47 | Falb et al., 2014 [83] | 2008 | Thai-Myanmar Border | Other non-population based design | Reproductive Health Assessment Toolkit for Conflict-Affected women | Cross-sectional | Multi-variable generalized estimated equations |
| Upper-middle category |
| 48 | Fellmeth et al., 2020 [84] | 2015–2016 | Thai-Myanmar Border | Other non-population based design | Not stated | Longitudinal | Multi-variable logistic regression |
| Upper-middle category |
| Multiple Countries | |||||||||
| 49 | Gibbs et al., 2019 [85] | 2016–2017 2017 | Afghanistan Palestine | Afghanistan: Intervention study Palestine: Population-based design | Afghanistan: WfWI Palestine: not stated | Cross-sectional (baseline) Cross-sectional | Multi-variable logistic regression |
| Upper-middle category |
| 50 | Misch and Yount, 2014 [86] | 2008–2009 2007 2010–2011 | Kenya Liberia Zimbabwe + | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression (violence typologies included within same model) |
| Upper-middle category |
| 51 | Gámez and Speizer, 2010 [87] | 2007 2007 2005–2006 | Liberia DRC Zimbabwe + | Population-based design | Demographic Health Survey | Cross-sectional | Multi-variable logistic regression |
| Upper-middle category |
| Impact Categories, by Level of Ecological Framework | Corresponding Article | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | |
| Individual/survivor level | |||||||||||||||||||
| HIV and other sexually transmitted infections | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Pregnancy, birth, and infancy | - | - | - | - | - | - | - | - | - | S | - | - | - | - | - | S | - | - | - |
| Substance use | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Mental health | S | - | - | S | S | S | - | - | - | - | - | - | - | - | - | - | - | - | |
| Overall health | - | N/A | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Fatal injuries | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Reproductive health | - | - | S | - | - | - | - | - | - | - | - | - | - | S | S | - | - | S | - |
| Perpetration | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Revictimization | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | S | - | - |
| Healthcare access, adherence, or disclosure | - | - | - | - | - | - | NS | - | - | - | S | - | - | - | - | - | - | - | - |
| Microsystem/relationship level | |||||||||||||||||||
| IPV perpetration during adulthood (children) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NS |
| Lifetime IPV victimization (children) | - | - | - | - | - | - | - | S | - | - | - | - | S | - | - | - | - | - | - |
| Physical health conditions (children) | - | - | - | - | - | - | - | - | - | - | - | S | - | - | - | - | - | - | - |
| Emotional/behavioral problems (children) | - | - | - | - | - | - | - | - | S | - | - | - | - | - | - | - | - | - | - |
| Accepting attitudes of IPV (children) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Martial disruption (partners) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Fatal injuries (familial homicides) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Impact Categories, by Level of Ecological Framework | Corresponding Article | ||||||||||||||||||
| 20 | 21 | 22 + | 23 | 24 | 25 | 26 | 28 | 29 | 30 | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 | 39 | |
| Individual/survivor level | |||||||||||||||||||
| HIV and other sexually transmitted infections | - | NS | - | S | S | S | - | - | - | - | S | - | - | - | - | - | - | - | - |
| Pregnancy, birth, and infancy | - | - | S | - | - | - | - | - | - | - | - | - | - | - | - | S | - | - | - |
| Substance use | NS | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Mental health | S | - | - | - | - | - | S | - | - | - | - | - | - | S | - | S | - | - | |
| Overall health | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Fatal injuries | - | - | - | - | - | - | - | - | - | - | - | - | N/A | - | - | - | - | - | - |
| Reproductive health | - | - | - | - | - | - | - | - | - | - | - | - | - | NS | - | - | - | - | - |
| Perpetration | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | S | - |
| Revictimization | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Healthcare access, adherence, or disclosure | - | NS | - | - | - | - | - | S | NS | - | - | - | - | - | - | - | - | - | - |
| Microsystem/relationship level | |||||||||||||||||||
| IPV perpetration during adulthood (children) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | S | S |
| Lifetime IPV victimization (children) | - | - | S | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Emotional/behavioral problems (children) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Physical health conditions (children) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Accepting attitudes of IPV (children) | - | - | - | - | - | - | - | - | - | - | - | S | - | - | - | - | - | - | - |
| Martial disruption (partners) | - | - | - | - | - | - | - | - | - | S | - | - | - | - | - | - | - | - | - |
| Fatal injuries (familial homicides) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Impact Categories, by Level of Ecological Framework | Corresponding Article | ||||||||||||||||||
| 40 | 41 | 42 | 43 | 44 | 45 | 46 | 47 | 48 | 49 | 50 | 51 | ||||||||
| Individual/survivor level | |||||||||||||||||||
| HIV and other sexually transmitted infections | S | - | S | - | - | - | - | - | - | - | - | - | |||||||
| Pregnancy, birth, and infancy | - | - | - | S | - | - | - | NS | - | - | S | - | |||||||
| Substance use | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Mental health | - | - | - | - | S | S | - | - | S | - | - | ||||||||
| Overall health | - | - | - | - | S | - | - | - | - | - | - | - | |||||||
| Fatal injuries | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Reproductive health | - | - | - | - | - | - | S | - | - | - | - | NS | |||||||
| Perpetration | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Revictimization | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Healthcare access, adherence, or disclosure | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Microsystem/relationship level | |||||||||||||||||||
| IPV perpetration during adulthood (children) | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Lifetime IPV victimization (children) | - | S | - | - | - | - | - | - | - | - | - | - | |||||||
| Emotional/behavioral problems (children) | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Physical health conditions (children) | - | - | - | - | - | - | - | - | - | - | - | ||||||||
| Accepting attitudes of IPV (children) | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Martial disruption (partners) | - | - | - | - | - | - | - | - | - | - | - | - | |||||||
| Fatal injuries (familial homicides) | - | - | - | - | - | - | - | - | - | S | - | - | |||||||
| IPV Variable Classification, by Level | Corresponding Article Number | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | |||
| Personal victimization of intimate partner violence | |||||||||||||||||||||
| Timeframe | Lifetime | - | x | x | x | x | - | x | - | - | - | x | - | - | x | x | - | - | x | - | |
| Current partnership | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Previous partnership | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | x | - | - | ||
| Past 12-mo or past year | x | - | - | x | - | - | - | - | - | - | - | x | - | - | - | - | - | - | - | ||
| Past 3-months | - | - | - | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Past 1-month | - | - | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| During pregnancy | - | - | - | - | - | - | - | - | - | x | - | - | - | - | - | x | - | - | - | ||
| Last incidence | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Forms | Multiple forms or any IPV | x | - | - | - | x | - | x | - | - | x | - | x | - | - | - | x | x | x | - | |
| AGBH | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Emotional | - | - | - | - | - | x | - | - | - | - | - | - | - | - | - | x | - | - | - | ||
| Physical | - | x | x | x | - | x | - | - | - | - | x | - | - | x | x | x | - | - | - | ||
| Physiological | - | - | x | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Sexual | - | - | x | x | - | x | - | - | - | - | x | x | - | x | x | x | - | x | - | ||
| Verbal | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Measurement | Nominal (binary) | x | x | x | - | - | x | x | - | - | x | x | - | - | x | x | x | x | x | - | |
| Nominal (>2 categories) | - | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Ordinal | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Interval | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Ratio | - | - | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Childhood witnessing of intimate partner violence between parents | |||||||||||||||||||||
| Timeframe | During childhood | - | - | - | - | - | - | - | x | x | - | - | x | x | - | - | - | - | - | x | |
| Forms | Multiple forms or any IPV | - | - | - | - | - | - | - | x | x | - | - | x | x | - | - | - | - | - | x | |
| Physical | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Measurement | Nominal (binary) | - | - | - | - | - | - | - | x | x | - | - | x | x | - | - | - | - | - | x | |
| Community rates of intimate partner violence | |||||||||||||||||||||
| Timeframe | Lifetime of respondents | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Past 5-years | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | x | - | ||
| Forms | Multiple forms | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | x | - | |
| Physical | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Sexual | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | x | - | ||
| Measurement | Nominal (binary) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Ordinal | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | ||
| Ratio | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | x | - | ||
| IPV Variable Classification, by Level | Corresponding Article Number | ||||||||||||||||||||
| 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 + | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 | 39 | ||
| Personal victimization of intimate partner violence | |||||||||||||||||||||
| Timeframe | Lifetime | x | x | x | x | x | x | x | x | - | x | - | x | - | - | - | x | x | x | x | - |
| Current partnership | - | - | - | - | - | - | - | - | x | - | - | - | - | - | x | - | - | - | - | - | |
| Previous partnership | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Past 12-mo or past year | - | - | - | - | - | - | - | - | - | - | x | - | - | - | - | - | x | - | - | - | |
| Past 3-months | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Past 1-month | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| During pregnancy | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | x | - | - | - | |
| Last incidence | - | - | - | - | - | - | - | - | - | - | - | - | - | x | - | - | - | - | - | - | |
| Forms | Multiple forms or any IPV | x | x | x | x | x | x | x | x | x | x | - | x | - | x | x | x | x | x | x | - |
| AGBH | - | - | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Emotional | - | x | x | - | x | - | - | - | - | - | x | - | - | - | - | x | x | - | - | - | |
| Physical | - | x | x | - | x | - | - | - | - | - | x | x | - | - | - | x | x | - | - | - | |
| Physiological | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Sexual | - | x | x | - | x | - | - | - | - | - | x | x | - | - | - | x | x | - | - | - | |
| Verbal | - | - | - | - | - | - | - | - | - | - | - | x | - | - | - | - | - | - | - | - | |
| Measurement | Nominal (binary) | x | x | x | x | x | - | x | x | x | x | x | x | - | x | x | - | x | x | x | - |
| Nominal (>2 categories) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Ordinal | - | - | - | - | - | - | - | - | - | - | - | x | - | - | - | x | - | - | - | - | |
| Interval | - | - | - | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Ratio | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Childhood witnessing of intimate partner violence between parents | |||||||||||||||||||||
| Timeframe | Lifetime of respondents | - | - | x | - | - | - | - | - | - | - | - | - | x | - | - | - | - | - | x | x |
| Forms | Multiple forms or any IPV | - | - | x | - | - | - | - | - | - | - | - | - | x | - | - | - | - | - | x | x |
| Physical | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Measurement | Nominal (binary) | - | - | x | - | - | - | - | - | - | - | - | - | x | - | - | - | - | - | x | x |
| Community rates of intimate partner violence | |||||||||||||||||||||
| Timeframe | Lifetime of respondents | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Past 5-years | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Forms | Multiple forms | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Physical | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Sexual | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Measurement | Nominal (binary) | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Ordinal | - | - | x | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Ratio | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| IPV Variable Classification, by Level | Corresponding Article Number | ||||||||||||||||||||
| 40 | 41 | 42 | 43 | 44 | 45 | 46 | 47 | 48 | 49 | 50 | 51 | ||||||||||
| Personal victimization of intimate partner violence | |||||||||||||||||||||
| Timeframe | Lifetime | x | - | - | x | x | x | - | x | x | - | - | - | ||||||||
| Current partnership | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Previous partnership | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Past 12-mo or past year | - | - | x | - | - | x | x | - | - | x | - | - | |||||||||
| Past 3-months | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Past 1-month | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| During pregnancy | - | - | - | - | - | - | - | - | - | - | x | - | |||||||||
| Last incidence | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Forms | Multiple forms or any IPV | - | - | - | - | - | x | - | x | x | - | - | - | ||||||||
| AGBH | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Emotional | - | - | - | - | x | x | x | - | - | - | x | - | |||||||||
| Physical | x | - | x | - | x | x | x | - | - | x | x | - | |||||||||
| Physiological | x | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Sexual | x | - | - | x | - | x | x | - | - | - | x | - | |||||||||
| Verbal | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Measurement | Nominal (binary) | x | - | x | x | - | x | x | x | x | x | x | - | ||||||||
| Nominal (>2 categories) | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Ordinal | - | - | - | - | x | - | - | - | - | - | - | - | |||||||||
| Interval | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Ratio | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Childhood witnessing of intimate partner violence between parents | |||||||||||||||||||||
| Timeframe | Lifetime of respondents | - | x | - | - | - | - | - | - | - | - | - | - | ||||||||
| Forms | Multiple forms or any IPV | - | x | - | - | - | - | - | - | - | - | - | - | ||||||||
| Physical | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Measurement | Nominal (binary) | - | x | - | - | - | - | - | - | - | - | - | - | ||||||||
| Community rates of intimate partner violence | |||||||||||||||||||||
| Timeframe | Lifetime of respondents | - | - | - | - | - | - | - | - | - | - | - | x | ||||||||
| Past 5-years | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Forms | Multiple forms | - | - | - | - | - | - | - | - | - | - | - | x | ||||||||
| Physical | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Sexual | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Measurement | Nominal (binary) | - | - | - | - | - | - | - | - | - | - | - | - | ||||||||
| Ordinal | - | - | - | - | - | - | - | - | - | - | - | - | |||||||||
| Ratio | - | - | - | - | - | - | - | - | - | - | - | x | |||||||||
| n | % | |
|---|---|---|
| Introduction | ||
| 1. Were the aims/objectives of the study clear? | 51 | 100.00% |
| Methods | ||
| 2. Was the study design appropriate for the stated aim(s)? + | 45 | 88.24% |
| 3. Was the sample size justified? | 28 | 54.90% |
| 4. Was the target/reference population clearly defined? (Is it clear who the research was about?) | 51 | 100.00% |
| 5. Was the sample frame taken from an appropriate population base so that it closely represented the target/reference population under investigation? | 41 | 80.39% |
| 6. Was the selection process likely to select subjects/participants that were representative of the target/reference population under investigation? | 45 | 88.24% |
| 7. Were measures undertaken to address and categorize non-responders? | 23 | 45.10% |
|
7.a Were measures undertaken to categories non-responders (i.e., do the authors identify the non-response rate)? | 43 | 84.31% |
|
7.b Were measures undertaken to address non-responders (i.e., do the authors identify how the non-response rate was addressed)? | 25 | 49.02% |
| 8. Were the risk factor and outcome variables measured appropriately to the aims of the study? | 25 | 49.02% |
| 9. Were the risk factor and outcome variables measured correctly using instruments/measurements that had been trialed, piloted, or published previously? | 13 | 25.49% |
|
9.a Were the independent IPV variables measured correctly using instruments/ measurements that had been trialed, piloted, or published previously? | 24 | 47.06% |
|
9.b Were the outcome variables measured correctly using instruments/ measurements that had been trialed, piloted, or published previously? | 18 | 35.29% |
| 10. Is it clear what was used to determined statistical significance and/or precision estimates (e.g., p values, CIs) ? | 50 | 98.04% |
| 10.a Was sensitivity testing conducted? | 2 | 3.92% |
| 11. Were the methods (including statistical methods) sufficiently described to enable them to be repeated? | 37 | 72.55% |
| Results | ||
| 12. Were the basic data adequately described? | 49 | 96.08% |
| 13. Does the response rate raise concerns about non-response bias? +,++ | 2 | 3.92% |
| 14. If appropriate, was information about non-responders described? + | 1 | 1.96% |
| 15. Were the results internally consistent? | 28 | 54.90% |
| 15.a Were bivariate and multivariate analyses available? +++ | 33 | 64.71% |
| 16. Were the results for the analyses described in the methods, presented? | 50 | 98.04% |
| Discussion | ||
| 17. Were the authors’ discussions and conclusions justified by the results? | 47 | 92.16% |
| 18. Were the limitations of the study discussed? | 49 | 96.09% |
| Other | ||
| 19. Were there any funding sources or conflicts of interest that may affect the authors’ interpretation of the results? ++ | 23 | 45.10% |
| 20. Was ethical approval or consent of participants attained? | 35 | 68.63% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meinhart, M.; Seff, I.; Troy, K.; McNelly, S.; Vahedi, L.; Poulton, C.; Stark, L. Identifying the Impact of Intimate Partner Violence in Humanitarian Settings: Using an Ecological Framework to Review 15 Years of Evidence. Int. J. Environ. Res. Public Health 2021, 18, 6963. https://doi.org/10.3390/ijerph18136963
Meinhart M, Seff I, Troy K, McNelly S, Vahedi L, Poulton C, Stark L. Identifying the Impact of Intimate Partner Violence in Humanitarian Settings: Using an Ecological Framework to Review 15 Years of Evidence. International Journal of Environmental Research and Public Health. 2021; 18(13):6963. https://doi.org/10.3390/ijerph18136963
Chicago/Turabian StyleMeinhart, Melissa, Ilana Seff, Katrina Troy, Samantha McNelly, Luissa Vahedi, Catherine Poulton, and Lindsay Stark. 2021. "Identifying the Impact of Intimate Partner Violence in Humanitarian Settings: Using an Ecological Framework to Review 15 Years of Evidence" International Journal of Environmental Research and Public Health 18, no. 13: 6963. https://doi.org/10.3390/ijerph18136963
APA StyleMeinhart, M., Seff, I., Troy, K., McNelly, S., Vahedi, L., Poulton, C., & Stark, L. (2021). Identifying the Impact of Intimate Partner Violence in Humanitarian Settings: Using an Ecological Framework to Review 15 Years of Evidence. International Journal of Environmental Research and Public Health, 18(13), 6963. https://doi.org/10.3390/ijerph18136963






