Does Workers’ Compensation Status Affect Outcomes after Lumbar Spine Surgery? A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
Inclusion and Exclusion Criteria
- Peer-reviewed studies of every level of evidence according to the Oxford Classification. We included in our research RCT and NRCT.
- Studies including working patients with no limitations of age and type of work.
- Studies that reported outcomes for patients undergoing any type of surgical procedure involving the lumbar spine.
- Studies that included at least one assessment for each type of outcome (LBP, disability, satisfaction after surgery and RTW). The pain outcome had to be evaluated by one or more of the following scales: numerical pain rating scale (NRS) and visual analogue scale (VAS). The disability outcome needed to be evaluated by one or more of the following scales: Oswestry Disability Index (ODI); 36-Item Short Form Health Survey (SF-36); 12-Item Short Form Health Survey (SF-12); Roland Morris Disability Questionnaire (RMDQ); functional status (FS) and Lumbar Back Outcome Scale (LBOS). RTW was evaluated as the number of patients that went back to their previous working activities at the time of the last follow-up. The satisfaction rate after surgery was assessed in patients as follows: “Excellent”, “Good”, “Almost complete relief”, “Good deal of relief”, and “Satisfied” were considered as satisfactory outcomes, whereas “Fair”, “Poor”, “Only a little relief”, “No relief or worse” and “Unsatisfied” were considered unsatisfactory. Moreover, in studies where the satisfaction rate was expressed in a numeric scale, values between 0 and 4 were considered unsatisfactory, whilst values between 5 and 10 were considered satisfactory.
- Only articles written in English and Italian were included.
2.2. Search
2.3. Study Selection
2.4. Data Extraction
2.5. Individual Study Quality
2.6. Quality of Evidence
- High Quality of Evidence: among 75% of articles included are considered with a low risk bias. Further research is useful to change either the estimate or confidence in results.
- Moderate Quality of Evidence: one of the GRADE domains is not met. Further studies are required to improve the quality of the study and the evidence.
- Low Quality of Evidence: two of the GRADE domains are not met. Further research is critical.
- Very Low Quality of Evidence: three of the GRADE domains are not met. The results of the study are very uncertain. In the case of studies with a sample size inferior to 300 subjects, the quality of the study is considered very low if there was also a high risk of bias (assessed with the ROBINS-I in the present study).
2.7. Summary Measures
2.8. Synthesis of Results
3. Results
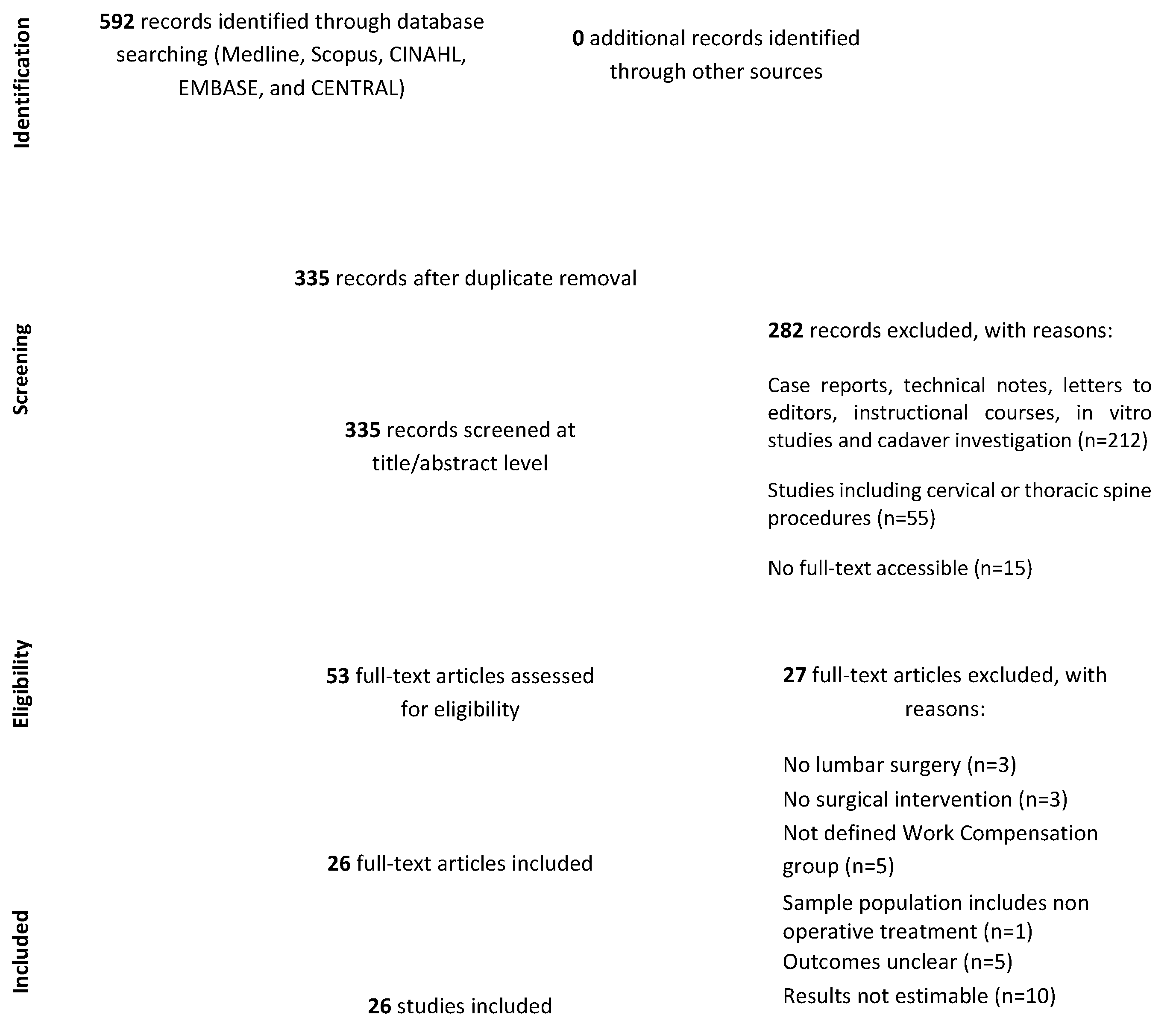
3.1. Study Selection
3.2. Study Characteristics
3.3. Methodological Quality
3.4. Results of Individual Studies
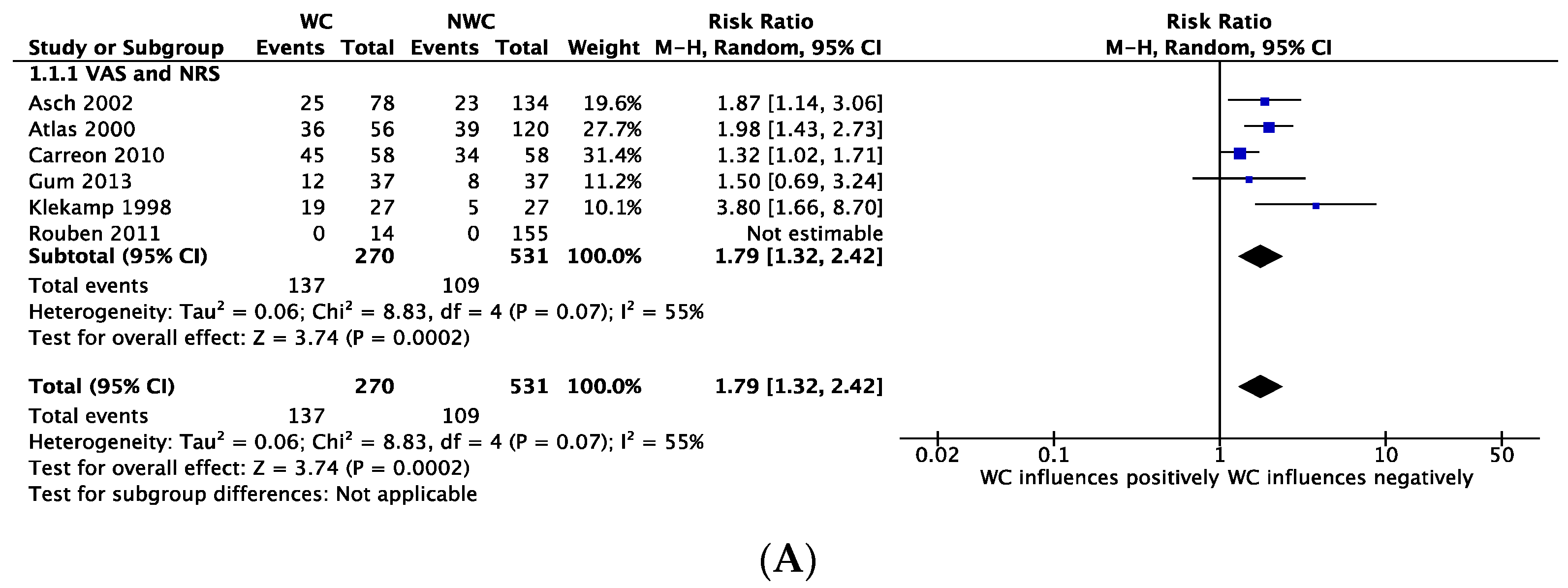
3.5. Outcome: Pain
3.6. Outcome: Disability
3.7. Outcome: Return to Work
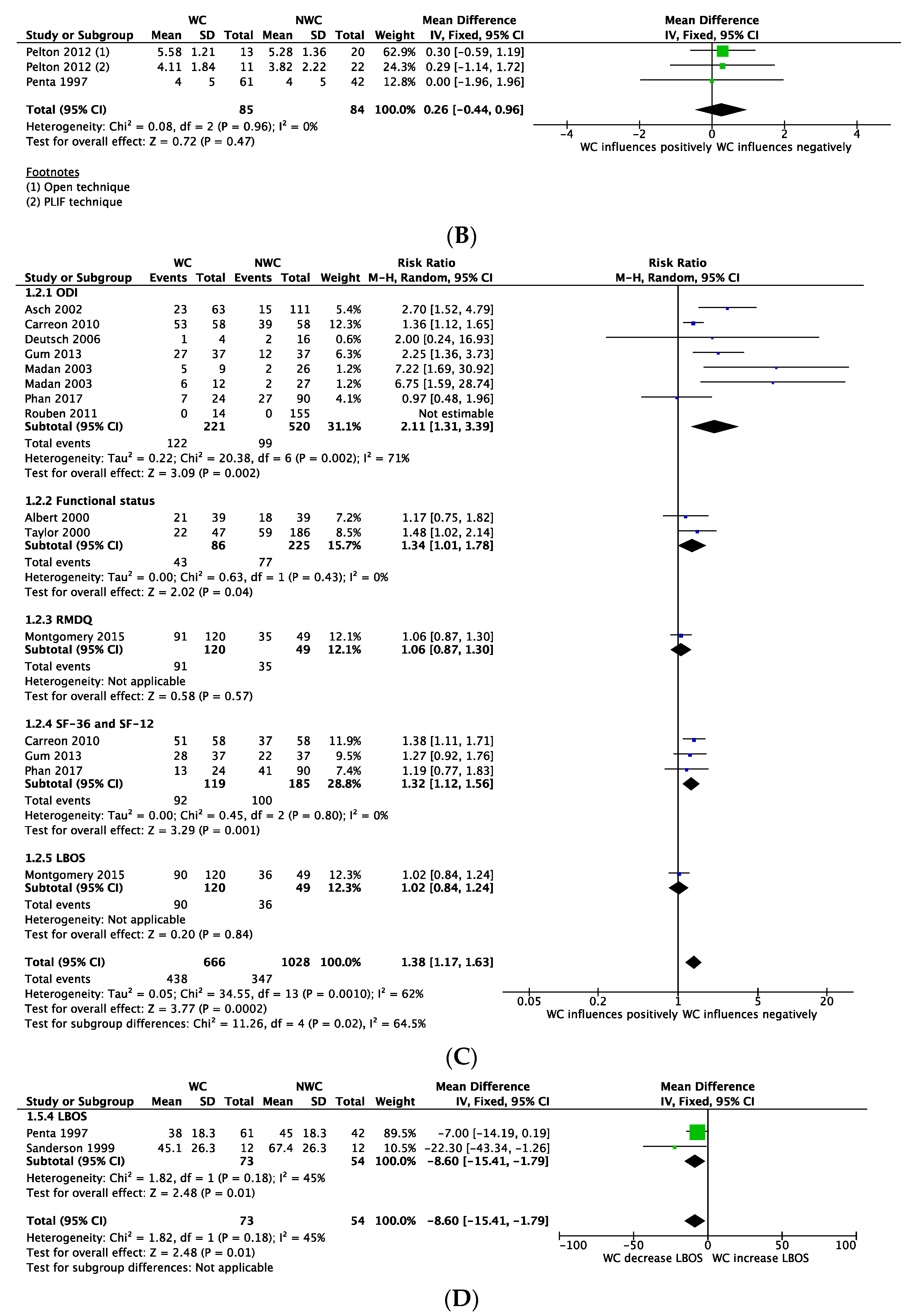
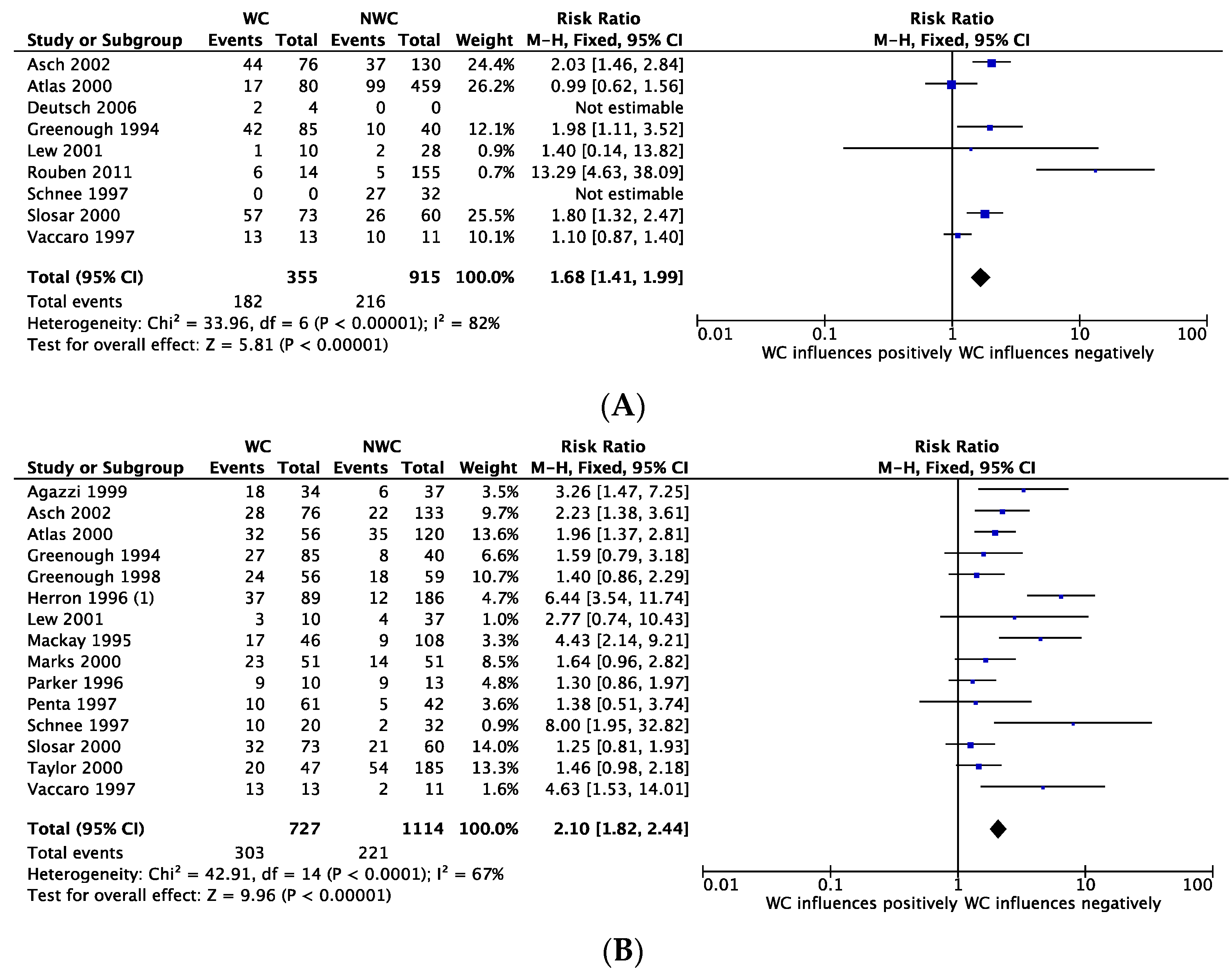
3.8. Outcome: Satisfaction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Disease, G.B.D.; Injury, I.; Prevalence, C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Franklin, G.M.; Wickizer, T.M.; Coe, N.B.; Fulton-Kehoe, D. Workers’ compensation: Poor quality health care and the growing disability problem in the United States. Am. J. Ind. Med. 2015, 58, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Kwon, B.K.; Vaccaro, A.R.; Grauer, J.N.; Beiner, J. Indications, techniques, and outcomes of posterior surgery for chronic low back pain. Orthop. Clin. N. Am. 2003, 34, 297–308. [Google Scholar] [CrossRef]
- Harris, I.; Mulford, J.; Solomon, M.; van Gelder, J.M.; Young, J. Association between compensation status and outcome after surgery: A meta-analysis. JAMA 2005, 293, 1644–1652. [Google Scholar] [CrossRef]
- Lippel, K.; Lotters, F. Public insurance systems: A comparison of cause-based and disability-based income support systems. In Handbook of Work Disability; Loisel, P., Anema, J., Eds.; Springer: New York, NY, USA, 2013; pp. 183–203. [Google Scholar]
- Gray, S.; Lane, T.; Sheehan, L.; Collie, A. Association between workers’ compensation claim processing times and work disability duration: Analysis of population level claims data. Health Policy 2019, 123, 982–991. [Google Scholar] [CrossRef] [PubMed]
- Kilgour, E.; Kosny, A.; McKenzie, D.; Collie, A. Interactions between injured workers and insurers in workers’ compensation systems: A systematic review of qualitative research literature. J. Occup. Rehabil. 2015, 25, 160–181. [Google Scholar] [CrossRef]
- Anderson, P.A.; Subach, B.R.; Riew, K.D. Predictors of outcome after anterior cervical discectomy and fusion: A multivariate analysis. Spine 2009, 34, 161–166. [Google Scholar] [CrossRef]
- Hou, W.H.; Tsauo, J.Y.; Lin, C.H.; Liang, H.W.; Du, C.L. Worker’s compensation and return-to-work following orthopaedic injury to extremities. J. Rehabil. Med. 2008, 40, 440–445. [Google Scholar] [CrossRef]
- Bhatia, S.; Piasecki, D.P.; Nho, S.J.; Romeo, A.A.; Cole, B.J.; Nicholson, G.P.; Boniquit, N.; Verma, N.N. Early return to work in workers’ compensation patients after arthroscopic full-thickness rotator cuff repair. Arthroscopy 2010, 26, 1027–1034. [Google Scholar] [CrossRef]
- Brinker, M.R.; Savory, C.G.; Weeden, S.H.; Aucoin, H.C.; Curd, D.T. The results of total knee arthroplasty in workers’ compensation patients. Bull. Hosp. Jt. Dis. 1998, 57, 80–83. [Google Scholar] [PubMed]
- Denard, P.J.; Ladermann, A.; Burkhart, S.S. Long-term outcome after arthroscopic repair of type II SLAP lesions: Results according to age and workers’ compensation status. Arthroscopy 2012, 28, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Holtby, R.; Razmjou, H. Impact of work-related compensation claims on surgical outcome of patients with rotator cuff related pathologies: A matched case-control study. J. Shoulder Elbow Surg. 2010, 19, 452–460. [Google Scholar] [CrossRef]
- Bartys, S.; Frederiksen, P.; Bendix, T.; Burton, K. System influences on work disability due to low back pain: An international evidence synthesis. Health Policy 2017, 121, 903–912. [Google Scholar] [CrossRef]
- Gum, J.L.; Glassman, S.D.; Carreon, L.Y. Is type of compensation a predictor of outcome after lumbar fusion? Spine 2013, 38, 443–448. [Google Scholar] [CrossRef]
- Siambanes, D.; Miz, G.S. Treatment of symptomatic anterior cervical nonunion using the Rogers interspinous wiring technique. Am. J. Orthop. 1998, 27, 792–796. [Google Scholar]
- Madan, S.S.; Boeree, N.R. Comparison of instrumented anterior interbody fusion with instrumented circumferential lumbar fusion. Eur. Spine J. 2003, 12, 567–575. [Google Scholar] [CrossRef]
- Kohl, C.; McIntosh, E.J.; Unger, S.; Haddaway, N.R.; Kecke, S.; Schiemann, J.; Wilhelm, R. Online tools supporting the conduct and reporting of systematic reviews and systematic maps: A case study on CADIMA and review of existing tools. Environ. Evid. 2018, 7, 8. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- NASS. Levels of Evidence for Primary Research Question. Available online: https://www.spine.org/Portals/0/Assets/Downloads/ResearchClinicalCare/LevelsofEvidence.pdf (accessed on 26 April 2021).
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Agazzi, S.; Reverdin, A.; May, D. Posterior lumbar interbody fusion with cages: An independent review of 71 cases. J. Neurosurg. 1999, 91, 186–192. [Google Scholar] [CrossRef]
- Albert, T.J.; Pinto, M.; Denis, F. Management of symptomatic lumbar pseudarthrosis with anteroposterior fusion. A functional and radiographic outcome study. Spine 2000, 25, 123–129. [Google Scholar] [CrossRef]
- Asch, H.L.; Lewis, P.J.; Moreland, D.B.; Egnatchik, J.G.; Yu, Y.J.; Clabeaux, D.E.; Hyland, A.H. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: Should 75 to 80% success rates be the norm? J. Neurosurg. 2002, 96, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Atlas, S.J.; Chang, Y.; Kammann, E.; Keller, R.B.; Deyo, R.A.; Singer, D.E. Long-term disability and return to work among patients who have a herniated lumbar disc: The effect of disability compensation. J. Bone Jt. Surg. Am. 2000, 82, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Carreon, L.Y.; Glassman, S.D.; Kantamneni, N.R.; Mugavin, M.O.; Djurasovic, M. Clinical outcomes after posterolateral lumbar fusion in workers’ compensation patients: A case-control study. Spine 2010, 35, 1812–1817. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, H.; Musacchio, M.J., Jr. Minimally invasive transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Neurosurg. Focus 2006, 20, E10. [Google Scholar] [CrossRef]
- Greenough, C.G.; Taylor, L.J.; Fraser, R.D. Anterior lumbar fusion: Results, assessment techniques and prognostic factors. Eur. Spine J. 1994, 3, 225–230. [Google Scholar] [CrossRef]
- Greenough, C.G.; Peterson, M.D.; Hadlow, S.; Fraser, R.D. Instrumented posterolateral lumbar fusion. Results and comparison with anterior interbody fusion. Spine 1998, 23, 479–486. [Google Scholar] [CrossRef]
- Herron, L.D.; Turner, J.A.; Novell, L.A.; Kreif, S.L. Patient selection for lumbar discectomy with a revised objective rating system. Clin. Orthop. Relat. Res. 1996, 148–155. [Google Scholar] [CrossRef]
- Klekamp, J.; McCarty, E.; Spengler, D.M. Results of elective lumbar discectomy for patients involved in the workers’ compensation system. J. Spinal Disord. 1998, 11, 277–282. [Google Scholar] [CrossRef]
- Lew, S.M.; Mehalic, T.F.; Fagone, K.L. Transforaminal percutaneous endoscopic discectomy in the treatment of far-lateral and foraminal lumbar disc herniations. J. Neurosurg. 2001, 94, 216–220. [Google Scholar] [CrossRef]
- MacKay, M.A.; Fischgrund, J.S.; Herkowitz, H.N.; Kurz, L.T.; Hecht, B.; Schwartz, M. The effect of interposition membrane on the outcome of lumbar laminectomy and discectomy. Spine 1995, 20, 1793–1796. [Google Scholar] [CrossRef]
- Marks, R.A. Transcutaneous lumbar diskectomy for internal disk derangement: A new indication. South. Med. J. 2000, 93, 885–890. [Google Scholar] [PubMed]
- Montgomery, A.S.; Cunningham, J.E.; Robertson, P.A. The Influence of No Fault Compensation on Functional Outcomes After Lumbar Spine Fusion. Spine 2015, 40, 1140–1147. [Google Scholar] [CrossRef]
- Parker, L.M.; Murrell, S.E.; Boden, S.D.; Horton, W.C. The outcome of posterolateral fusion in highly selected patients with discogenic low back pain. Spine 1996, 21, 1909–1916. [Google Scholar] [CrossRef]
- Pelton, M.A.; Phillips, F.M.; Singh, K. A comparison of perioperative costs and outcomes in patients with and without workers’ compensation claims treated with minimally invasive or open transforaminal lumbar interbody fusion. Spine 2012, 37, 1914–1919. [Google Scholar] [CrossRef] [PubMed]
- Penta, M.; Fraser, R.D. Anterior lumbar interbody fusion. A minimum 10-year follow-up. Spine 1997, 22, 2429–2434. [Google Scholar] [CrossRef]
- Phan, K.; Davies, S.; Rao, P.J.; Mobbs, R.J. Worker’s Compensation Status and Outcomes Following Anterior Lumbar Interbody Fusion: Prospective Observational Study. World Neurosurg. 2017, 103, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Rouben, D.; Casnellie, M.; Ferguson, M. Long-term durability of minimal invasive posterior transforaminal lumbar interbody fusion: A clinical and radiographic follow-up. J. Spinal Disord. Tech. 2011, 24, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, P.L.; Fraser, R.D.; Hall, D.J.; Cain, C.M.; Osti, O.L.; Potter, G.R. Short segment fixation of thoracolumbar burst fractures without fusion. Eur. Spine J. 1999, 8, 495–500. [Google Scholar] [CrossRef]
- Schnee, C.L.; Freese, A.; Ansell, L.V. Outcome analysis for adults with spondylolisthesis treated with posterolateral fusion and transpedicular screw fixation. J. Neurosurg. 1997, 86, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Slosar, P.J.; Reynolds, J.B.; Schofferman, J.; Goldthwaite, N.; White, A.H.; Keaney, D. Patient satisfaction after circumferential lumbar fusion. Spine 2000, 25, 722–726. [Google Scholar] [CrossRef]
- Taylor, V.M.; Deyo, R.A.; Ciol, M.; Farrar, E.L.; Lawrence, M.S.; Shonnard, N.H.; Leek, K.M.; McNeney, B.; Goldberg, H.I. Patient-oriented outcomes from low back surgery: A community-based study. Spine 2000, 25, 2445–2452. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.R.; Ring, D.; Scuderi, G.; Cohen, D.S.; Garfin, S.R. Predictors of outcome in patients with chronic back pain and low-grade spondylolisthesis. Spine 1997, 22, 2030–2034, discussion 2035. [Google Scholar] [CrossRef]
- Cheriyan, T.; Harris, B.; Cheriyan, J.; Lafage, V.; Spivak, J.M.; Bendo, J.A.; Errico, T.J.; Goldstein, J.A. Association between compensation status and outcomes in spine surgery: A meta-analysis of 31 studies. Spine J. 2015, 15, 2564–2573. [Google Scholar] [CrossRef]
- de Moraes, V.Y.; Godin, K.; Tamaoki, M.J.; Faloppa, F.; Bhandari, M.; Belloti, J.C. Workers’ compensation status: Does it affect orthopaedic surgery outcomes? A meta-analysis. PLoS ONE 2012, 7, e50251. [Google Scholar] [CrossRef]
- Anderson, J.T.; Haas, A.R.; Percy, R.; Woods, S.T.; Ahn, U.M.; Ahn, N.U. Return to Work After Diskogenic Fusion in Workers’ Compensation Subjects. Orthopedics 2015, 38, e1065–e1072. [Google Scholar] [CrossRef]
- Anderson, J.T.; Haas, A.R.; Percy, R.; Woods, S.T.; Ahn, U.M.; Ahn, N.U. Workers’ Compensation, Return to Work, and Lumbar Fusion for Spondylolisthesis. Orthopedics 2016, 39, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Mirza, S.K.; Martin, B.I.; Kreuter, W.; Goodman, D.C.; Jarvik, J.G. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010, 303, 1259–1265. [Google Scholar] [CrossRef] [PubMed]
- Lavin, R.A.; Tao, X.; Yuspeh, L.; Bernacki, E.J. Temporal relationship between lumbar spine surgeries, return to work, and workers’ compensation costs in a cohort of injured workers. J. Occup. Environ. Med. 2013, 55, 539–543. [Google Scholar] [CrossRef]
- Hedlund, R.; Johansson, C.; Hägg, O.; Fritzell, P.; Tullberg, T. Swedish Lumbar Spine Study Group. The long-term outcome of lumbar fusion in the Swedish lumbar spine study. Spine J. 2016, 16, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Rubinstein, S.M.; van Middelkoop, M.; Ostelo, R.; Verhagen, A.; Koes, B.; Peul, W.C. Surgery versus conservative management of sciatica due to a lumbar herniated disc: A systematic review. Eur. Spine J. 2011, 20, 513–522. [Google Scholar] [CrossRef]
- Lequin, M.B.; Verbaan, D.; Jacobs, W.C.; Brand, R.; Bouma, G.J.; Vandertop, W.P.; Peul, W.C.; Leiden-The Hague Spine Intervention Prognostic Study Group; Wilco, C.P.; Bart, W.K.; et al. Surgery versus prolonged conservative treatment for sciatica: 5-year results of a randomised controlled trial. BMJ Open 2013, 3, e002534. [Google Scholar] [CrossRef] [PubMed]
- Todd, N.V. The surgical treatment of non-specific low back pain. Bone Jt. J. 2017, 99, 1003–1005. [Google Scholar] [CrossRef]
- Sears, J.M.; Blanar, L.; Bowman, S.M.; Adams, D.; Silverstein, B.A. Predicting work-related disability and medical cost outcomes: Estimating injury severity scores from workers’ compensation data. J. Occup. Rehabil. 2013, 23, 19–31. [Google Scholar] [CrossRef]
- Sears, J.M.; Bowman, S.M.; Rotert, M.; Hogg-Johnson, S. A New Method to Classify Injury Severity by Diagnosis: Validation Using Workers’ Compensation and Trauma Registry Data. J. Occup. Rehabil. 2015, 25, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Daniels, A.H.; Kuris, E.O.; Kleinhenz, D.T.; Palumbo, M.A. Spine Surgery Outcomes in Workers’ Compensation Patients. J. Am. Acad. Orthop. Surg. 2017, 25, e225–e234. [Google Scholar] [CrossRef] [PubMed]
- Tabaraee, E.; Ahn, J.; Bohl, D.D.; Elboghdady, I.M.; Aboushaala, K.; Singh, K. The Impact of Worker’s Compensation Claims on Outcomes and Costs Following an Anterior Cervical Discectomy and Fusion. Spine 2015, 40, 948–953. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.T.; Haas, A.R.; Percy, R.; Woods, S.T.; Ahn, U.M.; Ahn, N.U. Chronic Opioid Therapy After Lumbar Fusion Surgery for Degenerative Disc Disease in a Workers’ Compensation Setting. Spine 2015, 40, 1775–1784. [Google Scholar] [CrossRef] [PubMed]
- Kukreja, S.; Kalakoti, P.; Ahmed, O.; Nanda, A. Predictors of reoperation-free survival following decompression-alone lumbar spine surgery for on-the-job injuries. Clin. Neurol. Neurosurg. 2015, 135, 41–45. [Google Scholar] [CrossRef]
- DeBerard, M.S.; Wheeler, A.J.; Gundy, J.M.; Stein, D.M.; Colledge, A.L. Presurgical biopsychosocial variables predict medical, compensation, and aggregate costs of lumbar discectomy in Utah workers’ compensation patients. Spine J. 2011, 11, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.T.; Haas, A.R.; Percy, R.; Woods, S.T.; Ahn, U.M.; Ahn, N.U. Clinical depression is a strong predictor of poor lumbar fusion outcomes among workers’ compensation subjects. Spine 2015, 40, 748–756. [Google Scholar] [CrossRef]
- Taylor, V.M.; Deyo, R.A.; Ciol, M.; Kreuter, W. Surgical treatment of patients with back problems covered by workers compensation versus those with other sources of payment. Spine 1996, 21, 2255–2259. [Google Scholar] [CrossRef] [PubMed]
- Rainville, J.; Sobel, J.B.; Hartigan, C.; Wright, A. The effect of compensation involvement on the reporting of pain and disability by patients referred for rehabilitation of chronic low back pain. Spine 1997, 22, 2016–2024. [Google Scholar] [CrossRef] [PubMed]
- Andreshak, T.G.; An, H.S.; Hall, J.; Stein, B. Lumbar spine surgery in the obese patient. J. Spinal Disord. 1997, 10, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Atlas, S.J.; Tosteson, T.D.; Hanscom, B.; Blood, E.A.; Pransky, G.S.; Abdu, W.A.; Andersson, G.B.; Weinstein, J.N. What is different about workers’ compensation patients? Socioeconomic predictors of baseline disability status among patients with lumbar radiculopathy. Spine 2007, 32, 2019–2026. [Google Scholar] [CrossRef]
- Hadler, N.M.; Carey, T.S.; Garrett, J. The influence of indemnification by workers’ compensation insurance on recovery from acute backache. North Carolina Back Pain Project. Spine 1995, 20, 2710–2715. [Google Scholar] [CrossRef]
- Volinn, E.; Van Koevering, D.; Loeser, J.D. Back sprain in industry. The role of socioeconomic factors in chronicity. Spine 1991, 16, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Schatman, M. Workers’ Compensation and Its Potential for Perpetuation of Disability. In Handbook of Occupational Health and Wellness; Gatchel, R.J., Schultz, I.Z., Eds.; Springer: Boston, MA, USA, 2012; pp. 341–361. [Google Scholar] [CrossRef]
- Khor, S.; Lavallee, D.; Cizik, A.M.; Bellabarba, C.; Chapman, J.R.; Howe, C.R.; Lu, D.; Mohit, A.A.; Oskouian, R.J.; Roh, J.R.; et al. Development and Validation of a Prediction Model for Pain and Functional Outcomes After Lumbar Spine Surgery. JAMA Surg. 2018, 153, 634–642. [Google Scholar] [CrossRef]
- Rudbeck, M.; Johansen, J.P.; Omland, Ø. A Follow-Up Study on Return to Work in the Year After Reporting an Occupational Injury Stratified by Outcome of the Workers’ Compensation System. J. Occup. Environ. Med. 2018, 60, 542–547. [Google Scholar] [CrossRef]
- Gallagher, R.M.; Williams, R.A.; Skelly, J.; Haugh, L.D.; Rauh, V.; Milhous, R.; Frymoyer, J. Workers’ Compensation and return-to-work in low back pain. Pain 1995, 61, 299–307. [Google Scholar] [CrossRef]
- Kenny, D.T. Returning to work after workplace injury: Impact of worker and workplace factors. J. Appl. Rehabil. Couns. 1998, 29, 13–19. [Google Scholar] [CrossRef]
- Glass, D. Investigation into the Management of Complex Workers Compensation Claims and WorkSafe Oversight; Victorian Ombudsman: Melbourne, Australia, 2016.
- Berecki-Gisolf, J.; Clay, F.J.; Collie, A.; McClure, R.J. The impact of aging on work disability and return to work: Insights from workers’ compensation claim records. J. Occup. Environ. Med. 2012, 54, 318–327. [Google Scholar] [CrossRef]
- ILO. GEIP: Contributing to Decent Work and the Social Protection Floor Guarantee in the Workplace. Available online: https://www.ilo.org/wcmsp5/groups/public/---ed_emp/---emp_ent/documents/publication/wcms_573083.pdf (accessed on 1 April 2021).
- Dworsky, M.; Broten, N. How Can Workers’ Compensation Systems Promote Occupational Safety and Health? Stakeholder Views on Policy and Research Priorities; RAND Corporation: Santa Monica, CA, USA, 2018. [Google Scholar] [CrossRef]
| Author | Year | Country | Type of Study | LOE | Sample Size WC | Sample Size NWC | Mean Age WC (y) | Mean Age NWC (y) | Mean Age (y) |
|---|---|---|---|---|---|---|---|---|---|
| Agazzi et al. [23] | 1999 | Switzerland | Retrospective | 3 | 34 | 37 | - | - | - |
| Albert et al. [24] | 2000 | USA | Retrospective | 3 | 28 | 9 | - | - | 40.3 ± 10.3 |
| Asch et al. [25] | 2002 | USA | Prospective | 2 | 80 | 132 | - | - | 41 ± 11.3 |
| Atlas et al. [26] | 2000 | USA | Prospective | 2 | 56 | 120 | 38.7 | 41.2 | - |
| Carreon et al. [27] | 2010 | USA | Case-control | 3 | 58 | 58 | 47.9 ± 9.4 | 47.8 ± 9.4 | - |
| Deutsch et al. [28] | 2006 | USA | Prospective | 2 | 4 | 16 | - | - | 49 |
| Greenough et al. [29] | 1994 | UK | Prospective | 2 | 106 | 45 | - | - | - |
| Greenough et al. [30] | 1998 | UK | Prospective | 2 | 66 | 62 | - | - | - |
| Gum et al. [16] | 2013 | USA | Case-control | 3 | 38 | 38 | 42 | 42.2 | - |
| Herron et al. [31] | 1996 | USA | Prospective | 2 | 89 | 186 | - | - | 43 (15–83) |
| Klekamp et al. [32] | 1998 | USA | Retrospective | 3 | 23 | 27 | 35.0 ± 7.1 | 39.5 ± 12.0 | - |
| Lew et al. [33] | 2001 | USA | Retrospective | 3 | 10 | 37 | 49.7 ± 9.8 | 50.7 ± 10.8 | - |
| MacKay et al. [34] | 1995 | USA | Prospective | 2 | 46 | 108 | - | - | 40 (20–79) |
| Madan et al. [18] | 2003 | UK | Prospective | 2 | 12 | 27 | - | - | 43 (25–67) |
| Marks et al. [35] | 2000 | USA | Retrospective | 3 | 51 | 51 | - | - | - |
| Montgomery et al. [36] | 2015 | New Zealand | Prospective | 2 | 120 | 49 | 53 (24–81) | 61 (31–82) | - |
| Parker et al. [37] | 1996 | USA | Prospective | 2 | 10 | 23 | - | - | 41 (22–56) |
| Pelton et al. [38] § | 2012 | USA | Prospective | 2 | 11 | 22 | - | - | 51.7 ± 12.2 |
| Pelton et al. [38] § | 2012 | USA | Prospective | 2 | 13 | 20 | - | - | 49.9 ± 10.7 |
| Penta et al. [39] | 1997 | Australia | Prospective | 2 | 61 | 42 | - | - | 48 (28–73) |
| Phan et al. [40] | 2017 | Australia | Prospective | 2 | 24 | 90 | 46.3 ± 10.4 | 60.2 ± 12.9 | - |
| Rouben et al. [41] | 2011 | USA | Retrospective | 3 | 14 | 155 | - | - | 44.5 ± 10.9 |
| Sanderson et al. [42] | 1999 | Australia | Retrospective | 3 | 12 | 12 | - | - | 33.1 ± 14.2 |
| Schnee et al. [43] | 1997 | USA | Retrospective | 3 | 20 | 32 | - | - | 53.4 (24–77) |
| Slosar et al. [44] | 2000 | USA | Retrospective | 3 | 73 | 60 | - | - | 38.8 (21–58) |
| Taylor et al. [45] | 2000 | USA | Prospective | 2 | 47 | 189 | - | - | 46 |
| Vaccaro et al. [46] | 1997 | USA | Case series | 4 | 13 | 11 | 37 | 39 | 38 (24–50) |
| Author | Last Follow-Up | Type of Surgery | Comparison | Outcomes Measures | Conclusions |
|---|---|---|---|---|---|
| Agazzi et al. [23] | 2 y | PLIF | Yes (internal) | Prolo economic and functional scale WC: 16/34 (47%); NWC: 31/37 (84%) RTW WC 2/33; NWC 24/30 | Socioeconomic factors and WC issues seem to be significant prognostic indicators of outcome. |
| Albert et al. [24] | 2 y | Anteroposterior fusion | Yes (internal) | Functional status Success: WC 18/27; NWC 9/27 Failure: WC 10/12; NWC 2/12 | WC increased the chance of functional failure, though this correlation was not statistically significant. |
| Asch et al. [25] | 3 y | Microdiscectomy | Yes (internal) | Pain relief success rate WC 67.9%; NWC 82.8% (p < 0.05) ODI success rate (< 40%) WC 63.5%; NWC 86.5% (p < 0.001) Satisfaction after surgery WC 63.2%; NWC 83.5% (p < 0.001) RTW WC 42.1%; NWC 71.5% (p < 0.001) | Progressively poorer outcomes occur with increasing patient age up to the late-50 s and confirms the disparity in outcomes between cases in which WC is being sought and those in which it is not. |
| Atlas et al. [26] | 4 y | Open discectomy, percutaneous discectomy | Yes | Relief from pain WC 20 (36%); NWC 81 (68%) RMDQ WC −9.3; NWC −12.5 Satisfaction WC 24 (43%); NWC 85 (71%) RTW WC 17/133 (13%); NWC 7/190 (4%) | Patients who have been receiving WC at baseline were more likely to be receiving disability benefits and were less likely to report relief from symptoms and improvement in quality of life at the time of the four-year follow-up than patients who had not been receiving WC at baseline. Nonetheless, most patients returned to work regardless of their initial disability status, and those who had been receiving WC at baseline were only slightly less likely to be working after four years. |
| Carreon et al. [27] | 2 y | PLF | Yes | NRS back WC 1.7 ± 3.1; NWC 2.5 ± 2.7 (p = 0.073) ODI WC 4.9 ± 14.1; NWC 13.3 ± 17.1 (p = 0.009) SF-36 WC −1.3 ± 9.7; NWC 3.9 ± 8.9 (p = 0.007) | Patients on WC have significantly less improvement of clinical outcomes in both mean change in ODI and SF-36, as well as the number of patients achieving substantial clinical benefit. |
| Deutsch et al. [28] | 1 y | Unilateral TLIF with PLF | Yes, but not clearly defined | ODI WC: 3/4 patients improved at 6 months RTW WC: 2/4 | No differences between WC and NWC were reported concerning to disability and RTW. |
| Greenough et al. [29] | 2 y | ALIF | Yes | Satisfaction after surgery (p < 0.05) 8–10: WC (35; 37%); NWC (28; 67%) 5–7: WC (37; 40%); NWC (8; 19%) 2–4: WC (18; 19%); NWC (3; 7%) 0–1: WC (4; 4%); NWC (3; 7%) LBOS (p < 0.01) Excellent: WC (8; 10%); NWC (13; 43%) Good: WC (19; 22%); NWC (10; 25%) Fair: WC (34; 40%); NWC (10; 25%) Poor: WC (24; 28%); NWC (7; 17%) | The rate of fusion was influenced by the presence of a WC claim. WC status and psychological disturbance at presentation were significant prognostic factors. Psychological disturbance at review had a profound effect on the outcome and patient satisfaction ratings. |
| Greenough et al. [30] | 2 y | PLF | Yes | LBOS WC 25 (7–72, n = 57); NWC 35 (7–75, n = 63) p < 0.001 Satisfaction after surgery WC 2 (0–3, n = 56); NWC 2 (0–3, n = 59) p < 0.02 VAS WC 6 (1–10, n = 57); NWC 5 (0–10, n = 62) p < 0.02 | Results of instrumented PLF are poor and indications for the procedure need careful consideration. The results are significantly influenced by WC but not by technical success. |
| Gum et al. [16] | 2 y | TLIF or PLF | Yes | VAS WC 0.94; NWC 2.51 (p = 0.011) ODI mean change WC 5.54; NWC 15.17 (p = 0.009) SF-36 mean change WC 1.69; NWC 4.09 (p = 0.235) | Patients receiving WC have the perception of poor clinical outcomes after lumbar fusion. |
| Herron et al. [31] | 4 y | Laminectomy and discectomy | Yes (internal) | Surgical outcome (p = 0.00) Good: WC 52 (58%); NWC 174 (94%) Fair: WC 16 (18%); NWC 10 (5%) Poor: WC 21 (24%); NWC 2 (1%) | Patients with WC or litigation issues were significantly more likely to have poor outcomes. |
| Klekamp et al. [32] | 11 m | Discectomy | Yes | WC: 29% of patients achieved good results NWC: 81% of patients achieved good results | WC group achieved worse results compared to NWC group. |
| Lew et al. [33] | 18 m (4–51 m) | Discectomy | Yes | Satisfaction after surgery (%) Excellent or good WC: 7 (70); NWC: 33 (89) p = 0.12 Excellent WC: 5 (50); NWC: 22 (60) p = 0.24 Good WC: 2 (20); NWC: 11 (30) p = 0.27 Fair WC: 0 (0); NWC: 2 (5.4) p = 0.62 Poor WC: 3 (30); NWC: 2 (5.4) p = 0.05 RTW WC: 90%; NWC: 93% p = 0.45 | WC recipients experienced significantly worse outcomes than the other patients in this study. Nevertheless, a high RTW rate was maintained (90%) in both groups. |
| MacKay et al. [34] | 1 y | Hemilaminotomy, discectomy | Yes | Prolo scale Satisfactory: WC: 63%; NWC: 92% (p < 0.0001) Unsatisfactory: WC: 37%; NWC: 8% | WC group had a lower success rate compared to NWC group. |
| Madan et al. [18] | 2.4 y (2–3.1 y) | PLF and PLIF | Yes (internal) | ODI ALIF group (p = 0.0056) Satisfied WC: 6 (50); NWC: 25 (92.6) Unsatisfied WC: 6 (50); NWC: 2 (7.4) PLIF (p = 0.0064) Satisfied WC: 4 (45); NWC: 24 (92.3) Unsatisfied WC: 5 (55.5); NWC 2 (7.7) | There were no differences between WC and NWC groups concerning to disability. |
| Marks et al. [35] | 30.7 ± 17.9 m | Percutaneous discectomy | Yes, but not clearly defined | Pain, Job function, Physical restrictions, medications WC and NWC no differences (data not available), p > 0.05 | WC status does not influence the outcomes. |
| Montgomery et al. [36] | 8 y (4–14 y) | Lumbar spinal fusion | Yes | RMDQ 1-year postoperative WC: 8.0, 6.8–9.2/NWC: 4.6, 2.8–6.5 (p < 0.05) At long-term follow-up WC: 5.9, 4.7–7.1/NWC: 3.8, 1.9–5.8 (p > 0.05) LBOS 1 year post-operative WC: 43.9, 39.9–48.0/NWC: 54.1, 48.4–59.9 (p < 0.05) Long term follow-up WC: 47.0, 43.5–50.4/NWC: 55.4, 49.3–61.6 (p > 0.05) SF12 Long term follow up WC 41.6 ± 11.5/NWC 44.0 ± 13.0 (p > 0.05) | ACC patients achieved equivalent improvements compared to non-ACC patients and NWC patients as per in the published literature. They also achieve function that is considerably better than that achieved in WC patients in adversarial compensation jurisdictions. |
| Parker et al. [37] | 47 m (27–84 m) | PLF | Yes | Clinical outcome pain, medications, and resume of previous activities WC: 1/10 good, 9/10 poor results NWC: 9/23 good or excellent, 3/23 fair, 11/23 poor results | Patients in WC group showed worse clinical outcomes compared to NWC group. |
| Pelton et al. [38] | 6 m | MIS-TLIF and open TLIF | Yes | VAS (MIS-TLIF cohort) Differences between WC and NWC (p = 0.712) VAS (open TLIF cohort) Differences between WC and NWC (p = 0.241) | Immediate outcomes and hospitalizations between NWC and WC populations did not differ regardless of surgical technique (MIS/open). Differences occurred in improved outcomes with an MIS-TLIF versus an open TLIF even in a WC environment. |
| Penta et al. [39] | 10 y | ALIF | Yes | LBOS WC: 38 (4–74); NWC: 45 (11–75) (p = 0.06) VAS WC: 4 (0–9), NWC: 4 (0–10) (p = 0.29) | WC had a negative effect on outcomes only in the first period (two years). After 10 years of follow up this effect disappeared. |
| Phan et al. [40] | 2 y | ALIF | Yes | SF-12 WC: 11.3; NWC: 9.1 (p = 0.691) ODI WC: 26.3; NWC: 33.4 (p = 0.232) | No significant differences found between WC and NWC patients in terms of fusion rates, complications, clinical outcomes. |
| Rouben et al. [41] | 50 m | MIS-TLIF | Yes (internal) | RTW 57% of WC patients (mean time: 17 weeks) ODI Mean change of 34% (p < 0.001) Post-operative VAS Significant improvement WC patients (p < 0.001) | WC patients responded well to surgical treatment. |
| Sanderson et al. [42] | 3.1 y | Short segment fixation | Yes | LBOS WC: 45.1; NWC: 67.4 (p < 0.05) | The presence of a WC claim positively influenced the outcomes after surgery. |
| Schnee et al. [43] | 18.6 m (6–36.7 m) | PLF | Not clearly defined | RTW WC: not defined; NWC: 84% of cases; Prolo scale Significant adverse effects of WC (p = 0.0001). Good pain results were seen in 81% of NWC | WC claims and smoking had very significant adverse impacts on both employment and pain results despite high fusion rates, particularly in patients under the age of 55. |
| Slosar et al. [44] | 37.2 m | ALIF + PLF | Yes, but not clearly defined | Satisfaction after surgery (p > 0.05) 1 (best): WC 7 (9.6%); NWC 7 (11.7%) 2: WC 36 (49.3); NWC 32 (53.3%) 3: WC 14 (19.1%); NWC 12 (20%) 4: WC 16 (22%); NWC 9 (15%) | There was not a statistically significant difference in terms of satisfaction following surgery between WC and NWC patients. |
| Taylor et al. [45] | 18 m | Discectomy, laminectomy, or fusion | Not clearly defined | Much better functioning WC: 52%; NWC: 68% p < 0.05 Very positive about the treatment WC: 57%; NWC: 71% p < 0.05 | The study results indicate that WC payments and litigation are two important predictors of poor outcomes after low back surgery in community practice. |
| Vaccaro et al. [46] | 37 m (18–64 m) | Uninstrumented PLF | No | Satisfaction after surgery Fair/poor results: WC: 13; NWC: 2 RTW None of the WC patients returned to work | WC is strongly associated with poor results of operative management of LBP in adult patients with low-grade spondylolisthesis. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Russo, F.; De Salvatore, S.; Ambrosio, L.; Vadalà, G.; Fontana, L.; Papalia, R.; Rantanen, J.; Iavicoli, S.; Denaro, V. Does Workers’ Compensation Status Affect Outcomes after Lumbar Spine Surgery? A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6165. https://doi.org/10.3390/ijerph18116165
Russo F, De Salvatore S, Ambrosio L, Vadalà G, Fontana L, Papalia R, Rantanen J, Iavicoli S, Denaro V. Does Workers’ Compensation Status Affect Outcomes after Lumbar Spine Surgery? A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(11):6165. https://doi.org/10.3390/ijerph18116165
Chicago/Turabian StyleRusso, Fabrizio, Sergio De Salvatore, Luca Ambrosio, Gianluca Vadalà, Luca Fontana, Rocco Papalia, Jorma Rantanen, Sergio Iavicoli, and Vincenzo Denaro. 2021. "Does Workers’ Compensation Status Affect Outcomes after Lumbar Spine Surgery? A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 11: 6165. https://doi.org/10.3390/ijerph18116165
APA StyleRusso, F., De Salvatore, S., Ambrosio, L., Vadalà, G., Fontana, L., Papalia, R., Rantanen, J., Iavicoli, S., & Denaro, V. (2021). Does Workers’ Compensation Status Affect Outcomes after Lumbar Spine Surgery? A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(11), 6165. https://doi.org/10.3390/ijerph18116165












