The Relationship between Reactive Balance Control and Back and Hamstring Strength in Physiotherapists with Non-Specific Back Pain: Protocol for a Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
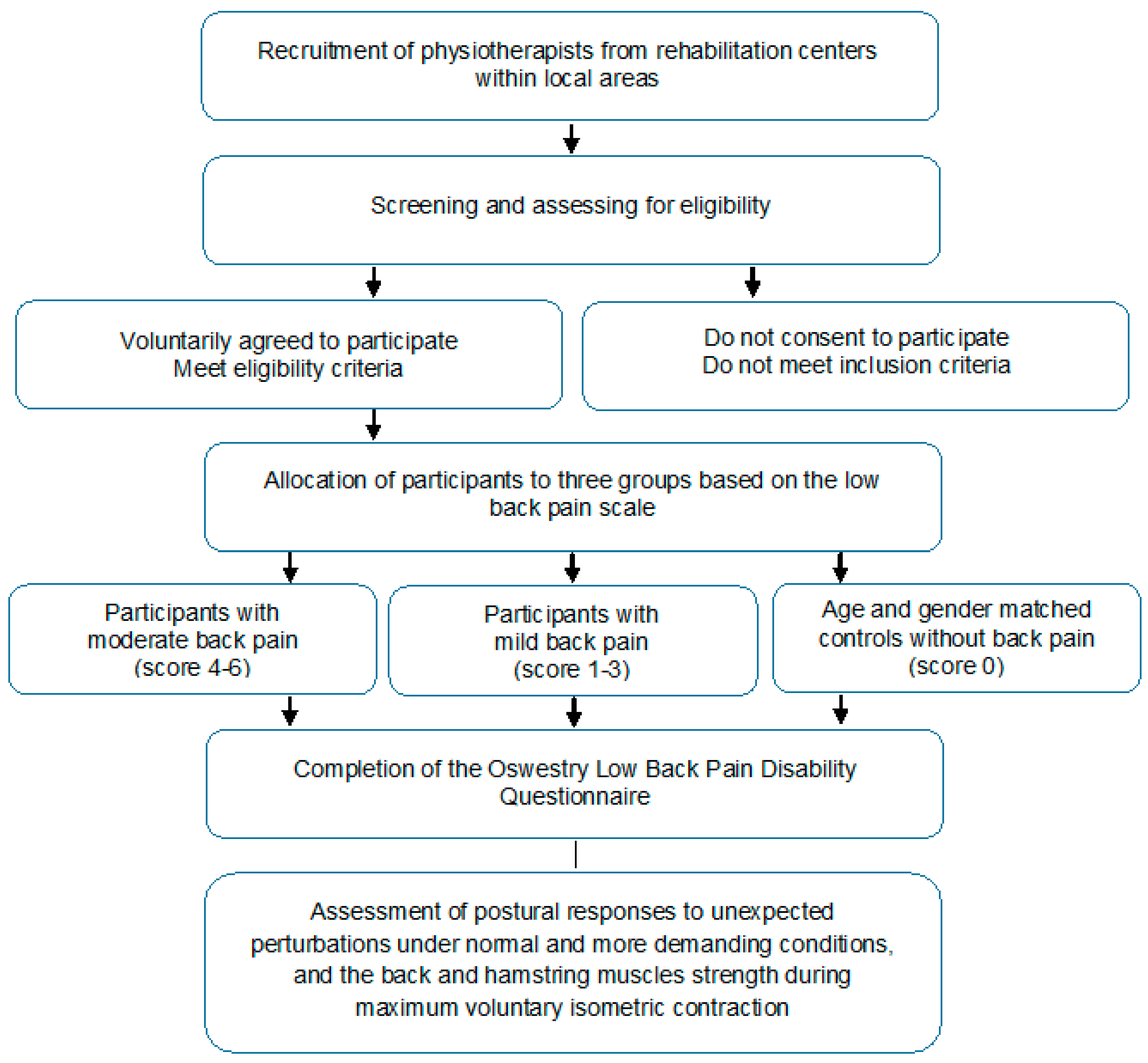
2.1. Study Design
2.2. Participants and Setting
2.3. Inclusion and Exclusion Criteria
2.4. Allocation
2.5. Sample Size Estimation
2.6. Procedures
2.7. Data Collection and Management
2.8. Descriptive Measures
2.9. Primary Outcomes
Oswestry Disability Index
2.10. Secondary Outcomes
2.10.1. Postural Responses to Unexpected Perturbations
2.10.2. Maximal Strength of the Back and Hamstring Muscles
2.11. Patient and Public Involvement
2.12. Ethics and Dissemination
2.13. Statistical Analysis
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Hogan, D.A.M.; O’Sullivan, L.W.; Nolan, S.; Greiner, B.A. Are Irish therapists at heightened risk for low back pain? Occup. Med. (Lond). 2016, 66, 351–357. [Google Scholar] [CrossRef]
- Mehrdad, R.; Narges Shams-Hosseini, N.S.; Aghdaei, S.; Yousefian, M. Prevalence of low back pain in health care workers and comparison with other occupational categories in Iran: A systematic review. Iran J. Med. Sci. 2016, 41, 467–478. [Google Scholar]
- Milhem, M.; Kalichman, L.; Ezra, D.; Alperovitch-Najenson, D. Work-related musculoskeletal disorders among physical therapists: A comprehensive narrative review. Int. J. Occup. Med. Environ. Health. 2016, 29, 735–747. [Google Scholar] [CrossRef] [PubMed]
- Awosan, K.J.; Yikawe, S.S.; Oche, O.M.; Oboirien, M. Prevalence, perception and correlates of low back pain among healthcare workers in tertiary health institutions in Sokoto, Nigeria. Ghana Med. J. 2017, 51, 164–174. [Google Scholar]
- Çınar-Medeni, Ö.; Elbasan, B.; Duzgun, I. Low back pain prevalence in healthcare professionals and identification of factors affecting low back pain. J. Back Musculoskelet. Rehabil. 2017, 30, 451–459. [Google Scholar] [CrossRef]
- Riccò, M.; Pezzetti, F.; Signorelli, C. Back and neck pain disability and upper limb symptoms of home healthcare workers: A case-control study from Northern Italy. Int. J. Occup. Med. Environ. Health. 2017, 30, 291–304. [Google Scholar] [CrossRef]
- Şimşek, S.; Yağcı, N.; Şenol, H. Prevalence of and risk factors for low back pain among healthcare workers in Denizli. Agri 2017, 29, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Alnaami, I.; Awadalla, N.J.; Alkhairy, M.; Alburidy, S.; Alqarni, A.; Algarni, A.; Alshehri, R.; Amrah, B.; Alasmari, M.; Mahfouz, A.A. Prevalence and factors associated with low back pain among health care workers in southwestern Saudi Arabia. BMC Musculoskelet. Disord. 2019, 20, 56. [Google Scholar] [CrossRef]
- Mekonnen, T.H. Work-related factors associated with low back pain among nurse professionals in East and West Wollega Zones, Western Ethiopia, 2017: A cross-sectional study. Pain Ther. 2019, 8, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Mroczek, B.; Łubkowska, W.; Jarno, W.; Jaraczewska, E.; Mierzecki, A. Occurrence and impact of back pain on the quality of life of healthcare workers. Ann. Agric. Environ. Med. 2020, 27, 36–42. [Google Scholar] [CrossRef]
- Koch, C.; Hänsel, F. Non-specific low back pain and postural control during quiet standing: A systematic review. Front. Psychol. 2019, 10, 586. [Google Scholar] [CrossRef]
- Ruhe, A.; Fejer, R.; Walker, B. Center of pressure excursion as a measure of balance performance in patients with non-specific low back pain compared to healthy controls: A systematic review of the literature. Eur. Spine J. 2011, 20, 358–368. [Google Scholar] [CrossRef] [PubMed]
- Zemková, E.; Kováčiková, Z.; Jeleň, M.; Neumannová, K.; Janura, M. Postural and trunk responses to unexpected perturbations depend on the velocity and direction of platform motion. Physiol. Res. 2016, 65, 769–776. [Google Scholar] [CrossRef]
- Zemková, E.; Štefániková, G.; Muyor, J.M. Load release balance test under unstable conditions effectively discriminates between physically active and sedentary young adults. Hum. Mov. Sci. 2016, 48, 142–152. [Google Scholar] [CrossRef]
- Henry, S.M.; Hitt, J.R.; Jones, S.L.; Bunn, J.Y. Decreased limits of stability in response to postural perturbations in subjects with low back pain. Clin. Biomech. (Bristol, Avon) 2006, 21, 881–892. [Google Scholar] [CrossRef]
- Behennah, J.; Conway, R.; Fisher, J.; Osborne, N.; Steele, J. The relationship between balance performance, lumbar extension strength, trunk extension endurance, and pain in participants with chronic low back pain, and those without. Clin. Biomech. 2018, 53, 22–30. [Google Scholar] [CrossRef]
- Biering-Sørensen, F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine (Phila Pa 1976) 1984, 9, 106–119. [Google Scholar] [CrossRef]
- Demoulin, C.; Vanderthommen, M.; Duysens, C.; Crielaard, J.M. Spinal muscle evaluation using the Sorensen test: A critical appraisal of the literature. Joint Bone Spine. 2006, 73, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Karwowski, W.; Marras, W.S. (Eds.) The Occupational Ergonomics Handbook; CRC Press: Boca Raton, FL, USA, 1999. [Google Scholar]
- Rosecrance, J.C.; Cook, T.M.; Golden, N.S. A comparison of isometric strength and dynamic lifting capacity in men with work-related low back injuries. J. Occup. Rehabil. 1991, 1, 197–205. [Google Scholar] [CrossRef]
- Zemková, E.; Cepková, A.; Uvaček, M.; Hamar, D. A new method to assess the power performance during a lifting task in young adults. Measurement 2016, 91, 460–467. [Google Scholar] [CrossRef]
- Zemková, E.; Poór, O.; Pecho, J. Peak rate of force development and isometric maximum strength of back muscles are associated with power performance during load-lifting tasks. Am. J. Men’s Health 2019, 13, 1–8. [Google Scholar] [CrossRef]
- Jones-Hershinow, C. An evaluation of the relationship between core endurance and lower extremity strength, and the ability to recover after perturbation. UNC’s Undergrad. Res. J. 2016, 5, 31–43. [Google Scholar]
- Balagué, F.; Mannion, A.F.; Pellisé, F.; Cedraschi, C. Non-specific low back pain. Lancet 2012, 379, 482–491. [Google Scholar] [CrossRef]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef]
- Burton, A.K.; Tillotson, K.M.; Main, C.J.; Hollis, S. Psychosocial predictors of outcome in acute and subchronic low back trouble. Spine (Phila Pa 1976) 1995, 20, 722–728. [Google Scholar] [CrossRef]
- Dunn, K.M.; Jordan, K.; Croft, P.R. Characterizing the course of low back pain: A latent class analysis. Am. J. Epidemiol. 2006, 163, 754–761. [Google Scholar] [CrossRef]
- Tamcan, O.; Mannion, A.F.; Eisenring, C.; Horisberger, B.; Elfering, A.; Müller, U. The course of chronic and recurrent low back pain in the general population. Pain 2010, 150, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Axén, I.; Bodin, L.; Bergström, G.; Halasz, L.; Lange, F.; Lövgren, P.W.; Rosenbaum, A.; Leboeuf-Yde, C.; Jensen, I. Clustering patients on the basis of their individual course of low back pain over a six month period. BMC Musculoskelet. Disord. 2011, 12, 99. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine. 2000, 25, 2940–2952. [Google Scholar] [CrossRef] [PubMed]
- Davidson, M.; Keating, J.L. A comparison of five low back disability questionnaires: Reliability and responsiveness. Phys. Ther. 2002, 82, 8–24. [Google Scholar] [CrossRef] [PubMed]
- Garhammer, J. A review of power output studies of Olympic and powerlifting: Methodology, performance prediction, and evaluation tests. J. Strength Cond. Res. 1993, 7, 76–89. [Google Scholar] [CrossRef]
- McCall, A.; Nedelec, M.; Carling, C.; Le Gall, F.; Berthoin, S.; Dupont, G. Reliability and sensitivity of a simple isometric posterior lower limb muscle test in professional football players. J. Sports Sci. 2015, 33, 1298–1304. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Mierzejewski, M.; Kumar, S. Prevalence of low back pain among physical therapists in Edmonton, Canada. Disabil. Rehabil. 1997, 19, 309–317. [Google Scholar] [CrossRef]
- Holder, N.L.; Clark, H.A.; DiBlasio, J.M.; Hughes, C.L.; Scherpf, J.W.; Harding, L.; Shepard, K.F. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Phys. Ther. 1999, 79, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.H.; Her, J.G.; Ko, T.; Ko, J.; Kim, H.; Lee, J.S.; Woo, J. Work-related musculoskeletal disorders among Korean physical therapists. J. Phys. Ther. Sci. 2013, 25, 55–59. [Google Scholar] [CrossRef][Green Version]
- Nourollahi, M.; Afshari, D.; Dianat, I. Awkward trunk postures and their relationship with low back pain in hospital nurses. Work 2018, 59, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Roffey, D.M.; Wai, E.K.; Bishop, P.; Kwon, B.K.; Dagenais, S. Causal assessment of awkward occupational postures and low back pain: Results of a systematic review. Spine J. 2010, 10, 89–99. [Google Scholar] [CrossRef]
- Radebold, A.; Cholewicki, J.; Panjabi, M.M.; Patel, T.C. Muscle response pattern to sudden trunk loading in healthy individuals and in patients with chronic low back pain. Spine (Phila Pa 1976) 2000, 25, 947–954. [Google Scholar] [CrossRef]
- Cholewicki, J.; Silfies, S.P.; Shah, R.A.; Greene, H.S.; Reeves, N.P.; Alvi, K.; Goldberg, B. Delayed trunk muscle reflex responses increase the risk of low back injuries. Spine (Phila Pa 1976) 2005, 30, 2614–2620. [Google Scholar] [CrossRef]
- Reeves, N.P.; Cholewicki, J.; Milner, T.E. Muscle reflex classification of low-back pain. J. Electromyogr. Kinesiol. 2005, 15, 53–60. [Google Scholar] [CrossRef]
- MacDonald, D.; Moseley, G.L.; Hodges, P.W. People with recurrent low back pain respond differently to trunk loading despite remission from symptoms. Spine (Phila Pa 1976) 2010, 35, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Borghuis, J.; Hof, A.L.; Lemmink, K.A. The importance of sensory-motor control in providing core stability: Implications for measurement and training. Sports Med. 2008, 38, 893–916. [Google Scholar] [CrossRef]
- de Sousa, C.S.; de Jesus, F.L.A.; Machado, M.B.; Ferreira, G.; Ayres, I.G.T.; de Aquino, L.M.; Fukuda, T.Y.; Gomes-Neto, M. Lower limb muscle strength in patients with low back pain: A systematic review and meta-analysis. J. Musculoskelet. Neuronal. Interact. 2019, 19, 69–78. [Google Scholar]
- Nourbakhsh, M.R.; Arab, A.M. Relationship between mechanical factors and incidence of low back pain. J. Orthop. Sports Phys. Ther. 2002, 32, 447–460. [Google Scholar] [CrossRef]
- Tsai, Y.-S.; Sell, T.C.; Smoliga, J.M.; Myers, J.B.; Learman, K.E.; Lephart, S.M. A comparison of physical characteristics and swing mechanics between golfers with and without a history of low back pain. J. Orthop. Sports Phys. Ther. 2010, 40, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Cai, C.; Kong, P.W. Low back and lower-limb muscle performance in male and female recreational runners with chronic low back pain. J. Orthop. Sports Phys. Ther. 2015, 45, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Cooper, N.A.; Scavo, K.M.; Strickland, K.J.; Tipayamongkol, N.; Nicholson, J.D.; Bewyer, D.C.; Sluka, K.A. Prevalence of gluteus medius weakness in people with chronic low back pain compared to healthy controls. Eur. Spine J. 2016, 25, 1258–1265. [Google Scholar] [CrossRef]
- Marshall, P.W.; Patel, H.; Callaghan, J.P. Gluteus medius strength, endurance, and co-activation in the development of low back pain during prolonged standing. Hum. Mov. Sci. 2011, 30, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Nadler, S.F.; Malanga, G.A.; Bartoli, L.A.; Feinberg, J.H.; Prybicien, M.; Deprince, M. Hip muscle imbalance and low back pain in athletes: Influence of core strengthening. Med. Sci. Sports Exerc. 2002, 34, 9–16. [Google Scholar] [CrossRef]
- Nadler, S.F.; Malanga, G.A.; DePrince, M.; Stitik, T.P.; Feinberg, J.H. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin. J. Sport Med. 2000, 10, 89–97. [Google Scholar] [CrossRef]
- Coulombe, B.J.; Games, K.E.; Neil, E.R.; Eberman, L.E. Core stability exercise versus general exercise for chronic low back pain. J. Athl. Train. 2017, 52, 71–72. [Google Scholar] [CrossRef] [PubMed]
- Bernet, B.A.; Peskura, E.T.; Meyer, S.T.; Bauch, P.C.; Donaldson, M.B. The effects of hip-targeted physical therapy interventions on low back pain: A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2019, 39, 91–100. [Google Scholar] [CrossRef]
- Kim, B.; Yim, J. Core stability and hip exercises improve physical function and activity in patients with non-specific low back pain: A randomized controlled trial. Tohoku J. Exp. Med. 2020, 251, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Karahan, A.; Kav, S.; Abbasoglu, A.; Dogan, N. Low back pain: Prevalence and associated risk factors among hospital staff. J. Adv. Nurs. 2009, 65, 516–524. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zemková, E.; Ďurinová, E.; Džubera, A.; Horníková, H.; Chochol, J.; Koišová, J.; Šimonová, M.; Zapletalová, L. The Relationship between Reactive Balance Control and Back and Hamstring Strength in Physiotherapists with Non-Specific Back Pain: Protocol for a Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 5578. https://doi.org/10.3390/ijerph18115578
Zemková E, Ďurinová E, Džubera A, Horníková H, Chochol J, Koišová J, Šimonová M, Zapletalová L. The Relationship between Reactive Balance Control and Back and Hamstring Strength in Physiotherapists with Non-Specific Back Pain: Protocol for a Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(11):5578. https://doi.org/10.3390/ijerph18115578
Chicago/Turabian StyleZemková, Erika, Eva Ďurinová, Andrej Džubera, Henrieta Horníková, Juraj Chochol, Jana Koišová, Michaela Šimonová, and Ludmila Zapletalová. 2021. "The Relationship between Reactive Balance Control and Back and Hamstring Strength in Physiotherapists with Non-Specific Back Pain: Protocol for a Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 11: 5578. https://doi.org/10.3390/ijerph18115578
APA StyleZemková, E., Ďurinová, E., Džubera, A., Horníková, H., Chochol, J., Koišová, J., Šimonová, M., & Zapletalová, L. (2021). The Relationship between Reactive Balance Control and Back and Hamstring Strength in Physiotherapists with Non-Specific Back Pain: Protocol for a Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(11), 5578. https://doi.org/10.3390/ijerph18115578






